Abstract
Objective
To examine 2-year changes in weight status and behaviors among children living in neighborhoods differing on nutrition and activity environments.
Methods
Prospective observational Neighborhood Impact on Kids study in King County, WA and San Diego County, CA. Children 6–12 years old and a parent/caregiver completed Time 1 (n=681) and Time 2 (n=618) assessments. Children lived in neighborhoods characterized as ‘high/favorable’ or ‘low/unfavorable’ in nutrition and activity environments, respectively (four neighborhood types). Child BMI z-score and overweight/obesity status were primary outcomes, with diet and activity behaviors as behavioral outcomes.
Results
Adjusting for sociodemographics and Time 1 values, children living in two of the three less environmentally-supportive neighborhoods had significantly less favorable BMI z-score changes (+0.11, CI 0.01 to 0.21; +0.12, CI 0.03 to 0.21) and all three less supportive neighborhoods had higher overweight/obesity (RRs 1.41 – 1.49, CIs 1.13 to 1.80) compared to children in the most environmentally-supportive neighborhoods. Changes in daily energy intake and sedentary behavior by neighborhood type were consistent with observed weight status changes, with unexpected findings for physical activity.
Conclusions
More walkable and recreation-supportive environments with better nutrition access were associated with better child weight outcomes and related behavior changes.
Keywords: environmental factors, pediatrics, dietary recalls, accelerometry
Introduction
Childhood obesity remains highly prevalent in the U.S.[1] Ecological models highlight factors across levels of influence (e.g., familial, neighborhood) that may impact children’s weight status and related behaviors [2–4]. Evidence linking neighborhood environment to children’s weight status and eating and physical activity behaviors is more limited than for adults, is mostly cross-sectional, and is weak or inconsistent [5,6]. A systematic review examining associations between nutrition environment and childhood obesity indicated that most studies found no significant associations between supermarket or fast food restaurant availability in the home neighborhood and obesity among children, although associations were more common within lower income neighborhoods or lower income families [7]. Another review found more consistent associations between neighborhood built environments that promote walkability and lower child weight status [8]. However, a recent meta-analysis indicated that walkable built environments are more often negatively related to younger children’s physical activity and more supportive of adolescents’ physical activity [9]. While most home neighborhood environment studies focus on either nutrition or activity environments [7], the baseline Time 1 cross-sectional component of our Neighborhood Impact on Kids (NIK) Study indicated that children living in neighborhoods with environments favorable for both physical activity and nutrition (i.e., the High Physical Activity Environment and Nutrition Environment or High PAE/High NE neighborhoods) had the lowest rates of overweight/obesity [10] compared to other neighborhood types.
More longitudinal studies are needed to examine whether children’s home neighborhood environments have lasting effects on the trajectory of children’s weight status and related behaviors over time. Among the few existing prospective studies examining such associations, Leung and colleagues found that having more convenience stores in home neighborhoods was related to higher weight status 3 years later among girls, whereas more produce outlets was related to lower overweight/obesity in the future [11]. Others found that girls with more supermarkets in their home neighborhoods had lower BMI and lower odds of obesity 3 years later, but having more proximal limited-service restaurants was related to higher child weight status in the future [12]. Other research examined associations between a child’s home neighborhood physical activity environment and weight status, with individual studies finding that more playable (e.g., proximal park space), walkable, and safer (e.g., further distance from high traffic streets) environments were related to healthier children’s weight status trajectories [13–15]. These prospective studies appear promising, but there remain few such studies, most have not examined combinations of nutrition and activity environments, and studies have not included robust measures of children’s diet and activity change.
The present analysis examined 2-year changes in child weight status and weight-related behaviors among children in the Neighborhood Impact on Kids study living in neighborhoods selected to differ on both nutrition and activity environments. We hypothesized that children living in the most favorable neighborhood environments for both nutrition and physical activity would have healthier weight status and behavioral changes over time, even after adjusting for neighborhood, household, and individual sociodemographic factors.
Method
Neighborhood selection
Details about neighborhood selection are provided elsewhere [10,16]. Neighborhoods were defined as census block groups in King County (Seattle area), WA and San Diego County, CA. Activity and nutrition environment data were collected (e.g., park quality, presence of supermarkets) or captured from existing spatial data (e.g., street network). Neighborhoods considered high (i.e., more favorable or supportive) if physical activity environments (PAE) were higher than the corresponding county median summed z-score values of residential density, retail floor area ratio, land use mix, street connectivity (i.e., walkability [17]) and had at least one high quality park. Quality of parks was evaluated through the Environmental Assessment of Public Recreation Spaces (EAPRS) direct observation tool [18], with high quality parks defined as those with EAPRS scores > 200 (for the EAPRS tool and scoring see http://www.seattlechildrens.org/research/child-health-behavior-and-development/saelens-lab/measures-and-protocols/). Low PAE neighborhoods were below county median score on walkability and had no parks within the block group or within the ¼ mile buffer around the block group. Block groups were buffered to capture facilities such as parks that were just beyond their boundaries and easily accessible by residents near the boundary. High nutrition environment (NE) neighborhoods had a supermarket in the block group or nearby (<½ mile buffer) and fewer fast food restaurants (≤16 for King County or ≤31 for San Diego County). Low NE neighborhoods had either no supermarket nearby or had a proximal supermarket but many fast food restaurants (>16 for King County; >31 for San Diego County). The criteria for fast food restaurant differed by county because San Diego County had more than twice the number of fast food restaurants than King County, and the specific cut-offs were based pragmatically on providing a sufficient number of families to recruit. The neighborhood selection process resulted in four neighborhood types: High PAE/ NE, High PAE and Low NE, Low PAE/High NE, and Low PAE/Low NE. Maps of these counties and eligible block groups are provided elsewhere [16]. Environmental data were collected or derived from existing data sources in 2006–2007.
Recruitment
Details about participant recruitment are provided elsewhere [10,16]. Households with children in eligible neighborhoods were identified through commercial marketing databases, mailed information about the study, and contacted by phone to determine eligibility and interest. Children 6–12 years old and one parent/caregiver were recruited, and initial (Time 1; T1) data collection occurred September 2007–January 2009. Time 2 data collection was scheduled for 2 years after T1 for each participant (September 2009–February 2011), with average length of follow-up being 23.7 months (±1.9). Eligibility included a) living in an eligible neighborhood; b) able to do at least moderate intensity physical activity; c) not having any medical conditions or treatment associated with obesity or growth; d) child being >10th percentile BMI for age and sex based on parent report; and e) child not having significant eating disorder psychopathology, being on a medically prescribed dietary regimen, or having a mental health problem that would interfere with participation. Only one child per household participated, so if multiple children in a household were eligible and interested, the child with the nearest birthday to the recruitment date was enrolled.
Participants
At Time 2 (T2), 642 of the 681 children available for cross-sectional T1 anthropometric analysis [10,16] completed the follow-up anthropometric measurement at a clinic or home visit, although 26 of these children had moved home residence since T1 and were excluded from the present longitudinal analyses. Children with any missing individual-level sociodemographic data (n=28) were also not included in analyses. The children with both T1 and T2 data came from 399 different census block groups.
Participant retention from T1 to T2 did not differ by neighborhood type (83.8% – 85.2%). Children lost to follow-up versus retained had participating parents with lower T1 age (39.7 versus 41.7, p<.003), were more likely to be Hispanic (24.7% versus 15.9%, p<.036), and had lower household income (<$50K; 23.9% versus 12.8%, p<.022). Children lost to follow-up had significantly higher T1 zBMI than those retained (0.63 versus 0.41, p<.03) but the retained versus lost sample did not differ in T1 overweight/obesity rates or on any T1 eating or activity behaviors. T1 block groups not represented in T2 had significantly lower percentages of White populations (68% versus 76%; p<.008) and lower resident median age (34.7 versus 37.0, p<.04) relative to retained block groups.
Measures
T1 and T2 anthropometric and behavioral measures were collected using the same procedures.
Anthropometrics
Child and parent height and weight were collected by a trained research assistant at the research clinic or at their home. Measures were obtained in triplicate to the nearest 0.1kg and 0.1cm, respectively, using a digital scale (Detecto 750; Detecto DR400C) and stadiometer (235 Heightronic digital stadiometer, portable SECA 214), with additional measurement until 3 of 4 consecutive measures were within 0.1kg and 0.5cm, respectively, and these most proximal values were averaged. Child BMI was calculated and standardized relative to CDC 2000 norms to determine Child BMI z-score [19]. Child overweight/obesity was defined as ≥85th BMI percentile for age and sex.
Physical activity and sedentary behavior
Child activity was measured by the GT1M Actigraph® accelerometer using 30 second epochs. Children were instructed to wear the accelerometer for seven consecutive days following the anthropometric visit. Children were asked to re-wear the accelerometer if <6 days of data (minimum of 10 waking hours per day) were recorded. Average minutes of moderate-to-vigorous physical activity (MVPA) per valid day were determined using age-based 3-MET cut-points,[20] with a valid day defined as 8 or more valid hours, and a valid hour defined as having no more than 20 minutes of consecutive zero activity counts. Average sedentary minutes per valid day was the sum of epochs with activity counts 0–50 (per 30 second epoch) among valid hours within valid days. Only children with 3+ valid days were included in analyses.
Dietary quality and energy intake
Child dietary intake was assessed by three random, 24-hour dietary recalls conducted by trained staff over the phone using the standard multiple-pass approach, after the anthropometric visit. A consensus recall approach was used with parents and children ≤ 8 years old, with older children reporting individually with parent assistance. Parent-child dyads used two-dimensional food models (Nutrition Consulting Enterprise) to assist with portion estimation during recalls. Recall data were analyzed using Nutrition Data System for Research (NDS-R) software (version 2.92). Only children with at 2+ daily recalls were included in analyses. Child diet quality was assessed via the DASH score [21], based on the sum score (range 0–80) of eight food groups (grains, vegetables, fruits, dairy, meat, nuts/seed/legumes, fats/oils, and sweets), with a maximum component score of 10 for each food group and higher values indicating higher diet quality [21,22]. Diet quality and energy intake (total kcal/day) estimates were averages across available days of dietary recall.
Sociodemographics
Demographic characteristics of participants’ block groups were gathered from 2000 U.S. Census, including median resident age, average family size (among family households), number of residents reporting being White, and median household income. Parents reported their age, highest level of education, number of children in the household, and annual household income (in $10K increments up to $100K+), as well as child sex, age, race, and ethnicity at T1.
This study was approved by Institutional Review Boards at Seattle Children’s Hospital, San Diego State University, and Emory University. Parents provided written consent, and children provided assent to participate.
Analyses
Assessments were available at both T1 and T2 for 618 children, though sample sizes varied by outcome and were attenuated by missing values for covariates. There were 586 children in the continuous zBMI analysis, as 2 children with extreme zBMI changes (>3 SDs) from T1 to T2 were excluded, but 588 children were retained in the categorical weight status change analysis. Missing or insufficient data for diet and activity assessments resulted in sample sizes of 573 and 558 respectively for the analyses of eating and activity behaviors.
For bivariate analyses, analysis of variance (ANOVA) examined change in continuous outcomes across neighborhood type. Chi-square tests for trend were used to examine child weight status at T2 across neighborhood type overall and then separately by T1 weight status. Primary analyses were based on multivariable regression models. For continuous outcomes (zBMI, DASH scores, energy intake, MVPA and sedentary time) linear regression was used. For child weight status, relative risk regression based on a modified Poisson regression approach was applied [23]. In all the regression models, T2 outcomes were treated as dependent variables, with corresponding T1 measures and baseline sociodemographics entered as predictors along with neighborhood type. Region (San Diego, Seattle) was entered, but was not significant in any model. Clustering by block group was not done because most participants were the only participants in their block group. Significance was defined as p≤.05.
Results
Parent age differed significantly by neighborhood type, but no other sociodemographic differences were found by neighborhood type (see Table 1). Child zBMI and behaviors at T1 and T2 are provided in Table 1. Across all models, values at T1 were significantly related to corresponding T2 values.
Table 1.
Longitudinal sample characteristics and child anthropometrics and behaviors by neighborhood type (n=618*)
| Low PAE/ Low NE neighborhoods | Low PAE/ High NE neighborhoods | High PAE/ Low NE neighborhoods | High PAE/ High NE neighborhoods | |
|---|---|---|---|---|
| Neighborhood Characteristics | ||||
|
| ||||
| # of block groups | n=108 | n=85 | n=91 | n=115 |
|
| ||||
| Average percent White | 78.3% | 76.9% | 73.1% | 75.7% |
|
| ||||
| Median resident age (years) | 38.1 (6.8) | 37.1 (6.2) | 35.4 (5.7) | 37.2 (7.0) |
|
| ||||
| Average family size | 3.2 (0.4) | 3.2 (0.3) | 3.1 (0.5) | 3.1 (0.5) |
|
| ||||
| Median household income ($) | 73449 (22783) | 64690 (23035) | 54190 (19676) | 56329 (19142) |
|
| ||||
| Child, Parent, or Household Characteristics | ||||
|
| ||||
| # of children* | 161 | 143 | 150 | 164 |
|
| ||||
| Baseline child age (years) | 9.1 (1.5) | 9.0 (1.6) | 9.0 (1.6) | 9.3 (1.5) |
|
| ||||
| Child sex (% female) | 50.9% | 50.3% | 49.3% | 54.3% |
|
| ||||
| Child ethnicity (% Hispanic) | 12.2% | 16.4% | 17.7% | 17.4% |
|
| ||||
| Child race (%) | ||||
| - White | 80.1% | 85.3% | 82.0% | 84.1% |
| - Black or African American | 5.0% | 1.4% | 1.3% | 1.8% |
| - Asian or Pacific Islander | 5.6% | 6.3% | 2.0% | 1.8% |
| - Other or multiple races | 9.3% | 6.9% | 14.7% | 12.2% |
|
| ||||
| Parent sex (% female) | 85.7% | 83.8% | 84.0% | 92.0% |
|
| ||||
| Baseline parent age (years) | 41.5 (5.8) | 41.4 (5.6) | 41.1 (5.8) | 42.8 (5.6) |
|
| ||||
| Baseline highest parent education in household | ||||
| - Up to some college | 24.8% | 27.3% | 23.0% | 18.8% |
| - Completed college | 39.2% | 40.3% | 37.8% | 41.3% |
| - More than college degree | 35.9% | 32.4% | 39.1% | 40.0% |
|
| ||||
| T1 parent BMI | 27.3 (6.3) | 27.1 (5.2) | 26.5 (5.8) | 26.5 (5.8) |
|
| ||||
| Baseline # of children <18 years old in household | 2.4 (1.0) | 2.4 (0.9) | 2.4 (0.9) | 2.3 (0.8) |
|
| ||||
| Baseline household income | ||||
| - <50K | 8.6% | 12.5% | 16.2% | 14.0% |
| - 50–100K | 36.2% | 34.6% | 41.2% | 38.9% |
| - >100K | 55.3% | 52.9% | 42.6% | 47.1% |
|
| ||||
| Child Anthropometrics and Behaviors | ||||
|
| ||||
| T1 child BMI z-score | 0.51 (0.99) | 0.45 (1.05) | 0.36 (0.94) | 0.32 (0.85) |
|
| ||||
| T2 child BMI z-score | 0.46 (1.04) | 0.46 (1.03) | 0.39 (0.99) | 0.23 (0.92) |
|
| ||||
| T1 child diet quality (DASH score) | 41 (8) | 42 (7) | 42 (7) | 42 (7) |
|
| ||||
| T2 child diet quality (DASH score) | 41 (7) | 41 (8) | 41 (8) | 41 (7) |
|
| ||||
| T1 child energy intake (kcals/day) | 1768 (348) | 1685 (388) | 1717 (414) | 1793 (455) |
|
| ||||
| T2 child energy intake (kcals/day) | 2028 (483) | 1878 (469) | 1878 (460) | 1902 (422) |
|
| ||||
| T1 child 3+ METs moderate-to-vigorous physical activity (minutes/day) | 146 (49) | 144 (51) | 150 (55) | 143 (57) |
|
| ||||
| T2 child 3+ METs moderate-to-vigorous physical activity (minutes/day) | 119 (65) | 121 (73) | 106 (43) | 103 (43) |
|
| ||||
| T1 child daily sedentary time (minutes/day) | 393 (72) | 396 (66) | 399 (68) | 399 (79) |
|
| ||||
| T2 child daily sedentary time (minutes/day) | 498 (157) | 479 (145) | 441 (76) | 445 (87) |
Note. Values are mean (standard deviation) or percentages as indicated; PAE = physical activity environment; NE = nutrition environment; non-percentage values are mean (standard deviation) unless otherwise noted;
some sample sizes are lower than this because of missing sociodemographic data (e.g., parental refusal to report on household income)
Change in child zBMI and weight status
In unadjusted analysis, child zBMI did not differ by neighborhood type at T1 or T2. However, after controlling for T1 child zBMI and sociodemographics, children in low PAE / high NE neighborhood and high PAE / low NE neighborhoods had significantly higher average zBMI at T2 than children in the high PAE / high NE neighborhoods. In adjusted models, BMI z-score for children in the low PAE / low NE neighborhoods did not differ significantly from high PAE / high NE neighborhood children. Older children had lower T2 zBMI values (see Table 2).
Table 2.
Linear regression model results for child Time 2 BMI z-score and related behaviors, adjusting for multi-level sociodemographics and corresponding T1 BMI z-score and related behaviors
| BMI z-score (n=586) | Energy Intake (kcal/day) (n=573) | 3+ MET MVPA (mins/day) (n=558) | Sedentary activity (mins/day) (n=558) | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Estimate | (95% CI) | Estimate | (95% CI) | Estimate | (95% CI) | Estimate | (95% CI) | |
|
| ||||||||
| Neighborhood typea | ||||||||
| - Low PAE / Low NE | 0.06 | (−0.04, 0.16) | 116.4* | (15.6, 217.2) | 7.3 | (−2.8, 17.4) | 50.2* | (22.2,78.2) |
| - Low PAE / High NE | 0.11* | (0.01, 0.21) | −8.2 | (−111.1, 94.7) | 12.3* | (2.2, 22.5) | 38.3* | (10.7, 66.5) |
| - High PAE / Low NE | 0.12* | (0.03, 0.21) | −15.9 | (−113.0, 81.1) | −4.7 | (−14.3, 5.0) | −9.9 | (−36.8, 17.0) |
|
| ||||||||
| Child age | −0.03* | (−0.05, −0.005) | 23.2 | (−0.9, 47.2) | −8.9* | (−12.1, −5.7) | 5.0 | (−2.5, 12.4) |
|
| ||||||||
| Child sex (girls)b | −0.02 | (−0.08, 0.05) | −236.3* | (−307.7, −165.0) | −13.7* | (−21.0, −6.5) | −6.3 | (−25.5, 12.9) |
|
| ||||||||
| Child race (non-White)c | 0.04 | (−0.05,0.13) | −43.3 | (−134.6, 48.0) | 0.5 | (−8.4, 9.3) | −1.7 | (−26.3, 23.0) |
|
| ||||||||
| Child ethnicity (Hispanic)d | 0.09 | (−0.01, 0.20) | −28.3 | (−136.1, 79.4) | 7.3 | (−3.1, 17.8) | 14.0 | (−15.2, 43.2) |
|
| ||||||||
| Parent age | 0.001 | (−0.006, 0.008) | 3.7 | (−3.5, 10.9) | −0.2 | (−0.9, 0.5) | 0.09 | (−1.9, 2.1) |
|
| ||||||||
| Parent education | −0.004 | (−0.04, 0.04) | 14.6 | (−26.5, 55.8) | −2.3 | (−6.3, 1.8) | 4.6 | (−6.7, 15.9) |
|
| ||||||||
| Parent BMI at T1 | 0.00003 | (−0.001, 0.001) | 0.1 | (−0.5, 0.7) | −0.02 | (−0.10, 0.06) | −0.02 | (−0.24, 0.19) |
|
| ||||||||
| Number of children in household | −0.009 | (−0.05, 0.03) | 2.9 | (−37.9, 43.8) | 2.1 | (−1.9, 6.2) | 3.6 | (−7.7, 14.8) |
|
| ||||||||
| Annual household income | 0.007 | (−0.008, 0.023) | 4.5 | (−11.9, 21.0) | 2.3* | (0.7, 3.9) | 1.6 | (−2.9, 6.1) |
|
| ||||||||
| Number of neighborhood residents reporting being White race | −0.0004 | (−0.0001, 0.0001) | 0.32 | (−0.02, 0.08) | 0.002 | (−.002, 0.007) | 0.01 | (−0.004, 0.023) |
|
| ||||||||
| Average family size in neighborhood | −.08 | (−0.195, 0.035) | 18.1 | (−100.3, 136.4) | 5.7 | (−6.0, 17.4) | 22.5 | (−10.1, 55.1) |
|
| ||||||||
| Median age of neighborhood residents | −0.005 | (−0.012, 0.003) | −1.2 | (−8.8, 6.4) | 0.2 | (−0.5, 1.0) | −0.2 | (−2.3, 1.9) |
|
| ||||||||
| Median household income | −1.15e−6 | (−3.06e-6, 7.65e-7) | 0.001 | (−0.001, 0.003) | 0.0002* | (0.00001, 0.00004) | −0.0001 | (−0.001, 0.0004) |
|
| ||||||||
| Corresponding Time 1 value | 0.94* | (0.91, 0.98) | 0.3* | (0.2, 0.4) | −0.5* | (−0.6, −.04) | 0.6* | (0.4, 0.7) |
|
| ||||||||
| Sample size | 586 | 573 | 558 | 558 | ||||
Note. Estimates are unstandardized beta coefficients; models also included site (Seattle versus San Diego area) and amount of time between measurement visits; sample sizes vary based on differences in data availability by outcome; PAE = Physical activity environment; NE = Nutrition environment;
Referent group = High PE / High NE neighborhoods;
Referent group = boys;
Referent group = White;
Referent group = Non-Hispanic;
p<.05
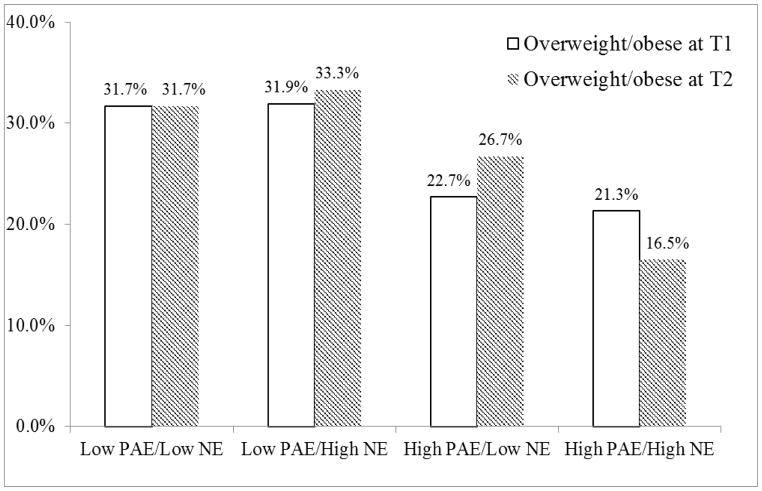
Children in the high PAE / high NE neighborhoods were significantly less likely to have overweight/obesity at T2 compared to children in all other neighborhood types (p<.003; Figure 1), with these differences sustained after controlling for T1 child weight status and sociodemographics. In the adjusted model, children in the three less-supportive neighborhood types were 41–49% more likely to have overweight/obesity at T2 than children in high PAE / high NE neighborhoods. Older children and girls were less likely to have overweight/obesity at T2, whereas Hispanic children were more likely to have overweight/obesity (Table 3).
Figure 1.
Proportion of children having overweight/obesity at T1 and T2 by neighborhood type; significant differences by neighborhood type at T2 (p<.003); analysis of T1 differences were reported previously [10].
Table 3.
Relative risks of child having overweight/obesity at Time 2 adjusting for multi-level sociodemographics and Time 1 weight status
| Among all children (n=588) | Among only children who had overweight/obesity at T1 (n=153) | |||
|---|---|---|---|---|
|
| ||||
| RR estimate | 95% CI | RR estimate | 95% CI | |
|
| ||||
| Neighborhood typea | ||||
| - Low PAE / Low NE | 1.41* | (1.13, 1.70) | 1.25 | (1.00,1.49) |
| - Low PAE / High NE | 1.49* | (1.19,1.78) | 1.25 | (0.99,1.51) |
| - High PAE / Low NE | 1.49* | (1.18,1.80) | 1.17 | (0.90,1.44) |
|
| ||||
| Child age | 0.88* | (0.80,0.96) | 0.91* | (0.85,0.97) |
|
| ||||
| Child sex (girls)b | 0.77* | (0.56,0.99) | 0.96 | (0.81,1.11) |
|
| ||||
| Child race (non-White)c | 1.21 | (0.98,1.45) | 1.15 | (0.99,1.31) |
|
| ||||
| Child ethnicity (Hispanic)d | 1.45* | (1.19,1.71) | 1.18 | (1.05,1.32) |
|
| ||||
| Parent age | 1.00 | (0.98,1.02) | 1.00 | (0.98,1.01) |
|
| ||||
| Parent education | 0.95 | (0.86,1.03) | 0.98 | (0.91,1.04) |
|
| ||||
| Parent BMI at T1 | 0.998* | (0.997,<1.000) | 1.01* | (1.00,1.03) |
|
| ||||
| Number of children in household | 0.97 | (0.86,1.09) | 0.98 | (0.88,1.08) |
|
| ||||
| Annual household income | 1.01 | (0.97,1.05) | 1.00 | (0.97,1.03) |
|
| ||||
| Number of neighborhood residents reporting being White race | 1.00 | (1.00,1.00) | 1.00 | (1.00,1.00) |
|
| ||||
| Average family size in neighborhood | 0.86 | (0.54,1.17) | 0.84 | (0.60,1.08) |
|
| ||||
| Median age of neighborhood residents | 1.00 | (0.98,1.02) | 1.01 | (0.99,1.02) |
|
| ||||
| Median household income | 1.00 | (1.00,1.00) | 1.00 | (1.00,1.00) |
|
| ||||
| Child who had overweight/obesity at T1 | 11.74* | (11.38,12.1) | ___ | ___ |
Note. Models also included site (Seattle versus San Diego area) and time between measurement visits; PAE = Physical activity environment; NE = Nutrition environment;
Referent group = High PE / High NE neighborhoods;
Referent group = boys;
Referent group = White;
Referent group = Non-Hispanic;
p<.05
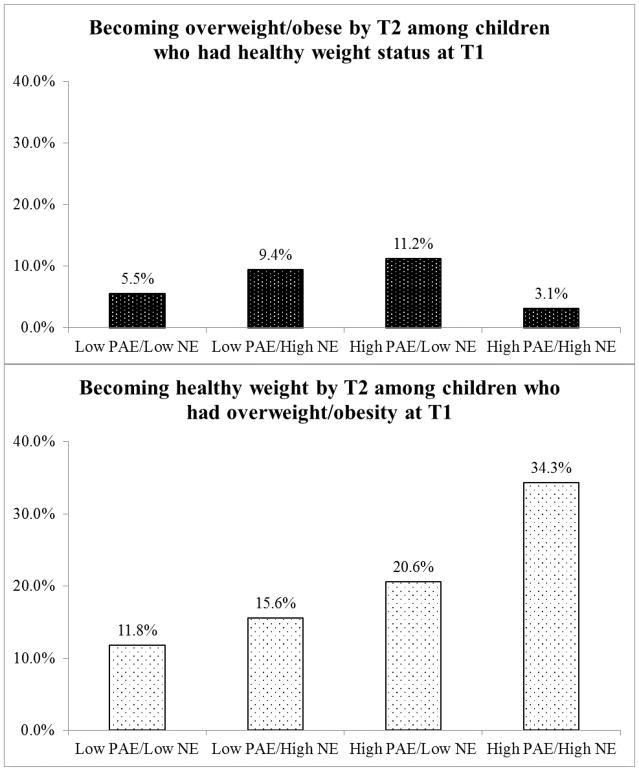
When analyzed in models unadjusted for sociodemographics, but separately by child T1 weight status, findings were in the expected direction, but were not significantly different by neighborhood type. Among children having overweight/obesity at T1, the proportion of children transitioning to not having overweight/obesity at T2 was not statistically significant different by neighborhood type (p=.057). The difference by neighborhood type in the proportion of children having overweight/obesity at Time 2 among those not having overweight/obesity at T1 was also not significant (p=.076). Both these results however were in the expected direction, with the high PAE / high NE neighborhoods having the best outcomes (Figure 2). Among children having overweight/obesity at T1 (n=153), differences in child T2 weight status across neighborhood types did not reach statistical significance in the adjusted model, although estimates for neighborhood type were moderate effect sizes and in the expected direction (Table 3). Effects of child age and Hispanic ethnicity were significant in this model, as in the all children model. The relative risk for a child having overweight/obesity at T2 for parent T1 BMI was significantly <1.00 in the all child adjusted model and >1.00 in the only child overweight/obesity at T1 adjusted model, although the magnitude of both of these estimates was small (Table 3).
Figure 2.
The percentage of children transitioning between T1 and T2 from having healthy weight status (n=435) to having overweight/obesity (p=.057 for differences by neighborhood type) and from having overweight/obesity (n=153) to having healthy weight status (p=.076 for differences by neighborhood type)
Child diet quality and energy intake
In bivariate analysis, there were no significant differences in DASH scores at T1 or T2 across neighborhood type (Table 2) or significant changes in DASH scores from T1 to T2 overall or differentially by neighborhood type.
Bivariate analysis indicated no significant differences in daily energy intake at T1 by neighborhood type, but there were differences in daily energy intake by neighborhood type at T2 (Table 1). Average energy intake increased significantly over time overall, with girls having lower energy intakes than boys. There significant differences in daily energy intake by neighborhood type at T2 after controlling for sociodemographics and T1 energy intake. Children in the Low PAE / Low NE neighborhoods had significantly higher increases over time in daily energy intake relative to children in High PAE / High NE neighborhoods (Table 2). Overall, girls had smaller increases in energy intake over time.
Child physical activity and sedentary time
In bivariate analysis, average daily minutes of 3+METs physical activity did not differ by neighborhood type at T1 or T2 (Table 1), but decreased significantly overall from T1 to T2. Unexpectedly, physical activity decreased significantly less among children in the Low PAE / High NE compared to children in the High PAE / High NE neighborhoods in the adjusted model (Table 2). Older children and girls had significantly larger decreases in physical activity over time, whereas children from higher income households and from higher income neighborhoods had significantly smaller decreases in physical activity.
Average daily sedentary time did not significantly differ by neighborhood type at T1, but did significantly differ at T2 (Table 1) and increased significantly overall from T1 to T2 based on bivariate analysis. In the adjusted model, there was significant differential change by neighborhood type in sedentary time, with higher increases among children in Low PAE / Low NE and Low PAE / High NE neighborhoods compared to children in the High PAE / High NE neighborhoods. No sociodemographic factors were related to sedentary time changes (Table 2).
Discussion
Present findings highlight the importance of having a favorable combination of physical activity and nutrition environments in neighborhoods where children live to support their healthy weight status trajectory and related behaviors. After adjusting for sociodemographics across multiple levels, children living in neighborhoods more conducive to walking, having at least one high quality park, and a favorable nutrition environment marked by the availability of at least one large grocery store without a high concentration of fast food restaurants, had significantly more favorable weight status changes than children in two of the three other less environmentally-supportive neighborhoods. Children in these most favorable neighborhood environments were nearly 50% less likely to have overweight/obesity by T2 compared to children in all other neighborhood types when accounting for initial child weight status and sociodemographics. Although not statistically significant, partially because the study was not designed for subgroup analyses, the transitions between having and not having overweight/obesity also were in a similar direction by neighborhood type (i.e., most favorable child weight status outcomes in the High PAE / High NE neighborhoods), even though children in the most favorable neighborhoods initially had the lowest level of having overweight/obesity among neighborhood types [10]. The decrease over time in average child BMI z-score seen in the most supportive neighborhoods was more than half the average change seen among children having overweight/obesity provided intense weight management intervention [24]. By T2, the overweight/obesity rate in these most favorable neighborhoods was nearly half that of two of the three types of less favorable neighborhood types and approximately half the national prevalence for childhood overweight/obesity [25]. Present findings are consistent with some other longitudinal findings regarding neighborhood environment and child weight status trajectories, e.g., [26].
Differential changes by neighborhood type in daily energy intake and sedentary behavior were generally consistent with the observed neighborhood environment-child weight status change differences. Across time, children living in the least favorable neighborhood environments increased their relative adjusted daily average energy intake by >100 kcals more and their daily sedentary time by >50 minutes more than children living in the most favorable neighborhood environments. Children residing in neighborhoods with poorer activity environments but better nutrition environments also had a relative increase in sedentary behavior. Unexpectedly, one of the neighborhood types (low PAE / high NE neighborhoods) with less-supportive environments for physical activity had children with the smallest declines in physical activity over time. However, recent reviews suggest that macro-environmental factors that contribute to walkability and to used define a more supportive physical activity environment in the present study (e.g., greater land use mix) are not consistently or highly related to children’s overall physical activity and have in some instanced been related to lower physical activity among younger children [27]. Other aspects of the built environment or parental travel and activity patterns may influence children’s physical activity changes over time. For example, analysis of other data from the Neighborhood Impact on Kids study found that micro-environment features immediately around a child’s home, such as sidewalk and street-crossing qualities, were significantly associated with children’s active travel, leisure activity, and accelerometer-assessed total physical activity [28]. Caregivers in low PAE neighborhoods with adequate time and financial resources may be transporting their children to public or private physical activity facilities and programs. Low PAE neighborhoods had higher median incomes, and families from these neighborhoods reported higher average household income compared high PAE neighborhood families. Higher household and neighborhood income were also related to lesser declines in physical activity from T1 to T2. More disadvantaged children living in low PAE may show different physical activity trajectories. The precipitous overall decline in children’s average physical activity observed with age has been previously documented [29], and further inquiry is clearly needed to identify and implement strategies to prevent this decline, particularly among disadvantaged youth.
There were some important study limitations. Neighborhood was defined by census block groups, without more fine-grained consideration of environmental features more immediately around children’s homes or perceptions of environment. This study was limited to two metropolitan areas in the western U.S. with relatively higher costs of living and the sample was more racially white and higher income than the neighborhoods in which they lived, with most parents having high education levels. Lack of sufficient racial/ethnic and income diversity within neighborhood types prevented exploration of interactions between sociodemographics and environment. Prior studies have found higher childhood obesity rates in more disadvantaged neighborhoods or households [30,31], with some evidence that built environment differences may explain these disparities [10,32]. Environmental factors and their quality are not equally distributed [33] and emerging evidence suggests that activity and nutrition environments may interact with socioeconomic factors to impact healthy behaviors and weight status [34]. Socioeconomic factors may be important in explaining disparities between different racial/ethnic groups in child weight status, with activity and nutrition environments perhaps contributing differently or to a lesser extent to weight-related behaviors in disadvantaged populations [35]. More research is needed to understand and then intervene on environmental inequities [36]. Present analyses also did not examine how neighborhood environment may be impacting children’s within-home environments or how much exposure children or their parent(s)/caregiver(s) had to their neighborhood environment, although prior analyses from this study did find relationships between parenting practices/rules around eating and children’s diet quality [37]. Unlike Chen and colleagues [12], this study did not examine changes to environments over time. More natural experiments are needed to evaluate changes in policies, systems, and environments designed to, or that may inadvertently, affect children’s weight outcomes [38]. However, such policy, systems, and environmental changes at the neighborhood level are not often implemented by researchers or institutions (e.g., schools), but rather by decision-makers within local governments. The Institute of Medicine has specific recommendations for local governments to improve neighborhood environments and policies to support healthy child weight [39]. The present study did not examine mechanisms by which environment has influence. Others speculate mechanisms could include cueing/prompting by environment (e.g., presence/signage of fast food restaurants prompts visitation), the convenience of facilities in environments in which to engage in desired behaviors (e.g., having a high quality park available for active recreation), and environment establishing social norms (e.g., seeing others being active in the park may prompt other children to be active there) [3,40] It is not known whether actual objective environment or whether perceptions of environment are predominant, with evidence that these may have independent effects on health behaviors including physical activity [41].
Results add credibility and urgency to recommendations to improve both nutrition and physical activity environments as components of solutions to the global childhood obesity epidemic [42]. The present definition of a salutogenic environment that includes walkability, high quality parks, proximal supermarkets, and relatively few fast food restaurants was shown to predict more favorable trajectories in child weight status, energy intake, and sedentary behavior. Creating more neighborhoods with these characteristics requires actions by municipal governments (zoning), transportation departments (street design), parks departments, multiple components of the food industry, and multiple government agencies that regulate food retail. Though making such changes might appear to be too complex to be feasible, in fact communities and states across the US are making changes like these, and they have been associated with reductions in childhood obesity (see https://stateofobesity.org/progress/). However, more evidence regarding the impact of environmental and policy interventions for childhood obesity prevention, particularly outside of school settings is needed [38,43], including evaluating the interactive effect of programmatic and environmental interventions.
Study Importance.
Evidence is limited regarding the impact of neighborhood built and nutrition environment on the change in children’s weight status over time.
Evidence is further limited examining associations of neighborhood environments with robust measures of changes in children’s weight-related behaviors.
The present study finds that children living in neighborhoods that are supportive in both physical activity and nutrition environments have more healthy changes in child weight status, energy intake, and sedentary behavior over time.
Changing neighborhood activity and nutrition environments has the potential to improve children’s weight status and related behaviors.
Acknowledgments
Funding: Funding for the Neighborhood Impact on Kids (NIK) study was from NIH National Institute of Environmental Health Sciences (ES014240), USDA 2007-55215-17924, and by grants to the Seattle Children’s Pediatric Clinical Research Center, which were supported by grants UL1 RR025014, KL2 RR025015, and TL1 RR025016 from the NIH National Center for Research Resources.
The authors thank the children and parents/caregivers who participated in NIK and the excellent research staff that helped to conduct this work.
Footnotes
Disclosures: The authors declared no conflict of interest. All authors have read, contributed to, and approved the contents of this manuscript
References
- 1.Ogden CL, Carroll MD, Lawman HG, et al. Trends in Obesity Prevalence Among Children and Adolescents in the United States, 1988–1994 Through 2013–2014. JAMA. 2016;315:2292–2299. doi: 10.1001/jama.2016.6361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davison KK, Birch LL. Childhood overweight: a contextual model and recommendations for future research. Obes Rev. 2001;2:159–171. doi: 10.1046/j.1467-789x.2001.00036.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sallis JF, Owen N. Ecological models of health behavior. In: Glanz K, Rimer BK, Viswanath K, editors. Health Behavior: Theory, Research and Practice. 5. San Francisco: Wiley/Jossey-Bass Inc; 2015. pp. 43–64. [Google Scholar]
- 4.Sallis JF, Glanz K. Physical activity and food environments: solutions to the obesity epidemic. Milbank Q. 2009;87:123–154. doi: 10.1111/j.1468-0009.2009.00550.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dunton GF, Kaplan J, Wolch J, Jerrett M, Reynolds KD. Physical environmental correlates of childhood obesity: a systematic review. Obes Rev. 2009;10:393–402. doi: 10.1111/j.1467-789X.2009.00572.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Papas MA, Alberg AJ, Ewing R, Helzlsouer KJ, Gary TL, Klassen AC. The built environment and obesity. Epidemiol Rev. 2007;29:129–143. doi: 10.1093/epirev/mxm009. [DOI] [PubMed] [Google Scholar]
- 7.Cobb LK, Appel LJ, Franco M, Jones-Smith JC, Nur A, Anderson CA. The relationship of the local food environment with obesity: A systematic review of methods, study quality, and results. Obesity (Silver Spring) 2015;23:1331–1344. doi: 10.1002/oby.21118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Casey R, Oppert JM, Weber C, et al. Determinants of childhood obesity: what can we learn from built environment studies? Food Qual Preference. 2014;31:164–172. [Google Scholar]
- 9.McGrath LJ, Hopkins WG, Hinckson EA. Associations of objectively measured built-environment attributes with youth moderate-vigorous physical activity: a systematic review and meta-analysis. Sports Med. 2015;45:841–865. doi: 10.1007/s40279-015-0301-3. [DOI] [PubMed] [Google Scholar]
- 10.Saelens BE, Sallis JF, Frank LD, et al. Obesogenic neighborhood environments, child and parent obesity: the Neighborhood Impact on Kids study. Am J Prev Med. 2012;42:e57–64. doi: 10.1016/j.amepre.2012.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leung CW, Laraia BA, Kelly M, et al. The influence of neighborhood food stores on change in young girls’ body mass index. Am J Prev Med. 2011;41:43–51. doi: 10.1016/j.amepre.2011.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen HJ, Wang Y. Changes in the Neighborhood Food Store Environment and Children’s Body Mass Index at Peripuberty in the United States. J Adolesc Health. 2016;58:111–118. doi: 10.1016/j.jadohealth.2015.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Duncan DT, Sharifi M, Melly SJ, et al. Characteristics of walkable built environments and BMI z-scores in children: evidence from a large electronic health record database. Environ Health Perspect. 2014;122:1359–1365. doi: 10.1289/ehp.1307704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jerrett M, McConnell R, Chang CC, et al. Automobile traffic around the home and attained body mass index: a longitudinal cohort study of children aged 10–18 years. Prev Med. 2010;50(Suppl 1):S50–58. doi: 10.1016/j.ypmed.2009.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wolch J, Jerrett M, Reynolds K, et al. Childhood obesity and proximity to urban parks and recreational resources: a longitudinal cohort study. Health Place. 2011;17:207–214. doi: 10.1016/j.healthplace.2010.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Frank LD, Saelens BE, Chapman J, et al. Objective assessment of obesogenic environments in youth: geographic information system methods and spatial findings from the Neighborhood Impact on Kids study. Am J Prev Med. 2012;42:e47–55. doi: 10.1016/j.amepre.2012.02.006. [DOI] [PubMed] [Google Scholar]
- 17.Frank LD, Sallis JF, Saelens BE, et al. The development of a walkability index: application to the Neighborhood Quality of Life Study. Br J Sports Med. 2010;44:924–933. doi: 10.1136/bjsm.2009.058701. [DOI] [PubMed] [Google Scholar]
- 18.Saelens BE, Frank LD, Auffrey C, Whitaker RC, Burdette HL, Colabianchi N. Measuring physical environments of parks and playgrounds: EAPRS instrument development and inter-rater reliability. Journal of Physical Activity and Health. 2006;3(Suppl 1):S190–S207. doi: 10.1123/jpah.3.s1.s190. [DOI] [PubMed] [Google Scholar]
- 19.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States advance data from vital and health statistics; no. 314. Hyattsville, MD: National Center for Health Statistics; 2000. [PubMed] [Google Scholar]
- 20.Trost SG, Way R, Okely AD. Predictive validity of three ActiGraph energy expenditure equations for children. Med Sci Sports Exerc. 2006;38:380–387. doi: 10.1249/01.mss.0000183848.25845.e0. [DOI] [PubMed] [Google Scholar]
- 21.Gunther AL, Liese AD, Bell RA, et al. Association between the dietary approaches to hypertension diet and hypertension in youth with diabetes mellitus. Hypertension. 2009;53:6–12. doi: 10.1161/HYPERTENSIONAHA.108.116665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.U.S. Department of Health and Human Services, U.S. Department of Agriculture. Dietary Guidelines for Americans, 2005. Washington, D.C: U.S. Government Printing Office; 2005. [Google Scholar]
- 23.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 24.U.S. Preventive Services Task Force. Grossman DC, Bibbins-Domingo K, et al. Screening for Obesity in Children and Adolescents: US Preventive Services Task Force Recommendation Statement. JAMA. 2017;317:2417–2426. doi: 10.1001/jama.2017.6803. [DOI] [PubMed] [Google Scholar]
- 25.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fiechtner L, Cheng ER, Lopez G, Sharifi M, Taveras EM. Multilevel Correlates of Healthy BMI Maintenance and Return to a Healthy BMI among Children in Massachusetts. Child Obes. 2017;13:146–153. doi: 10.1089/chi.2016.0261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Timperio A, Reid J, Veitch J. Playability: Built and Social Environment Features That Promote Physical Activity Within Children. Curr Obes Rep. 2015;4:460–476. doi: 10.1007/s13679-015-0178-3. [DOI] [PubMed] [Google Scholar]
- 28.Cain KL, Millstein RA, Sallis JF, et al. Contribution of streetscape audits to explanation of physical activity in four age groups based on the Microscale Audit of Pedestrian Streetscapes (MAPS) Soc Sci Med. 2014;116:82–92. doi: 10.1016/j.socscimed.2014.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nader PR, Bradley RH, Houts RM, McRitchie SL, O’Brien M. Moderate-to-vigorous physical activity from ages 9 to 15 years. JAMA. 2008;300:295–305. doi: 10.1001/jama.300.3.295. [DOI] [PubMed] [Google Scholar]
- 30.Grow HM, Cook AJ, Arterburn DE, Saelens BE, Drewnowski A, Lozano P. Child obesity associated with social disadvantage of children’s neighborhoods. Soc Sci Med. 2010;71:584–591. doi: 10.1016/j.socscimed.2010.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Van Hulst A, Gauvin L, Kestens Y, Barnett TA. Neighborhood built and social environment characteristics: a multilevel analysis of associations with obesity among children and their parents. Int J Obes (Lond) 2013;37:1328–1335. doi: 10.1038/ijo.2013.81. [DOI] [PubMed] [Google Scholar]
- 32.Carroll-Scott A, Gilstad-Hayden K, Rosenthal L, et al. Disentangling neighborhood contextual associations with child body mass index, diet, and physical activity: the role of built, socioeconomic, and social environments. Soc Sci Med. 2013;95:106–114. doi: 10.1016/j.socscimed.2013.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sallis JF, Slymen DJ, Conway TL, et al. Income disparities in perceived neighborhood built and social environment attributes. Health Place. 2011;17:1274–1283. doi: 10.1016/j.healthplace.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 34.Burgoine T, Forouhi NG, Griffin SJ, Brage S, Wareham NJ, Monsivais P. Does neighborhood fast-food outlet exposure amplify inequalities in diet and obesity? A cross-sectional study. Am J Clin Nutr. 2016;103:1540–1547. doi: 10.3945/ajcn.115.128132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sharifi M, Sequist TD, Rifas-Shiman SL, et al. The role of neighborhood characteristics and the built environment in understanding racial/ethnic disparities in childhood obesity. Prev Med. 2016;91:103–109. doi: 10.1016/j.ypmed.2016.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Smith M, Hosking J, Woodward A, et al. Systematic literature review of built environment effects on physical activity and active transport - an update and new findings on health equity. Int J Behav Nutr Phys Act. 2017;14:158. doi: 10.1186/s12966-017-0613-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Couch SC, Glanz K, Zhou C, Sallis JF, Saelens BE. Home food environment in relation to children’s diet quality and weight status. J Acad Nutr Diet. 2014;114:1569–1579 e1561. doi: 10.1016/j.jand.2014.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mayne SL, Auchincloss AH, Michael YL. Impact of policy and built environment changes on obesity-related outcomes: a systematic review of naturally occurring experiments. Obes Rev. 2015;16:362–375. doi: 10.1111/obr.12269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.IOM (Institute of Medicine) and National Research Council. Local Government Actions to Prevent Childhood Obesity. Washington, DC: The National Academies Press; 2009. [PubMed] [Google Scholar]
- 40.Cohen DA. Obesity and the built environment: changes in environmental cues cause energy imbalances. Int J Obes (Lond) 2008;32(Suppl 7):S137–142. doi: 10.1038/ijo.2008.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Orstad SL, McDonough MH, Stapleton S, Altincekic C, Troped PJ. A Systematic Review of Agreement Between Perceived and Objective Neighborhood Environment Measures and Associations With Physical Activity Outcomes. Environment and Behavior. 2016;0:0013916516670982. [Google Scholar]
- 42.IOM (Institute of Medicine) Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation. Washington, DC: The National Academies Press; 2012. [Google Scholar]
- 43.Cauchi D, Glonti K, Petticrew M, Knai C. Environmental components of childhood obesity prevention interventions: an overview of systematic reviews. Obes Rev. 2016;17:1116–1130. doi: 10.1111/obr.12441. [DOI] [PubMed] [Google Scholar]