Abstract
Background:
The incidence of coexisting osteochondral lesions (OCLs) of the tibia and talus has been negatively correlated with successful clinical outcomes, yet these lesions have not been extensively characterized.
Purpose:
To determine the incidence of coexisting tibial and talar OCLs, assess the morphologic characteristics of these lesions, and evaluate whether these characteristics are predictive of outcome.
Study Design:
Case series; Level of evidence, 4.
Methods:
A total of 83 patients who underwent surgery for a talar OCL were evaluated for coexisting OCLs of the distal tibia with preoperative magnetic resonance images. Size, location, containment, International Cartilage Repair Society (ICRS) grade, patient age, and patient sex were analyzed for predictors of coexisting lesions or patient outcome. The talar and tibial surfaces were each divided into 9 zones, with 1 corresponding to the most anteromedial region and proceeding laterally and then posteriorly. The Foot and Ankle Outcome Score (FAOS) was evaluated pre- and postoperatively.
Results:
Twenty-six patients (31%) had coexisting tibial and talar OCLs, with 9 (35%) identified as kissing lesions. Age correlated with coexisting lesion incidence, as older patients were more likely to have a coexisting tibial OCL (P = .038). More than half of talar OCLs were found in zone 4 (61%), whereas the majority of tibial OCLs were located in zones 2, 4, and 5 (19% each). Patients with coexisting lesions were more likely to have a lateral talar OCL (P = .028), while those without a coexisting tibial lesion were more likely to have a talar OCL in zone 4 (P = .016). There was no difference in FAOS result or lesion size between patients with and without coexisting OCLs, but patients with coexisting lesions were more likely to have an ICRS grade 4 talar OCL (P = .034). For patients with coexisting lesions, kissing lesions were more likely to be located in zone 6 (P = .043). There was no difference in OCL size or containment between kissing and nonkissing coexisting OCLs.
Conclusion:
The incidence of coexisting talar and tibial OCLs may be more prevalent than what previous reports have suggested, with older patients being more likely to present with this pathology. The location of a talar OCL correlates with the incidence of a coexisting tibial OCL.
Keywords: osteochondral, kissing lesion, incidence, coexisting, cartilage, ankle
Osteochondral lesions (OCLs) are common defects in weightbearing joints involving the articular cartilage and/or subchondral bone and are typically caused by a single or multiple traumatic events in the ankle joint.36 OCLs of the tibial plafond are less common than those of the talus, but both defects have a poor repair capacity because of the limited vascular supply of cartilage. Therefore, untreated OCLs may result in chronic ankle pain, functional impairment, and subchondral cyst formation, and they have the potential to chronically degrade, leading to posttraumatic osteoarthritis.2,3,23,30 The frequency with which talar and tibial OCLs co-occur was previously reported and varied from 15.8% to 45%.10,29 No study to date has investigated the relationship between the morphologic characteristics of one lesion and the incidence of a coexisting OCL on either counter surface in the ankle.
Predictors of outcome in the surgical treatment of talar OCLs are lesion size, containment, concurrent lateral ankle instability, and the presence of a coexisting tibial OCL.6,17,21,33,35 Consequently, current surgical treatment paradigms for talar OCLs are determined principally by these factors but do not account for a coexisting tibial OCL.34 It is unknown whether the morphologic characteristics of talar OCLs affect the incidence of coexisting tibial OCLs, whether the morphologic characteristics of coexisting tibial OCLs influence outcomes following treatment, or how coexisting OCL characteristics may direct treatment strategies overall.
The purpose of this study was to determine the incidence of coexisting OCLs of the talus and distal tibia in patients who were treated for symptomatic talar lesions, to investigate the relationship of morphologic characteristics between them, and to evaluate whether these relationships correlate with patient outcome.
Methods
Study Population
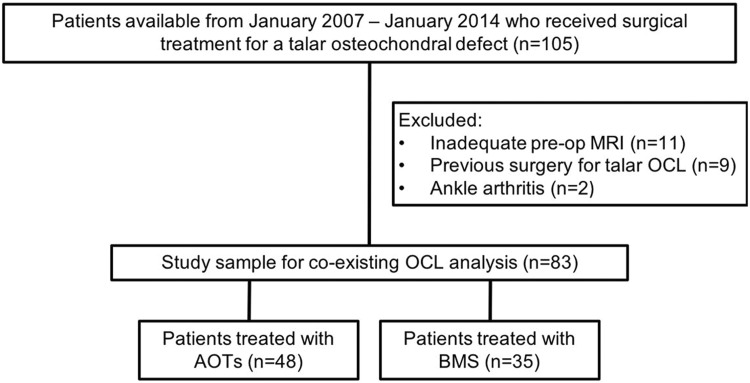
This study was approved by the hospital’s institutional review board and was performed in compliance with regulations from the Health Insurance Portability and Accountability Act. Patients who underwent surgery for the treatment of a talar OCL, including bone marrow stimulation (BMS) or autologous osteochondral transplantation (AOT), between 2007 and 2014 at the senior author’s (J.G.K.) institution (Hospital for Special Surgery) were included in this study (Figure 1). The exclusion criteria for this study were as follows: rheumatoid arthritis, signs of degenerative joint change on preoperative imaging, inadequate preoperative magnetic resonance imaging (MRI) regarding quality or availability, and previous ankle surgery. Demographic information about each patient was also collected.
Figure 1.
CONSORT (Consolidated Standards of Reporting Trials) flow diagram illustrating exclusion criteria and grouping of surgical operations performed. AOT, autologous osteochondral transplantation; BMS, bone marrow stimulation; MRI, magnetic resonance imaging; OCL, osteochondral lesion.
Surgical Technique
The treatment strategy for talar OCLs was based on lesion size, with a lesion <15 mm in diameter receiving BMS and larger lesions receiving AOTs.37 The operative techniques for BMS and AOT were performed as previously described by the senior author.19,26 BMS was performed arthroscopically by debriding the cartilage defect through the calcified layer to expose the subchondral bone. This was followed by perforations through the subchondral plate with a 2 mm–diameter microfracture awl at 3- to 4-mm intervals to allow fibrin clot formation. The AOT procedure involved removing an osteochondral core from the defect site, followed by harvesting an osteochondral graft from a nonweightbearing portion of the ipsilateral knee of the patient and placing it into the defect site in the ankle. A Chevron-type medial malleolar osteotomy was typically utilized for medial lesions,20 and an anterolateral tibial osteotomy was used for lateral lesions if required.15 All cases received an intra-articular injection of concentrated bone marrow aspirate as a biological adjuvant therapy.31 Patients who had coexisting tibial lesions were treated with BMS at the time of surgery and with concentrated bone marrow aspirate in a similar fashion. All procedures were performed by the senior author.
Clinical Evaluation
Clinical evaluation was carried out with the Foot and Ankle Outcome Score (FAOS) before surgery and at final follow-up.
MRI Assessment
Preoperative MRI was performed with a clinical imaging system at 3 T (GE Healthcare). A board-certified musculoskeletal radiologist (T.W.D.) reviewed all images. The radiologist was aware that all patients had a talar OCL, was instructed to investigate if any coexisting lesions on the tibia were present, and was blinded to the initial radiology reports and clinical data. There was a consensus meeting between the authors and the radiologist for the diagnosis, staging, and location of OCLs before imaging interpretation commenced. Lesion size was determined by calculating the area with the following formula5: area = coronal length × sagittal length × 0.79. A lesion was uncontained if it was located on the medial or lateral shoulder of the talus.
MRI scans were graded with the modified International Cartilage Repair Society (ICRS) classification system for grading OCLs.9 This system divides OCLs on MRI into 4 categories: grade 1, thickening of the cartilage without disruption, including bone marrow edema or fluid at the bone-lesion interface; grade 2, cartilage breached and fluid at partial but not entire interface; grade 3, cartilage completely disrupted with fluid interface surrounding lesion; and grade 4, displaced fragment.12
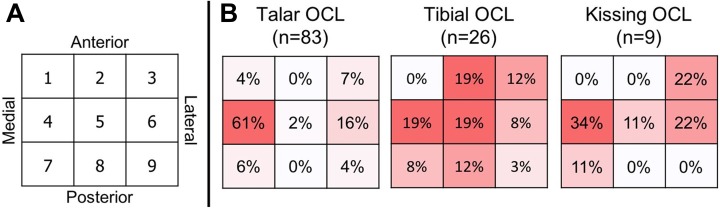
To describe the location of the OCLs, the talar and tibial surfaces were each divided into 9 zones with a 3 × 3 grid as previously described.10,11 Each zone was equal in area and assigned a number between 1 and 9, with 1 corresponding to the most anteromedial region and proceeding laterally and then posteriorly (Figure 2). If a lesion was contained in >1 zone, the lesion was recorded to exist in the zone where its center was located. If there were ≥2 OCLs, the largest lesion was assessed and included in the analysis. The presence of a kissing lesion, defined as lesions where the talar and tibial OCLs were in the same zone location, was also identified (Figure 3).
Figure 2.
Zone locations shown in (A) a grid format and (B) corresponding heat maps showing the distribution of all talar (n = 83), tibial (n = 26), and kissing (n = 9) osteochondral lesions (OCLs). Heat map colors correspond with the percentage of lesions found in each zone, with darker red indicating the higher percentages and white showing zero values.
Figure 3.
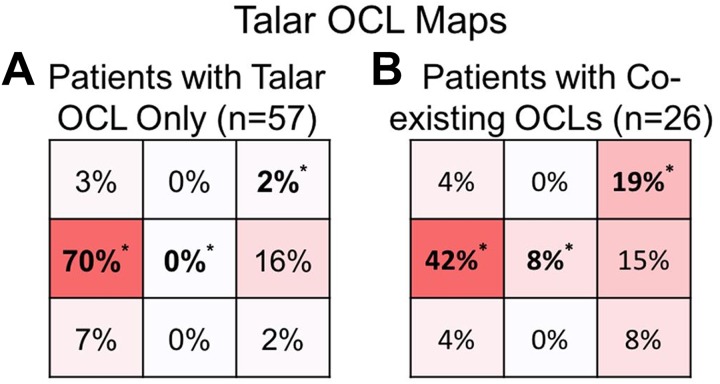
Heat maps of talar osteochondral lesion (OCL) locations divided between (A) patients without a coexisting tibial lesion (n = 57) and (B) patients with a coexisting tibial lesion (n = 26). Heat map colors correspond with percentage of lesions found in each zone. *P < .05 between groups based on chi-square test.
Statistical Analysis
Statistical analysis was carried out with RStudio software (v 1.0.153; RStudio Inc). We performed t tests to compare lesion size, patient age, and pre- and postoperative FAOS between independent patient subgroups, which included sex, existence of a coexisting lesion, and kissing lesions among those with coexisting lesions. Two-group comparisons were performed with a chi-square test. Comparisons were made between the following groups: incidence of coexisting lesions with sex, FAOS with sex, lesion location between patient subgroups, ICRS stage between patient subgroups, and talar lesion containment between patient subgroups. An odds ratio (OR) and 95% CI were computed for all comparisons that showed significance from chi-square test results, except for groups containing a zero cell value for one of the elements. Multiple linear regression was performed to determine the relationship between patient variables (age and sex) and lesion characteristics (size, containment, location, and ICRS grade) on postoperative FAOS. Logistic regression was performed to determine the relationship between the same patient variables and lesion characteristics on the incidence of a coexisting lesion. Lesion size was represented as mean ± SD. For all analyses, P < .05 was considered statistically significant.
Results
Demographics and Clinical Outcome
A total of 105 patients who underwent surgery for talar OCL were identified (BMS, 35 patients; AOT, 48 patients), and 83 were included after exclusion (Figure 1). Patient demographic and clinical outcomes are shown in Table 1. Age was significantly higher in the coexisting OCL group than the talar OCL group (P = .038). All patients showed increased postoperative FAOS at a mean follow-up of 32 months (P < .001). We detected no difference in mean pre- or postoperative FAOS between patients with only talar OCL and coexisting OCL (P = .115 and .711, respectively). In addition, no difference was found in postoperative FAOS between patients who received AOTs and BMS (P = .421).
TABLE 1.
Demographics by Lesion Typea
| All Patients (N = 83) | Patients by Incidence of Coexisting OCL | |||
|---|---|---|---|---|
| Talar OCL Only (n = 57) | Coexisting OCL (n = 26) | P | ||
| Age | 38.4 ± 14.5 | 36.1 ± 13.8 | 43.5 ± 14.8 | .038 |
| Sex | .135 | |||
| Male | 41 (49) | 25 (44) | 16 (62) | |
| Female | 42 (51) | 32 (56) | 10 (38) | |
| FAOS | ||||
| Preoperative | 53.9 ± 15.9 | 56.0 ± 14.3 | 49.4 ± 18.6 | .115 |
| Postoperative | 82.9 ± 13.2 | 82.5 ± 12.6 | 83.8 ± 14.7 | .711 |
aValues are presented as mean ± SD or n (%). Bolded P value indicates statistically significant difference between groups (P < .05). FAOS; Foot and Ankle Outcome Score; OCL, osteochondral lesion.
Multiple linear regression results showed that patient age and lateral talar OCL location (zones 3, 6, and 9) correlated with the incidence of a coexisting lesion, where older patients and patients with a lateral talar OCL were more likely to have a coexisting lesion (P = .012 and .009, respectively); however, talar lesion size did not significantly correlate with coexisting OCL incidence (P = .062) (Appendix Table A1). For the relationship of patient variables and lesion characteristics with patient outcome, only sex correlated with postoperative FAOS: female patients had a lower postoperative FAOS as compared with male patients (P = .034) (Appendix Table A2).
Lesion Characteristics
The assessment of talar and tibial lesion characteristics is shown in Table 2. Fifty-seven patients (68.7%) had only a talar OCL, and 26 (31.3%) had coexisting talar and tibial OCLs. Of the 26 patients with coexisting lesions, 9 had kissing lesions and 17 had nonkissing lesions. Figure 2 shows the distribution of talar and tibial OCLs. In talar OCLs, 61% were in zone 4, with zone 6 as the second-most common location (16%); for coexisting tibial OCLs, the highest frequency was found in zones 2, 4, and 5 (19% each) (Figure 2B). Overall, coexisting tibial OCLs occurred more frequently in zones 2, 5, and 8 (P < .001; OR, 9.64; 95% CI, 1.75-53.24; P = .002, and P = .002, respectively), and talar OCLs occurred more frequently in zone 4 (OR, 6.69; 95% CI, 2.29-19.53; P < .001).
TABLE 2.
Talar and Tibial OCL Characteristicsa
| All Talar OCLs (n = 83) | All Tibial OCLs (n = 26) | P | χ2 | |
|---|---|---|---|---|
| Lesion size, mm2 | 85.4 ± 50.9 | 63.6 ± 58.4 | .096 | |
| Location of lesion | <.001 | 43.52 | ||
| Zone 1 | 3 (4) | 0 (0) | .326 | 0.966 |
| Zone 2 | 0 (0) | 5 (19) | <.001 | 16.73 |
| Zone 3 | 6 (7) | 3 (12) | .486 | 0.485 |
| Zone 4 | 51 (61) | 5 (19) | <.001 | 14.12 |
| Zone 5 | 2 (2) | 5 (19) | .002 | 9.322 |
| Zone 6 | 13 (16) | 2 (8) | .303 | 1.060 |
| Zone 7 | 5 (6) | 2 (8) | .762 | 0.092 |
| Zone 8 | 0 (0) | 3 (12) | .002 | 9.848 |
| Zone 9 | 3 (4) | 1 (3) | .956 | 0.003 |
| ICRS grade | .001 | 15.48 | ||
| 1 | 20 (24) | 11 (42) | .072 | 3.226 |
| 2 | 55 (66) | 10 (39) | .012 | 6.358 |
| 3 | 6 (7) | 0 (0) | .158 | 1.989 |
| 4 | 2 (3) | 5 (19) | .002 | 9.322 |
aValues are presented as mean ± SD or n (%). Bolded P values indicate statistically significant difference between groups (P < .05). ICRS, International Cartilage Repair Society; OCL, osteochondral lesion.
There was no significant difference in size between talar and tibial lesions (P = .096); however, the mean size of talar OCLs was larger than that of tibial OCLs. There was a significant difference in ICRS grade between talar OCLs and tibial OCLs (P < .001), with talar OCLs more likely to be classified as grade 2 (OR, 3.14; 95% CI, 1.26-7.82; P = .012). Additionally, tibial OCLs were more likely than talar OCLs to be classified as grade 4 (OR, 9.64; 95% CI, 1.75-53.24; P = .002) (Table 2).
Talar Lesion Characteristics by Coexistence of Tibial Lesions
Table 3 shows the assessment of talar lesion characteristics according to the presence of coexisting tibial OCL. There was no difference in the size of talar OCLs between patients with coexisting lesions and those without (P = .196). Patients with a talar OCL in zones 3 and 5 were more likely to have a coexisting tibial OCL (OR, 13.3; 95% CI, 1.47-120.92; P = .004 and .034, respectively), while patients with a talar OCL in zone 4 were less likely to have a coexisting tibial OCL (OR, 7.26; 95% CI, 2.15-24.50; P = .016). Figure 3 shows the distribution of talar OCLs divided by patients with and without coexisting tibial OCL. Talar OCLs among patients who had a coexisting tibial OCL were more likely to have an ICRS grade of 4 (P = .034).
TABLE 3.
Talar OCL Characteristics by Coexistence of Tibial OCLa
| Talar OCL Without Tibial OCL (n = 57) | Talar OCL With Tibial OCL (n = 26) | P | χ2 | |
|---|---|---|---|---|
| Lesion size, mm2 | 79.6 ± 41.6 | 98.1 ± 66.1 | .196 | |
| Location of lesion | .013 | 16.23 | ||
| Zone 1 | 2 (3) | 1 (4) | .939 | 0.006 |
| Zone 2 | 0 (0) | 0 (0) | ≥.999 | 0.000 |
| Zone 3 | 1 (2) | 5 (19) | .004 | 8.132 |
| Zone 4 | 40 (70) | 11 (42) | .016 | 5.853 |
| Zone 5 | 0 (0) | 2 (8) | .034 | 4.493 |
| Zone 6 | 9 (16) | 4 (15) | .963 | 0.002 |
| Zone 7 | 4 (7) | 1 (4) | .573 | 0.317 |
| Zone 8 | 0 (0) | 0 (0) | ≥.999 | 0.000 |
| Zone 9 | 1 (2) | 2 (8) | .179 | 1.807 |
| ICRS grade | .176 | 4.941 | ||
| 1 | 13 (23) | 7 (27) | .684 | 0.165 |
| 2 | 40 (70) | 15 (57) | .265 | 1.245 |
| 3 | 4 (7) | 2 (8) | .912 | 0.012 |
| 4 | 0 (0) | 2 (8) | .034 | 4.493 |
| Uncontained | 49 (86) | 19 (73) | .157 | 2.003 |
aValues are presented as mean ± SD or n (%). Bolded P values indicate statistically significant difference between groups (P < .05). ICRS, International Cartilage Repair Society; OCL, osteochondral lesion.
Talar and Tibial Lesion Characteristics by Occurrence of Kissing Lesions
Table 4 shows the assessment of lesion characteristics according to occurrence of kissing lesions. Out of the 26 patients who had a coexisting tibial OCL, 9 (35%) had kissing lesions. Kissing lesions were found only in zones 3 through 7, with the majority found in zone 4 (34%) (Figure 2B). There was no significant difference in OCL size, containment, FAOS, or ICRS grade between kissing and nonkissing lesions. However, tibial kissing OCLs were more likely to be found in zone 6 when compared with nonkissing coexisting tibial lesions (P = .043). Additionally, among patients with coexisting lesions, talar kissing lesions were more likely to be ICRS grade 3 compared with nonkissing talar lesions (P = .043).
TABLE 4.
Talar and Tibial OCL Characteristics by Occurrence of Kissing Lesionsa
| Talar OCL | Tibial OCL | |||||||
|---|---|---|---|---|---|---|---|---|
| Nonkissing (n = 17) | Kissing (n = 9) | P | χ2 | Nonkissing (n = 17) | Kissing (n = 9) | P | χ2 | |
| Lesion size, mm2 | 103.4 ± 73.2 | 88.1 ± 52.4 | .545 | 70.6 ± 65.2 | 50.4 ± 43.1 | .355 | ||
| Location of lesion | .619 | 4.431 | .143 | 1.90 | ||||
| Zone 1 | 1 (6) | 0 (0) | .458 | 0.551 | 0 (0) | 0 (0) | ≥.999 | 0.000 |
| Zone 2 | 0 (0) | 0 (0) | ≥.999 | 0.000 | 5 (28) | 0 (0) | .070 | 3.278 |
| Zone 3 | 3 (18) | 2 (22) | .778 | 0.079 | 1 (6) | 2 (22) | .215 | 1.539 |
| Zone 4 | 8 (46) | 3 (34) | .500 | 0.454 | 3 (18) | 3 (34) | .366 | 0.816 |
| Zone 5 | 1 (6) | 1 (11) | .634 | 0.227 | 3 (18) | 1 (11) | .660 | 0.193 |
| Zone 6 | 2 (12) | 2 (22) | .482 | 0.494 | 0 (0) | 2 (22) | .043 | 4.093 |
| Zone 7 | 0 (0) | 1 (11) | .161 | 1.964 | 1 (6) | 1 (11) | .634 | 0.227 |
| Zone 8 | 0 (0) | 0 (0) | ≥.999 | 0.000 | 3 (18) | 0 (0) | .180 | 1.795 |
| Zone 9 | 2 (12) | 0 (0) | .284 | 1.147 | 1 (6) | 0 (0) | .458 | 0.551 |
| ICRS grade | .141 | 5.465 | .188 | 3.346 | ||||
| 1 | 4 (23) | 3 (34) | .592 | 0.287 | 6 (35) | 5 (56) | .320 | 0.990 |
| 2 | 11 (65) | 4 (44) | .320 | 0.990 | 6 (35) | 4 (44) | .648 | 0.208 |
| 3 | 0 (0) | 2 (22) | .043 | 4.093 | 0 (0) | 0 (0) | ≥.999 | 0.000 |
| 4 | 2 (12) | 0 (0) | .284 | 1.147 | 5 (30) | 0 (0) | .070 | 3.277 |
| Uncontained | 12 (71) | 7 (78) | .694 | 0.155 | — | — | — | — |
aValues are presented as mean ± SD or n (%). Bolded P values indicate statistically significant difference between groups (P < .05). P value for lesion size based on independent t test; P value for all other parameters based on chi-square test. ICRS, International Cartilage Repair Society; OCL, osteochondral lesion.
Discussion
The current study showed a 31% incidence of coexisting tibial lesions among patients with talar OCL, supporting our previous findings and those of other investigations that OCLs of the talus and distal tibia are not rare.7,29 Cuttica et al7 reported a similar incidence (30.7%) in a study of 13 patients who were treated for a tibial OCL. Elias et al10 and You et al38 both reported about half of that incidence (15.8%) in studies of 38 and 297 patients, respectively. The differences between these reports may be a result of differences in study design, as Cuttica et al7 and Elias et al10 evaluated patients with tibial OCLs for coexisting talar OCLs. In contrast, our study evaluated patients with talar OCLs for coexisting tibial OCLs. Additionally, our study had a larger sample size and may have more accurately captured the incidence of coexisting lesions in the ankle. The study by You et al38 had the largest sample size but included patients who were diagnosed with talar OCLs regardless of whether they pursued surgery after diagnosis. Our study excluded patients who did not require surgery, and our results showed a higher incidence of coexisting lesions. As conservative treatment had failed for the patients in our study group, this finding suggests that patients with symptomatic talar OCLs may be more likely to present with a coexisting tibial OCL.
The current investigation demonstrated that overall talar OCL size did not correlate with the incidence of a coexisting tibial OCL. Larger talar OCLs were shown to correlate with poorer clinical outcomes,5,7,8,16 but we did not find an association with larger tibial lesions and poorer scores either clinically or radiologically. Additionally, we found that the incidence of a coexisting lesion did not result in any differences in postoperative FAOS. This finding could be attributed to the type of lesion found on the tibial surface, as the most common ICRS grade for the tibial lesions was grade 1 (42%), indicating bone marrow edema. This would explain why no difference in postoperative FAOS was observed between patients with coexisting lesions and those with only a talar lesion, as bone bruises continuous with the adjacent articular surface can heal without intervention.36 Choi et al4 reported that the number of coexisting intra-articular lesions, including soft tissue impingement, subchondral cysts, ankle instability, and tibial lesions, could predict poor clinical outcomes, with patients having 3 associated lesions being more likely to experience in clinical failure. However, it has not been shown that coexisting lesions are independently correlated with poorer clinical outcomes.21
In the current study, the highest frequency of talar OCLs were found in zone 4 (61.0%), which is consistent with previous studies.11,18 Among patients who had coexisting lesions, 42% of talar OCLs were located in lateral zones (3, 6, or 9), as opposed to only 20% among patients who did not have a coexisting tibial OCL. Results also showed that patients with a talar OCL located laterally were more likely to have a coexisting tibial OCL as compared with patients with a talar OCL in any other location (OR, 3.07; 95% CI, 1.12-8.49; P = .028). Trauma and lateral ankle instability are 2 factors that predispose patients for developing a lateral-side talar OCL.13,21,32,35 Therefore, we speculate that patients who have had a traumatic injury paired with lateral ankle instability would be predisposed to a lateral talar OCL and a coexisting tibial OCL. It has been postulated that lateral ligament disruption causes subtle subluxation of the talus from its mechanical mortise, resulting in divergent wear patterns on the lateral half of the talus and eventual cartilage damage.32,35 Our results support the position that injuries resulting in OCL formation on the lateral side of the talus are more likely to result in concurrent damage to the tibial cartilage.
The current study also found that age correlates with incidence of coexisting lesions, with older patients more likely to have cartilage damage to both ankle joint surfaces. This has been reported by previous studies investigating patients diagnosed and treated surgically for talar OCLs.4 Older age is considered a risk factor for osteoarthritis development,14,25,28 and in vitro studies have shown that chondrocyte synthetic activity decreases with age.22 Therefore, once the cartilage tissue is damaged on both surfaces, chondrocytes in older patients have a lesser capacity for repair, and there is a higher risk that the damage may develop into coexisting OCLs.
It has been speculated that the etiology of tibial OCLs may be related to the difference in mechanical properties of the articular cartilage, as OCLs on the talar dome are more common and distal tibial cartilage has been shown to be stiffer than talar cartilage.1,24,27,36 Specifically, the anterolateral and posteromedial cartilage at the distal tibia is stiffer,1 which corresponds to the locations where coexisting tibial OCLs were less frequently positioned in this study (Figure 3B). The most common location for coexisting tibial lesions was in the central zones (2, 5, and 8), corresponding to the more compliant regions of cartilage. Therefore, our results indicate that the stiffer regions of cartilage on the distal tibia are less prone to coexisting OCL development.
Out of the 26 patients with coexisting OCLs in this study, 34.6% presented with kissing lesions. Cuttica et al7 found that 1 of 4 patients with coexisting OCLs of the tibia and talus had a true kissing lesion. Elias et al10 reported a similar result, with 1 of 6 patients with coexisting OCLs having a kissing lesion. The current study identified a higher incidence of kissing lesions, which could be attributed to the larger sample size of patients who presented with coexisting lesions, thereby more accurately capturing the prevalence of kissing lesions. This may be an aspect of the study design, as patients who received surgical treatment for a symptomatic talar OCL were included in our study. There is still variability in the incidence of kissing lesions among studies, thus indicating that future studies are warranted to determine the incidence of kissing lesions among patients with coexisting talar and tibial OCLs and to evaluate if coexisting tibial lesions influence clinical outcomes among patients with talar OCLs.
A limitation to this study was that our patient cohort consisted of those who were diagnosed with a talar OCL and received surgery to remedy the osteochondral defect. This excluded patients who had asymptomatic or only mildly symptomatic OCLs, where conservative treatment is sufficient and surgery is not warranted; therefore, our incidence of coexisting lesions is not representative of patients with asymptomatic talar OCLs. While our study population consisted of a relatively small sample size, we were still able to confirm trends found in previous publications and report new findings. This was a retrospective study, and only 1 senior radiologist scored the MRI for the ICRS grading system, without accounting for any intraobserver error. Additionally, true coexisting lesions cannot be identified in cases of early arthritis, so that population of patients could not be included in our study.
Conclusion
The incidence of coexisting talar and tibial OCLs may be more prevalent than what previous reports have suggested. We found that age correlates with incidence of coexisting talar and tibial OCLs and that patients with a lateral talar OCL are more likely to present with a coexisting tibial OCL. This information may help surgeons evaluate tibial cartilage more carefully when operating on talar OCLs.
APPENDIX
TABLE A1.
Logistic Regression Results for the Relationship Between Patient Parameters and Lesion Characteristics on the Incidence of Coexisting OCLsa
| Original Model | Reduced Model | |||
|---|---|---|---|---|
| Model = glm(coexist ∼ age + sex + talar grade + talar lateral zone + talar size + talar containment) | Model = glm(coexist ∼ age + talar lateral zone) | |||
| Parameter | Coefficient | P | Coefficient | P |
| Age | 0.043 | .039 | 0.050 | .012 |
| Sex | 0.199 | .734 | ||
| Talar grade | 0.548 | .210 | ||
| Talar lateral zone | 1.699 | .015 | 1.512 | .009 |
| Talar lesion size | 0.011 | .062 | ||
| Talar containment | –0.849 | .228 | ||
aOriginal model (left), with all parameters included, was evaluated first, which revealed 2 statistically significant parameters: age and talar osteochondral lesions (OCLs) located in lateral zones. The model was reduced to these 2 parameters (right), where age and talar OCLs located in lateral zones were significant. An analysis of variance was performed to confirm that reducing the model to include only age and talar lateral zone accepts the null hypothesis that the other parameter coefficients from the original model are equal to zero. All statistical analyses were performed with R, and P < .05 is considered statistically significant (in bold).
TABLE A2.
Linear Regression Results for the Relationship Between Patient Parameters and Talar OCL Characteristics on Postoperative FAOSa
| Original Model | Reduced Model | |||
|---|---|---|---|---|
| Model = lm(postoperative FAOS ∼ age + sex + talar grade + talar zone + talar size + talar containment + coexist) | Model = lm(postoperative FAOS ∼ sex) | |||
| Parameter | Coefficient | P | Coefficient | P |
| Age | –0.173 | .127 | ||
| Sex | 5.993 | .046 | 6.119 | .034 |
| Talar grade | –0.060 | .980 | ||
| Talar zone | 0.120 | .909 | ||
| Talar lesion size | –0.031 | .301 | ||
| Talar containment | –1.670 | .684 | ||
| Coexisting OCL | 1.816 | .592 | ||
aOriginal model (left), with all parameters included, was evaluated first, which revealed 1 statistically significant parameter: patient sex. The model was reduced to this single parameter (right), where patient sex was significant. An analysis of variance was performed to confirm that reducing the model to include only patient sex accepts the null hypothesis that the other parameter coefficients from the original model are equal to zero. All statistical analyses were performed with R, and P < .05 is considered statistically significant (in bold). FAOS, Foot and Ankle Outcome Score; OCL, osteochondral lesion.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: J.G.K. is a consultant for Arteriocyte Medical Systems and receives support from the Ohnell Family Foundation and Mr. and Mrs. Michael J. Levitt.
Ethical approval for this study was obtained from the Hospital for Special Surgery.
References
- 1. Athanasiou KA, Niederauer GG, Schenck RC. Biomechanical topography of human ankle cartilage. Ann Biomed Eng. 1995;23(5):697–704. [DOI] [PubMed] [Google Scholar]
- 2. Buckwalter JA, Mankin HJ. Articular cartilage: degeneration and osteoarthritis, repair, regeneration, and transplantation. Instr Course Lect. 1998;47:487–504. [PubMed] [Google Scholar]
- 3. Bui-mansfield LT, Kline M, Chew FS, Rogers LF, Lenchik L. Osteochondritis dissecans of the tibial plafond: imaging characteristics and a review of the literature. AJR Am J Roentgenol. 2000;175(5):1305–1308. [DOI] [PubMed] [Google Scholar]
- 4. Choi WJ, Kim BS, Lee JW. Osteochondral lesion of the talus: could age be an indication for arthroscopic treatment? Am J Sports Med. 2012;40(2):419–424. [DOI] [PubMed] [Google Scholar]
- 5. Choi WJ, Park KK, Kim BS, Lee JW. Osteochondral lesion of the talus: is there a critical defect size for poor outcome? Am J Sports Med. 2009;37(10):1974–1980. [DOI] [PubMed] [Google Scholar]
- 6. Chuckpaiwong B, Berkson EM, Theodore GH. Microfracture for osteochondral lesions of the ankle: outcome analysis and outcome predictors of 105 cases. Arthroscopy. 2008;24(1):106–112. [DOI] [PubMed] [Google Scholar]
- 7. Cuttica DJ, Smith WB, Hyer CF, Philbin TM, Berlet GC. Arthroscopic treatment of osteochondral lesions of the tibial plafond. Foot Ankle Int. 2012;33(8):662–668. [DOI] [PubMed] [Google Scholar]
- 8. Cuttica DJ, Smith WB, Hyer CF, Philbin TM, Berlet GC. Osteochondral lesions of the talus: predictors of clinical outcome. Foot Ankle Int. 2011;32(11):1045–1051. [DOI] [PubMed] [Google Scholar]
- 9. Dipaola JD, Nelson DW, Colville MR. Characterizing osteochondral lesions by magnetic resonance imaging. Arthroscopy. 1991;7(1):101–104. [DOI] [PubMed] [Google Scholar]
- 10. Elias I, Raikin SM, Schweitzer ME, Besser MP, Morrison WB, Zoga AC. Osteochondral lesions of the distal tibial plafond: localization and morphologic characteristics with an anatomical grid. Foot Ankle Int. 2009;30(6):524–529. [DOI] [PubMed] [Google Scholar]
- 11. Elias I, Zoga AC, Morrison WB, Besser MP, Schweitzer ME, Raikin SM. Osteochondral lesions of the talus: localization and morphologic data from 424 patients using a novel anatomical grid scheme. Foot Ankle Int. 2007;28(2):154–161. [DOI] [PubMed] [Google Scholar]
- 12. Ellermann JM, Donald B, Rohr S, et al. Magnetic resonance imaging of osteochondritis dissecans: validation study for the ICRS classification system. Acad Radiol. 2016;23(6):724–729. [DOI] [PubMed] [Google Scholar]
- 13. Flick AB, Gould N. Osteochondritis dissecans of the talus (transchondral fractures of the talus): review of the literature and new surgical approach for medial dome lesions. Foot Ankle. 1985;5(4):165–185. [DOI] [PubMed] [Google Scholar]
- 14. Gelber AC, Hochberg MC, Mead LA, Wang NY, Wigley FM, Klag MJ. Joint injury in young adults and risk for subsequent knee and hip osteoarthritis. Ann Intern Med. 2000;133:321–328. [DOI] [PubMed] [Google Scholar]
- 15. Gianakos AL, Hannon CP, Ross KA, et al. Anterolateral tibial osteotomy for accessing osteochondral lesions of the talus in autologous osteochondral transplantation: functional and T2 MRI analysis. Foot Ankle Int. 2015;36(5):531–538. [DOI] [PubMed] [Google Scholar]
- 16. Gobbi A, Francisco RA, Lubowitz JH, Allegra F, Canata G. Osteochondral lesions of the talus: randomized controlled trial comparing chondroplasty, microfracture, and osteochondral autograft transplantation. Arthroscopy. 2006;22(10):1085–1092. [DOI] [PubMed] [Google Scholar]
- 17. Harrington KD. Degenerative arthritis of the ankle secondary to long-standing lateral ligament instability. J Bone Joint Surg Am. 1979;61(3):354–361. [PubMed] [Google Scholar]
- 18. Hembree WC, Wittstein JR, Vinson EN, et al. Magnetic resonance imaging features of osteochondral lesions of the talus. Foot Ankle Int. 2012;33(7):591–597. [DOI] [PubMed] [Google Scholar]
- 19. Kennedy JG, Murawski CD. The treatment of osteochondral lesions of the talus with autologous osteochondral transplantation and bone marrow aspirate concentrate: surgical technique. Cartilage. 2011;2(4):327–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lamb J, Murawski CD, Deyer TW, Kennedy JG. Chevron-type medial malleolar osteotomy: a functional, radiographic and quantitative T2-mapping MRI analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21(6):1283–1288. [DOI] [PubMed] [Google Scholar]
- 21. Lee M, Kwon JW, Choi WJ, Lee JW. Comparison of outcomes for osteochondral lesions of the talus with and without chronic lateral ankle instability. Foot Ankle Int. 2015;36(9):1050–1057. [DOI] [PubMed] [Google Scholar]
- 22. Martin JA, Ellerbroek SM, Buckwalter JA. Age-related decline in chondrocyte response to insulin-like growth factor-I: the role of growth factor binding proteins. J Orthop Res. 1997;15(4):491–498. [DOI] [PubMed] [Google Scholar]
- 23. McCullough CJ, Venugopal V. Osteochondritis dissecans of the talus: the natural history. Clin Orthop Relat Res. 1979;144:264–268. [PubMed] [Google Scholar]
- 24. Mologne TS, Ferkel RD. Arthroscopic treatment of osteochondral lesions of the distal tibia. Foot Ankle Int. 2007;28(8):865–872. [DOI] [PubMed] [Google Scholar]
- 25. Mont MA, Sedlin ED, Weiner LS, Miller AR. Postoperative radiographs as predictors of clinical outcome in unstable ankle fractures. J Orthop Trauma. 1992;6:352–357. [DOI] [PubMed] [Google Scholar]
- 26. Murawski CD, Kennedy JG. Operative treatment of osteochondral lesions of the talus. J Bone Joint Surg Am. 2013;95(11):1045–1054. [DOI] [PubMed] [Google Scholar]
- 27. O’Loughlin PF, Heyworth BE, Kennedy JG. Current concepts in the diagnosis and treatment of osteochondral lesions of the ankle. Am J Sports Med. 2010;38(2):392–404. [DOI] [PubMed] [Google Scholar]
- 28. Phillips WA, Schwartz HS, Keller CS, et al. A prospective, randomized study of the management of severe ankle fractures. J Bone Joint Surg Am. 1985;67:67–78. [PubMed] [Google Scholar]
- 29. Ross KA, Hannon CP, Deyer TW, et al. Functional and MRI outcomes after arthroscopic microfracture for treatment of osteochondral lesions of the distal tibial plafond. J Bone Joint Surg Am. 2014;96(20):1708–1715. [DOI] [PubMed] [Google Scholar]
- 30. Schachter AK, Chen AL, Reddy PD, Tejwani NC. Osteochondral lesions of the talus. J Am Acad Orthop Surg. 2005;13(3):152–158. [DOI] [PubMed] [Google Scholar]
- 31. Smyth NA, Murawski CD, Haleem AM, Hannon CP, Savage-Elliott I, Kennedy JG. Establishing proof of concept: platelet-rich plasma and bone marrow aspirate concentrate may improve cartilage repair following surgical treatment for osteochondral lesions of the talus. World J Orthop. 2012;3(7):101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Taga I, Shino K, Inoue M, Nakata K, Maeda A. Articular cartilage lesions in ankles with lateral ligament injury: an arthroscopic study. Am J Sports Med. 1993;21(1):120–127. [DOI] [PubMed] [Google Scholar]
- 33. Van Bergen CJ, De leeuw PA, Van dijk CN. Treatment of osteochondral defects of the talus. Rev Chir Orthop Reparatrice Appar Mot. 2008;94(suppl 8):398–408. [DOI] [PubMed] [Google Scholar]
- 34. Van Bergen CJ, Kox LS, Maas M, Sierevelt IN, Kerkhoffs GM, Van dijk CN. Arthroscopic treatment of osteochondral defects of the talus: outcomes at eight to twenty years of follow-up. J Bone Joint Surg Am. 2013;95(6):519–525. [DOI] [PubMed] [Google Scholar]
- 35. Van Dijk CN, Bossuyt PM, Marti RK. Medial ankle pain after lateral ligament rupture. J Bone Joint Surg Br. 1996;78(4):562–567. [PubMed] [Google Scholar]
- 36. Van Dijk CN, Reilingh ML, Zengerink M, van Bergen CJ. The natural history of osteochondral lesions in the ankle. Instr Course Lect. 2010;59:375–386. [PubMed] [Google Scholar]
- 37. Yasui Y, Wollstein A, Murawski CD, Kennedy JG. Operative treatment for osteochondral lesions of the talus: biologics and scaffold-based therapy. Cartilage. 2017;8(1):42–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. You JY, Lee GY, Lee JW, Lee E, Kang HS. An osteochondral lesion of the distal tibia and fibula in patients with an osteochondral lesion of the talus on MRI: prevalence, location, and concomitant ligament and tendon injuries. AJR Am J Roentgenol. 2016;206(2):366–372. [DOI] [PubMed] [Google Scholar]