Highlights
-
•
Here we reported a rare case of hepatic portal venous gas with a relevant review of literature.
-
•
Actually the mechanism of HPVG is still unknown.
-
•
The case present in literature are few and the mortality, generally caused by complications like necrotizing enterocolitis, is still high.
Keywords: Portal system, Endoscopy/gastrointestinal, Intestinal fistula
Abstract
Introduction
Hepatic portal venous gas (HPVG) is a rare radiological finding in which gas enters the portal venous system and it is associated in case of necrotizing colitis with a mortality of 75%. We report a case of iatrogenic HPVG with a review of literature.
Presentation of case
A 41 years old patient underwent total colectomy and ileal pouch- anal anastomosis with derivative ileostomy for a familiar adenomatous polyposis coli in June 2008. A stenosis of the pouch-anal anastomosis developed. The patient underwent several endoscopic dilations. A recurrence of the stenosis was observed. The patient underwent to several endoscopic procedure. After the last colonoscopy the patient showed a fever with abdominal pain. A CT scan showed little peri-anastomotic collections and massive hepatic portal venous gas.
Discussion
The management of HPVG varied from surgical intervention to non-operative procedure. The surgical approach it's reserved to clinically unstable patients or those with evidence of peritonitis or bowel perforation. Stable patients, like those with an HPVG consequence of an endoscopic procedure, can be treated with non- operative management.
Conclusion
Our experience confirm that hepatic portal venous gas can be related to endoscopic procedure; thus, it can be managed on the basis of patient's general clinical conditions, and in selected cases it will disappear without therapeutic interventions with a good outcome.
1. Introduction
Hepatic portal venous gas (HPVG) is a rare radiological finding in which gas enters the portal venous system and it is associated in case of necrotizing colitis [1] with a mortality of 75% [2].
In 2001 and 2009 Kinoshita [1] and Nelson [3] respectively, demonstrated a decrease of mortality up to 39%.
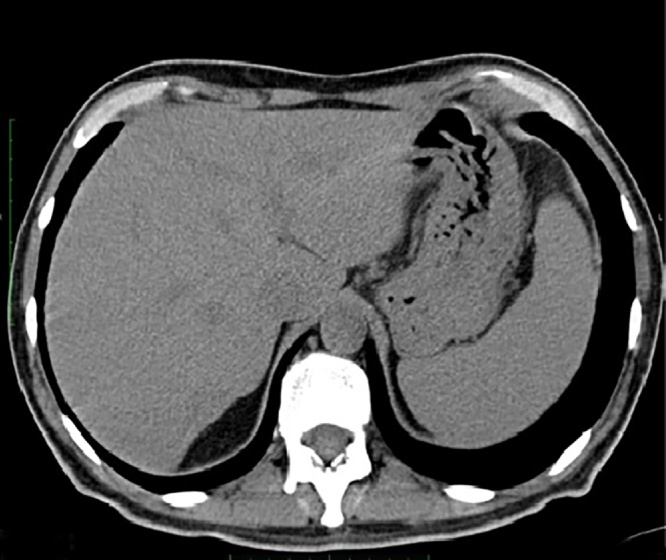
Different conditions are predisposing for HPVG such as, abdominal infections, bowel ischemia, gastric emphysema, Crohn’s disease or endoscopic procedures. In last years thanks to the development of radiological techniques such as CT scan and ultrasonography the diagnosis of case of HPVG is increased, with a better prognosis for iatrogenic cases (Fig. 1, Fig. 2, Fig. 3, Fig. 4). Our work has been reported in line with the SCARE criteria [5].
Fig. 1.
xxxxx.
Fig. 2.
xxxxx.
Fig. 3.
xxxxx.
Fig. 4.
xxxxx.
2. Presentation of case
A 41 years old patient underwent total colectomy and ileal pouch-anal anastomosis with derivative ileostomy for a familiar adenomatous polyposis coli in June 2008. Pathologic examination of the specimen showed a pT1 N1 adenocarcinoma of the rectum. The patient underwent chemo-radiation and subsequent adjuvant chemotherapy. A stenosis of the pouch-anal anastomosis developed. The patient underwent several endoscopic dilations. The ileostomy was taken down in March 2016. A recurrence of the stenosis and a peri-anastomotic collection were observed. An endoscopic drainage of the collection was performed on October 3rd, 2016. The CT scan performed on October 7th showed a reduction of peri-anastomotic fluid collection without evidence of portal pneumatosis. The endoluminal drainage was removed and during an endoscopic procedure with CO2 the fistula was closed with an OVESCO® clip on October 10th. The patient was re-admitted on October 19th with fever (38.8 °C) without leucocytosis.An endoscopic examination of the pouch showed absence of purulent discharge but many fistulous orifices around the pouch- anal anastomosis were detected (Table 1).
Table 1.
XXXX.
| Authors- years | Underlying clinical conditions | Number of patients |
|---|---|---|
| Vollman [8], 1976 | Necrotizing enterocolites | 1 (infant) |
| Bach [9], 1982 | Intra-abdomial abscess | 1 |
| Birnberg [10], 1983 | Ulcerative colitis | 1 |
| Merritt [11], 1984 | Necrotizing enterocolites | 12 (infants) |
| Benson [12], 1985 | Digestive tract dilation | 1 |
| Huycke [13], 1985 | Complication of endoscopic procedure |
1 |
| Radin [14], 1987 | Digestive tract dilation | 1 |
| Chezmar [15] 1989 | Liver transplant | 7 |
| Kirsch [16],1990 | Crohn’s disease | 1 |
| Lee [17], 1993 | Suppurative cholangitis | n.v |
| Herman [18], 1995 | Complication of endoscopic procedure |
1 |
| Quirke [19], 1995 | Ileus | 1 |
| Mallens [20], Li 1995 | Cystic fibrosis | 1 |
| Chen [21], 1997 | Seizures | 1 |
| Nguyen [22], 1998 | Complication of endoscopic procedure |
1 |
| Chang [23], 1999 | Gastric ulcer | 1 |
| Nakao [24], 1999 | Intra-abdomial abscess - tumor | 1 |
| Saksena [25], 2003 | Colchicine toxicity | 1 |
| Sellner [26], 2007 | diverticulitis | 1 |
| Sen [27], 2009 | diverticulitis | 1 |
| Hussain [28] 2009 | Gastric ulcer | 1 |
| Siswojo [29], 2010 | Mesenteric ischemiae | 1 |
| Oehler [30], 2013 | Mesenteric ischemiae | 1 |
| Cunningham [31], 2014 | Crohn’s disease | 1 |
| Khalaf [32], 2014 | Mesenteric ischemiae | 1 |
| Maezawa [33], 2015 | Mesenteric ischemiae | 1 |
| Sadatomo [34]2015 | Complication of endoscopic procedure | 1 |
| Solakoglu [35] 2016 | Complication of endoscopic procedure |
1 |
| Sawano [36] 2016 | Complication of endoscopic procedure |
1 |
| Castreen [37] 2016 | Complication of right hemicolectomy | 1 |
| Moser [38] 2016 | Complication of diverticulitis | 1 |
| Yamadera [39] 2016 | Crohn’s disease | 1 |
| Nevins [40] 2016 | Dilatated loops of small bowel | 1 |
| Okada [41] 2016 | Complication of abdominal surgery | 4 |
| Ginesu [42] 2017 | Complication of left colectomy | 1 |
| Bangash [43] 2017 | Complication of radical cystectomy and neobladder formation | 1 |
| Ghoz [44] 2017 | Perforation of antral gastric ulcer |
1 |
| Mc Nicholas [45] 2017 | Acute pancreatitis | 1 |
| Li [46] 2017 | Complicaiton of colon cancer resection |
1 |
| Niu [47] 2018 | Complication of transcatheter cardiac defibrillator implantation |
1 |
A CT scan showed little peri-anastomotic collections (panel B) with air-fluid levels and massive hepatic portal venous gas (panel A). The patient was in good clinical conditions, apyretic, blood tests showed: WBC: 4290/μL, Procalcitonin: 010 ng/ml.
Based on clinical findings, antibiotic treatment with meropenem (500 mg tid i.v.) was administered without further diagnostic or therapeutic interventions, assuming that the portal pneumatosis was due to the endoscopic examination. One day later a new CT scan detected a marked reduction of hepatic portal venous gas (panel C); the patient resumed oral feeding and three days later was discharged.
3. Discussion
Wolfe [4] in 1955 first described a case of HPVG in infants associated with serious underlying disease and high mortality rate. Finding of a relevant amount of gas in portal venous system has traditionally been associated with serious clinical conditions with poor outcome, as it happens in abdominal abscess or intestinal infarction [5]. HPVG is the result of accumulation of gas in the porto-mesenteric system through veins or lymphatics of the intestinal wall [6].
In some cases, venous hepatic gas is an incidental finding and it has been described as a consequence of diagnostic or therapeutic invasive procedures such as surgery, hepatic artery embolization, operative endoscopic procedures [7].
The management of HPVG varied from surgical intervention to non-operative procedure. The surgical approach it’s reserved to clinically unstable patients or those with evidence of peritonitis or bowel perforation. Stable patients, like those with an HPVG consequence of an endoscopic procedure, can be treated with non-operative management. In our case, an abdominal abscess was present but clinical serious signs of sepsis were absent. Probably in our patient the cause of HPVG was related to mucosa injury during the endoscopic procedure with consequent quick absorption of gas from the intestine into the mesenteric, then portal, venous system. Generally, this condition has been related to acute intestinal ischemia, as a consequence of a bacterial translocation through a wall defect.
4. Conclusion
Our experience confirm that hepatic portal venous gas can be related to endoscopic procedure; thus, it can be managed on the basis of patient’s general clinical conditions, and in selected cases it will disappear without therapeutic interventions with a good outcome.
Conflicts of interest
All authors disclose any financial and personal relationships with other people or organisations.
Sources of funding
No sources of funding was used for this research.
Ethical approval
This study is exempt from ethnical approval in our institution.
Consent
“Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request”.
Author contribution
G.T. Capolupo MD PhD. - G. Mascianà MD – F. Carannante MD: Patient care and management; image contribution.
M. Caricato MD PhD FACS: revision and final approval of the manuscript.
Registration of research studies
N/A.
Guarantor
M. Caricato MD, FACS.
References
- 1.Kinoshita H., Shinozaki M., Tanimura H., Umemoto Y., Sakaguchi S., Takifuji K. Clinical features and management of hepatic portal venous gas: four case reports and cumulative review of the literature. Arch. Surg. 2001;136:1410–1414. doi: 10.1001/archsurg.136.12.1410. [DOI] [PubMed] [Google Scholar]
- 2.Liebman P.R., Patten M.T., Manny J., Benfield J.R., Hechtman H.B. Hepatic—portal venous gas in adults: etiology, pathophysiology and clinical significance. Ann. Surg. 1978;187:281–287. doi: 10.1097/00000658-197803000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nelson A.L., Millington T.M., Sahani D., Chung R.T., Bauer C., Hertl M. Hepatic portal venous gas: the ABCs of management. Arch. Surg. 2009;144:575–581. doi: 10.1001/archsurg.2009.88. [DOI] [PubMed] [Google Scholar]
- 4.Wolfe J.N., Evans W.A. Gas in the portal veins of the liver in infants; a roentgenographic demonstration with postmortem anatomical correlation. Am. J. Roentgenol. Radium Ther. Nucl. Med. 1955;74:486–488. [PubMed] [Google Scholar]
- 5.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., for the SCARE Group The SCARE Statement: consensus- based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 6.Sebastià C., Quiroga S., Espin E. Portomesenteric vein gas: pathologic mechanisms, CT findings, and prognosis. Radiographics. 2000;20(5):1213–1224. doi: 10.1148/radiographics.20.5.g00se011213. [DOI] [PubMed] [Google Scholar]
- 7.Shah P.A., Cunningham S.C., Morgan T.A. Hepatic gas: widening Spectrum of causes detected at CT and US in the interventional era. Radiographics. 2011;31:1403–1413. doi: 10.1148/rg.315095108. [DOI] [PubMed] [Google Scholar]
- 8.Vollman J.H., Smith W.L., Tsang R.C. Necrotizing enterocolitis with recurrent hepatic portal venous gas. J. Pediatr. (Rio J) 1976;88:486–487. doi: 10.1016/s0022-3476(76)80275-2. [DOI] [PubMed] [Google Scholar]
- 9.Bach M.C., Anderson L.G., Martin T.A., Jr, McAfee R.E. Gas in the hepatic portal venous system. A diagnostic clue to an occult intra-abdominal abscess. Arch. Intern. Med. 1982;142:1725–1726. [PubMed] [Google Scholar]
- 10.Birnberg F.A., Gore R.M., Shragg B., Margulis A.R. Hepatic portal venous gas: a benign finding in a patient with ulcerative colitis. J. Clin. Gastroenterol. 1983;5:89–91. [PubMed] [Google Scholar]
- 11.Merritt C.R., Goldsmith J.P., Sharp M.J. Sonographic detection of portal venous gas in infants with necrotizing enterocolitis. AJR Am. J. Roentgenol. 1984;143:1059–1062. doi: 10.2214/ajr.143.5.1059. [DOI] [PubMed] [Google Scholar]
- 12.Benson M.D. Adult survival with intrahepatic portal venous gas secondary to acute gastric dilatation, with a review of portal venous gas. Clin. Radiol. 1985;36:441–443. doi: 10.1016/s0009-9260(85)80339-1. [DOI] [PubMed] [Google Scholar]
- 13.Huycke A., Moeller D.D. Hepatic portal venous gas after colonoscopy in granulomatous colitis. Am. J. Gastroenterol. 1985;80:637–638. [PubMed] [Google Scholar]
- 14.Radin D.R., Rosen R.S., Halls J.M. Acute gastric dilatation: a rare cause of portal venous gas. AJR Am. J. Roentgenol. 1987;(148):279–280. doi: 10.2214/ajr.148.2.279. [DOI] [PubMed] [Google Scholar]
- 15.Chezmar J.L., Nelson R.C., Bernardino M.E. Portal venous gas after hepatic transplantation: sonographic detection and clinical significance. AJR Am. J. Roentgenol. 1989;153(December (6)):1203–1205. doi: 10.2214/ajr.153.6.1203. [DOI] [PubMed] [Google Scholar]
- 16.Kirsch M., Bozdech J., Gardner D.A. Hepatic portal venous gas: an unusual presentation of Crohn’s disease. Am. J. Gastroenterol. 1990;85:1521–1523. [PubMed] [Google Scholar]
- 17.Lee C.S., Kuo Y.C., Peng S.M., Lin D.Y., Sheen I.S., Lin S.M., Chuah S.K., Chien R.N. Sonographic detection of hepatic portal venous gas associated with suppurative cholangitis. J. Clin. Ultrasound. 1993;21:331–334. doi: 10.1002/jcu.1870210507. [DOI] [PubMed] [Google Scholar]
- 18.Herman J.B., Levine M.S., Long W.B. Portal venous gas as a complication of ERCP and endoscopic sphincterotomy. Am. J. Gastroenterol. 1995;90:828–829. [PubMed] [Google Scholar]
- 19.Quirke T.E. Hepatic-portal venous gas associated with ileus. Am. Surg. 1995;61:1084–1086. [PubMed] [Google Scholar]
- 20.Mallens W.M., Schepers-Bok R., Nicolai J.J., Jacobs F.A., Heyerman H.G. Portal and systemic venous gas in a patient with cystic fibrosis: CT findings. AJR Am. J. Roentgenol. 1995;165:338–339. doi: 10.2214/ajr.165.2.7618551. [DOI] [PubMed] [Google Scholar]
- 21.Chen K.W., Shin J.S., Chi C.H., Cheng L. Seizure: a rare and transient cause of portal venous gas. Am. J. Gastroenterol. 1997;92:351–352. [PubMed] [Google Scholar]
- 22.Nguyen H.N., Purucker E., Riehl J., Matern S. Hepatic portal venous gas following emergency endoscopic sclerotherapy of gastric varices. Hepatogastroenterology. 1998;45:1767–1769. [PubMed] [Google Scholar]
- 23.Chang Y.S., Wang H.P., Huang G.T., Wu M.S., Lin J.T. Sonographic “gastric corona sign”: diagnosis of gastric pneumatosis caused by a penetrating gastric ulcer. J. Clin. Ultrasound. 1999;27:409–412. doi: 10.1002/(sici)1097-0096(199909)27:7<409::aid-jcu9>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 24.Nakao A., Iwagaki H., Isozaki H., Kanagawa T., Matsubara N., Takakura N., Tanaka N. Portal venous gas associated with splenic abscess secondary to colon cancer. Anticancer Res. 1999;19:5641–5644. [PubMed] [Google Scholar]
- 25.Saksena M., Harisinghani M.G., Wittenberg J., Mueller P.R. Case report. Hepatic portal venous gas: transient radiographic finding associated with colchicine toxicity. Br. J. Radiol. 2003;76:835–837. doi: 10.1259/bjr/13712140. [DOI] [PubMed] [Google Scholar]
- 26.Sellner F., Sobhian B., Baur M., Sellner S., Horvath B., Mostegel M. Intermittent hepatic portal vein gas complicating diverticulitis–a case report and literature review. Int. J. Colorectal Dis. 2007;22:1395–1399. doi: 10.1007/s00384-007-0346-3. [DOI] [PubMed] [Google Scholar]
- 27.Sen M., Akpinar A., Inan A., Sis_man M., Dener C., Akin K. Extensive hepatic-portal and mesenteric venous gas due to sigmoid diverticulitis. World J. Gastroenterol. 2009;15:879–881. doi: 10.3748/wjg.15.879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hussain A., Mahmood H., Ansari T., El-Hasani S. Pneumomediastinum, stomach wall and hepatic portal vein gas secondary to partial necrosis of the stomach wall. Singapore Med. J. 2009;50(May (5)):e166–169. [PubMed] [Google Scholar]
- 29.Siswojo A., Ihle B.U. Hepatic portal venous gas in a patient with intestinal necrosis. Emerg. Med. Australas. 2010;22:187–188. doi: 10.1111/j.1742-6723.2010.01274.x. [DOI] [PubMed] [Google Scholar]
- 30.Oehler E., Deniel M.C., Rouget B., Valour F. Mesenteric ischaemia with massive hepatic portal venous gas. BMJ Case Rep. 2013;2013 doi: 10.1136/bcr-2013-200076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cunningham G., Cameron G., De Cruz P. Hepatic portal venous gas in Crohn’s disease. BMJ Case Rep. 2014;2014(September) doi: 10.1136/bcr-2014-206244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Khalaf N., Mittal S. Hepatic portal venous gas: an ominous sign of mesenteric ischemia. Clin. Gastroenterol. Hepatol. 2014;12 doi: 10.1016/j.cgh.2014.01.011. xxix–xxx. [DOI] [PubMed] [Google Scholar]
- 33.Maezawa S., Fujita M., Sato T., Kushimoto S. Delayed intestinal stricture following non-resectional treatment for non-occlusive mesenteric ischemia associated with hepatic portal venous gas: a case report. BMC Surg. 2015;15:37. doi: 10.1186/s12893-015-0028-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sadatomo A., Koinuma K., Kanamaru R., Miyakura Y., Horie H., Lefor A.T., Yasuda Y. Hepatic portal venous gas after endoscopy in a patient with anastomotic obstruction. World J. Gastrointest. Surg. 2015;7:21–24. doi: 10.4240/wjgs.v7.i2.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Solakoglu T., Sari S.O., Koseoglu H., Basaran M., Akar M., Buyukasik S., Ersoy O. A case of hepatic portal venous gas after colonoscopy. Arab. J. Gastroenterol. 2016;17:140–142. doi: 10.1016/j.ajg.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 36.Sawano T., Nemoto T., Tsubokura M., Leppold C., Ozaki A., Kato S., Kanazawa Y. Asymptomatic hepatic portal venous gas with gastric emphysema as a chronic complication of gastrostomy tube placement: a case report. J. Med. Case Rep. 2016;10(234) doi: 10.1186/s13256-016-1037-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Castren E.E., Hakeem A.R., Mahmood N.S., Aryal K. Case of pneumatosis intestinalis and hepatic portal venous gas following a laparoscopic right hemicolectomy. BMJ Case Rep. 2016;2016(March) doi: 10.1136/bcr-2016-214431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moser A., Stauffer A., Wyss A., Schneider C., Essig M., Radke A. Conservative treatment of hepatic portal venous gas consecutive to a complicated diverticulitis: a case report and literature review. Int. J. Surg. Case Rep. 2016;23:186–189. doi: 10.1016/j.ijscr.2016.04.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yamadera M., Kajiwara Y., Shinto E., Hokari R., Shimazaki H., Yamamoto J., Hase K., Ueno H. Small intestinal Crohn’s disease with hepatic portal venous gas: a case report. Surg. Case Rep. 2016;2(1) December):66. doi: 10.1186/s40792-016-0193-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nevins E.J., Moori P., Ward C.S., Murphy K., Elmes C.E., Taylor J.V. A rare case of ischaemic pneumatosis intestinalis and hepatic portal venous gas in an elderly patient with good outcome following conservative management. Int. J. Surg. Case Rep. 2016;25:167–170. doi: 10.1016/j.ijscr.2016.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Okada S., Azuma T., Kawashita Y., Matsuo S., Eguchi S. Clinical evaluation of hepatic portal venous gas after abdominal surgery. Case Rep. Gastroenterol. 2016;10(1) May):99–107. doi: 10.1159/000444444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ginesu G.C., Barmina M., Cossu M.L., Feo C.F., Fancellu A., Addis F., Porcu A. Conservative approach to hepatic portal venous gas: a case report. Int. J. Surg. Case Rep. 2017;30:183–185. doi: 10.1016/j.ijscr.2016.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bangash H.K., McCombie S.P., Bangash O.K., Hayne D. Neobladder obstruction: a non-ischemic cause for hepatic PortalVenous gas: case report. Urol. Case Rep. 2017;(March (12)):31–33. doi: 10.1016/j.eucr.2017.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ghoz H.M., Sheikh S.M., Khandelwal K., Fiore J., James N., Weinstock J. A case of hepatic portal venous gas: hypothesis of a transient direct communication between a penetrating antral gastric ulcer and mesenteric varices. Case Rep. Gastrointest. Med. 2017 doi: 10.1155/2017/8185132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McNicholas D.P., Kelly M.E., Das J.P., Bowden D., Murphy J.M., Malone C. Disappearing portal venous gas in acute pancreatitis and small bowel ischemia. Radiol. Case Rep. 2017;12(Febuary (2)):269–272. doi: 10.1016/j.radcr.2017.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Li Z., Su Y., Wang X., Yan H., Sun M., Shu Z. Hepatic portal venous gas associated with colon cancer: a case report and literature review. Medicine(Baltimore) 2017;96(December (50)) doi: 10.1097/MD.0000000000009352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Niu D.G., Li C., Fang H.C. Hepatic portal venous gas associated with transcatheter cardiac defibrillator implantation: a case report. Int. J. Surg. Case Rep. 2018;44:57–61. doi: 10.1016/j.ijscr.2018.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]