Abstract
Objective
We evaluated the sensitivity and specificity of bedside ultrasound (US) for determining the success of reduction of displaced distal radius fractures. In addition, we determined the ability of US to diagnose causes of unsuccessful reduction.
Methods
In a prospective, double-blind fashion, patients over 18 of age whose acute distal radius fracture was to be reduced were approached for inclusion. The closed reductions were performed by orthopedics residents. Post-reduction, the fracture was checked by an Emergency Medicine (EM) resident by US. Ultrasound images were evaluated by an EM attending physician blinded to X-ray findings and post-reduction X-ray images were evaluated by an orthopedic surgeon blinded to the US findings.
Results
Sixty patients agreed to participate in the study. Of these, reduction was deemed successful by X-ray in 40 (66.7%). Of these 40, 39 (97.5%) were found to be successful reductions by US. In the 20 of 60 (33.3%) patients with unsuccessful reduction by X-ray, 19 (95%) were considered unsuccessful reductions by US. In evaluating the success of distal radius fracture reduction, compared to X-rays, US was 97.5% (95% CI 86.8 to 99.9) sensitive and 95% (95% CI 75.1 to 99.9) specific; its positive predictive value was 97.5% (95% CI 85.2 to 99.6) and negative predictive value 95% (95% CI 73.2 to 99.2).
Conclusions
Ultrasonography is highly sensitive and specific in determining the success of distal radius fracture reduction.
Keywords: Ultrasonography, Fracture, Distal radius, Reduction
1. Introduction
Wrist injuries comprise almost 2.5% of emergency department (ED) visits. Distal radius fractures are the most common fractures of the wrist.1 In daily practice, closed reduction and immobilization is the preferred method of managing stable distal radius fractures. Adequate anatomic reduction, determined usually by 2-view X-rays, plays a key role inlong-term treatment success. In the event that reduction is seen to be inadequate by imaging studies, reduction is attempted again on the patient, often after ensuring more adequate analgesia.2 Ultrasound (US) can be used in the management of the patients with distal radius fractures due to its easy use at the bedside and instantaneous provision of images during the reduction process.3, 4, 5 Ultrasonography implemented reduction procedure may help physicians to evaluate reduction success just before the post-reduction X-ray. Also reductions made with help of US may need less time and have high procedure precision. However, still limited number of studies has evaluated the efficacy of US alone in determining the success of fracture reduction. In this study, we aimed to determine the accuracy of bedside US in the detection of success in the reduction of distal radius fractures.6, 7, 8 We also aimed to determine how effective US was in detecting the causes of unsuccessful reduction of distal radius fractures.
2. Methods
2.1. Study design & patient selection
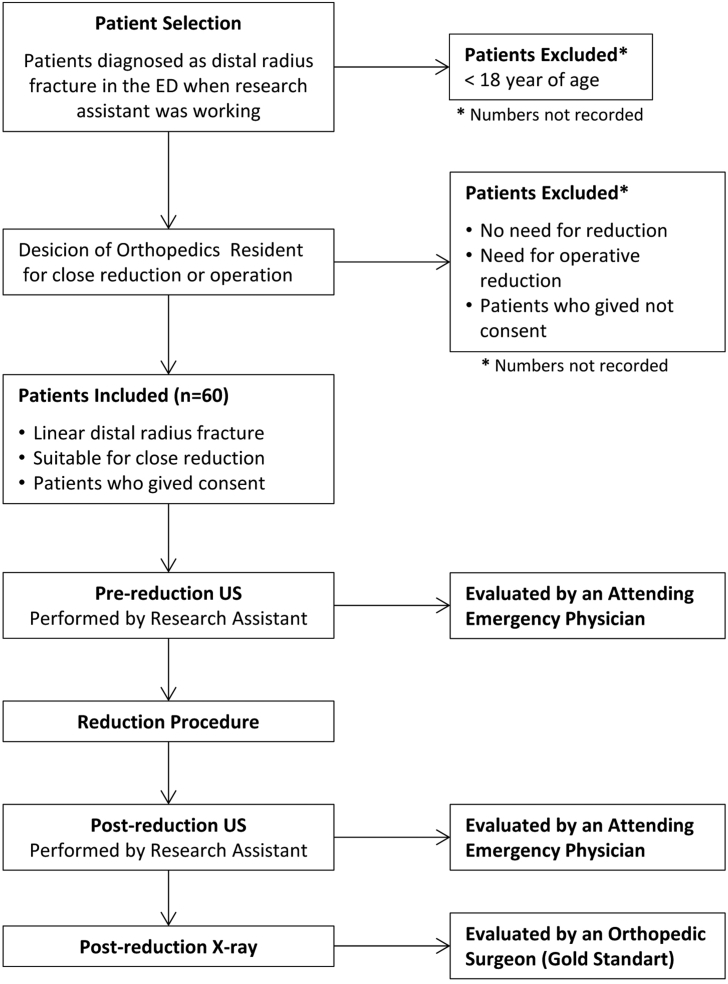
The study protocol was approved by our university's Clinical Research Ethics Committee. Consecutive patients over age 18 with a linear distal radius fracture requiring closed reduction who were evaluated in our university hospital ED between April and September 2013 were asked to participate in this prospective double-blind, cross-sectional, diagnostic accuracy study. Those who were taken to the operation room for operative reduction and who have a linear fracture which doesn't need a reduction were excluded from the study. Selection was made according to the desicion of the research assistant- emergency medicine (EM) resident (convenience sampling). Patient selection and study design details are shown in Fig. 1.
Fig. 1.
Patient flow diagram.
2.2. Research team
Research Asistant (Sonographer): The research team comprised an EM resident trained in extremity US with 2 years experience. He practised with normal and fractured patients under the supervision of the EM Attending Physician at least 25 patients.
Orthopedics Resident: Orthopedics residents who is on duty in the ED, has decided for close reduction and also performed fracture reduction and applied a plaster cast. These residents has at least one year experience.
Orthopedic Surgeon: Senior faculty member who evaluated post-reduction X-rays has not seen the patient nor US images. This surgeon was an expert on hand surgery, and his evaluation for X-ray images of distal radius fractures is accepted as gold standart.
EM Attending Physician: The EM physician is a senior EM faculty and has expertise on ultrasonography and she is an instructor more than 5 years evaluated the US images.
2.3. Ultrasound techniques
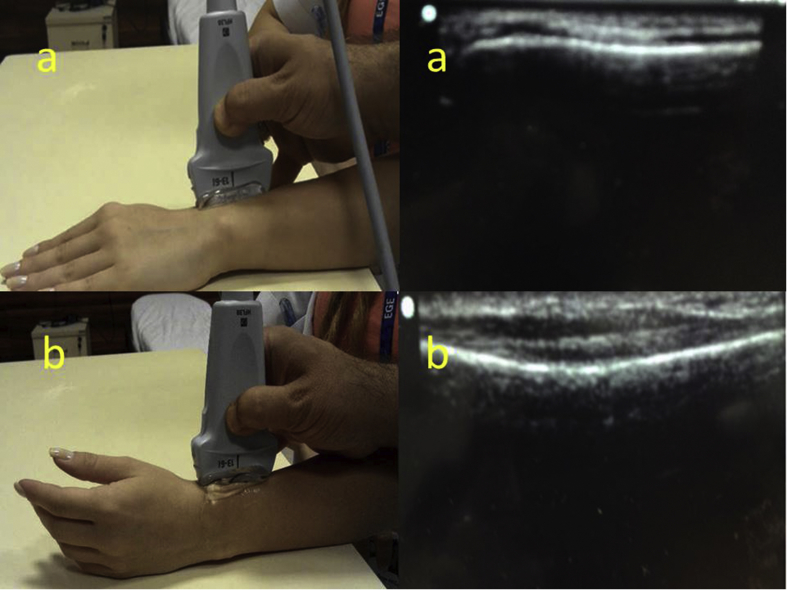
Probe Location: Pre- and post reduction US images are obtained from the dorsal and lateral side of distal radius, US performed with a 6–13 MHz linear transducer on a SonoSite MicroMaxx (SonoSite Inc., USA) machine. The transduser was located in vertical plane as dorsaly and also lateraly, index of the probe was indicating distal part of radius (see examples in Fig. 2). No side effect was observed during performance of ultrasonography.
Fig. 2.
Performing of the ultrasonography from the dorsal (a) and lateral (b) of the distal radius and corresponding US images.
Evaluation of Angulation of Dorsal or Volar Fractures: Disruption of the cortical alignment on the US images were accepted as a fracture. According to the location of the fragment the angulation was defined as dorsale or volar. Unfortunately the degree of angulation was not calculated because of bone cortex was not a linear line in US images.
Evaluation of Foreshortening of the Radius: Images obtained in vertical plane from the dorsal of the distal radius and index of the probe was indicating distal radius. Overlapping of proximal and distal parts of fracture, and also not coming together end-to-end of the bone cortices was accepted as a radial foreshortening. Images of the fracture line were obtained only from dorsal and lateral sides, therefore it was not possible find an index point to measure the radial shortening and it is stated only as positive and negative manner.
Evaluation of Multiple Fragments in the Dorsum of the Distal Fragment: Fracture line evaluated from dorsal side, if multiple bone fragments are imaged it is accepted as presence of multiple fragments.
2.4. Procedure
For all the patients who gave informed consent for including to the study appropriate monitorization also sedation and anestesia was applied before the procedure. After 2-view X-rays showed a distal radius fracture, a pre-reduction US (dorsovertical ve dorsolateral images) was performed by the sonographer.
The US result was not reported to the orthopedics residents. Under procedural sedation and analgesia, closed reduction of the distal radius fracture was performed by orthopedics residents after he/she viewed the X-ray. Immediately afterwards, again without reporting its result to the orthopedics residents, post-reduction US (dorsovertical and dorsolateral) images were obtained. After the plaster cast, post-reduction X-rays were taken and reviewed by the same orthopedics residents. If he/she deemed the reduction to be unsatisfactory, the cast was removed and reduction and postreduction AP and lateral X-ray were performed again.
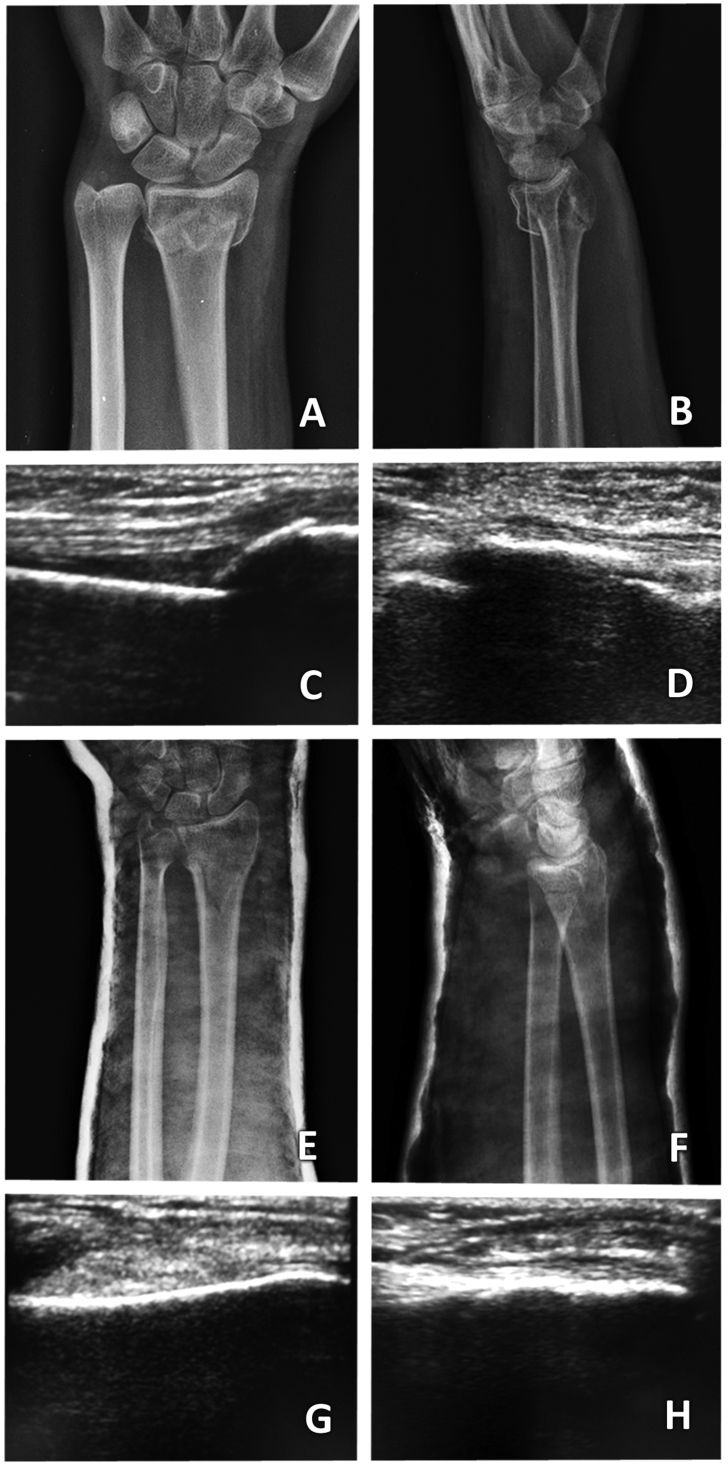
Ultrasound images were later evaluated by the EM Attending Physician who had not seen the patient nor X-ray images. Reduction was deemed successful if the bone cortices of the fracture surfaces detected on pre-reduction US came together end-to-end on the post-reduction US images (Fig. 3). The fracture reduction was deemed unsuccessful if any of the following were seen on the US images: no linear integrity between the bone cortices, a space or overlap between the two cortices, or displacement and angulation between the cortices (Fig. 4). In addition, the EM Attending Physician evaluated the US images for angulation, foreshortening of the radius, and for the presence of comminuted fracture (Fig. 5).
Fig. 3.
Successful fracture reduction as seen on pre- and post-reduction X-ray and US images. A) Pre-reduction AP X-ray, B) Pre-reduction lateral X-ray, C) Pre-reduction fracture line by US (dorsal image), D) Pre-reduction fracture line by US (lateral image), E) Post-reduction AP X-ray, F) Post-reduction lateral X-ray, G) Post-reduction fracture line by US (dorsal image), H) Post-reduction fracture line by US (lateral image).
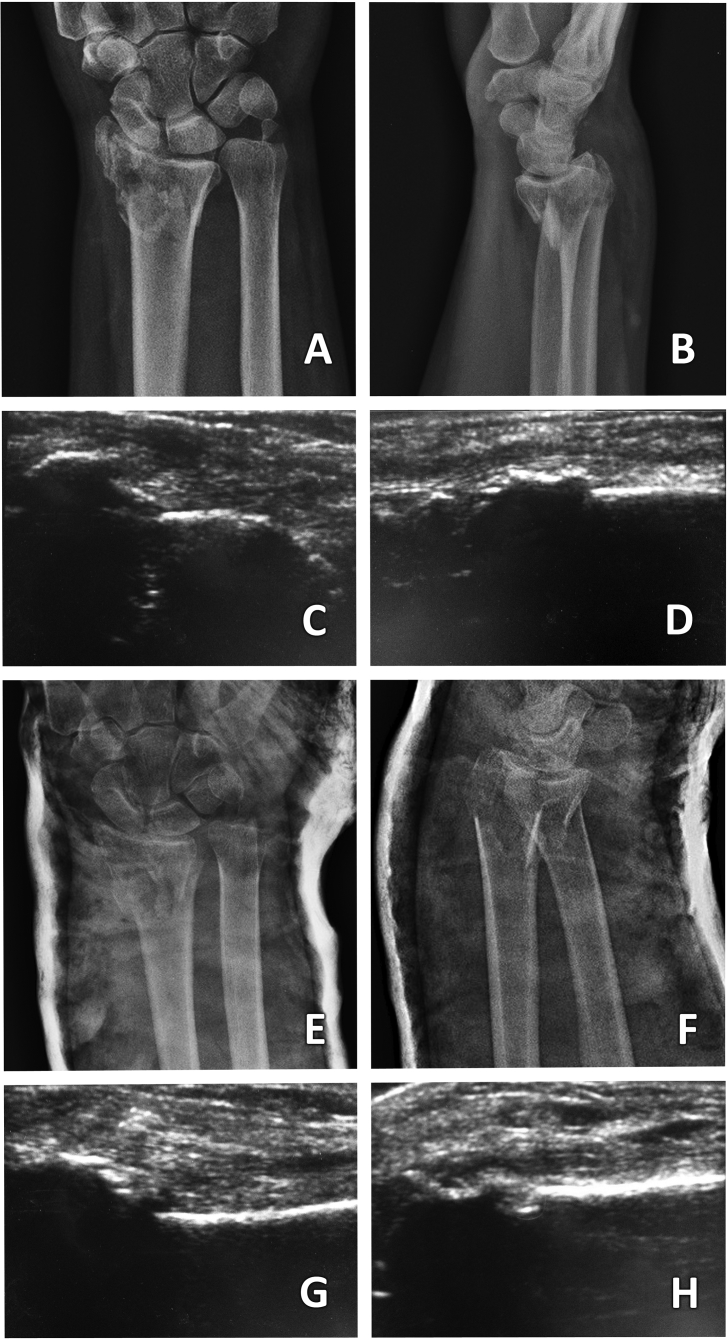
Fig. 4.
Pre-and post-reduction X-ray and US images of a failed fracture reduction. A)Pre-reduction AP X-ray, B) Pre-reduction lateral X-ray, C) Pre-reduction fracture line by US (dorsal image), D) Pre-reduction fracture line by US (lateral image), E) Post-reduction AP X-ray, F) Post-reduction lateral X-ray,G) Post-reduction fracture line by US (dorsal image), H) Post-reduction fracture line by US (lateral image).
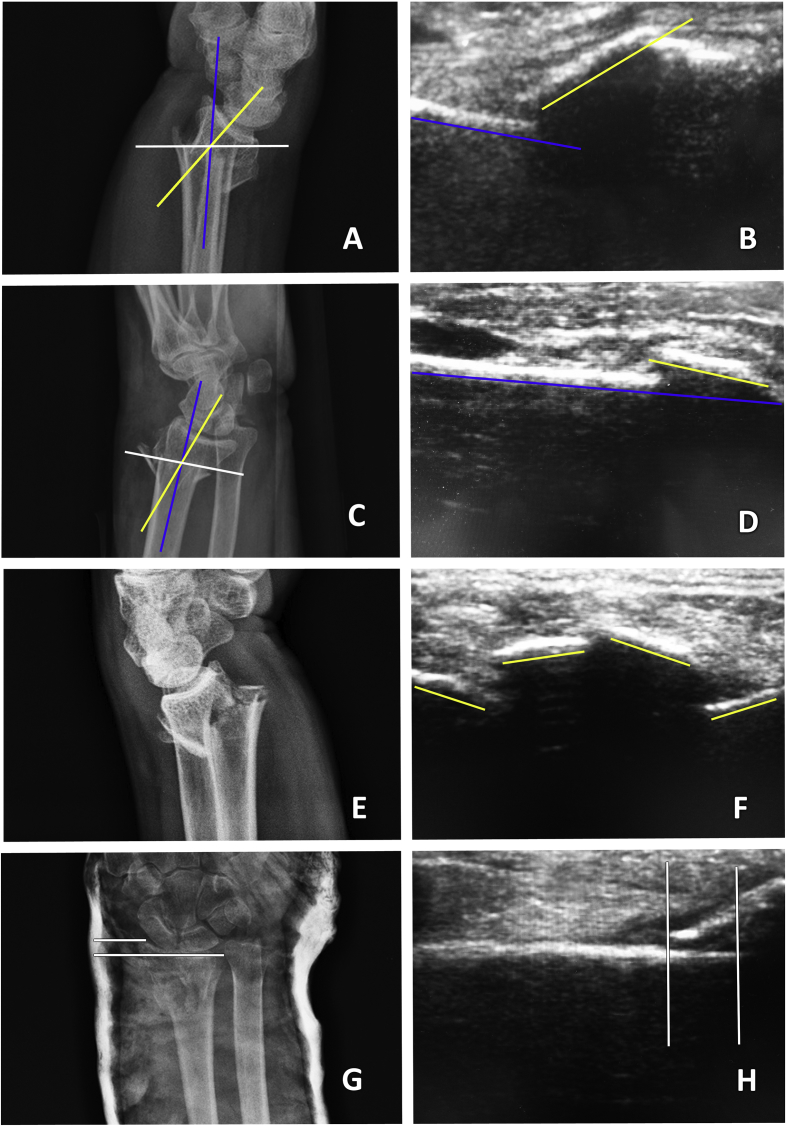
Fig. 5.
X-ray and corresponding US images of a distal radius fracture. A) The fracture (yellow line) is angulated dorsally (X-ray), long axis of the distal radius (blue line) B) The fracture (yellow line) is angulated dorsally (US), bone cortex axis of the proximal of the fracture (blue line) C) The fracture (yellow line) is angulated towards the volar part (X-ray), long axis of the distal radius (blue line) D) The fracture line angulated towards the volar part (US), bone cortex axis of the proximal of the fracture (blue line) E) Multiple-fracture lines seen on the dorsal image (X-ray), F) Multiple-fracture lines seen on the dorsal image (US), G) Radial shortening (X-ray), H) Radial shortening (US) (lateral image).
Post-reduction X-rays were later evaluated by an orthopedic surgeon who had not seen the patient nor the US images. A radial height of ≥5 mm, radial angulation of 15°–25°, and volar tilt angle between 0° and 20° were considered as radiographic criteria for acceptable reduction.9 If any of these parameters were outside the normal range, the reduction was deemed to be unsuccessful. In addition, the orthopedic surgeon evaluated the X-rays for angulation of the distal fragment, foreshortening of the radius, and for the presence of multiple fragments in the dorsum of the distal fragment. In the evaluation of reduction success, the opinion of the orthopedic surgeon who had evaluated the X-rays in a blinded fashion was accepted as the final diagnosis. Diagnoses made by the EM Attending Physician and orthopedic surgeon were compared by validation analysis, sensitivity, specificity, and positive and negative predictive values were calculated in terms of reduction success, dorsal/volar angulation, the presence of multiple fragments, and radial shortening, confidence interval (CI) is accepted as 95% in these analysis. For comparing the effect of the angulation, the presence of multiple fragments, and radial shortening on reduction success in terms of used imaging technique (US/X-ray) Chi-square tests are provided. SPSS 18.0 and MedCalc statistical software was used for statistical analysis. P values less than 0.05 were considered statistically significant.
3. Results
Sixty patients agreed to participate in the study; mean age was 49.2 ± 17.4 years old (range 18–83 years old) and 33.3% were male. The cause was low energy trauma (a simple fall) in 70% (n = 42) of patients and high energy trauma (13.3% fall from height, 10% traffic accident, 6.7% other causes) in the rest. All data about patients' demographic and clinical charachteristics are given in Table 1.
Table 1.
Demographic and clinical characteristics.
| Variables | |
|---|---|
| Sex, n (%) | |
| Male | 20 (33.3) |
| Comorbidities, n (%) | |
| No Comorbity | 36 (60.0) |
| Cardiovascular Disease | 14 (23.4) |
| Thyroid Disease | 3 (5.0) |
| Asthma | 2 (3.3) |
| Osteoporosis | 2 (3.3) |
| Malignancy | 2 (3.3) |
| Hepatic Disease | 1 (1.7) |
| Mechanism of Fall, n (%) | |
| Fall On Flat Surface | 42 (70.0) |
| Fall from Height | 8 (13.3) |
| Traffic Accident | 6 (10.0) |
| Other | 4 (6.7) |
According to the data given in Table 2, diagnostic accuracy test were performed. US was 97.5% (95% CI 86.8 to 99.9) sensitive and 95.0% (95% CI 75.1 to 99.9) specific in determining distal radius fracture reduction success; it had a positive predictive value (PPV) of 97.5% (95% CI 85.2 to 99.6) and negative predictive value (NPV) of 95.0% (95% CI 73.2 to 99.2) When compared to X-rays, US was 100% (95% CI 93.3 to 100.0) sensitive and 100% (95% CI 59.4 to 100.0) specific in determining the direction of angulation (dorsal vs. volar) of the distal fracture fragment (PPV and NPV 100% (95% CI 100.0%) (Table 3). When compared to X-rays, US was 86.5% (95% CI 71.2 to 95.5) sensitive and 73.9% (95% CI 51.6 to 89.8) specific in determining the presence of multiple fragments (PPV 84.2% (95% CI 72.6 to 91.5) and NPV 77.3% (95% CI 59.2 to 88.8)), while it was 67.5% (95% CI 50.9 to 81.4) sensitive and 65% (95% CI 40.8 to 84.6) specific in determining the presence of radial shortening (PPV 79.4% (95% CI 67.1 to 87.9) and NPV 50% (95% CI 36.6 to 63.4)) (Table 3).
Table 2.
Determining reduction success through X-ray and US.
| Successful Reduction Through X-ray n (%) | Unsuccessful Reduction Through X-ray n (%) | |
|---|---|---|
| Successful Reduction Through US | 39 (98.0) | 1 (2.0) |
| Unsuccessful Reduction Through US | 1 (5.0) | 19 (95.0) |
Table 3.
Identifying factors affecting reduction success through X-ray and US.
|
Angulation According To X-ray |
|||
|---|---|---|---|
| Dorsal, n (%) | Volar, n (%) | ||
| Angulation According To US | Dorsal | 53 (100) | 0 |
| Volar | 0 | 7 (100) | |
|
Comminuted fracture On X-ray |
|||
|
Yes, n (%) |
No, n (%) |
||
| Comminuted fracture On US | Yes | 32 (84.2) | 6 (15.8) |
| No | 5 (22.7) | 17 (77.3) | |
|
Radial Shortening On X-ray |
|||
|
Present n(%) |
None n(%) |
||
| Radial Shortening On US | Present | 27 (79.4) | 7 (20.6) |
| None | 13 (50.0) | 13 (50.0) | |
Characteristics affecting reduction success, such as angulation of the distal fragment, number of distal fragments, and radial shortening, as demonstrated by X-ray and US are shown in Table 4. Volar angulation of the distal fragment and multiple distal fracture fragments, seen by both X-ray and US, were associated in a significant fashion with reduced success of fracture reduction. While radial shortening seen on X-ray was associated with reduction failure, its appearance on US was not statistically associated with the failure of reduction. One patient deemed to have a successful reduction by US but unsuccessful reduction by X-ray probably had an artifact on the X-ray due to the plaster cast applied, making interpretation of the plain film difficult.
Table 4.
Determining reduction success through ultrasonography and X-ray in accordance with the identification of the factors affecting reduction success.
| Method of Identifying The Factor Affecting Reduction Success | Reduction Success in X-ray |
p | ||
|---|---|---|---|---|
| Successful n (%) | Unsuccessful n (%) | |||
| Angulation on X-ray | Dorsal | 38 (71.7) | 15 (28.3) | 0.036* |
| Volar | 2 (28.6) | 5 (71.4) | ||
| Angulation on US | Dorsal | 38 (71.7) | 15 (28.3) | 0.036* |
| Volar | 2 (28.6) | 5 (71.4) | ||
| Comminuted fracture on X-ray | No | 21 (91.3) | 2 (8.7) | 0.002* |
| Yes | 19 (51.4) | 18 (48.6) | ||
| Comminuted fracture on US | No | 19 (86.3) | 3 (13.7) | 0.022* |
| Yes | 21 (55.3) | 17 (44.7) | ||
| Radial Shortening on X-ray | Present | 22 (55.0) | 18 (45.0) | 0.008* |
| None | 18 (90.0) | 2 (10.0) | ||
| Radial Shortening on US | Present | 24 (70.6) | 10 (29.4) | 0.582 |
| None | 16 (61.5) | 10 (38.5) | ||
4. Discussion
Despite current technological developments in the medical sector, trauma continues to be a major cause of mortality and morbidity in the middle-aged, productive population. Distal fractures of the radius and the ulna are the most common serious injuries affecting the wrist.10 Proper initial treatment may lead to earlier return to work and optimal function in the long term.
In recent studies, US has been found to have high sensitivity and specificity in the diagnosis and reduction success of distal radius fractures in children.3,4,11, 12, 13 However, in adults, few studies have examined the use of US in the reduction of distal radius fractures. Ang et al. studied US by emergency physicians in distal radius fracture reduction success in adults by examining radial angle, radial height, and volar tilt.5 They found that volar tilt values were most accurate in predicting reduction success, and that reduction was most successful and associated with fewer manipulations when performed under US guidance. Esmailian et al. in their study of adults with distal radius fractures, found that US was 99.3% sensitive and 100% specific in the diagnosis of successful radius fracture reduction, with a 100% PPV and 88.9% NPV.14
In the 2011 study by Chinnock et al. of patients aged 3–87 years old undergoing distal radial fracture reduction using US guidance, the reduction success rate was compared to that of reduction success as determined by X-rays.2 They found that US diagnosed successful fracture reduction with 94% sensitivity, 56% specificity, 89% positive predictive value and 71% negative predictive value. The overall success rate of fracture reduction was 83% with US and 80% in historical controls (without US).
Socransky et al. found that implementation of bedside US for evaluation of distal radius fractures reduction process will lead to reduce of repetition of reduction attempts in 40%.6
Kodama et al. pointed out that post-reduction US has high correlation with X-ray findings despite it has some limitations and cannot measure directly the same parameters as radiographic images. Kodama et al. recommend that real time US providing while reduction procedure of the distal radius fracture should be considered as an additional tool in daily practice.7
To date, still there are few studies has examined reduction success and the pre-reduction findings of fracture instability by ultrasound in the patients with distal radius fracture, for example presence of multiple fragments, radial shortening in the fractured area, and volar or dorsal angulation of the fracture fragments.6, 7, 8,15,16 In our study, we found that volar or dorsal angulation of the fracture fragment and the presence of multiple fractures by US were easily seen. However, the sensitivity and specificity of US for measuring radial shortening was quite a bit lower; because of the lack of a linear reference point on the lateral or dorsal sides of the fracture lines. Volar angulation and the presence of multiple fragments on US were associated with fewer successful reductions. Although lower reduction success was found in patients with radial shortening on X-ray, the same was not found using US measurements.
US seems to be as an useful additional tool, which may help to reduction procedure of the distal radius fractures for better and quick evaluation of post-reduction success. Bedside US will also present additional data to the physicians before the reduction. Our results showed US had a high sensitivity and spesificity for prediction of reduction success and for direction of the angulation of the fracture.
5. Limitations
When the fracture line was examined over the lateral and dorsal faces, a reference point could not be easily determined for measuring radial shortening by US. This may have led to inaccurate measurements of radial shortening. Angulation was only defined according its direction as dorsal or volar. Measuring of the degree of angulation was not possible because of bone cortex was not a linear line in US images.
For determination of failed reductions we preferred to choose the criteria which are made possible and correctly calculated in both X-ray and US evaluation, such as volar angulation, radial shortening and comminuted fracture. Despite this selection we even failed mostly to define radial shortening because of difficulties for finding of any reference point for calculation. We didn't calculated radial inclination, ulnar variance and also intraarticular stepping. The types of distal radius fractures were not defined as detailed because of the main aim was to evaluate the accuracy of the US in distal radius fracture reduction.
No sample size analysis was made, patients enrolled consecutively to the study because of unpredictable number of the patient admissions to the ED, this situation caused a relatively small sample size. Another limitation issue was to use only one sonographer, which made our results operator-depended.
6. Conclusions
Characteristics of distal radius fractures needing fracture reduction are easily seen on bedside ultrasound and can predict reduction success. Also US presents quick, reliable and useful data to the physicians, for managing distal radius fracture reductions. Therefore, implementation of the sonographic evaluation to the reduction procedure of the distal radius fractures seems to be helpful for the orthopedics and emergency physicians. In future prospective studies, US findings of instability (multiple fracture fragments, angulation, and radial shortening) should be taken into account when EM physicians manage distal radius fractures needing reduction and also patient groups may be compared in terms of reduction success, according to whether ultrasonography is applied or not during the reduction procedure.
Authors contributions
ME, OB, FKA conceived the study and designed the trial. ME, OB, FKA, SY, SM and LK contributed on study design and ME analyzed the data. ME, OB, FKA, SY, SM, LK drafted the manuscript, and all authors contributed substantially to its revision. ME takes responsibility for the paper as a whole.
Conflicts of interest
The authors have no commercial associations or sources of support that might pose a conflict of interest.
Footnotes
Peer review under responsibility of The Emergency Medicine Association of Turkey.
References
- 1.Escarza R., Loeffel M.L., Uehara D.T. Wrist injuries. In: Tintinalli J.E., Stapczynski J.S., Ma O.J., Yealy D.M., Meckler G.D., Cline D.M., editors. Emergency Medicine: a Comprehensive Study Guide. eighth ed. McGraw-Hill; New York, NY: 2016. pp. 1801–1815. [Google Scholar]
- 2.Chinnock B., Khaletskiy A., Kuo K., Hendey G.W. Ultrasound-guided reduction of distal radius fractures. J Emerg Med. 2011;40:308–312. doi: 10.1016/j.jemermed.2009.09.018. [DOI] [PubMed] [Google Scholar]
- 3.Chen L., Kim Y., Moore C.L. Diagnosis and guided reduction of forearm fractures in children using bedside ultrasound. Pediatr Emerg Care. 2007;23:528–531. doi: 10.1097/PEC.0b013e318128f85d. [DOI] [PubMed] [Google Scholar]
- 4.Patel D.D., Blumberg S.M., Crain E.F. The utility of bedside ultrasonography in identifying fractures and guiding fracture reduction in children. Pediatr Emerg Care. 2009;25:221–225. doi: 10.1097/pec.0b013e31819e34f7. [DOI] [PubMed] [Google Scholar]
- 5.Ang S.H., Lee S.W., Lam K.Y. Ultrasound-guided reduction of distal radius fractures. Am J Emerg Med. 2010;28:1002–1008. doi: 10.1016/j.ajem.2009.05.022. [DOI] [PubMed] [Google Scholar]
- 6.Socransky S., Skinner A., Bromley M. Ultrasound-Assisted distal radius fracture reduction. Cureus. 2016;8 doi: 10.7759/cureus.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kodama N., Takemura Y., Ueba H., Imai S., Matsusue Y. Ultrasound-assisted closed reduction of distal radius fractures. J Hand Surg Am. 2014;39:1287–1294. doi: 10.1016/j.jhsa.2014.02.031. [DOI] [PubMed] [Google Scholar]
- 8.Sabzghabaei A., Shojaee M., Arhami Dolatabadi A., Manouchehrifar M., Asadi M. Ultrasound-Guided reduction of distal radius fractures. Emerge. 2016;4:132–135. [PMC free article] [PubMed] [Google Scholar]
- 9.Perez E.A. Fractures of the shoulder, arm, and forearm. In: Canale S.T., Beate J.H., editors. Campbell's Operative Orthopaedics. twelfth ed. Elsevier – Mosby; Philedelphia: 2013. pp. 2829–2916. [Google Scholar]
- 10.Chung K.C., Spilson S.V. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001;26:908–915. doi: 10.1053/jhsu.2001.26322. [DOI] [PubMed] [Google Scholar]
- 11.Herren C., Sobottke R., Ringe M.J. Ultrasound-guided diagnosis of fractures of the distal forearm in children. Orthop Traumatol Surg Res. 2015;101:501–515. doi: 10.1016/j.otsr.2015.02.010. [DOI] [PubMed] [Google Scholar]
- 12.Eckert K., Ackermann O., Schweiger B., Radeloff E., Liedgens P. Ultrasound as a viable alternative to standard X-rays for the diagnosis of distal forearm fractures in children. Z für Orthop Unfallchirurgie. 2012;150:409–414. doi: 10.1055/s-0032-1314974. [DOI] [PubMed] [Google Scholar]
- 13.Chaar-Alvarez F.M., Warkentine F., Cross K., Herr S., Paul R.I. Bedside ultrasound diagnosis of nonangulated distal forearm fractures in the pediatric emergency department. Pediatr Emerg Care. 2011;27:1027–1032. doi: 10.1097/PEC.0b013e318235e228. [DOI] [PubMed] [Google Scholar]
- 14.Esmailian M., Zargarbashi E.H., Masoumi B., Karami M. Accuracy of ultrasonography in confirmation of adequate reduction of distal radius fractures. Emerge. 2013;1:7–10. [PMC free article] [PubMed] [Google Scholar]
- 15.Kurklu M., Koca K., Ege T., Mahirogulları M., Basbozkurt M. Current management approaches to distal radius fractures. TOTBİD Dergisi. 2012;11:41–48. [Google Scholar]
- 16.Chen N.C., Jupiter J.B. Management of distal radial fractures. J Bone Joint Surg Am. 2007;89:2051–2062. doi: 10.2106/JBJS.G.00020. [DOI] [PubMed] [Google Scholar]