Abstract
Introduction
Restless legs syndrome (RLS) is a common disorder in hemodialysis patients. The present study was conducted to determine the effect of near-infrared (NIR) light therapy given to acupoints on the severity of RLS in patients undergoing hemodialysis.
Methods
This single-blind, randomized controlled trial was performed on 60 hemodialysis patients with RLS. Participants who met the inclusion criteria were randomly assigned to an intervention group (n = 30) or a control group (n = 30). Data were collected using the International Restless Legs Syndrome Rating Scale (IRLSRS) and demographic information questionnaire. The intervention group received 12 sessions of NIR light therapy (940 nm) to acupoints in the legs and feet during hemodialysis three times a week, while the control group received sham treatment. Data were analyzed using SPSS version 22 software.
Results
The results indicated that there were statistically and clinically significant differences between the intervention and control groups at the end of the intervention sessions (P < 0.001, mean difference [MD] = 3.8). However, after the treatment was discontinued, the difference was not clinically significant (MD = 2.4). In the within-group compression, the mean RLS scores of the intervention group decreased significantly during the intervention sessions (MD = 3.2, P < 0.001); however, after the treatment was discontinued, the difference was not clinically significant (MD = 1.67).
Conclusion
The present study showed that the application of NIR light to acupoints in the legs and feet was as an effective treatment for attenuating the symptoms of RLS in hemodialysis patients.
Keywords: Restless legs syndrome, Acupuncture, Infrared
Restless legs syndrome (RLS) is a common chronic sensory–motor disorder that is characterized by a strong urge to move the legs at rest and bedtime. The development of this disorder in hemodialysis patients is progressive, affecting various physical and psychological dimensions over time.1,2 The symptoms of this syndrome are greatly intensified at rest, and are relieved by moving the extremities, especially the legs.3 In hemodialysis patients, the symptoms mainly occur during dialysis when the patient is at rest and cause discomfort.1 Evidence suggests that RLS in hemodialysis patients is associated with a risk of cardiovascular disease, osteoporosis, musculoskeletal pain, and increased mortality.4–8 In the general population and in patients with end-stage renal disease (ESRD), the potential causes of RLS include anemia, pregnancy, iron deficiency, the dysfunction of dopamine within the central nervous system, a family history of RLS, and peripheral neuropathy.9,10 In patients with ESRD, iron deficiency, anemia, and dialysis are predisposing factors that can lead to RLS.9
Pharmaceutical and non-pharmaceutical therapeutic approaches are used to treat RLS.1 Pharmaceutical treatments involve drugs, such as dopamine agonists, benzodiazepines, opioids, and gabapentin.11–14 These pharmaceuticals temporarily relieve the symptoms of RLS, but are not considered to cure the disorder.15 The prescribed drugs are also associated with adverse effects, such as nausea, vomiting, dizziness, and drowsiness. The long-term use of dopamine agonists may lead to drug tolerance and an increased severity or recurrence of the symptoms of RLS.16,17
Non-pharmaceutical methods, such as acupuncture, also known as complementary therapies, are safer and have less complications than the pharmaceutical methods.18,19 However, despite its long use throughout history, there have always been some obstacles to the use of acupuncture, including the pain caused by the insertion of needles into the skin, the possibility of the transmission of infection, the risk of damage to internal organs, and the general invasive nature of the procedure.19 Thus, since the mid-20th century, many efforts have been made to find an alternative method to the use of needles, including the use of infrared light.19,20
In physics, near-infrared (NIR) light refers to the part of the spectrum of electromagnetic waves with wavelengths longer than the visible light spectrum and shorter than the spectrum of radio waves.21 Stimulating acupoints with NIR light is considered to be safer and requires less time than performing acupuncture with needles. In addition, the non-invasive nature of this method prevents the transmission of infectious diseases and is not associated with the occurrence of pain or the fear of needles.22–24
There have been no studies on the impact of NIR light therapy on RLS in patients undergoing hemodialysis. Therefore, the present study was conducted to determine the effect of NIR light therapy given to acupoints on the severity of RLS in hemodialysis patients.
Materials and Methods
Study Design and Participants
This single-blind randomized controlled trial was performed in 2017 on 60 hemodialysis patients in Imam Reza and Imam Khomeini hospitals in Kermanshah, Iran. First, a convenience sampling method was used to select possible participants. Hemodialysis patients with RLS who met the inclusion criteria were then randomly allocated to an intervention group (n = 30) or a control group (n = 30).
Inclusion and Exclusion Criteria
The inclusion criteria were as follows: informed consent to participate in the study; suffering from RLS; between the ages of 18 years and 65 years; a history of chronic renal failure treated with regular and continuous hemodialysis for at least 3 months; a regular dialysis program at least 3 times a week; no vascular access in the leg area, such as an arteriovenous shunt; the absence of peripheral neuropathy and vascular problems in the lower extremities; not pregnant; not currently taking drugs for RLS, such as dopamine agonists, benzodiazepines, opioids, and gabapentin; and no history of other motor disorders, such as Parkinson's disease, dyskinesia, and dystonia. The exclusion criteria were as follows: an unwillingness to continue to participate in the study; a failure to take part in more than three light therapy sessions; a kidney transplant; and death.
Research Tools
Data were collected using a demographic information questionnaire and the International Restless Legs Syndrome Rating Scale (IRLSRS). The demographic information questionnaire, which also provided disease information, was designed by the researcher. It consisted of questions about the age, gender, duration of hemodialysis treatment, and the most current information in the patient records, including hemoglobin, hematocrit, iron, hemodialysis adequacy, and underlying diseases.
The International RLS Study Group designed and implemented the IRLSRS. In the present study, the IRLSRS consisted of two parts. The first part was used to diagnose RLS using the following four diagnostic features:
the urge to move the legs at rest;
the beginning or worsening of symptoms during a period of rest;
the temporary relief of unpleasant sensations by moving the legs; and
the beginning or worsening of symptoms in the evening or at night.
It should be noted that all four criteria had to be met at the same time for a definitive diagnosis of RLS in the patient.25 Habibzade et al26 confirmed the validity and reliability of this tool in Iran in 2011. In their research, the content validity was used to determine the validity of the tool and Cronbach's alpha coefficient was used to obtain the reliability. The reliability of this tool was confirmed by a Cronbach’s alpha coefficient of 0.90.26
The second part of the IRLSRS contained 10 questions designed to measure the severity of RLS. The items were scored on a 5-point Likert scale ranging from zero to four: 0 = none; 1 = mild; 2 = moderate; 3 = severe; and 4 = very severe. The scores for each of the 10 questions were added with the total score varying from 0 to 40.26 The minimal clinically significant change for the IRLSRS was a decrease of three or more points between the beginning and the end of the intervention session.27 The validity and reliability of this tool have been confirmed by numerous studies; for example, in the study by Habibzade et al,26 the content validity was confirmed by 10 experts and the reliability of the tool was confirmed by a Cronbach’s alpha coefficient of 0.97.
Sampling Process
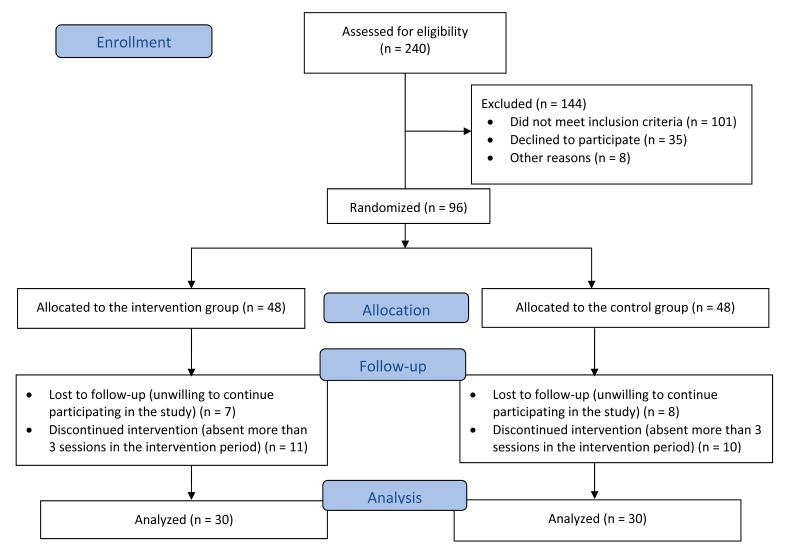
In the initial stage of the sampling process, 240 hemodialysis patients completed the first part of the IRLSRS to determine a diagnosis of RLS. A researcher administered the questionnaire through a structured interview. In addition to determining the development of RLS, other inclusion criteria were evaluated. A total of 96 patients met the inclusion criteria. Patients were assigned to either the intervention or control groups using a random allocation method and sealed envelopes. During the intervention and follow-up, 18 individuals were excluded from each group. Data analysis was done on 30 patients in each group (Figure 1).
Figure 1.
Flow diagram of the study.
In order to blind the study, none of the participants knew which group was the intervention group and which was the control group. The participants chose one of two envelopes to determine which group they were in. The intervention group was identified with the number one (“1”) written inside the envelope, while the control group was identified with the number two (“2”) written inside the envelope.
The intervention group was given 12 sessions of NIR light therapy three times a week for one month during hemodialysis, while the control group received sham treatment. For the sham treatment, the researcher pretended to implement the treatment using a probe that was not turned on; no light was exposed to the acupoints in these individuals.
The RLS severity was measured using the second part of the IRLSRS. Individuals who were literate completed the scale themselves; a structured interview was conducted for those individuals who were illiterate.
Intervention and Time Schedule
The timing of the measurements of RLS severity for the intervention and control groups is shown in Table 1. The intervention and control groups completed the IRLSRS at four distinct times.
Table 1.
Timing of RLS severity measurements in the intervention and control groups.
| Time point | ||||||
|---|---|---|---|---|---|---|
|
|
||||||
| Pre-Intervention | Intervention sessions | Post-Intervention | ||||
|
|
|
|
||||
| Baseline | 1st week | 2nd week | 3rd week | 4th week | 6th week | |
| Measurement of RLS severity | Before starting NIR light therapy | -- | End of week | -- | End of week | End of 2nd week after completing intervention |
NIR, near infrared; RLS, restless legs syndrome; --, no measurement
The NIR light therapy sessions were performed using BioBeam 940 (SyroLight Ltd., Yahud, Israel) light source. This over-the-counter handheld probe uses low-level narrow band (LLNB) light technology in the NIR spectrum. The device is easy to use, and is marketed in the USA for over-the- counter use under the US Food and Drug Administration (FDA) 510(k) regulation.28 The specifications of the BioBeam 940 are as follows: wavelength = 940 nm; the operating mode is a pulse wave; the beam area at focus is 2 cm2; the total peak light power at focus is 210 mW; the typical peak power at focus is 35 mW/cm2; the typical frequency is 130 Hz; the typical duty ratio is 10%; and 21 mW is the total average power at focus.29
In this study, the radiation angle of 90° was applied to each foot acupoint. The entire plantar surface of the foot was exposed to the NIR light. It should be noted that the energy transfer time to each acupoint was 2 min. The "bathing method" was used to transfer the energy to the foot; the infrared probe was moved across the plantar surface of the foot for 2 min.2
NIR light was applied to each of the following acupoints. The Zusanli (ST36) point is located four finger widths (3 cun) down from the bottom of the lateral side of the leg below the knee and 2.5 cun lateral to the tibia. The Sanyinjiao (SP6) point is located on the inner side of the leg, 3 cun above the ankle and posterior to the medial crest of the tibia. The Yang Ling Quan (GB34) point is located in the anterior and inferior to the head of the fibula. The Cheng Shan (BL57) point is located in the midline below the calf muscle, between the back of the knee and the heel.
In order to perform the intervention, the researcher (the first author) was trained by a physical medicine specialist. The intervention was performed on four patients at the first session in the presence of the specialist. A physiotherapist experienced in this field supervised and guided the researcher during all the intervention sessions. The intervention was performed on each patient during dialysis.
Ethical Considerations
The present study was adapted from a Master's thesis approved by the Ethics Committee of Kermanshah University of Medical Sciences, Iran (ethics code: KUMS. REC.1396.191), and registered in the Iranian Registry of Clinical Trials (IRCT2016112727779N3). To collect information for this study, the research objectives, advantages, and disadvantages were explained to each participant. Written informed consent was obtained from all participants; each person had the right to choose whether to participate in the study.
Statistical Analysis
Data were analyzed using SPSS version 22 software (IBM Corp, Armonk, NY, USA). Descriptive statistics, including the frequency distribution, mean, standard deviation, and profile plot, were used to describe the variables. Analytical statistics, including the chi-square test and independent samples t-test, were used to check the homogeneity of the two groups. The repeated measures ANOVA determined the within-subjects, between-subjects, and interaction effects. Subsequently, pairwise comparisons were performed by a post-hoc analysis with a Bonferroni adjustment, and the independent t-test was used to compare the groups. The partial eta squared (np 2) and Cohen's d were calculated to estimate the effect size (ES). For example, for np 2 = 0.01, the ES was small; for np 2 = 0.06, the ES was medium; for np 2 = 0.14, the ES was large; Cohen's d = 0.2 represented a small ES, Cohen's d = 0.5 represented a ES, and Cohen's d = 0.8 represented a large ES. The assumption of a normal distribution of data was analyzed using descriptive evidence and the Kolmogorov–Smirnov test. In addition, the assumption of sphericity was examined using Mauchly's test. The significance level for all tests was < 0.05. The power of the study was assessed to be 90%. In the present study, a mean difference (MD) ≥ 3 points was considered to be clinically significant;27 therefore, a statistically significant difference may not have been clinically significant.
Results
The baseline characteristics of the patients in the intervention and control groups are shown in Table 2. There was no significant difference at baseline between the intervention and control groups (P > 0.05). Based on the results of the repeated measures ANOVA, time was a strong main effect: Ftime (3, 174) = 12.99 (P < 0.001). The interaction effect between the time and group was also statistically significant: Ftime × group (3, 174) = 16.79 (P < 0.001). Therefore, the effect of time in the intervention and control groups was calculated separately (simple effects). The results showed that the effect of time in the intervention group was statistically significant, Ftime (3, 87) = 20.79 (P < 0.001), which meant that the RLS severity in the intervention group decreased with time. In this group, the ES (np 2) = 0.417, which was large, and could explain 41.7% of the variability. In the control group, the effect of time was not statistically significant: Ftime (2.59, 75.24) = 0.546 (P = 0.627). In this group, the ES (np 2) was only 0.018, which meant that it could explain only 1.8% of the variability. The results of a repeated measures ANOVA also showed that the between-subjects effects were statistically significant: Fgroup (1, 58) = 22.41 (P < 0.001). Therefore, the independent samples t-test was used for each of the treatment stages; there were no statistically and clinically significant differences at baseline between the intervention and control groups (P = 0.498, ES = 0.176, MD ≤ 3). However, there were statistically and clinically significant differences between the intervention and control groups at the end of the intervention sessions (i.e., at the end of week 4) (P < 0.001, ES = 2.231, MD = 3.8; Table 3). While there was a statistically significant difference between the intervention and control groups at the 6th week (P < 0.001), this difference was not clinically significant (MD ≤ 3).
Table 2.
Characteristics of patients in the intervention and control groups at baseline.
| Groups | ||
|---|---|---|
|
|
||
| Variables | Intervention | Control |
| Gender | ||
| Male (n=34) | 18 | 16 |
| Female (n=26) | 12 | 14 |
| Age (year) | 56.11 ± 12.66 | 57.36 ± 12.14 |
| Duration of hemodialysis treatment (month) | 35.54 ± 11.18 | 38.21 ± 13.84 |
| Hb (g/dL) | 11.95 ± 0.72 | 11.88 ± 0.85 |
| Hct | 36.18 ± 1.22 | 36.32 ± 1.13 |
| Kt/V | 1.22 ± 0.05 | 1.21 ± 0.06 |
| Iron (μg/dL) | 72.49 ± 8.16 | 69.31 ± 10.61 |
| Underlying diseases | ||
| Diabetes (n=14) | 8 | 6 |
| Cardiovascular disease (n=23) | 12 | 11 |
| Glomerulonephritis (n=9) | 4 | 5 |
| Other (n=14) | 6 | 8 |
Continuous data were expressed as mean ± standard deviation.
Kt/V, dialysis adequacy; Hct, hematocrit; Hb, hemoglobin
Table 3.
Statistical comparison of RLS severity in the intervention and control groups at each phase of intervention.*
| Time | Pre-Intervention | Intervention Sessions | Post-Intervention | ES ( p2) | Pgroup** | Ptime × group** | Ptime** | |
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| Group | Baseline | 2nd week | 4th week | 6th week | ||||
| Intervention group | 23.44±2.51 | 21.41±2.27 | 20.24±1.59 | 21.77±2.85 | 0.417 | < 0.001 | < 0.001 | < 0.001 |
| Control group | 23.84±2.02 | 24.04±2.13 | 24.04±1.81 | 24.17±2.31 | 0.018 | 0.627 | ||
| P value (between-group)*** | 0.498 | < 0.001 | < 0.001 | < 0.001 | ||||
| MD (between-group) | 0.4 | 2.6 | 3.8CS | 2.4 | ||||
| ES (Cohen’s d) | 0.176 | 1.195 | 2.231 | 0.925 | ||||
All data are presented as mean ± standard deviation.
The repeated-measures ANOVA was used.
The independent samples t-test was used.
MD, mean difference; CS, clinically significant (MD ≥ 3 points); ES, effect size
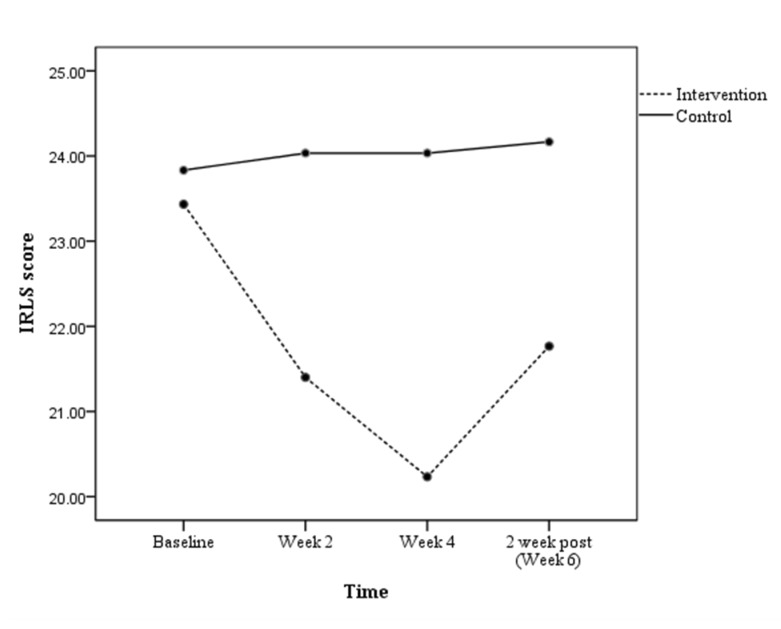
The results of the pairwise comparisons in the intervention group showed statistically and clinically significant differences between the baseline scores and the end of the treatment sessions (week 4) (P < 0.001, ES = 1.484, MD = 3.2; Table 4). This result was clinically significant because the MD ≥ 3 points. However, at the end week 4, after the treatment was discontinued, the mean RLS severity increased and the MD between the baseline scores and the week 6 measurement was not clinically significant (MD ≤ 3) (Figure 2).
Table 4.
Pairwise comparisons in the intervention group.
| Time (I) vs. | Time (J) | MD (I–J) | P value (within-group)* | ES (Cohen’s d) |
|---|---|---|---|---|
| Baseline vs. | 2nd week | 2.03 | P < 0.001 | 1.021 |
| 4th week | 3.20CS | P < 0.001 | 1.484 | |
| 6th week | 1.67 | P < 0.001 | 0.545 | |
|
| ||||
| 2nd week vs. | 4th week | 1.17 | 0.039 | 0.535 |
| 6th week | −0.37 | 1.001 | 0.137 | |
|
| ||||
| 4th week vs. | 6th week | −1.53 | 0.006 | 0.671 |
Bonferroni adjustment was used for multiple comparisons.
Abbreviations: MD, mean difference; CS, clinically significant (MD ≥ 3 points); ES, effect size
Figure 2.
RLS severity scores during the study.
Discussion and Conclusion
The present study showed that the use of NIR light on acupoints in the leg can reduce RLS severity in hemodialysis patients. Mitchell et al18,21,30 also used NIR light to treat patients with RLS, although they did not apply the NIR light to acupoints in the leg. Guffey et al1 investigated the use of NIR light on leg acupoints; however, their study had weaknesses, such as a lack of a control group.
Different principles have been proposed to explain the effect of NIR light therapy. For example, recent evidence suggests that infrared waves result in the release of nitric oxide from vascular endothelium, which improves the peripheral circulation and facilitates and sustains the vasodilatation process. Nitric oxide also acts as a neurotransmitter and is effective in facilitating and sustaining neurotransmission. Therefore, NIR light therapy causes changes in neurotransmitters.1,21,31,32 NIR light therapy also affects pain, which is one of the factors linked to RLS. NIR light changes the permeability of the cell membrane, increases the production of endorphins, and increases the threshold of the action potential in nerve cells, which ultimately leads to pain relief.33 Therefore, NIR light therapy can affect the three factors that are associated with RLS: blood circulation, neurotransmitters, and pain.21,30
There is no well-known mechanism in conventional medicine that can be used to explain how acupoints can be curative; conventional medicine attributes the effect of acupoints to neurological, neurohormonal, and psychological mechanisms.34,35 Therefore, it is necessary to investigate the main mechanism of the effect of acupoints according to traditional Chinese medicine (TCM). TCM states that the mechanism of stimulating the acupoints is linked to the regeneration and balance of vital energy (qi), which contributes to the treatment of diseases.34
The present study attempted to integrate acupuncture treatments with NIR light therapy in order to devise a new therapeutic approach to treat hemodialysis patients with RLS. This approach did not have the common complications seen with acupuncture, such as pain and infection, or the complications seen with conventional medicine. This study used a combination of conventional medicine with TCM, which takes advantage of both approaches.
The present study showed that during the sessions of NIR light therapy, the severity of RLS was reduced significantly. However, the severity of RLS reappeared once the treatment was discontinued. In spite of this, the use of this novel therapeutic approach was preferred to pharmaceutical treatments because the available medications only provide temporary relief and have several complications.15–17 For example, the long-term use of dopamine agonists in the treatment of RLS may lead to drug tolerance and the increased severity of some symptoms.16,17 In contrast, the new acupuncture method introduced in this study did not have any special side effects. Nevertheless, further studies are needed in this regard.
In this study, the reduction of RLS severity was 3.2 points at the end of the intervention sessions, which was clinically significant. Therefore, if this intervention were continued, it is assumed there would be a greater reduction in the severity of RLS. Future studies should investigate the effect of NIR light therapy to acupoints in the legs on reduction of severity of RLS symptoms for study durations longer than 4 weeks.
As the main members of the treatment team for hemodialysis patients, nurses have the most communication with the patients. In a study, Woloshyn36 examined the historical course of light therapy equipment and used the term "Nursing with Flare" to describe the pivotal role of nurses in the use of light and NIR light therapy. The phrase "Nursing with Flare" can be revived and applied to nurses who apply NIR light therapy to acupoints as a palliative and curative treatment, as well as during hemodialysis as part of nursing care.
One of the limitations of this study was the lack of examination of circadian rhythm sleep disorders. Because RLS is classified as a sleep disorder, it would seem necessary to understand the different aspects of a person’s sleep rhythm. Therefore, it is recommended that future studies that measure the RLS severity also conduct an overnight polysomnographic study. Another limitation was that the patients possibly experienced heat when they were treated with NIR and, thus, deduced which group they were assigned. It is recommended that future studies consider this issue in their design.
In conclusion, the current study showed that the application of NIR light therapy to acupoints in the leg effectively reduced the severity of RLS in hemodialysis patients. The results indicate the necessity of holding in-service training for the health care team, especially nurses, so that this technique can be included in the health care program scheduled for hemodialysis patients.
Acknowledgments
We gratefully acknowledge the Kermanshah University of Medical Sciences for their financial support (no. 96407). This work was performed in partial fulfillment of the requirements for the degree of Master of Science in Medical Surgical Nursing of Mohammad Mehdi Mohammadi in the Faculty of Nursing and Midwifery, Kermanshah University of Medical Sciences, Kermanshah, Iran.
References
- 1.Guffey JS, Motts S, Barymon D, et al. Using near infrared light to manage symptoms associated with restless legs syndrome. Physiother Theory Pract. 2016;32(1):34–44. [DOI] [PubMed] [Google Scholar]
- 2.Pérez-Díaz H, Iranzo A, Rye DB, Santamaría J. Restless abdomen: A phenotypic variant of restless legs syndrome. Neurology. 2011;77(13):1283–1286. [DOI] [PubMed] [Google Scholar]
- 3.Stefanidis I, Vainas A, Giannaki CD, et al. Restless legs syndrome does not affect 3-year mortality in hemodialysis patients. Sleep Med. 2015;16(9):1131–1138. [DOI] [PubMed] [Google Scholar]
- 4.Sahli ZT, Jo J, Mousa SA, Tarazi FI. Clinical management of restless legs syndrome in end-stage renal disease patients. CNS Spectr. 2017;22(01):14–21. [DOI] [PubMed] [Google Scholar]
- 5.Hershey LA. Do women with restless legs syndrome have less bone loss? Neurology. 2016;86(13):e144–e146. [DOI] [PubMed] [Google Scholar]
- 6.Hoogwout SJ, Paananen MV, Smith AJ, et al. Musculoskeletal pain is associated with restless legs syndrome in young adults. BMC Musculoskelet Disord. 2015;16(1):294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Winter AC, Berger K, Glynn RJ, Buring JE, Gaziano JM, Schurks M, Kurth T. Vascular risk factors, cardiovascular disease, and restless legs syndrome in men. Am J Med. 2013;126(3):228–35, 35.e1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rodrigues RN, Rodrigues AA, Corso JT, Peixoto TF. Restless legs syndrome associated with cardiac failure and aggravated after valvular replacement: Vespers curse? Arq Neuropsiquiatr. 2008;66(3A):539–541. [DOI] [PubMed] [Google Scholar]
- 9.Haider I, Anees M, Shahid SAH. Restless legs syndrome in end stage renal disease patients on haemodialysis. Pak J Med Sci. 2014;30(6):1209–1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ekbom K, Ulfberg J. Restless legs syndrome. J Intern Med. 2009;266(5):419–431. [DOI] [PubMed] [Google Scholar]
- 11.Razazian N, Azimi H, Heidarnejadian J, Afshari D, Ghadami MR. Gabapentin versus levodopa-c for the treatment of restless legs syndrome in hemodialysis patients: a randomized clinical trial. Saudi J Kidney Dis Transpl. 2015;26(2):271–8. [DOI] [PubMed] [Google Scholar]
- 12.Wilt TJ, MacDonald R, Ouellette J, Khawaja IS, Rutks I, Butler M, Fink HA. Pharmacologic therapy for primary restless legs syndrome: a systematic review and meta-analysis. JAMA Intern Med. 2013;173(7):496–505. [DOI] [PubMed] [Google Scholar]
- 13.Aurora RN, Kristo DA, Bista SR, et al. American Academy of Sleep Medicine. The treatment of restless legs syndrome and periodic limb movement disorder in adults--an update for 2012: practice parameters with an evidence-based systematic review and meta-analyses: an American Academy of Sleep Medicine Clinical Practice Guideline. Sleep. 2012;35(8):1039–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Scholz H, Trenkwalder C, Kohnen R, Riemann D, Kriston L, Hornyak M. Dopamine agonists for restless legs syndrome. Cochrane Database Syst Rev. 2011;(3):CD006009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ondo WG. Restless legs syndrome. Neurol Clin. 2009;27(3):779–799, vii. [DOI] [PubMed] [Google Scholar]
- 16.Ferini-Strambi L, Aarskog D, Partinen M, et al. Effect of pramipexole on RLS symptoms and sleep: A randomized, double-blind, placebo-controlled trial. Sleep Med. 2008;9(8):874–881. [DOI] [PubMed] [Google Scholar]
- 17.Winkelman JW, Johnston L. Augmentation and tolerance with long-term pramipexole treatment of restless legs syndrome (RLS). Sleep Med. 2004;5(1):9–14. [DOI] [PubMed] [Google Scholar]
- 18.Mitchell UH. Use of near-infrared light to reduce symptoms associated with restless legs syndrome in a woman: a case report. J Med Case Reports. 2010;4(1):286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ebneshahidi NS, Heshmatipour M, Moghaddami A, Eghtesadi-Araghi P. The effects of laser acupuncture on chronic tension headache - a randomised controlled trial. Acupunct Med. 2005;23(1):13–18. [DOI] [PubMed] [Google Scholar]
- 20.Round R, Litscher G, Bahr F. Auricular acupuncture with laser. Evid Based Complement Alternat Med. 2013; 2013:984763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mitchell UH, Johnson AW, Myrer B. Comparison of two infrared devices in their effectiveness in reducing symptoms associated with RLS. Physiother Theory Pract. 2011;27(5):352–359. [DOI] [PubMed] [Google Scholar]
- 22.Al Rashoud AS, Abboud RJ, Wang W, Wigderowitz C. Efficacy of low-level laser therapy applied at acupuncture points in knee osteoarthritis: a randomised double-blind comparative trial. Physiotherapy. 2014;100(3):242–248. [DOI] [PubMed] [Google Scholar]
- 23.Lin M-Y, Fu C-T, Hsueh S-C. Incremental update on probabilistic frequent itemsets in uncertain databases. In: Proceedings of the 6th International Conference on Ubiquitous Information Management and Communication; February 20–22, 2012; Kuala Lumpur, Malaysia. Article No. 75. 10.1145/2184751.2184841. [DOI] [Google Scholar]
- 24.Baxter GD, Bleakley C, McDonough S. Clinical effectiveness of laser acupuncture: a systematic review. J Acupunct Meridian Stud. 2008;1(2):65–82. [DOI] [PubMed] [Google Scholar]
- 25.Aliasgharpour M, Abbasi Z, Pedram Razi S, Kazemnezhad A. The effect of stretching exercises on severity of restless legs syndrome in patients on hemodialysis. Asian J Sports Med. 2016;7(2):e31001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Habibzade H, Khalkhali H, Ghaneii R. Study of the relationship between restless legs syndrome and sleep disturbance among patients in Critical Care Units. Iranian Journal of Critical Care Nursing. 2011;4(3):153–158. Available at: http://pdfarchive.ir/pack-16/Do_40113900308.pdf Last accessed May 24, 2018. [Google Scholar]
- 27.Allen RP. Minimal clinically significant change for the International Restless Legs Syndrome Study Group rating scale in clinical trials is a score of 3. Sleep Med. 2013;14(11):1229. [DOI] [PubMed] [Google Scholar]
- 28.Food and Drug Administration. 510(k) Summary for narrow band, near-IR energy, pain therapy devices. 510(k) Number: K042813. February 23, 2005. Available at: https://www.accessdata.fda.gov/cdrh_docs/pdf4/K042813.pdf Accessed May 17, 2017.
- 29.Syrolight. BioBeam 940: features and advantages. Available from: http://www.syrolight.com/biobeam-940/features Last accessed: May 24, 2018.
- 30.Mitchell UH, Myrer JW, Johnson AW, Hilton SC. Restless legs syndrome and near-infrared light: An alternative treatment option. Physiother Theory Pract. 2011;27(5):345–351. [DOI] [PubMed] [Google Scholar]
- 31.Falaki F, Nejat AH, Dalirsani Z. The Effect of Low-level Laser Therapy on Trigeminal Neuralgia: A Review of Literature. J Dent Res Dent Clin Dent Prospects. 2014;8(1):1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mitchell UH, Mack GL. Low-level laser treatment with near-infrared light increases venous nitric oxide levels acutely: a single-blind, randomized clinical trial of efficacy. Am J Phys Med Rehabil. 2013;92(2):151–156. [DOI] [PubMed] [Google Scholar]
- 33.Hawkins D, Abrahamse H. Phototherapy—a treatment modality for wound healing and pain relief. Afr J Biomed Res. 2007;10:99–109. [Google Scholar]
- 34.Cui Y, Wang Y, Liu Z. Acupuncture for restless legs syndrome. Cochrane Database Syst Rev. 2008;(4):CD006457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Smith CA, Hay PP. Acupuncture for depression. Cochrane Database Syst Rev. 2005. April 18;(2):CD004046. [DOI] [PubMed] [Google Scholar]
- 36.Woloshyn TA. Nursing with flare: The operators of light therapy, c.1890–1940. Dermatol Nurs (Lond). 2016;15(1):47–52. [PMC free article] [PubMed] [Google Scholar]