Keywords: nerve regeneration, intracerebral hemorrhage, acupuncture, Baihui (DU20), Qubin (GB7), inflammation, Mincle/Syk signaling pathway, nerve protection, neural regeneration
Abstract
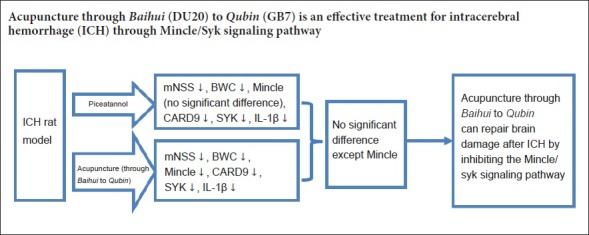
Inflammation plays an important role in nerve defects caused by intracerebral hemorrhage. Repairing brain damage by inhibiting the macrophage-inducible C-type lectin/spleen tyrosine kinase (Mincle/Syk) signaling pathway is a potential new target for treating cerebral hemorrhage. In this study, we aimed to determine whether acupuncture through Baihui (DU20) to Qubin (GB7) is an effective treatment for intracerebral hemorrhage through the Mincle/Syk signaling pathway. An intracerebral hemorrhage rat model was established by autologous blood infusion into the caudate nucleus. Acupuncture through Baihui to Qubin was performed for 30 minutes, once every 12 hours, for a total of three times. Piceatannol (34.62 mg/kg), a Syk inhibitor, was intraperitoneally injected as a control. Modified neurological severity score was used to assess neurological function. Brain water content was measured. Immunohistochemistry and western blot assay were used to detect immunoreactivity and protein expression levels of Mincle, Syk, and CARD9. Real-time polymerase chain reaction was used to determine interleukin-1β mRNA levels. Hematoxylin-eosin staining was performed to observe histopathological changes. Our results showed that acupuncture through Baihui to Qubin remarkably improved neurological function and brain water content, and inhibited immunoreactivity and expression of Mincle, Syk, CARD9, and interkeukin-1β. Moreover, this effect was similar to piceatannol. These findings suggest that acupuncture through Baihui to Qubin can improve neurological impairment after cerebral hemorrhage by inhibiting the Mincle/Syk signaling pathway.
Introduction
Approximately 2 million individuals worldwide are diagnosed with intracerebral hemorrhage (ICH) each year (Sudlow and Warlow, 1997; Broderick et al., 2007; Lloyd-Jones et al., 2009; Qureshi et al., 2009). Furthermore, ICH is one of the most fatal types of stroke, and results in severe mental dysfunction generated by secondary nerve damage in patients who survive the primary stroke (Aronowski and Zhao, 2011). Current therapies for ICH have a poor impact on prognosis (Mayer and Rincon, 2005; Keep et al., 2012). Cytotoxicity, oxidative stress, and especially, inflammation play key roles in secondary injury after ICH (Keep et al., 2012; Zhou et al., 2014). Consequently, regulation of inflammation after ICH may provide insight for future ICH therapies (Zhao et al., 2007).
Acupuncture is one of the most important components of traditional Chinese medicine and widely used in the treatment of various diseases (Lou et al., 2016). Moreover, its curative effect has been widely recognized and accepted worldwide (Meng et al., 2011; Liu et al., 2016, 2017) by the international medical community. Our previous study revealed that acupuncture through Baihui (DU20) to Qubin (GB7) has a “reparative” function by inducing expression of endogenous glial cell line-derived neurotrophic factor during acute cerebral hemorrhage (Zhang et al., 2012). More specifically, acupuncture can improve recovery of neural stem cells by suppressing expression of both Notch1 and Hes1 (Zou et al., 2015). Acupuncture can also antagonize inflammatory brain injury generated by cerebral hemorrhage by suppressing the classical nuclear factor-κB pathway (Liu et al., 2017). Thus, acupuncture is an effective means of lowering expression of inflammatory mediators in the nervous system. Furthermore, according to current reports, acupuncture has greatly contributed to reducing the rate of stroke-induced disability and improving recovery of neural function. Studies investigating acupuncture have found that it is a highly potent therapy for reducing neural inflammation (Liu et al., 2016), suppressing cell apoptosis, and alleviating nerve dysfunction (Ma et al., 2016) after stroke. Altogether, these studies show that acupuncture has great potential for treating cerebral hemorrhage by inhibiting inflammation.
The immune system plays an important role in the inflammatory response. Compared with the adaptive immune system (which is highly pathogen specific), innate immune receptors recognize a variety of pathogens with similar structures (Park et al., 2006; Tang et al., 2007; Shichita et al., 2012). Toll-like receptors are a classical example of innate immune receptors, and are a “hot topic” of research because of their participation in inflammation induced by neural system disease, including ischemic stroke and cerebral hemorrhage (Fadakar et al., 2014; Lan et al., 2017). Macrophage-inducible C-type lectin (Mincle) is a recently discovered innate immune receptor that was originally recognized as a macrophage target in the peritoneum (Matsumoto et al., 1999). Toll-like receptors recognize ligands expressed on necrotic cells, and interact with downstream spleen tyrosine kinase (Syk) to active a pathway that can induce generation of several inflammatory cytokines, including interleukin (IL)-1β (Brown, 2008). The Mincle/Syk pathway plays a role in traumatic brain injury (de Rivero Vaccari et al., 2015), subarachnoid hemorrhage, and ischemic stroke (Suzuki et al., 2013; He et al., 2015; Xie et al., 2017). However, the regulatory mechanism of the Mincle/Syk pathway in cerebral hemorrhage remains unclear. Furthermore, it is also not known whether acupuncture can treat cerebral hemorrhage by regulating the Mincle/Syk pathway.
In this study, we first used an autohemic blood infusion method to establish a rat model of cerebral hemorrhage for studying the effectiveness of acupuncture through Baihui to Qubin. We then determined the therapeutic mechanism of acupuncture through the Mincle/Syk pathway.
Materials and Methods
Animals
A total of 312 male specific pathogen-free Sprague-Dawley rats, aged 8 weeks and weighing 280–320 g, were purchased from the Laboratory Animal Center, Heilongjiang University of Chinese Medicine, China (license No. SYXK (Hei) 2016-015). All experiments were approved by the Animal Care and Use Committee of Heilongjiang University of Chinese Medicine of China (approval No. 2016-09-02-01). Animal care and experimental procedures were performed in accordance with the United State National Institutes of Health Guide for the Care and Use of Laboratory Animals (publication No. 85–23, revised 1985). All surgeries were performed under pentobarbital anesthesia, and all efforts were made to minimize suffering. Rats were housed under a 12-hour light/dark cycle at 21 ± 2°C and 50 ± 5% relative humidity, with unlimited access to standard food and water. Rats were randomly divided into four groups: sham (n = 72), intracerebral hemorrhage (ICH) (n = 72), piceatannol (a Syk inhibitor) (n = 72), and acupuncture (n = 72). All groups were evenly divided into four subgroups (n = 18 each), which were assessed at 6, 12, 24, and 72 hours after treatment.
Establishment of a cerebral hemorrhage rat model
Rats were anesthetized with pentobarbital (60 mg/kg; intraperitoneally) (Royalton, Dalian, China), and fixed on a stereotactic frame (STW-3X; Chengdu Instrument Factory, Chengdu, China). Bregma and the coronal sulcus were exposed by cutting the scalp midline. A dental drill was used at the interchange of 0.2 mm behind and 3.5 mm right from bregma. Drilling was performed to a diameter of 1 mm until the meninges was reached. Autologous tail tip blood was injected into the caudate nucleus (20 μL/min) (anteroposterior: −0.24 mm, lateral: 3.5 mm, dorsal: 6 mm) (right side is the injury side) (Paxinos and Watson, 2007). The microsyringe was exited from the caudate–putamen after 5 minutes. The wound was filled using dental cement, and subsequently stitched, bandaged, and sterilized (Liu et al., 2017). According to Berderson's scale (Bederson et al., 1986), the model was successful if the score was 1 to 3 at 2 hours after modeling.
Operations for sham models were identical except for blood injection.
Treatment
After successful model establishment, in the acupuncture group, Baihui (DU20) (specific location: head between the middle ears) and Qubin (GB7) (specific location: leading edge of ear root) points were identified (Li, 2007). Hair was cut around the Baihui (DU20) point, and a 0.30 × 25 mm acupuncture needle (Hua Tuo Brand; Suzhou Medical Appliance, Suzhou, China) used to pierce from the epicranial aponeurosis to the Qubin (GB7) point in the bottom right direction. The needle pierced to a depth of 15 mm, and was then rotated at 200 r/min for 5 minutes. For each 30-minute session, needling at 200 r/min was performed for three session, each lasting for 5 minutes.
In the sham and ICH groups, rats were fixed on the frame for 30 minutes without any operation.
In the piceatannol group, rats were intraperitoneally injected with piceatannol (34.62 mg/kg) (license No. 10083-24-6; Selleck, Shanghai, China) at 1 hour after model establishment.
Modified neurological severity score (mNSS)
The mNSS was analyzed at 6, 12, 24, 72, and 168 hours after model establishment (Lei et al., 2015). Higher scores indicate poorer neurological function. More detailed information is provided in Additional file 1 (341.2KB, tif) .
Brain water content (BWC)
Brains were obtained by decapitation at 6, 12, 24, and 72 hours after treatment in each subgroup. Left and right hemispheres were separated. Wet weight was weighed. Dry weight was weighed after a 72-hour incubation in a drying cabinet (Binder, Germany) at 105°C. BWC was calculated by: wet weight – dry weight) / wet weight × 100%.
Histopathological assay
Brain tissue of rats in each group was collected at 72 hours after surgery, perfused with 4% paraformaldehyde, and cut into 4-μm slices for routine hematoxylin and eosin staining to observe organizational structure. Images were captured using an optical microscope (Leica, Germany) at 200× magnification.
Immunohistochemistry
Rats were treated with pentobarbital (60 mg/kg) by intraperitoneal injection, followed by perfusion fixation with 4% paraformaldehyde. Brain tissue was obtained after decapitation, and fixed in paraformaldehyde following dehydration. After paraffin embedding and histological sectioning (5 μm), sections were incubated with primary antibodies, namely rabbit anti-Mincle (1:500; Bioss, Beijing, China), rabbit anti-Syk (1:500; Bioss), and rabbit anti-caspase recruitment domain family member 9 (CARD9) (1:500; Abcam, Cambridge, UK) overnight at 4°C. Sections were then incubated with goat anti-rabbit IgG (1:2000; Abcam) as a secondary antibody at 37°C for 30 minutes. Images were captured using a microscope imaging system (Moticam 3000; Motic, Hong Kong Special Administrative Region, China). Each sample was examined in captured images from five non-overlapping visual fields under a 400× magnification. Average number of positive cells was calculated (Xue et al., 2014).
Western blot assay
The right hemisphere of rats at 6, 12, 24, and 72 hours after ICH was lysed, with protein samples isolated and collected. Fifty micrograms (50 μg) of sample was loaded onto a sodium dodecyl polyacrylamide gel and transferred to a polyvinylidene difluoride membrane. The membrane was then blocked using 5% non-fat dry milk, and subsequently incubated with primary antibody overnight at 4°C, followed by secondary antibody at room temperature for 2 hours. Rabbit anti-Mincle (1:1000; Bioss), rabbit anti-Syk (1:1000; Bioss), rabbit anti-CARD9 (1:1000; Abcam), and rabbit anti-β-actin (1:1000; Bioss) were used as primary antibodies. Goat anti-rabbit IgG (1:2000; Abcam) was used as the secondary antibody. Protein signal was marked using a commercially available 3, 3′-diaminobenzidine (DAB) electrochemiluminescence system (Beyotime, Jiangsu, China), and images captured (Duris et al., 2011). Optical density values for specific bands were measured using ImageJ software (NIH, Bethesda, MD, USA).
Real-time polymerase chain reaction (PCR)
RNA was extracted from the brain using a commercially available kit (RNAiso Plus; Takara Bio Inc., Dalian, China), according to the manufacturer's instructions. Complementary DNA (cDNA) was reverse transcribed using the Prime Script II 1st Strand cDNA Synthesis Kit (Takara Bio Inc.). The reverse transcription conditions were: 42°C for 60 minutes, 95°C for 5 minutes, and then storage on ice. The primers used were: β-actin-forward, 5′-AAC ACC CCA GCC ATG TAC GTA-3′; β-actin-reverse, 5′-TGG CCA TCT CTT GCT CGA A-3′; IL-1β-forward, 5′-AAG GGG ACA TTA GGC AGC AC-3′; and IL-1β-reverse, 5′-ATG AAA GAC CTC AGT GCG GG-3′. Real-time PCR was performed using the SYBR Premix Ex Taq kit (Takara Bio Inc.). The PCR conditions were: 95°C for 30 seconds, 95°C for 5 seconds, and 60°C for 34 seconds for 40 cycles, with reactions held at 4°C. IL-1β mRNA was calculated by the 2-ΔΔCt method (Xie et al., 2017).
Statistical analysis
Data are represented as mean ± SD for mNSS, western blotting, and as median (interquartile range) for BWC, immunohistochemistry, and real-time PCR. All analyses were performed using Graph Pad Prism 6 software (GraphPad, San Diego, CA, USA). P values for mNSS and western blotting were determined by one-way analysis of variance followed by Tukey's post hoc test. BWC, immunohistochemistry and real-time PCR were examined using the Kruskal-Wallis test followed by Mann-Whitney U test for pairwise comparisons. A value of P < 0.05 was considered statistically significant.
Results
Effect of acupuncture on neural function after ICH
No significant differences in mNSS were detectable among subgroups (6, 12, 24, 72, and 168 hours) in the sham group (P > 0.05). Compared with the sham group, mNSS score was significantly increased in the ICH group (P < 0.01). mNSS was significantly lower in the acupuncture and piceatannol groups compared with the ICH group (P < 0.01). No significant differences were observed in mNSS score between the acupuncture and piceatannol groups (P > 0.05; Figure 1).
Figure 1.
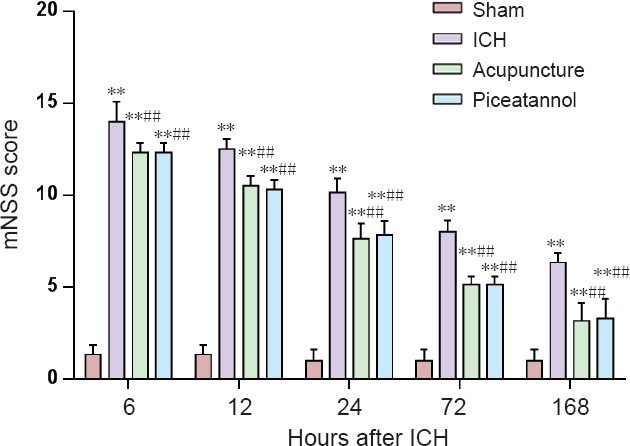
Effect of acupuncture through Baihui (DU20) to Qubin (GB7) on mNSS in a rat model of intracerebral hemorrhage.
Data are expressed as the mean ± SD (n = 6; one-way analysis of variance followed by Tukey's post hoc test). **P < 0.01, vs. sham group; ##P < 0.01, vs. ICH group. mNSS: Modified neurological severity score; ICH: intracerebral hemorrhage.
Effect of acupuncture on BWC after ICH
BWC was relatively minor in the sham group (Figure 2). However, compared with the sham group, BWC was significantly increased in the ICH group (P < 0.05). BWC was significantly lower in the acupuncture and piceatannol groups compared with the ICH group (P < 0.05). No significant difference in BWC was observed between the acupuncture and piceatannol groups (P > 0.05; Figure 2).
Figure 2.
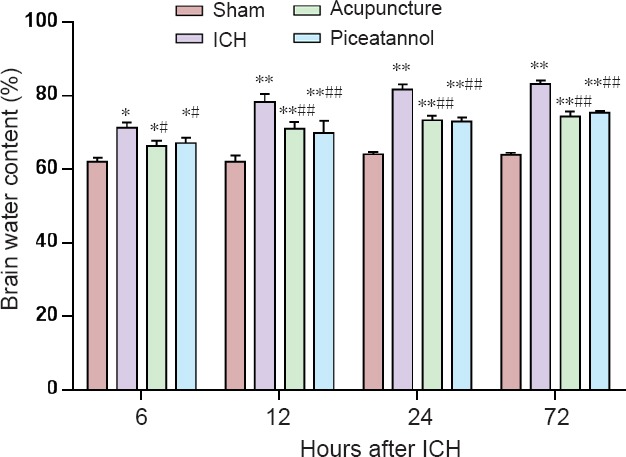
Effect of acupuncture through Baihui (DU20) to Qubin (GB7) on brain water content in a rat model of intracerebral hemorrhage.
Brain water content = wet weight – dry weight / wet weight × 100%. Data are expressed as the mean ± SD (n = 6; Kruskal-Wallis test followed by Mann-Whitney U test). *P < 0.05, **P < 0.01, vs. sham group; #P < 0.05, ##P < 0.01, vs. ICH group. ICH: Intracerebral hemorrhage. The primary data of Figure 2 are expressed in Additional file 2 (521KB, tif) .
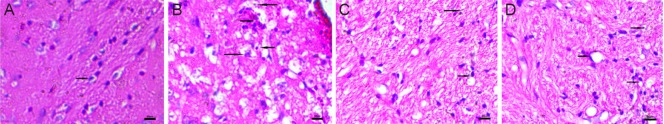
Effect of acupuncture on brain histopathology after ICH
Hematoxylin and eosin staining was performed to examine histological changes 72 hours after ICH (Figure 3). Rats receiving sham surgery had no blood injection into the brain and showed normal microscopic features, with no inflammatory infiltration from the semi-dark area. However, the ICH group showed intracranial blood injection, tissue edema, partial nerve cell necrosis, glial cell swelling, intracellular vacuoles, and inflammatory cell infiltration. Furthermore, in rats receiving acupuncture or piceatannol treatment after blood injection, the pathological features were less severe.
Figure 3.
Effect of acupuncture through Baihui (DU20) to Qubin (GB7) on brain histopathology of rats after intracerebral hemorrhage (hematoxylin and eosin staining, original magnification, 200×).
(A) Sham group; (B) ICH group; (C) piceatannol group; (D) acupuncture group. Rats in the sham group had no blood injection into the brain, and showed no inflammatory infiltration (arrows) from the semi-dark area and normal microscopic features. Pathological features (arrows) in the ICH group were intracranial blood injection, tissue edema, partial nerve cell necrosis, glial cell swelling, intracellular vacuoles, and inflammatory cell infiltration. Pathological features (arrows) were less severe in rats receiving acupuncture or piceatannol treatment after blood injection. ICH: Intracerebral hemorrhage.
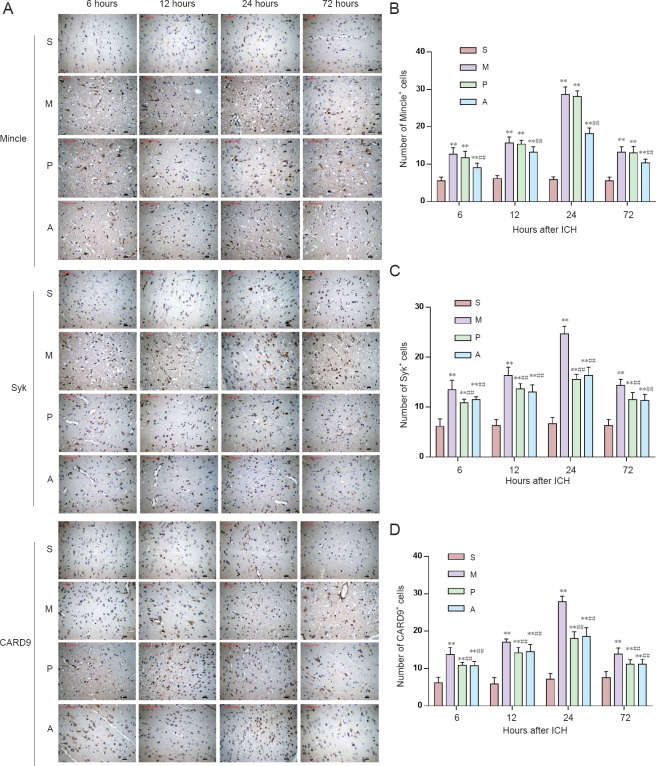
Effect of acupuncture on the Mincle/Syk pathway in rats with ICH
Immunopositivity of Mincle, Syk, and CARD9 in the brain as detected by immunohistochemistry
Immunopositivity of Syk and CARD9 were significantly reduced in the acupuncture and piceatannol groups compared with the ICH group (P < 0.05). Immunopositivity of Syk and CARD9 showed no statistical differences between the acupuncture and piceatannol groups (P > 0.05). Compared with the ICH group, Mincle immunopositivity was decreased in the acupuncture group (P < 0.05). However, Mincle immunopositivity was not significantly different between the ICH and piceatannol groups (P > 0.05; Figure 4).
Figure 4.
Effect of acupuncture through Baihui (DU20) to Qubin (GB7) on immunoreactivity of Mincle, Syk, and CARD9 in the brain of rats at 6, 12, 24, and 72 hours after intracerebral hemorrhage (immunohistochemistry).
(A) Immunohistochemical staining of brain tissue (original magnification, 400×). Positive cells are indicated by arrows. Scale bars: 50 μm. (B–D) Number of Mincle+, Syk+, and CARD9+ cells in 400-fold fields, respectively. Data are presented as the mean ± SD (n = 6; Kruskal-Wallis test followed by Mann-Whitney U test). *P < 0.05, vs. sham group; #P < 0.05, vs. ICH group. S: Sham group; M: model group; P: piceatannol group; A: acupuncture group; ICH: intracerebral hemorrhage.
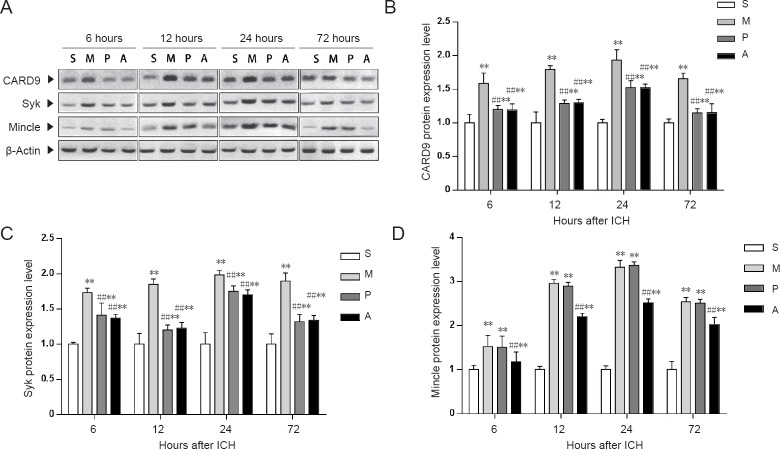
Protein expression of Mincle, Syk, and CARD9 in the brain as detected by western blot assay
Expression levels of Syk and CARD9 were significantly reduced in the acupuncture and piceatannol groups compared with the ICH group (P < 0.01). There were no statistically significant differences in Syk and CARD9 expression levels between the acupuncture and piceatannol groups (P > 0.05). Compared with the ICH group, Mincle expression levels were significantly decreased in the acupuncture group (P < 0.01). However, Mincle expression levels were not significantly different between the ICH and piceatannol groups (P > 0.05; Figure 5.
Figure 5.
Effect of acupuncture through Baihui (DU20) to Qubin (GB7) on protein expression of CARD9, Syk, and Mincle in the brain of rats at 6, 12, 24, and 72 hours after intracerebral hemorrhage (western blot assay).
(A) Western immunoblotting analysis of proteins relevant to intracerebral hemorrhage in rats. Protein levels were normalized to β-actin as a loading control. (B–D) Quantitative analysis of protein expression levels of CARD9, Syk, and Mincle, respectively. Data are presented as the mean ± SD (n = 6; one-way analysis of variance followed by Tukey's post hoc test); **P < 0.01, vs. sham group; ##P < 0.01, vs. ICH group. S: Sham group; M: model group; P: piceatannol group; A: acupuncture group; ICH: intracerebral hemorrhage; Mincle: macrophage-inducible C-type lectin; Syk: spleen tyrosine kinase.
IL-1β mRNA expression in the brain as detected by real-time PCR
IL-1β mRNA levels were significantly increased in the ICH group compared with the sham group (P < 0.01). Compared with the ICH group, expression levels of IL-1β mRNA were significantly decreased in the acupuncture and piceatannol groups (P < 0.01). However, expression levels of IL-1β mRNA were not different between the acupuncture and piceatannol groups (P > 0.05; Figure 6).
Figure 6.
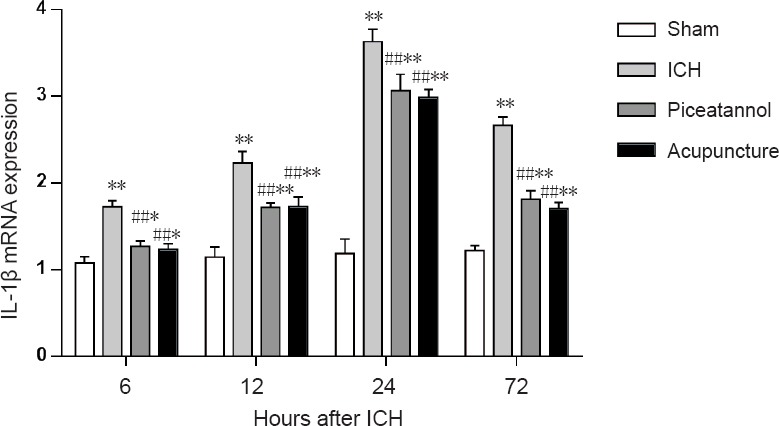
Effect of acupuncture through Baihui (DU20) to Qubin (GB7) on mRNA expression of IL-1β at 6, 12, 24, and 72 hours in the brain of rats after intracerebral hemorrhage.
Relative mRNA expression of IL-1β was determined by real-time polymerase chain reaction. Data are presented as the mean ± SD (n = 6; Kruskal-Wallis test followed by Mann-Whitney U test). *P < 0.05, **P < 0.01, vs. sham group; #P < 0.05, ##P < 0.01, vs. ICH group. ICH: Intracerebral hemorrhage; IL: interleukin.
Discussion
Peripheral tissues are exposed to a massive amount of blood after ICH, which in turn provokes a variety of cellular and molecular effects. Activation of cells and inflammation can trigger infiltration of polymorphonuclear leukocytes and monocytes, activation of microglia, damage to the blood-brain barrier, and development of brain edema, which contributes to secondary brain injury (Aronowski and Hall, 2005; Wang and Dore, 2007). Meanwhile, previous studies have shown that acupuncture can reduce neural inflammation (Liu et al., 2016), suppress cell apoptosis, and alleviate nerve dysfunction (Ma et al., 2016) after stroke, but it remains unclear whether acupuncture is effective for treating cerebral hemorrhage. Consequently, in this study, we first examined the protective effects of acupuncture through Baihui (DU20) to Qubin (GB7) in a cerebral hemorrhage animal model. We then further investigated the effect of acupuncture on inflammation and its protective mechanism. Our results indicate that acupuncture could be an excellent tool for ICH therapy.
As already described, inflammation plays an important role in ICH (Tang et al., 2017). Inflammation leads to cell swelling and damage, which in turn induces brain edema. Inflammation, clotting, and erythrocyte lysis caused by primary injury can result in brain edema, which is associated with poor recovery from injury and may lead to more severe and prolonged brain injury (Zheng et al., 2016). Thus, decreasing brain edema is critical for protecting neurovascular structures. Acupuncture is one of the most important components of traditional Chinese medicine, and has greatly contributed to reducing the rate of stroke-induced disability and improving recovery of neural function. Our results show that acupuncture through Baihui (DU20) to Qubin (GB7) can decrease mNSS and reduce BWC in a cerebral hemorrhage animal model. Moreover, hematoxylin-eosin staining showed that acupuncture through Baihui (DU20) to Qubin (GB7) also decreased capillary permeability and leakage. Our data are consistent with other similar studies (Liu et al., 2017).
The innate immune system is critical in development of neurovascular injury and a major reason for excessive parenchymatous inflammation. Fang et al., (2013) found that both innate immunity and inflammation participate in the pathological process of ICH. Necrosis of leukocytes can induce microglial cells and macrophages to release proinflammatory cytokines, thereby leading to further brain injury (Wang and Dore, 2007). Animal experiments have shown that factors inhibiting microglia/macrophages can remarkably reduce brain injury and improve neural function in rodents (Zhao et al., 2011).
Mincle is a pattern-recognition receptor primarily expressed in myeloid cells, especially antigen-presenting cells. It is also expressed on the surface of B cells, microglia, neurons, and mast cells (Flornes et al., 2004; McKimmie et al., 2006; Ribbing et al., 2011; Kawata et al., 2012; He et al., 2015). Mincle expression is low under normal circumstances. During infection and tissue damage, Mincle is upregulated and binds to endogenous antigens, leading to recruitment and activation of Syk. Syk can activate protein kinase C-δ, which phosphorylates downstream CARD9. This activates the nuclear factor-κB pathway via CARD9/B-cell lymphoma/leukemia 10 (BCL 10), which ultimately generates biologically active IL-1β (Takizawa et al., 2001; Strasser et al., 2012; Yasukawa et al., 2014). As a mediator of the immune response and activation point of inflammation, IL-1β expression levels directly reflect grades of inflammation after cerebral hemorrhage (Gross et al., 2009). Previous studies have shown that the Mincle/Syk signaling pathway is involved in many innate immune responses including ischemic stroke, traumatic brain injury, and subarachnoid hemorrhage (Suzuki et al., 2013; de Rivero Vaccari et al., 2015; He et al., 2015; Arumugam et al., 2017; Xie et al., 2017). Our study found that acupuncture markedly suppressed protein expression in the Mincle/Syk pathway and decreased IL-1β expression in rat brain tissue following hemorrhage. These results suggest that acupuncture through Baihui (DU20) to Qubin (GB7) may mitigate cerebral hemorrhage injury neuritis and improve neural function by suppressing the Mincle/Syk pathway, which further downregulates expression levels of downstream inflammatory cytokines.
Piceatannol, a Syk inhibitor, suppresses Syk/CARD9 expression during ischemic stroke and subarachnoid hemorrhage, reduces IL-1β levels, improves neural function, and facilitates brain edema therapy (Suzuki et al., 2013; He et al., 2015; Xie et al., 2017). Our study found no significant differences in the effects of therapy in rats treated with acupuncture compared with the piceatannol group. This further suggests that acupuncture through Baihui (DU20) to Qubin (GB7) can in fact affect the Mincle/Syk pathway, mitigate inflammatory brain injury, improve neural function, and alleviate brain edema.
Our study has a few limitations. First, we have searched relevant literature within and outside China, but reports on the Mincle/Syk signaling pathway are still limited. The mechanism by which blocking Mincle improves ICH outcome needs further investigation. Second, we did not examine changes of Mincle/Syk between different time points after ICH as the purpose of our study was to determine whether the therapeutic effect of acupuncture was significant compared with the other experimental groups at the same time point. Third, connections between Mincle and other signaling pathways after ICH requires further studies.
In summary, acupuncture through Baihui (DU20) to Qubin (GB7) may suppress the Mincle/Syk pathway and reduce the release of proinflammatory cytokines, thereby mitigating neurological damage after cerebral hemorrhage.
Additional files:
Additional file 1 (341.2KB, tif) : Modified neurological severity score points.
Modified neurological severity score points
Additional file 2 (521KB, tif) : The primary data of Figure 2.
The primary data of Figure 2
Footnotes
Conflicts of interest: None declared.
Financial support: This study was supported by the National Natural Science Foundation of China, No. 81473764, No. 81273824; the Key Project of Natural Science Foundation of Heilongjiang Province of China, No. ZD201204; the Doctoral Fund Program of Ministry of Education of China, No. 20102327110003. All authors declare that financial support does not affect the opinion of the article and the objective statistical analysis and report of the research results in this study.
Institutional review board statement: All experiments were approved by the Animal Care and Use Committee of Heilongjiang University of Chinese Medicine of China (approval No. 2016-09-02-01). Animal care and experimental procedures were performed in accordance with the United State National Institutes of Health Guide for the Care and Use of Laboratory Animals (publication No. 85-23, revised 1985).
Copyright license agreement: The Copyright License Agreement has been signed by all authors before publication.
Data sharing statement: Datasets analyzed during the current study are available from the corresponding author on reasonable request.
Plagiarism check: Checked twice by iThenticate.
Peer review: Externally peer reviewed.
Open peer reviewer: Clarissa Cavarsan, Universidade Federal do Paraná, Brazil.
Funding: This study was supported by the National Natural Science Foundation of China, No. 81473764, 81273824; the Key Project of Natural Science Foundation of Heilongjiang Province of China, No. ZD201204; the Doctoral Fund Program of Ministry of Education of China, No. 20102327110003.
(Copyedited by Yu J, Li CH, Qiu Y, Song LP, Zhao M)
References
- Aronowski J, Hall CE. New horizons for primary intracerebral hemorrhage treatment: experience from preclinical studies. Neurol Res. 2005;27:268–279. doi: 10.1179/016164105X25225. [DOI] [PubMed] [Google Scholar]
- Aronowski J, Zhao X. Molecular pathophysiology of cerebral hemorrhage: secondary brain injury. Stroke. 2011;42:1781–1786. doi: 10.1161/STROKEAHA.110.596718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arumugam TV, Manzanero S, Furtado M, Biggins PJ, Hsieh YH, Gelderblom M, MacDonald KP, Salimova E, Li YI, Korn O, Dewar D, Macrae IM, Ashman RB, Tang SC, Rosenthal NA, Ruitenberg MJ, Magnus T, Wells CA. An atypical role for the myeloid receptor Mincle in central nervous system injury. J Cereb Blood Flow Metab. 2017;37:2098–2111. doi: 10.1177/0271678X16661201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bederson JB, Pitts LH, Tsuji M, Nishimura MC, Davis RL, Bartkowski H. Rat middle cerebral artery occlusion: evaluation of the model and development of a neurologic examination. Stroke. 1986;17:472–476. doi: 10.1161/01.str.17.3.472. [DOI] [PubMed] [Google Scholar]
- Broderick J, Connolly S, Feldmann E, Hanley D, Kase C, Krieger D, Mayberg M, Morgenstern L, Ogilvy CS, Vespa P, Zuccarello M, American Heart Association/American Stroke Association Stroke Council; American Heart Association/American Stroke Association High Blood Pressure Research Council; Quality of Care and Outcomes in Research Interdisciplinary Working Group Guidelines for the management of spontaneous intracerebral hemorrhage in adults: 2007 update: a guideline from the American Heart Association/American Stroke Association Stroke Council, High Blood Pressure Research Council, and the Quality of Care and Outcomes in Research Interdisciplinary Working Group. Circulation. 2007;116:e391–413. doi: 10.1161/CIRCULATIONAHA.107.183689. [DOI] [PubMed] [Google Scholar]
- Brown GD. Sensing necrosis with Mincle. Nat Immunol. 2008;9:1099–1100. doi: 10.1038/ni1008-1099. [DOI] [PubMed] [Google Scholar]
- de Rivero Vaccari JC, Brand FJ, 3rd, Berti AF, Alonso OF, Bullock MR, de Rivero Vaccari JP. Mincle signaling in the innate immune response after traumatic brain injury. J Neurotrauma. 2015;32:228–236. doi: 10.1089/neu.2014.3436. [DOI] [PubMed] [Google Scholar]
- Duris K, Manaenko A, Suzuki H, Rolland WB, Krafft PR, Zhang JH. alpha7 nicotinic acetylcholine receptor agonist PNU-282987 attenuates early brain injury in a perforation model of subarachnoid hemorrhage in rats. Stroke. 2011;42:3530–3536. doi: 10.1161/STROKEAHA.111.619965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fadakar K, Dadkhahfar S, Esmaeili A, Rezaei N. The role of Toll-like receptors (TLRs) in stroke. Rev Neurosci. 2014;25:699–712. doi: 10.1515/revneuro-2013-0069. [DOI] [PubMed] [Google Scholar]
- Fang H, Wang PF, Zhou Y, Wang YC, Yang QW. Toll-like receptor 4 signaling in intracerebral hemorrhage-induced inflammation and injury. J Neuroinflammation. 2013;10:27. doi: 10.1186/1742-2094-10-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flornes LM, Bryceson YT, Spurkland A, Lorentzen JC, Dissen E, Fossum S. Identification of lectin-like receptors expressed by antigen presenting cells and neutrophils and their mapping to a novel gene complex. Immunogenetics. 2004;56:506–517. doi: 10.1007/s00251-004-0714-x. [DOI] [PubMed] [Google Scholar]
- Gross O, Poeck H, Bscheider M, Dostert C, Hannesschlager N, Endres S, Hartmann G, Tardivel A, Schweighoffer E, Tybulewicz V, Mocsai A, Tschopp J, Ruland J. Syk kinase signalling couples to the Nlrp3 inflammasome for anti-fungal host defence. Nature. 2009;459:433–436. doi: 10.1038/nature07965. [DOI] [PubMed] [Google Scholar]
- He Y, Xu L, Li B, Guo ZN, Hu Q, Guo Z, Tang J, Chen Y, Zhang Y, Tang J, Zhang JH. Macrophage-inducible C-type Lectin/Spleen tyrosine kinase signaling pathway contributes to neuroinflammation after subarachnoid hemorrhage in rats. Stroke. 2015;46:2277–2286. doi: 10.1161/STROKEAHA.115.010088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawata K, Illarionov P, Yang GX, Kenny TP, Zhang W, Tsuda M, Ando Y, Leung PS, Ansari AA, Gershwin ME. Mincle and human B cell function. J Autoimmun. 2012;39:315–322. doi: 10.1016/j.jaut.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keep RF, Hua Y, Xi G. Intracerebral haemorrhage: mechanisms of injury and therapeutic targets. Lancet Neurol. 2012;11:720–731. doi: 10.1016/S1474-4422(12)70104-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lan X, Han X, Li Q, Li Q, Gao Y, Cheng T, Wan J, Zhu W, Wang J. Pinocembrin protects hemorrhagic brain primarily by inhibiting toll-like receptor 4 and reducing M1 phenotype microglia. Brain Behav Immun. 2017;61:326–339. doi: 10.1016/j.bbi.2016.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lei C, Wu B, Cao T, Zhang S, Liu M. Activation of the high-mobility group box 1 protein-receptor for advanced glycation end-products signaling pathway in rats during neurogenesis after intracerebral hemorrhage. Stroke. 2015;46:500–506. doi: 10.1161/STROKEAHA.114.006825. [DOI] [PubMed] [Google Scholar]
- Li Z. Beijing: China Press of Traditional Chinese Medicine; 2007. Experimental Acupuncture Science. [Google Scholar]
- Liu H, Sun X, Zou W, Leng M, Zhang B, Kang X, He T, Wang H. Scalp acupuncture attenuates neurological deficits in a rat model of hemorrhagic stroke. Complement Ther Med. 2017;32:85–90. doi: 10.1016/j.ctim.2017.03.014. [DOI] [PubMed] [Google Scholar]
- Liu W, Wang X, Yang S, Huang J, Xue X, Zheng Y, Shang G, Tao J, Chen L. Electroacupunctre improves motor impairment via inhibition of microglia-mediated neuroinflammation in the sensorimotor cortex after ischemic stroke. Life Sci. 2016;151:313–322. doi: 10.1016/j.lfs.2016.01.045. [DOI] [PubMed] [Google Scholar]
- Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, Ford E, Furie K, Go A, Greenlund K, Haase N, Hailpern S, Ho M, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott M, et al. Heart disease and stroke statistics--2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009;119:480–486. doi: 10.1161/CIRCULATIONAHA.108.191259. [DOI] [PubMed] [Google Scholar]
- Lou YJ, Liu Y, Shan HJ, Cao CH, Jie XS. Effect of acupuncture of “Xingnao Kaiqiao” on the behavior of an immature rat model of cerebral palsy and the underlying mechanism. Zhongguo Zuzhi Gongcheng Yanjiu. 2016;20:7314–7319. [Google Scholar]
- Ma R, Yuan B, Du J, Wang L, Ma L, Liu S, Shu Q, Sun H. Electroacupuncture alleviates nerve injury after cerebra ischemia in rats through inhibiting cell apoptosis and changing the balance of MMP-9/TIMP-1 expression. Neurosci Lett. 2016;633:158–164. doi: 10.1016/j.neulet.2016.09.033. [DOI] [PubMed] [Google Scholar]
- Matsumoto M, Tanaka T, Kaisho T, Sanjo H, Copeland NG, Gilbert DJ, Jenkins NA, Akira S. A novel LPS-inducible C-type lectin is a transcriptional target of NF-IL6 in macrophages. J Immunol. 1999;163:5039–5048. [PubMed] [Google Scholar]
- Mayer SA, Rincon F. Treatment of intracerebral haemorrhage. Lancet Neurol. 2005;4:662–672. doi: 10.1016/S1474-4422(05)70195-2. [DOI] [PubMed] [Google Scholar]
- McKimmie CS, Roy D, Forster T, Fazakerley JK. Innate immune response gene expression profiles of N9 microglia are pathogen-type specific. J Neuroimmunol. 2006;175:128–141. doi: 10.1016/j.jneuroim.2006.03.012. [DOI] [PubMed] [Google Scholar]
- Meng X, Xu S, Lao L. Clinical acupuncture research in the West. Front Med. 2011;5:134–140. doi: 10.1007/s11684-011-0135-9. [DOI] [PubMed] [Google Scholar]
- Park JS, Gamboni-Robertson F, He Q, Svetkauskaite D, Kim JY, Strassheim D, Sohn JW, Yamada S, Maruyama I, Banerjee A, Ishizaka A, Abraham E. High mobility group box 1 protein interacts with multiple Toll-like receptors. Am J Physiol Cell Physiol. 2006;290:C917–924. doi: 10.1152/ajpcell.00401.2005. [DOI] [PubMed] [Google Scholar]
- Paxinos G, Watson C. 6th Edition. Academic Press/Elsevier; 2007. The Rat Brain in Stereotaxic Coordinates. [Google Scholar]
- Qureshi AI, Mendelow AD, Hanley DF. Intracerebral haemorrhage. Lancet. 2009;373:1632–1644. doi: 10.1016/S0140-6736(09)60371-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ribbing C, Engblom C, Lappalainen J, Lindstedt K, Kovanen PT, Karlsson MA, Lundeberg L, Johansson C, Nilsson G, Lunderius-Andersson C, Scheynius A. Mast cells generated from patients with atopic eczema have enhanced levels of granule mediators and an impaired Dectin-1 expression. Allergy. 2011;66:110–119. doi: 10.1111/j.1398-9995.2010.02437.x. [DOI] [PubMed] [Google Scholar]
- Shichita T, Hasegawa E, Kimura A, Morita R, Sakaguchi R, Takada I, Sekiya T, Ooboshi H, Kitazono T, Yanagawa T, Ishii T, Takahashi H, Mori S, Nishibori M, Kuroda K, Akira S, Miyake K, Yoshimura A. Peroxiredoxin family proteins are key initiators of post-ischemic inflammation in the brain. Nat Med. 2012;18:911–917. doi: 10.1038/nm.2749. [DOI] [PubMed] [Google Scholar]
- Strasser D, Neumann K, Bergmann H, Marakalala MJ, Guler R, Rojowska A, Hopfner KP, Brombacher F, Urlaub H, Baier G, Brown GD, Leitges M, Ruland J. Syk kinase-coupled C-type lectin receptors engage protein kinase C-sigma to elicit Card9 adaptor-mediated innate immunity. Immunity. 2012;36:32–42. doi: 10.1016/j.immuni.2011.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sudlow CL, Warlow CP. Comparable studies of the incidence of stroke and its pathological types: results from an international collaboration. International Stroke Incidence Collaboration. Stroke. 1997;28:491–499. doi: 10.1161/01.str.28.3.491. [DOI] [PubMed] [Google Scholar]
- Suzuki Y, Nakano Y, Mishiro K, Takagi T, Tsuruma K, Nakamura M, Yoshimura S, Shimazawa M, Hara H. Involvement of Mincle and Syk in the changes to innate immunity after ischemic stroke. Sci Rep. 2013;3:3177. doi: 10.1038/srep03177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takizawa T, Tada T, Kitazawa K, Tanaka Y, Hongo K, Kameko M, Uemura KI. Inflammatory cytokine cascade released by leukocytes in cerebrospinal fluid after subarachnoid hemorrhage. Neurol Res. 2001;23:724–730. doi: 10.1179/016164101101199243. [DOI] [PubMed] [Google Scholar]
- Tang CL, Li J, Zhao B, Shi S, Shen H, Xia ZY. Effects of dexmedetomidine combined with sodium creatine phosphate on inflammation, oxidative stress, and neurological function recovery in patients undergoing intracranial hematoma evacuation: study protocol for a multi-center, prospective randomized parallel-cohort controlled trial. Asia Pac J Clin Trials Nerv Syst Dis. 2017;2:1–8. [Google Scholar]
- Tang SC, Arumugam TV, Xu X, Cheng A, Mughal MR, Jo DG, Lathia JD, Siler DA, Chigurupati S, Ouyang X, Magnus T, Camandola S, Mattson MP. Pivotal role for neuronal Toll-like receptors in ischemic brain injury and functional deficits. Proc Natl Acad Sci U S A. 2007;104:13798–13803. doi: 10.1073/pnas.0702553104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J, Dore S. Inflammation after intracerebral hemorrhage. J Cereb Blood Flow Metab. 2007;27:894–908. doi: 10.1038/sj.jcbfm.9600403. [DOI] [PubMed] [Google Scholar]
- Xie Y, Guo H, Wang L, Xu L, Zhang X, Yu L, Liu Q, Li Y, Zhao N, Zhao N, Ye R, Liu X. Human albumin attenuates excessive innate immunity via inhibition of microglial Mincle/Syk signaling in subarachnoid hemorrhage. Brain Behav Immun. 2017;60:346–360. doi: 10.1016/j.bbi.2016.11.004. [DOI] [PubMed] [Google Scholar]
- Xue X, You Y, Tao J, Ye X, Huang J, Yang S, Lin Z, Hong Z, Peng J, Chen L. Electro-acupuncture at points of Zusanli and Quchi exerts anti-apoptotic effect through the modulation of PI3K/Akt signaling pathway. Neurosci Lett. 2014;558:14–19. doi: 10.1016/j.neulet.2013.10.029. [DOI] [PubMed] [Google Scholar]
- Yasukawa S, Miyazaki Y, Yoshii C, Nakaya M, Ozaki N, Toda S, Kuroda E, Ishibashi K, Yasuda T, Natsuaki Y, Mi-ichi F, Iizasa E, Nakahara T, Yamazaki M, Kabashima K, Iwakura Y, Takai T, Saito T, Kurosaki T, Malissen B, et al. An ITAM-Syk-CARD9 signalling axis triggers contact hypersensitivity by stimulating IL-1 production in dendritic cells. Nat Commun. 2014;5:3755. doi: 10.1038/ncomms4755. [DOI] [PubMed] [Google Scholar]
- Zhang GW, Zou W, Liu F. Effects of the scalp acupuncture at Baihui (DU20) through qubin (GB7) on the expressions of GDNF VEGF in the brain tissue of rats with acute intracerebral hemorrhage. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2012;32:1264–1270. [PubMed] [Google Scholar]
- Zhao F, Hua Y, He Y, Keep RF, Xi G. Minocycline-induced attenuation of iron overload and brain injury after experimental intracerebral hemorrhage. Stroke. 2011;42:3587–3593. doi: 10.1161/STROKEAHA.111.623926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao X, Sun G, Zhang J, Strong R, Song W, Gonzales N, Grotta JC, Aronowski J. Hematoma resolution as a target for intracerebral hemorrhage treatment: role for peroxisome proliferator-activated receptor gamma in microglia/macrophages. Ann Neurol. 2007;61:352–362. doi: 10.1002/ana.21097. [DOI] [PubMed] [Google Scholar]
- Zheng H, Chen C, Zhang J, Hu Z. Mechanism and therapy of brain edema after intracerebral hemorrhage. Cerebrovasc Dis. 2016;42:155–169. doi: 10.1159/000445170. [DOI] [PubMed] [Google Scholar]
- Zhou Y, Wang Y, Wang J, Anne Stetler R, Yang QW. Inflammation in intracerebral hemorrhage: from mechanisms to clinical translation. Prog Neurobiol. 2014;115:25–44. doi: 10.1016/j.pneurobio.2013.11.003. [DOI] [PubMed] [Google Scholar]
- Zou W, Chen QX, Sun XW, Chi QB, Kuang HY, Yu XP, Dai XH. Acupuncture inhibits Notch1 and Hes1 protein expression in the basal ganglia of rats with cerebral hemorrhage. Neural Regen Res. 2015;10:457–462. doi: 10.4103/1673-5374.153696. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Modified neurological severity score points
The primary data of Figure 2