Abstract
Objective
To assess the efficacy of Platelet Rich Fibrin (PRF) on the pain and healing of the extraction socket associated with Alveolar Osteitis (Dry Socket, AO) after removal of maxillary and mandibular molars.
Study design
100 adult patients with age group ranging from 18 to 40 years along with established dry socket after maxillary and mandibular molar extractions who have not received any treatment for the same were included in the study. PRF was placed in the maxillary and mandibular molar extraction sockets after adequate irrigation of the socket. All the patients evaluated for the various study variables which include pain, degree of inflammation, and healthy granulation tissue formation at 1st, 3rd, 7th, and 14th post operative day. Data were analyzed using Shapirowilk’s test, chi square test and/or student-t test, Friedman’s test, Wilcoxson’s signed rank test, and Bonferroni test, with the significance level set at P < 0.05.
Results
There was significant reduction in pain associated with AO at the 3rd and 7th postoperative day along with better wound healing by the end of 2nd week.
Conclusion
Use of PRF in this study illustrates the promising results in terms of reduced pain and better healing in the patients with Alveolar Osteitits.
Keywords: Dry socket, Alveolar osteitis, Tooth extraction, Pain, Platelet rich fibrin
1. Introduction
Dry socket or acute alveolar osteitis is a quite painful and debilitating condition for the patients who underwent extractions. The phrase dry socket was first formulated by Crawford1 in 1896; it has been previously described by various terminologies in the literature2, 3 and it can be defined by Blum as the presence of “postoperative pain in and around the site, which extraction increases in severity at any time between 1 and 3 days after the extraction, accompanied by a partially or totally disintegrated blood clot within the alveolar socket, with or without halitosis.4
It’s incidence after dental extractions is range from 1 to 30%.3 As a result, dry socket leads to stress for the dentists in managing the patient after extractions of teeth. The essential characteristic of sicca dolorosa is loss of the normal clot from the socket along with exposed bony walls and sensitive on gentle probing. Halitosis (Bad Breath) is a common complaint from the patient; fever is occasionally present.5, 6 It is generally exist within 1–4 days following dental extraction of teeth commonly mandibular molars. Commonly seen in the age group of 30 years or above; females are commonly affected than males.7, 8, 9
Alveolar osteitis have been associated with various etiologies.8, 10, 11, 12, 13, 14, 15 In recent past, a plethora of various researches had been done regarding the prevention and management of dry socket3, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25; nonetheless, none of them provided the effective treatment of the AO.
Contemporary review of literature depicts that a lot of research has been done on Platelet Rich Fibrin (PRF) and numerous cases have been reported regarding the use of PRF clot and PRF membranes. Majority of the research has been concentrated on the use of PRF in oral surgery for bone augmentation, sinus lifts, avulsion sockets etc and its applications in periodontology and endodontics.
Studies show that PRF can be used as filling material in extraction sockets. As a filling material in extraction sockets, PRF will act as a stable blood clot for neovascularization and accelerated tissue regeneration. This can be used to improve wound healing in immunocompromised and diabetic patients.26, 27, 28, 29, 30, 31
In lieu of the above mentioned versatility of PRF; the aim of the present study was to appraise the efficacy of PRF in the management of established alveolar osteitis consequently after the extraction of maxillary and mandibular molars (intra/trans alveolar).
2. Materials and method
A simple non-randomized observational, clinical, and prospective study was conducted with approbation of Department of Oral and Maxillofacial Surgery over a period of eighteen months from September 2014 to March 2016. All procedures performed in study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards and the regional Ethical Review Board of Institution approved the study. The procedure was explained to all the patients and informed consent was obtained from all participants included in the study. Those who were not ready and failed to report according to the set criteria were excluded from the surgery.
2.1. Inclusion and exclusion criteria
100 patients ranging from 18 to 40 years of age group, with established dry socket after maxillary and mandibular molar extraction, usually reporting on 3rd–5th post-operative day, who have not received any treatment for the same were included. Patients free from any systemic diseases and without any signs of active infection in extracted socket were included. Exclusion Criteria were pregnant and lactating women or patients on oral contraceptives, previous history of antibiotic and anti-inflammatory therapy for the treatment of dry socket, subjects with any underlying systemic disease or compromised immunity, patients who were unable to provide informed consent to the maxillofacial surgeon at the time of procedure. Patients who have already received treatment for dry socket e.g. local dressing with Zinc oxide eugenol pack, honey etc. were also excluded.
2.2. Study process
PRF was placed in the molar extraction sites with established localized osteitis, 100 sites total and in 100 consecutive patients was treated. The patients were managed with standard surgical techniques, and without any postoperative analgesic and antibiotic coverage. All patients were re-evaluated after 1st, 3rd, 7th, and 14th post-operative day. In order to control the bias, a single operator had treated all the patients.
2.3. Method of preparation of platelet rich fibrin
The platelet rich fibrin (PRF) was prepared according to the protocol of Choukroun J. et al.23 which is as follows: the Institutional Review Board has approved the study, according to PRF protocol blood samples were treated with a table centrifuge and collection kits provided by REMI, MUMBAI, INDIA (R-8C BL, Remi Labs, India). In short, samples were retreated from the patient without an anticoagulant in 10-ml glass-coated plastic tubes (Poly Medicure Ltd, New Dehli, India) and subjected to centrifugation at 3000 rpm for 12 min. A fibrin clot was formed in the middle part, acellular plasma present in the upper part of the tube, and the red corpuscles in the bottom part. The fibrin clot was abstracted comfortably from the basal part of the tube. The segregated PRF was placed into the dry socket, and stabilized with the help of figure of eight suture.
2.4. Clinical parameters
Various parameters were used to appraise the study subjects (Table 1, Table 2).
Table 1.
Pre-operative evaluation criteria.
| Pain | Degree of inflammation | Exposed bone | |
|---|---|---|---|
| Method | Visual analogue scale | Clinical assessment | Number of socket walls exposed |
| Score | 1–10 | 1- 1- Mild 2- 2- Moderate 3- Severe |
1- one wall 2- two walls 3-three walls 4-four walls |
Table 2.
Post-operative evaluation criteria.
| Pain | Number of packs | Criteria for healing | |
|---|---|---|---|
| Method | Visual analogue scale | Clinical assessment | Clinical assessment |
| Score | 1–10 | Actual no. of patient visits. | 4-Four walls 3-Three walls 2-Two walls 1-One wall 0-Zero wall |
2.4.1. Pain
It was assessed using 10 point Visual Analogue Scale, with a score of “0” equals “no pain” and “10” equals “very severe pain” (Fig. 1).
Fig. 1.
Visual Analogue Scale.
Pain was evaluated pre-operatively and post-operative 1st, 3rd and 7th day.
Moreover, all the patients were asked not to take any pain killers i.e. NSAID’s for the post-operative pain in order to assess the anti-nociceptive property of PRF. Furthermore, the time required achieve clinical healing were also noted.
2.4.2. Degree of inflammation
It was evaluated using gingival severity index32 for inflammation from 0 to 3 which comprised of 0- Normal gingiva; 1- mild inflammation- slight change in color, slight oedema. No bleeding on probing; 2- moderate inflammation- redness, oedema and glazing. Bleeding on probing; 3- severe inflammation- marked redness and oedema, ulceration and tendency to spontaneous bleeding on 1st, 3rd, and 7th day post-operatively. Inflammation was assessed clinically by gentle probing of the extraction socket to ensure presence or absence of gingival bleeding.
2.4.3. Granulation tissue formation
Granulation tissue formation at the molar extraction site treated with PRF was assessed clinically. This is evident clinically by the coverage of the exposed bone at the site of alveolar osteitis by soft granulation tissue. The granulation tissue was divided into healthy (pink in colour and does not bleed on probing) and unhealthy granulation tissue (dark red in colour and often bleeds on probing). Granulation tissue formation was evaluated on 1st, 3rd, 7th, and 14th postoperative day.
The results of the clinical examination were recorded on a specific form. The data was subjected to statistical analysis using Shapirowilk’s test, chi square test and/or student-t test, Friedman’s test, Wilcoxson’s signed rank test, and Bonferroni test, and SPSS version 20 (Chicago, Illinois, USA) software as per data requirements. The level of significance was concluded at P < 0.05.
3. Results
Out of hundred patients of dry socket, twenty one were males and seventy nine were females with a ratio of 4:1. Dry socket was seen more commonly occurring in females. Patients less than 25 years of age were more commonly affected. Incidence of dry socket was more in mandible than the maxilla (P = 0.045). All patients measured severe pain on day 1 on visual analogue scale but, there was significant fall in the pain score on the 3rd and 7th post-operative day (p < 0.05). The degree of inflammation which was more on the pre-operative and 1st post-operative day was also significantly decreased by the 7th day (p < 0.05). Denuded bony walls, which were visible before the placement of PRF in the extraction sockets and in the immediate post-operative day, were gradually replaced by granulation tissue. By the end of two weeks, no bony walls were exposed in any of the extraction sites (p < 0.05) (Tables 3–6 ) (Figs. 2–5 ).
Table 3.
Demographic details.
| Age | N | Percentage |
|---|---|---|
| <25 years | 41 | 40.6 |
| 26–35 years | 38 | 37.6 |
| >36 years | 21 | 20.8 |
| Total | 100 | 100.0 |
| Male | 21 | 20.8 |
| Female | 79 | 78.2 |
| Total | 100 | 100.0 |
| Maxilla | 26 | 25.7 |
| Mandible | 74 | 73.3 |
| Total | 100 | 100.0 |
Table 4.
Mean, SD and mean rank of participants VAS scores.
| N | Mean | Std. Deviation | Mean rank | Chi square | p value | |
|---|---|---|---|---|---|---|
| Pre op | 100 | 8.51 | .55 | 4.00 | 302.41 | 0.000a |
| Post op 1 day | 100 | 4.57 | .62 | 2.99 | ||
| Post op 3 day | 100 | 2.38 | .48 | 2.01 | ||
| Post op 7 day | 100 | .00 | .00 | 1.00 |
| Pair wise comparisons | ||
|---|---|---|
| Comparator | Compared with | p value |
| Pre operative | Post op 1 day | 0.000 |
| Post op 3 day | 0.000 | |
| Post op 7 day | 0.000 | |
| Post op 1 day | Post op 3 day | 0.000 |
| Post op 7 day | 0.000 | |
| Post op 3 day | Post op 7 day | 0.000 |
As Friedman’s test showed statistical significant difference between different time intervals, post hoc pairwise comparisons were done by Wilcoxsons signed rank test with Bonferroni corrections. Thus p < 0.0125 was considered as significant for post hoc test.
Friedman’s test P < 0.05.
Table 5.
Mean, SD and mean rank of participant’s degree of inflammation.
| N | Mean | Std. Deviation | Mean rank | Chi square | p value | |
|---|---|---|---|---|---|---|
| Pre op | 100 | 2.64 | .48 | 3.81 | 290.85 | 0.000* |
| Post op 1 day | 100 | 2.02 | .14 | 3.18 | ||
| Post op 3 day | 100 | 1.03 | .17 | 2.02 | ||
| Post op 7 day | 100 | .00 | .00 | 1.00 |
| Pair wise comparisons | ||
|---|---|---|
| Comparator | Compared with | p value |
| Pre operative | Post op 1 day | 0.000 |
| Post op 3 day | 0.000 | |
| Post op 7 day | 0.000 | |
| Post op 1 day | Post op 3 day | 0.000 |
| Post op 7 day | 0.000 | |
| Post op 3 day | Post op 7 day | 0.000 |
As Friedman’s test showed statistical significant difference between different time intervals, post hoc pairwise comparisons were done by Wilcoxsons signed rank test with Bonferroni corrections. Thus p < 0.0125 was considered as significant for post hoc test.
*Friedman’s test P < 0.05.
Fig. 2.
Shapirowilk’s test revealed non normal distribution of visual analogue scores.
Fig. 3.
VAS Mean scores of participants over different time intervals.
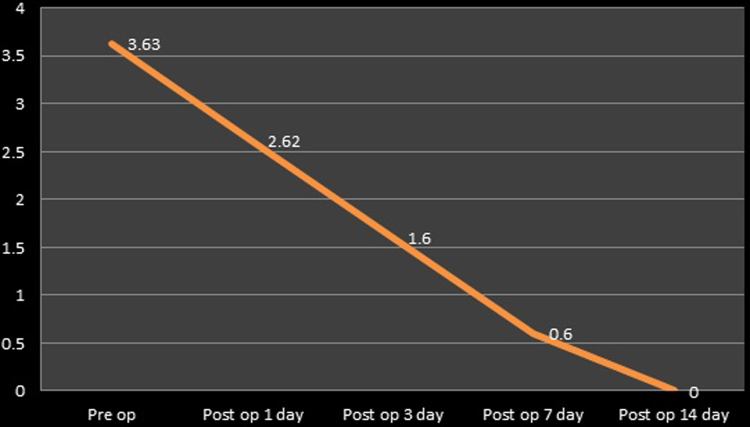
Fig. 4.
Mean scores of degree of inflammation of participants over different time intervals.
Fig. 5.
Mean bony walls exposed in participants over different time intervals.
4. Discussion
Dry socket is a frequent drawback of exodontia and results in pertubance of the patient. It is a post-operative sequelae often associated with removal of mandibular third molars.3 Several methods have been advocated to reduce the incidence of dry socket. Alveolar osteitis is known to have a multifactorial origin8 where bacteria play an important role. The part of Actinomyces viscosus and Treponema denticola in dry socket has been propagated by various studies.11, 12 Because of which use of antibiotics in the form of mouth wash and intra-socket medication gained popularity.3 Various pharmacological agents were proposed and designed for interception of dry socket for instance chlorhexidine in forms of gel and mouthwash.16
Topical anaesthetics and obtundents or combinations of all three,3 have also been used. Intra-socket medications like zincoxide and eugenol impregnated cotton pellets, bismuth subnitrate, iodoform paste and alvogyl dentalone (BIPP) on ribbon gauze are other alternatives used for treatment of dry socket.
Certain studies implicated the use of topical parahydroxy benzoic acid and tranexamic acid18 and the use of polymer polylactic acid19 in the prevention of dry socket. But these treatment options have not shown satisfactory results. Antimicrobial photodynamic therapy was employed in the management of dry socket but further studies are required.20
Choukroun et al.22 in France advocated the use of PRF which is a second generation platelet concentrate. PRF is a stringently autologous fibrin matrix. Dohan et al.26 suggested that PRF addition can correct destructive reactions in the natural process of healing of wound tissues. Thus this determines that PRF immune regulatory mechanism over the inflammation.
Although PRF has been used for several procedures such as ridge augmentation, in sinus lift procedures, for filling furcation defect, for avulsion sockets etc, however no studies were done on the use of PRF in managing dry socket and its associated pain and inflammation. The present study is an attempt which harnessed the healing potential of PRF and its immune regulatory capacity in the management of dry socket after extraction of molars.
Within the clot in the socket, the inflammatory response takes place. The epithelial cells, which have osteogenic potential, invade the clot and eventually lay down bone. In dry socket, where clot has been disintegrated, the process of wound healing is delayed. The platelet-rich fibrin (PRF) is a high concentration of autologous platelets.
Healing and immunity is benefit by the PRF which is an immune and platelet concentrate aggregate on a single fibrin membrane that comprise of all the ingredients of blood. The development of microvascularization and cell migration into a wound can be compliment by PRF which is an indigenous fibrin-based biomaterial. Moreover, this grid contains leukocytes and assists their movement. In case of infected wounds its acceptance appears to be of eminent concern.
In a clinical example depicted by Choukroun et al.23 in which he used the PRF as a filling material in extraction socket; clinically he confirms that neovascularisation and epithelial coverage of the extraction socket can be achieved with the use of PRF. Lastly, accelerated healing of the wound is contemplated without pain, dryness, or purulent complexities in the infectious and inflammatory wounds. This suggests that use of the PRF as a grafting material for the treatment of dry socket may improve the clinical healing. This perhaps due to copious amount of growth factors such as platelet-derived growth factor (PDGF), transforming growth factor beta (TGF-β), epidermal growth factor (EGF), insulin-like growth factor (IGF), and hepatocyte growth factor (HGF) liberated from PRF mesh; these factors plays a essential role in reconstitution of forfeited tissue, covering of the wound, and re-establishing the vascular integrity. Contemporary literature demonstrated that PRF membrane has a very eloquent slow continuous release of essential growth factors for at least seven and up to 28 days, which means during the period of remodelling the membrane activates its background for a significant period. Furthermore, these molecules could accelerate a process that occurs by itself (it does not create a new process). Thus it provides a great potential during wound healing in dry sockets.
In the present study females were seen more commonly affected (78.2%). This is in accordance to other studies by Xu J.L. et al.8 and Eshghpour M. et al.30 and the reason cited behind this high percentage is due to the use of oral contraceptives and menstruation.
The present study implies that the ubiquity of AO more in the mandible than in maxilla; perhaps due to more deliverance of direct tissue activators secondary to bone marrow inflammation following more difficult and hence, more traumatic extractions.28
Pain is inevitable for patients with dry socket which hampers the regular activities of life. The present study showed how severe pain was measured in the VAS scale pre-operatively, but after the application of PRF, there was marked reduction in pain. Kumar Y et al.29 reported of reduction in pain level by use of PRF. PRF act as an immune regulator and may decrease the deleterious effects of inflammation as described by the Dohan et al.27
It implies that the fibrin matrix results in angiogenesis and contributes towards natural immunity thus reducing inflammatory process. Therefore it provides natural resurfacing of the dry socket wound, which ultimately results in the covering of the exposed nerve endings in the socket as a result there was a significant decrease in the amount of pain associated with the condition.
A highly significant reduction in inflammatory response was also clinically observed in the present study. In a study by Eshghpour M. et al.31 also reported of reduction of inflammation with use of PRF. Studies have shown PRF can stimulate defence mechanism to prevent infections and has immune regulatory action.27
Denuded bony walls characteristically seen in dry sockets showed better healing and there was coverage of bony walls due to granulation tissue formation on 2nd week post-operatively, after being treated with PRF (Table 6). This is attributing to the PRF inherent property of releasing growth factors in a controlled manner. The encouragement of the mitogenic response in the periosteum for bone repair during normal wound healing is due to the growth factors released after activation from the platelets entangled within fibrin matrix.23
Table 6.
Mean, SD and mean rank of participants bony walls exposed.
| N | Mean | Std. Deviation | Mean rank | Chi square | p value | |
|---|---|---|---|---|---|---|
| Pre op | 100 | 3.63 | .48 | 4.99 | 394.69 | 0.000* |
| Post op 1 day | 100 | 2.62 | .48 | 4.01 | ||
| Post op 3 day | 100 | 1.60 | .49 | 3.00 | ||
| Post op 7 day | 100 | .60 | .49 | 1.80 | ||
| Post op 14 day | 100 | .00 | .00 | 1.20 |
| Pair wise comparisons | ||
|---|---|---|
| Comparator | Compared with | p value |
| Pre operative | Post op 1 day | 0.000 |
| Post op 3 day | 0.000 | |
| Post op 7 day | 0.000 | |
| Post op 14 day | 0.000 | |
| Post op 1 day | Post op 3 day | 0.000 |
| Post op 7 day | 0.000 | |
| Post op 14 day | 0.000 | |
| Post op 3 day | Post op 7 day | 0.000 |
| Post op 14 day | 0.000 | |
| Post op 7 day | Post op 14 day | 0.000 |
*Friedman’s test P < 0.05.
As Friedman’s test showed statistical significant difference between different time intervals, post hoc pairwise comparisons were done by Wilcoxsons signed rank test with Bonferroni corrections. Thus p < 0.01 was considered as significant for post hoc test.
5. Conclusion
The occurrence of dry socket in an everyday oral surgery or dental practice is inescapable. The risk factors associated with AO are discernibly analyzed. Though various methods of prevention of dry socket have been employed, the management of established alveolar osteitis is a limited and difficult subject. With Platelet Rich Fibrin gaining grounds as a potent wound healer, the present study focussed on managing the bothersome pain and delayed healing associated with dry socket with this autologous material. Significant decrease in pain level was noted by use of PRF and better wound healing was promoted.
Conflict of interest
The authors have none to declare.
Research involving human participants and/or animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Source of funding
None.
Acknowledgement
None.
Contributor Information
Sanjay Rastogi, Email: docos79@gmail.com.
Rupshikha Choudhury, Email: rupmds12@gmail.com.
Ashish Kumar, Email: drashish_kumar@hotmail.com.
Shiva Manjunath, Email: drmanju75@rediffmail.com.
Aanchal Sood, Email: dr.periodontics08@gmail.com.
Himanshu Upadhyay, Email: siddhivinayaketah@gmail.com.
References
- 1.Crawford J.Y. Dry socket. Dent Cosmos. 1896;38:929–993. [Google Scholar]
- 2.Metin M., Tek M., Sener I. Comparison of two chlorhexidine rinse protocols on the incidence of alveolar osteitis following surgical removal of impacted third molars. J Contemp Dent Pract. 2006;7:79–86. [PubMed] [Google Scholar]
- 3.Bloomer C.R. Alveolar osteitis prevention by immediate placement of medicated packing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:282–284. doi: 10.1067/moe.2000.108919. [DOI] [PubMed] [Google Scholar]
- 4.Blum I.R. Contemporary views on dry socket (alveolar osteitis): a clinical appraisal of standardization, aetiopathogenesis and management: a critical review. Int J Oral Maxillofac Surg. 2002;31:309–317. doi: 10.1054/ijom.2002.0263. [DOI] [PubMed] [Google Scholar]
- 5.Oginno F.O. Dry socket: a prospective study of prevalent risk factors in a Nigerian population. J Oral Maxillofac Surg. 2008;66:2290–2295. doi: 10.1016/j.joms.2008.01.063. [DOI] [PubMed] [Google Scholar]
- 6.Quinley J.F. Dry socket after mandibular odontectomy and use of soluble tetracycline hydrochloride. Oral Surg Oral Med Oral Pathol. 1960;13:38–42. doi: 10.1016/0030-4220(60)90390-x. [DOI] [PubMed] [Google Scholar]
- 7.Birn H. Aetiology and pathogenesis of fibrinolytic alveolitis (Dry socket) Int J Oral Surg. 1973;2:251–263. [Google Scholar]
- 8.Tarakji B., Saleh L.A., Umair A., Azzeghaiby S.N., Hanouneh S. Systemic review of dry socket: aetiology, treatment and prevention. J Clin Diagn Res. 2015;9:ZE10–3. doi: 10.7860/JCDR/2015/12422.5840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fernandes G.J., Hatton M.N. Prevention of alveolar osteitis. A case report and review of literature. N Y State Dent J. 2016;82:21–25. [PubMed] [Google Scholar]
- 10.Wates E., Ria B. The prevention and management of dry socket. Do antibiotics have a role to play? Prim Dent J. 2015;4:42–43. doi: 10.1308/205016815815944696. [DOI] [PubMed] [Google Scholar]
- 11.Hedstrom L., Sjogren P. Effect estimates and quality of randomized controlled trials about prevention of alveolar osteitis following tooth extraction. Oral Surg Oral Med Oral Pathol Oral Rad Endod. 2007;103:8–15. doi: 10.1016/j.tripleo.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 12.Nitzan D.W. On the genesis of dry socket. J Oral Maxillofac Surg. 1983;41:706–710. doi: 10.1016/0278-2391(83)90185-4. [DOI] [PubMed] [Google Scholar]
- 13.Freudenthal N., Stemudd M., Jansson L., Wannfors K. A double blind-randomized study evaluating the effect of intra-alveolar chlorhexidine gel on alveolar osteitis after removal of third molars. J Oral Maxillofac Surg. 2015;73:600–605. doi: 10.1016/j.joms.2014.08.035. [DOI] [PubMed] [Google Scholar]
- 14.Rakhshan V. Common risk factors for postoperative pain following the extraction of wisdom teeth. J Korean Assoc Oral Maxillofac Surg. 2015;41:59–65. doi: 10.5125/jkaoms.2015.41.2.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xu J.L., Sun L., Liu C. Effect of oral contraceptives use on the incidence of dry socket in females following impacted third molar extraction: a meta- analysis. Int J Oral Maxillofac Surg. 2015;44:1160–1165. doi: 10.1016/j.ijom.2015.05.017. [DOI] [PubMed] [Google Scholar]
- 16.Jesudasan J.S., Wahab P.U., Sekhar M.R. Effectiveness of 0.2% chlorhexidine gel and a eugenol based paste on postoperative alveolar osteitis in patients having third molars extracted: a randomised controlled clinical trial. Br J Oral Maxillofac Surg. 2015;53:826–830. doi: 10.1016/j.bjoms.2015.06.022. [DOI] [PubMed] [Google Scholar]
- 17.Khiyavi R., Barghi V., Yazdani J. Effect of Biotene mouth wash on prevention of alveolar Osteitis after extraction of permanent Mandibular first molar Teeth. Elixir Hum Physiol. 2012;47:8672–8674. [Google Scholar]
- 18.Anand K.P., Patro S., Mohapatra A., Mishra S. The efficacy of Tranexamic acid in the reduction of incidence of dry socket: an Institutional double blind study. J Clin Diagn Res. 2015;9:ZC25–8. doi: 10.7860/JCDR/2015/11267.6464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hooley J.R., Gordon D.P. The effect of polylactic acid granules on the incidence of alveolar osteitis after third molar surgery. A prospective randomized study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:279–283. doi: 10.1016/s1079-2104(05)80383-x. [DOI] [PubMed] [Google Scholar]
- 20.Goran J., Nikola B., Nebojsa K., Milos T., Simona S. Assessment of the effectiveness of low level laser in the treatment of alveolar osteitis. Vojnosanitetski pregled. 2011;68:506–510. doi: 10.2298/vsp1106506j. [DOI] [PubMed] [Google Scholar]
- 21.Goldsmith S., De Silva R., Tong D., Love R. Influence of a pedicle flap design on acute postoperative sequelae after lower third molar removal. Int J Oral Maxillofac Surg. 2012;41:371–375. doi: 10.1016/j.ijom.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 22.Ross R., Glomset J., Kariya B., Harker L. A platelet-dependent serum factor that stimulates the proliferation of arterial smooth muscle cells in vitro. Proc Natl Acad Sci U S A. 1974;71:1207–1210. doi: 10.1073/pnas.71.4.1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Choukroun J., Diss A., Simonpieri A. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part V. Histologic evaluations of PRF effects on bone allograft maturation in sinus lift. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:299–303. doi: 10.1016/j.tripleo.2005.07.012. [DOI] [PubMed] [Google Scholar]
- 24.Haraji A., Lassemi E., Motamedi M., Alavi M., Adibnejad S. Effect of plasma rich in growth factors on alveolar osteitis. Natl J Maxillofac Surg. 2012;3:38–41. doi: 10.4103/0975-5950.102150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pal U.S., Singh B.P., Verma V. Comparative evaluation of zinc oxide eugenol versus gelatin sponge soaked in plasma rich in growth factor in the treatment of dry socket: an initial study. Contemp Clin Dent. 2013;4:37–41. doi: 10.4103/0976-237X.111592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Corso M.D., Toffler M., David M., Ehrenfest D. Use of autologous leukocyte and platelet rich fibrin (L-PRF) membrane in post avulsion sites: an overview of Choukroun’s PRF. J Implant Adv Clin Dent. 2010;1:27–35. [Google Scholar]
- 27.Dohan D.M., Choukroun J., Diss A. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part III. leucocyte activation: a new feature for platelet concentrates? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e51–e55. doi: 10.1016/j.tripleo.2005.07.010. [DOI] [PubMed] [Google Scholar]
- 28.Bortoluzzi M.C., Manfro R., De Déa B.E., Dutra T.C. Incidence of dry socket, alveolar infection, and postoperative pain following the extraction of erupted teeth. J Contemp Dent Pract. 2010;11:E033–40. [PubMed] [Google Scholar]
- 29.Kumar Y., Mohanty S., Verma M. Platelet-rich fibrin: the benefits. Br J Oral Maxillofac Surg. 2016;54:57–61. doi: 10.1016/j.bjoms.2015.10.015. [DOI] [PubMed] [Google Scholar]
- 30.Eshghpour M., Rezaei N.M., Nejat A. Effect of menstrual cycle on frequency of alveolar osteitis in women undergoing surgical removal of mandibular third molar: a single-blind randomized clinical trial. J Oral Maxillofac Surg. 2013;71:1484–1489. doi: 10.1016/j.joms.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 31.Eshghpour M., Dastmalchi P., Nekooei A.H., Nejat A. Effect of platelet-rich fibrin on frequency of alveolar osteitis following mandibular third molar surgery: a double-blinded randomized clinical trial. J Oral Maxillofac Surg. 2014;72:1463–1467. doi: 10.1016/j.joms.2014.03.029. [DOI] [PubMed] [Google Scholar]
- 32.Loe H. The gingival index, the plaque index and the retention index systems. J Periodontol. 1967;38(Suppl. 6):610–616. doi: 10.1902/jop.1967.38.6.610. [DOI] [PubMed] [Google Scholar]