Abstract
AIM:
The study aimed to determine the effects of the health promotion toolkit on empowering families caring for children with developmental disability. It hypothesised that health promotion toolkit would effectively improve families’ empowerment and alleviate parental stress.
METHODS:
The research design was quasi-experimental. A convenience sample of 30 children with DD and their families enrolled at Shoaa ElAmal Center in Umluj participated. Tools were Health Promotion Assessment Sheet, Family Empowerment Scale, and the Parent Stress Index.
RESULTS:
The results documented significant lower levels of parental stress and higher levels of family empowerment among mothers at posttest than pretest. A significant negative correlation between family empowerment and parental stress was reported.
CONCLUSION:
Health promotion toolkit had a positive effect on empowering families as well as lowering parental stress. Recommendation Health promotion toolkit should be integrated as a monitoring method of health care needs of health promotional activities for children with developmental disabilities.
Keywords: Developmental disabilities, Health promotion, empowerment
Introduction
Developmental disability is a major health concern. It includes a wide range of impairments that begin before the age of 18 years. These impairments include physical, intellectual and behavioural domains of development that may affect day-to-day functioning [1]. An American study showed that about one in six or about 15% of children have at least one type of developmental disabilities. They include physical disabilities, sensory-related disabilities, communication disabilities and intellectual disabilities [2].
Intellectual disability is a complex phenomenon refers to the mental ability and self-care skills that are below the expected level of an individual’s age [3]. It results in significant deficits at an intellectual level in addition to adaptive skills [4] [5].
Approximately, 10% of the population in developed countries and 12% of the population in developing countries are disabled [6]. In Saudi Arabia, The prevalence MR is 8.9 per 1000 children [7]. Another study reported that mental retardation was the most common neurological disorder among Saudi children with a prevalence rate of 26.3 per 10000. The researchers stressed the priority for health care planning for those children [8]. As they are at high risk for adverse health conditions such as epilepsy, neurological, gastrointestinal and behavioural disorders [9]. Generally, they have poor or fair health status [10]. However, children who received early intervention, adequate education, appropriate supports and sustained care generally have improved life outcomes. In fact, they can live independently with family support [11].
Pediatric nurses are vital in providing support to families caring for a child with intellectual disabilities. To build the necessary supportive and collaborative relationships with those families, nurses should understand the concept of empowerment and its’ process [12]. Empowerment concept is widely used in health sciences particularly nursing [13].
Family empowerment is upheld as a creative strategy to provide high quality of care for chronic childhood illnesses and intellectual disabilities across a family-centred care approach [14] [15]. This approach of care delves into providing the effective family strategies that adequate care and support intellectually disable children [16].
In other words, educating parents about their child’s condition, teaching them the needed new skills, offering and providing them with the support services they need is known as empowerment strategies [17]. Hence, empowerment strategies possess the essence of health promotion that is about “enabling individuals to take control over their health and its determinants that improve their health. Thereby, they will be able to live an active and productive life [18]. Additionally, health promotion maintenance is a method utilised to maintain and enhance the existed levels of health through the implementation of effective programs, services and policies [19].
It includes health teaching, decision-making, supportive activities (screening, self-care skills, advocating for environmental change, positive health behaviours, and choices) and supportive policies in work and community settings. Therefore, health promotion categorised into three activities: prevention, protection and health education [20].
As the goals of nursing care for developmentally disabled children with are to promote their optimal social, physical, cognitive and adaptive development [21], pediatric rehabilitation nurses must be a part of the interdisciplinary team that can establish an effective management plan. They can help to maximise children’s potential by advocating, health teaching, promoting and coordinating health promotion practices as supportive care intervention [22].
Although the prevalence of developmental disabilities particularly, intellectual in Saudi Arabia is similar to that reported in other countries [7] [8], limited studies are conducted. Also, there are various obstacles when researching disability field in Saudi Arabia [23].
Moreover, the cost of preventive efforts is significantly lesser than the management of expected complication; thus, cost-effectiveness favours the prevention approach [24]. The earlier the health/rehabilitative care is delivered, the more the chance of reducing the effect of disability and its’ expected complication, and the more quality of life of the person [25].
Therefore, the current study could be of great help for the development of comprehensive strategies for improvement of the quality of life for families that have one or more child with intellectual disability. For these reasons, this study was conducted to determine the effectiveness of health promotion toolkit on empowering families caring for developmentally disabled children.
Research question
1. What are the effects of a health promotion toolkit on empowering families caring for children with developmental disabilities?
This study aimed to determine the effectiveness of a health promotion toolkit for children with developmental disabilities on the family empowerment.
Research Objectives
Identify basic health-care needs of children with developmental disabilities.
Set a health promotion toolkit for promoting the health of children with developmental disabilities.
Examine parental stress among families caring for children with developmental disabilities.
Hypothesis
Health promotion toolkit would effectively improve families’ empowerment.
Utilization of the health promotion toolkit would alleviate parental stress.
Methodology
The current study utilised a quasi-experimental design.
The study carried out at Shoaa El-Aml day care centre for disabled children in Umluj city at Tabuk region KSA. It is a non-profit organisation licensed by the Ministry of work.
The researcher calculated the sample size by the formula: n = [(Zα)2*(S)2]÷d2 at a confidence level of 0.95 and test power 80%. Where n is the sample size, Zα is the level of confidence, S is the standard deviation and d is the desired precision. The estimated sample size was 138 participants, however; the convenient number was 30 children and their families. They were included based on inclusion criteria (a) children who had a diagnosis of developmental disabilities, (b) age ranges between 3-18 years and (c) IQ ranges 50-70. The researcher excluded children who had chronic renal failure and those who enrolled in a health education program during the last 3 months.
The Research Ethics committee at the Deanship of the academic research at Tabuk University granted ethical approval for this research. The researcher clarified the objectives, importance, and safety of the study to participants. Therefore parents were voluntary participate and assured confidentiality of their data.
The researcher utilised three tools for data collection, they include:
-
Tool one: Health promotion Assessment sheet. It is a structured interview questionnaire designed by the researcher to assess the current health status of children and mother’s knowledge about developmental disabilities. It consisted of four parts.
- a) Part one included data about children characteristic such as gender, age, weight, height, parental age, education and occupation and family number.
- b) Part two included data regarding medical history, immunisation, health problems and dental problems.
- c) Part three included self-care skills, social problems, behavioural problems, physical activity and eating habits and safety.
-
d) Part four contained data regarding mothers’ perception of their children health and their knowledge about developmental disabilities.Scoring system: - Scores for the evaluated items (health problems, medical history, dental problems, behavioral problems, social problems and safety) are absent (3), to some degree (2) and present (1); - Scores for self-care skills are independent (3), partially dependent (2) and completely dependent (1); - Scores for mothers’ knowledge are complete (3), incomplete (2) and wrong (1).
Tool two: Family Empowerment Scale (FES) that developed by Koren [26]. The scale consisted of three subscales that related to family, child’s services and parents’ involvement in the community. The items of the scale ranged from 1 (never) to 5 (very often). Scores above 30 on the family and child’s services sub-scales and above 25 on the parents’ involvement in the community sub-scale indicated empowered families. Total scores on FES were 170 points. Scores above 85 indicate significant familial empowerment.
Tool Three: “Parent Stress Index-Short Form” developed by Abidin [27]. It is a 36-item self-reported questionnaire developed to measure parental stress. It composed of three domains that are parent-distress (PD); parent-child dysfunctional interaction (PCDI); and difficult child (DC). The items of the scale range from 1 (strongly disagree) to 5 (strongly agree). Scores above 33 on the PD and DC sub-scales and above 27 on the PCDI sub-scale are considered clinically elevated. Total score of the scale was 180 points. Scores above 90 indicate significant high level of parental stress.
Validity and reliability
Once the researcher adopted or designed the tools for data collection, she tested its content validity. Three experts in pediatric nursing and a paediatrician ascertain their relevance and completeness.
Reliability of the tools was determined to assess the extent to which items were related to each other. The reliability of Health Promotion Assessment tool was r = 0.69 by Cronbach’s test. Koren [32] documented that Family Empowerment Scale has adequate internal consistency for each of the three subscales (Family: α = 0.88; Service System: α = 0.87; Community/Political: α = 0.88). The test-retest reliability was also found to be adequate for the three subscales (Family: r = 0.83; Service System: r = 0.77; Community/Political: r = 0.85). Abidin [33] confirmed the reliability of the parent stress index by Test-retest reliability coefficients that was 0.84 and by Cronbach’s test was (r = 0.68).
Data collection and procedure
Written permission: The researcher attained an authorisation from Shoaa El-Aml Day Care Center to conduct the study after explaining the purpose of the study and methods of data collection.
Pilot study: A pilot study carried out on 10 mothers to assure clarity, consistency and feasibility of the tools. The researcher did not modify the tools.
-
Procedure: Data collection process is starting from March 2017 to September 2017 and contained three phases:
- Phase I (assessment phase): children and parents assessment were performed to obtain baseline data regarding children and parents’ characteristics, parents’ knowledge about developmental disabilities, parent’s perception of children overall health, children self-care skills, health problems and/or symptoms, behavioral problems, dental health, children safety, parents’ stress level and empowerment level. Referral to Umliuj hospital was done for five children.
- Planning Phase: the researcher designed health promotion toolkit. It consisted of educational and training sessions for mothers which developed based on the identified areas of weakness in mothers’ knowledge and health practices; it included the number of sessions, content and methods of teaching. The objectives for health promotion toolkit were set as follows.
General objective
To provide mothers with knowledge, skills and positive attitudes toward caring for children with developmental disabilities.
Specific objectives
By the end of the educational sessions, mothers would be able:
To list the causes and types of developmental disability.
To identify how to manage different stressors adaptively.
To explain how to manage different behavioural problems.
To determine the methods used for managing enuresis.
To utilise the healthy eating pyramid for planning healthy meals.
To follow the steps of prevention of infectious diseases.
To perform first aids skills for children.
To apply safety measures for children.
To show a positive attitude toward the importance of periodic checkup for children.
To show a positive attitude toward the importance of dental care and hygiene.
-
To show a positive attitude toward the importance of physical activity.
iii. Implementation Phase: The health promotion toolkit implemented in the training unit at Shoaa ElAmal Day Care Center. The program implemented for five days with three educational and training sessions per day. Each session lasted from 30 to 45 minutes. Each session contained from 10-20 mothers. The researcher utilised think-pair-share, workshop, discussion, storytelling, debate, roleplaying, and demonstration teaching strategies. Also, PowerPoint presentation, videos, first aids’ manikin, brochures, colouring books for children and dental care equipment teaching aids. These sessions held based on the four steps of family empowerment model which were:
a) Knowledge increase
During this stage, the researcher meant to increase mothers’ knowledge. Mothers were assigned to four groups in which five mothers/group. The researcher discussed the following topic: concept of developmental disabilities, causes, types, diseases associated with or caused by developmental disabilities, prevention of infectious diseases, periodic checkup schedule for children, dental health and care, healthy eating, physical activity, children safety, first aids skills, management of behavioral problems, enuresis management and stress management.
b) Improvement of self-efficacy
Once the researcher completed the content of the training sessions, she asked mothers to demonstrate the learned practical skills. Their participation and achievement increase their self-efficacy and encourage them to learn more.
c) Increase self-esteem
At this phase, the researcher asked mothers who achieved the trained skills correctly to train another mother who could not demonstrate the skill. Therefore, they actively participated in the education process that improves their self-esteem.
d) Process evaluation
By the end of each session, the researcher got oral feedback from the mothers by asking questions and allowed free comments. Also, demonstration of selected skills.
iv. Evaluation Phase
Mothers’ knowledge, stress and level of empowerment were evaluated after completion of the sessions.
Data Analysis
The collected data were coded for entry and analysis. The researcher utilised IBM Statistical Package for Social Science (SPSS) statistical package version 19 for data analysis and Excel program for graphic design.
Data analysed by the mean (X), standard deviation (SD), one-way ANOVA, frequency distribution, chi-square (χ2) test. However, if the expected value of any cell in the table was less than 5, the researcher utilised the Fisher Exact test. The P-value < 0.05 was the set level of significance for all statistical tests.
Results
Table 1 shows the distribution of parents according to their characteristics. As indicated in the table, the mean and standard deviation of mothers’ age was 39.33 ± 7.67 and 44.93 ± 7.99 for fathers. Approximately half of the mothers (56.7%) can read and write. Meanwhile, 56.7% of the fathers were illiterate. For occupation, most of the mothers (90%) did not work and about half of the fathers (53.3%). More than half of families (53.3%) have a family number > 5-8 members.
Table 1.
Distribution of parents according to their characteristics
| Biosocial characteristics of studied parents | No | % |
|---|---|---|
| Age | Mean ± SD | |
| Mothers | 39.33 ± 7.67 | |
| Fathers | 44.93 ± 7.99 | |
| Mother’s Education level | ||
| Illiterate | 0 | 0 |
| Read and write | 17 | 56.7 |
| Secondary | 8 | 26.7 |
| University | 5 | 16.7 |
| Father’s Education level | ||
| Illiterate | 17 | 56.7 |
| Read and write | 9 | 30.0 |
| Secondary | 4 | 13.3 |
| University | 0 | 0 |
| Mother’s occupation | ||
| Work | 3 | 10.0 |
| Don’t work | 27 | 90.0 |
| Father’s occupation | ||
| Work | 16 | 53.3 |
| Don’t work | 14 | 46.7 |
| Family Number | ||
| 3-5 | 9 | 30.0 |
| >5-8 | 16 | 53.3 |
| >8 | 5 | 16.7 |
Figure 1 shows the distribution of families according to their income. It clarified that approximately 73% of families have an insufficient income per month.
Figure 1.

Distribution of families according to Family income
Table 2 shows the characteristics of the developmentally disabled children. It demonstrated that the mean age of children was 7.36 and more than half of them were boys (53.3%). The mean and standard deviation of their weight was 21.53 ± 5.9. For height, it was 99.32 ± 16.12. More than one-third of children diagnosed as mentally retarded.
Table 2.
Characteristics of developmentally disabled children
| Characteristics of Children | No | % |
|---|---|---|
| Mean ± SD | ||
| Age | 7.36 ± 2.98 | |
| Gender | ||
| Girls | 14 | 46.7 |
| Boys | 16 | 53.3 |
| Weight | 21.53 ± 5.9 | |
| Height | 99.32 ± 16.12 | |
| Diagnosis | ||
| Autism | 7 | 23.3 |
| Down syndrome | 7 | 23.3 |
| Attention Deficient Hyperactivity | 5 | 16.7 |
| Mental Retardation | 11 | 36.7 |
Figure 2 clarified mothers’ perception regarding their children health. It demonstrated that about half of mothers (53.3%) perceive good health of children and only 10 % perceive fair health.
Figure 2.
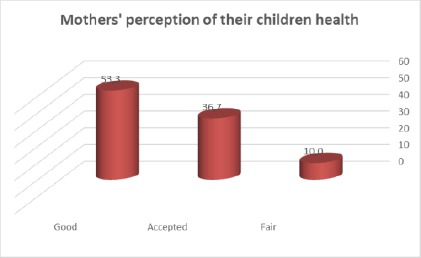
Mothers’ perception regarding their children health
Figure 3 shows mothers’ knowledge about developmental disabilities at pretest and posttest. It calcified that there was an improvement in knowledge of mothers’ about developmental disabilities at posttest than on pretest. For this reason, there was the statistical significant difference at 5% levels of statistical significance.
Figure 3.
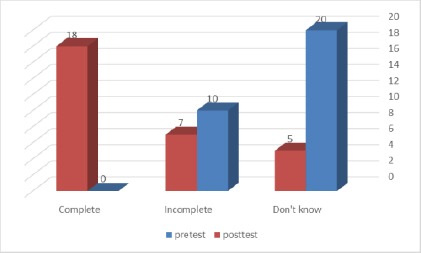
Mothers’ knowledge about developmental disabilities at pretest and posttest
Table 3 describes the health problems among children with developmental disabilities. It illustrated that more than half of children (56.7%) have dental problems, more than a third of children (46.7%) have convulsion and more than half of children (60%) suffer from enuresis. Approximately one-third of children (36.7%, 33.3%) has fatigue and pain symptoms. For the sleep problem, 16.5 % of children have sleep problems.
Table 3.
Health problems among children with developmental disabilities
| Health problems | No (N = 30) | % |
|---|---|---|
| Dental problems | 17 | 56.7 |
| Convulsions | 14 | 46.7 |
| Enuresis | 18 | 60 |
| Fatigue | 11 | 36.7 |
| Pain | 10 | 33.3 |
| Sleep problems | 5 | 16.5 |
Table 4 shows the distribution of common problems among children with developmental disabilities. It revealed that more than half of children (53.3%) have some independence in performing self-care skills and approximately one third (40%) were independent.
Table 4.
Distribution of problems among children with developmental disabilities
| Health problems | No (N = 30) | % |
|---|---|---|
| Self-care skills | 12 | 40 |
| Independent | 16 | 53.3 |
| Some independence | 2 | 6.7 |
| Dependent | ||
| Mean ± SD | 14.8 ± 4.86 | |
| Behavioural problems | 23 | 76.7 |
| Self-injuries behaviours | 28 | 93.3 |
| Others- injuries behaviours | 15 | 50 |
| Masturbation | 3 | 10 |
| Mood fluctuation | 20 | 66.7 |
| Social problems | 20 | 66.7 |
| Hyperactivity | 19 | 63.3 |
| Agitation | 16 | 53.3 |
| Fear and anxiety | 15 | 50 |
The majority of children (76.7%, 93.3%) have behavioural problems and self-injury behaviours. Meanwhile, two-thirds of children (66.7%) have mood fluctuation and social problems. Moreover, more than half of children (63.3%, 53.3%, and 50%) have hyperactivity, agitation and fear and anxiety problems consequently.
Table 5 demonstrates the means and standard deviations of parental stress on pretest and posttest. It clarified that mothers at posttest had lower levels of parental distress (34.0 ± 5.45), parent-child dysfunctional interaction (33.63 ± 4.9), difficult child (33.1 ± 2.26) and total parent stress index score (101.46 ± 10.48). There were high statistical significant differences between levels of parental stress among mothers at pretest and posttest.
Table 5.
Means and Standard deviations of Parents Stress on Pretest and Posttest
| Parent stress index | Pre-test (n = 30) X ± SD | Post-test (n = 30) X ± SD | ANOVA test | P-value |
|---|---|---|---|---|
| Parental Distress | 38.63 ± 7.13 | 34.0 ± 5.45 | 97.33 | <0.001** |
| Parent–Child Dysfunctional Interaction | 37.3 ± 6.07 | 33.63 ± 4.9 | 31.79 | <0.001** |
| Difficult child | 37.3 ± 3.24 | 33.1 ± 2.26 | 12.0 | <0.001** |
| Total Parent stress index score | 113.33 ± 12.12 | 101. 46 ± 10.48 | 15.95 | <0.001** |
Table 6 shows the means and Standard deviations of family empowerment on pretest and posttest. It clarified that mothers at posttest had the highest levels of family empowerment scores (105.0 ± 16.48). Moreover, mothers at posttest demonstrated high levels of empowerment within the three subscales family (42.06 ± 4.79), child’s services (37.66+8.16) and parents’ involvement in the community (25.73 ± 8.14). Therefore, the difference between the levels of family empowerment among mothers at pretest and posttest was statistically significant.
Table 6.
Means and Standard deviations of family empowerment on pretest and posttest
| Family Empowerment | Pre-test (n = 30) X- ± SD | Post-test (n = 30) X- ± SD | ANOVA test | p-value |
|---|---|---|---|---|
| Family | 30.0 ± 3.15 | 42.06 ± 4.79 | 2.44 | 0.045 <0.01* |
| Child’s services | 28.66 ± 4.06 | 37.66 ± 8.16 | 2.67 | 0.034<0. 01* |
| parents’ involvement in the community | 23.6 ± 4.94 | 25.73 ± 8.14 | 2.79 | 0.027<0. 01* |
| Total Family Empowerment score | 82.6 ± 8.33 | 105.0 ± 16.48 | 2.87 | 0.049 |
| <0.01* |
P < 0.05.
Table 7 clarifies the Pearson correlation test between parental stress and family empowerment subscales on the posttest. It clarified that there was a highly statistically significant negative correlation between parental stress index score and family empowerment total score (r = -0.439), family (r = -0.51) and parents’ involvement in the community (r = -0.476) on posttest at 1% level of significance. Also, parent stress was not statistically correlated to child’s service subscale (r = -0.083) of family empowerment.
Table 7.
Pearson correlation test between parental stress and family empowerment subscales on the posttest
| Parameter | Parent stress index Score | |
|---|---|---|
| R | p-value | |
| Family | -0.51 | 0.004 |
| <0.001** | ||
| Child’s services | -0.083 | 0.66ns |
| parents’ involvement in the community | -0.476 | 0.008 |
| <0.001** | ||
| Total Family Empowerment score | -0.439 | 0.015 |
| <0.001** | ||
nsP > 0.05; *P<0.05; **P<0.001.
Figure 4 shows the Pearson correlation between parental stress and family empowerment on the posttest. It illustrated that there was a negative correlation at 1% between family empowerment and parental stress index on the posttest.
Figure 4.
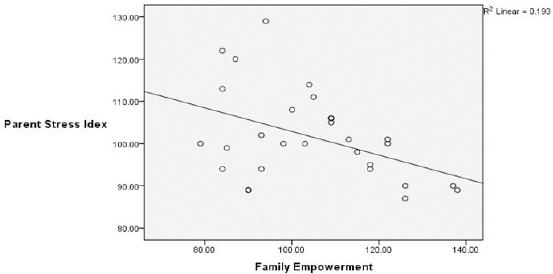
Pearson correlation between parental stress and family empowerment on the posttest
Discussion
Developmental disability is a major health concern. It includes a wide range of impairments that begin before the age of 18 years. These impairments may affect day-to-day functioning. Developmentally disabled children have high rates of adverse health conditions such as neurological, gastrointestinal disorders and generally, poor health status [9] [10]. Therefore, nurses should promote and coordinate health promotion practices to maximise children potential. However, a family is a central component in their children’s life. Nurses should empower those families to maintain and enhance the existing levels of their children health and thereby being able to live an active and productive life [18]. The current study hypothesised that health promotion toolkit would effectively improve families’ empowerment and utilisation of the health promotion toolkit would alleviate parental stress.
Concerning children characteristics, the current study revealed that the mean age of children 7.36 years and more than half (53.3%) of children were boys. These findings are consistent with the finding of a Saudi survey conducted by El-Hzmi et al., [7]. They found that 53.2 % of studied children were males. In agreement with Mash and Wolfe [28] who indicated that the prevalence rate of mental handicapping conditions among boys is about one-half times more than girls are. Also, they demonstrated that the majority of children (70%) were in 5-15 years age group that is consistent with the children’s mean age (7.36 years) of the current study.
Regarding parents’ level of education, the results of the current study revealed that approximately half (56.7%) of mothers and 30% of fathers were read and write meanwhile, 56.7% of fathers were illiterate. These findings are consistent with Ghoneim et al., [29] who demonstrated that about half (52.7% & 58.1%) of fathers and mothers were without educational qualifications. This reflects that perhaps those families need to know more information regarding developmental disabilities and its care.
Concerning frequency of health problems among children with developmental disability, findings of the current study illustrated numerous problems that were dental problems (56.7%), convulsions (46.7%), enuresis (60%), fatigue (36.7%) and pain (33.3%). In addition, self-injuries behavior (93.3%), behavioral problems (76.7%), social problems (66.7%), mood fluctuation (66.7%), hyperactivity (63.3%), self-care deficit (53.3%) with a mean and standard deviation 14.8 ± 4.86, agitation (53.3%) and anxiety (50%).
These findings are congruent with studies conducted by Moes et al., [30], Abbeduto et al., [31] who reported the great prospect of behaviour problems in children with DD. Moreover, Yousef et al., [32] documented that mentally disabled children had behavioural, emotional, speech and language problems. They stated that impulsivity comprised 55.5% of behavioural problems and 56.3% of children suffered from social problems. Also, Ghoneim et al., [29] reported that mentally disabled children suffered from problems related to growth and development, mood, behavioural and social.
The presence of these problems provides a further challenge and a potential source of stress to the family. Identification of these problems will help in recognising and enhancing parents’ abilities to meet their children needs solve their problems and mobilise the necessary resources [33].
Regarding mothers’ perception of their children health, the current study documented that more than half (53.3%) of mothers perceived good health for their children and only 10% perceived fair health although those children had numerous health problems.
These findings could be related to traditions that impose mothers to hinder the actual health complaints of developmentally disabled children to protect them from social stigma. Moreover, some mothers still denial that her child has any developmental disability. Another reason could be attributed to inadequate mothers’ awareness regarding their children health. This explanation is supported by another finding in the present study that two thirds (66.6%) of mothers did not know adequate knowledge about developmental disabilities before implementing the health promotion toolkit.
Regarding parental stress, findings of the current study revealed that parental distress levels were high in all three subscales and the total score of the Parent Stress Index. The mean and stander deviation of parental distress was (38.63 ± 7.13), parent-child dysfunctional interaction (37.3 ± 6.07), difficult child (37.3 ± 3.24) and total parent stress index score (113.33 ± 12.12). These results are consistent with the findings by Dardas and Ahmed [34]. They clarified that the highest score among the three subscales of parent stress index was PD (40.29) meanwhile; the lowest was PCDI (37.7).
Moreover, the scores of parental stress equal to or higher than 85th percentile that was pathologically high [35]. Also, high mean scores on child domain (132.38 ± 24.01) and parent domain (132.38 ± 26.13) of the PSI were documented [36]. Moreover, in agreement with Estes et al., [37] who proved the evidence for high levels of parent stress and psychological distress among parents of children with developmental disability.
This high level of parental stress could attribute to the fact that families of children with developmental disability have multiple demands on family resources. Another reason could be related to lack of sufficient income or adequate knowledge about developmental disabilities and access to community resources. This explanation was supported by the findings of the present study where the majority of families reported insufficient income and two-thirds of mothers lack adequate knowledge about developmental disabilities.
Concerning family empowerment, the current study revealed that mothers at posttest had significantly high levels of family empowerment total scores (105.0 ± 16.48) and within the three subscales family (42.06 ± 4.79), child’s services (37.66 ± 8.16) and parents’ involvement in the community (25.73 ± 8.14).
In agreement with Minjarez et al., [38], these findings were consistent with their pretest-posttest study in which they concluded that rating on family empowerment scale showed a significant change from pre to post-treatment indicating an increased level of family empowerment.
These findings are supported by the point of view of Dempsey and Dunst [39] who stated that enabling practices perceived as the prominent predictive variable of families’ empowerment regardless of demographics. This could be attributed to the fact that educational programs increase mothers’ knowledge and in turn change their practices and attitudes to become more adaptive. In other words, they indirectly empowered to provide adequate care for their children.
About the Pearson correlation test between parental stress and family empowerment subscales on the posttest. There was a high statistical significant negative correlation between parental stress index score and family empowerment total score (r = -0.439), family (r = -0.51) and parents’ involvement in the community (r = -0.476) on the posttest. These findings were consistent with Minjarez et al. who reported that parents felt a high level of empowerment when they had a low level of stress [38].
Also, behavioural problems of children associated with high levels of parental stress had a negative effect on family empowerment [36]. Moreover, a correlational analysis between FES and PSI scales’ confirmed the presence of a linear inverse relationship between parental stress and empowerment [40].
Finally, the findings of the current study clarified that health promotion toolkit had a positive effect on empowering families as well as lowering parental stress. Therefore, health promotion toolkit should be utilised as an approach for empowering families caring for children with developmental disabilities in Tabuk.
Recommendation
Health promotion toolkit should be integrated as a monitoring method of health care needs of health promotional activities for children with developmental disabilities.
Scientifically established clinical pathway of managing developmental disabilities using health promotion toolkit should be designed.
Home visits programs should be designed for families of developmentally disabled children to assess and meet their health needs based on implementing health promotion toolkit.
Establishing a support system for children with developmental disabilities and their families in Umulij and its surrounding villages through coordination between Ministry of Health, Tabuk University, and Shoaa El Aml Day Care Center.
Establishing a unit and/or outpatient clinic at Umlij general hospital provide sustained health and medical care for children with developmental disabilities.
Establishing societies in Umlij city to care for those families and their children.
-
The current study needs to be applied to a wider range of sample to ensure the generalizability of results.
The current study concluded that mothers of developmentally disabled children had high levels of parental stress and low levels of familial empowerment. Those levels are improved after implementing health promotion toolkit in which parental stress level is decreased, and familial empowerment level is increased. Also, a negative correlation between family empowerment and parent stress had been reported.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Center for Disease Control and Prevention. Developmental Disabilities [Internet]. National Center on Birth Defects and Developmental Disabilities. 2015. Sep 8, [[updated 2017 April 21; cited 2017]]. Available from: www.cdc..gov/ncbddd .
- 2.Boyle CA, Boulet S, Schieve L, Cohen RA, Blumberg SJ, Yeargin Allsopp M, Visser S, Kogan MD. Trends in the Prevalence of Developmental Disabilities in US Children 1997–2008. Pediatrics. 2011;27:1034–1042. doi: 10.1542/peds.2010-2989. https://doi.org/10.1542/peds.2010-2989 PMid:21606152. [DOI] [PubMed] [Google Scholar]
- 3.Batshaw ML. Children with Disabilities. 5th ed. Paul H, Brookes Publishing comp; 2002. Retrieved from: http://www.dbeds.org . [Google Scholar]
- 4.Ansberry C. Erasing a Hurtful Label from the Books:Decades-long quest by disabilities advocates finally persuades state, federal governments to end official use of retarded. Wall Street Journal. (New York). Sect. US (col.1) 2010 [Google Scholar]
- 5.Wilmshurst L. General learning disability Clinical and Educational Child Psychology an Ecological-Transactional Approach to Understanding Child Problems and Interventions. Hoboken: Wiley; 2012. p. 168. https://doi.org/10.1002/9781118440728. [Google Scholar]
- 6.Verep S. Affect of nursery education given to mothers of the children with mental disability to decrease mothers'fatigue [Master Thesis] [Erzurum, Türkiye]:Atatürk University, Graduate School of Health Sciences. 2005 [Google Scholar]
- 7.El-Hazmi MA, Al-Swailem AA, Al-Mosa NA, Al-Jarallah AA. Prevalence of mental retardation among children in Saudi Arabia. East Mediterr Health J. 2003;9(1-2):6–11. PMid:15562727. [PubMed] [Google Scholar]
- 8.Al Salloum AA El, Mouzan MI, Al Omar AA, Al Herbish AS, Qurashi MM. The prevalence of neurological disorders in Saudi children:a community-based study. J Child Neurol. 2011;26(1):21–24. doi: 10.1177/0883073810371510. https://doi.org/10.1177/0883073810371510 PMid:21212450. [DOI] [PubMed] [Google Scholar]
- 9.Krahn GL, Fox MH. Health disparities of adults with intellectual disabilities. JARID. 2013;27(5):431–446. doi: 10.1111/jar.12067. PMid:23913632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haider SI, Ansari Z, Vaughan L, Matters H, Emerson E. Health and wellbeing of Victorian adults with intellectual disability compared to the general Victorian population. Research in Developmental Disabilities. 2013;34(11):4034–4042. doi: 10.1016/j.ridd.2013.08.017. https://doi.org/10.1016/j.ridd.2013.08.017 PMid:24036484. [DOI] [PubMed] [Google Scholar]
- 11.American Association on Intellectual & Developmental Disabilities. Intellectual Disability:Definition, Classification, and Systems of Supports. 11th Ed. Washington DC: American Association on Intellectual & Developmental Disabilities; 2011. [Google Scholar]
- 12.Gibson CH. A Study of Empowerment in Mothers of Chronically ill Children. [Dissertation]:Boston College. 1993 [Google Scholar]
- 13.Mugno D, Ruta L, Genitori D'Arrigo V, Mazzone L. Impairment of quality of life in parents of children and adolescents with pervasive developmental disorder. Health and Quality of Life Outcomes. 2007;(5):22. doi: 10.1186/1477-7525-5-22. https://doi.org/10.1186/1477-7525-5-22 PMid:17466072 PMCid:PMC1868708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coyne I. Disruption of parent participation:Nurse's strategies to manage parents on children's wards. JCN. 2007;(17):3150–3158. doi: 10.1111/j.1365-2702.2006.01928.x. [DOI] [PubMed] [Google Scholar]
- 15.Jolley J, Shields L. The evolution of family-centered cure. Journal of Pediatric Nursing. 2009;24(2):164–170. doi: 10.1016/j.pedn.2008.03.010. https://doi.org/10.1016/j.pedn.2008.03.010 PMid:19268238. [DOI] [PubMed] [Google Scholar]
- 16.Bagner DM, Eyberg SM. Parent-child interaction therapy for disruptive behavior in children with mental retardation:A randomized controlled trial. JCCAP. 2007;(36):418–429. doi: 10.1080/15374410701448448. [DOI] [PubMed] [Google Scholar]
- 17.Panicker L. Nurses'perceptions of parent empowerment in chronic illness. Contemporary Nurse. 2013;45(2):210–219. doi: 10.5172/conu.2013.45.2.210. https://doi.org/10.5172/conu.2013.45.2.210 PMid:24299249. [DOI] [PubMed] [Google Scholar]
- 18.Geneva. The Urgency of Health Promotion Overview. 7th Global Conference on Health promotion;October, 2009, Kenya. Available from: http://www.who.int/healthpromotion/conferences/7gchp/overview/en/index.html .
- 19.Goodstadt MS, Simpson RI, Loranger PO. Health promotion:a conceptual integration. American Journal of Health Promotion. 1986;1(3):58–63. doi: 10.4278/0890-1171-1.3.58. https://doi.org/10.4278/0890-1171-1.3.58. [DOI] [PubMed] [Google Scholar]
- 20.Edelman CL, Kudzma EC, Mandle CL. Health Promotion throughout Life Span. 8th ed. Mosby: Elsevier Inc; 2014. [Google Scholar]
- 21.Klossner N, Hatifield N. Introductory Maternity and Nursing. 9th ed. Ch. 34. Philadelphia: Lippincott Williams and Wilkins Company; 2006. pp. 798–800. [Google Scholar]
- 22.Al-Jadid MS. Disability in Saudi Arabia. Saudi Med J. 2013;34(5):453–460. PMid:23677260. [PubMed] [Google Scholar]
- 23.Loisel P, Lemaire J, Poitras S, Durand MJ, Champagne F, Stock S, et al. Cost-benefit and cost-effectiveness analysis of a disability prevention model for back pain management:six years follow up study. Occup Environ Med. 2002;(59):807–815. doi: 10.1136/oem.59.12.807. https://doi.org/10.1136/oem.59.12.807 PMid:12468746 PMCid:PMC1763600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.World Health Organization. World report on disability. Geneva (CH): World Health Organization; 2011. [Google Scholar]
- 25.Koren P, DeChillo N, Friesen B.J. Measuring Empowerment in Families Whose Children Have Emotional Disabilities:A Brief Questionnaire. Rehabilitation psychology. 1992;37(4):305–320. https://doi.org/10.1037/h0079106. [Google Scholar]
- 26.Abidin RR. A Professional Manual for Parenting Stress Index. 3rd Ed. Odessa, FL: PAR, Psychological Assessment Resources, Inc; 1995. PMid:7702825. [Google Scholar]
- 27.Mash J, Wolfe A. Abnormal Child Psychology. 3rd ed. Chapter:9. USA: Thomson Wadsworth Company; 2005. pp. 262–280. PMCid:PMC3843355. [Google Scholar]
- 28.Ghoneim A, Khalifa M, Thabet A, Salah S. Impact of Mental Retardation on Quality of Life of Children at Shebin Elkom [Master thesis] [Shebin Elkom]:Menofia University. 2008:150. [Google Scholar]
- 29.Moes D, Koegel R, Schreibman L, Loos L. Stress profiles for mothers and fathers of children with autism. Psychological Reports. 1992;71:1272–4. doi: 10.2466/pr0.1992.71.3f.1272. https://doi.org/10.2466/pr0.1992.71.3f.1272 PMid:1480714. [DOI] [PubMed] [Google Scholar]
- 30.Abbeduto L, Seltzer M, Shattuck P, Kruss M, Orsmond G, Murphy M. Psychological well-being and coping in mothers of youths with autism, Down syndrome, or fragile X syndrome. American Journal on Mental Retardation. 2004;109:237–54. doi: 10.1352/0895-8017(2004)109<237:PWACIM>2.0.CO;2. https://doi.org/10.1352/0895-8017(2004)109<237:PWACIM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 31.Yousef Y, Darwish I, Shehata A. Behavioral problems of mental retardation handicapped children encountered by their mothers. Bulletin of High Institute of Public Health. 2004;34(1) [Google Scholar]
- 32.Gibson CH. The process of empowerment in mothers of chronically ill children. Journal of Advanced Nursing. 1995;(21):1201–10. doi: 10.1046/j.1365-2648.1995.21061201.x. https://doi.org/10.1046/j.1365-2648.1995.21061201.x PMid:7665789. [DOI] [PubMed] [Google Scholar]
- 33.Dardas LA, Ahmad MM. Psychometric properties of the Parenting Stress Index with parents of children with autistic disorder. JIDR. 2013;2013 doi: 10.1111/jir.12053. [DOI] [PubMed] [Google Scholar]
- 34.Shatla R, Sayyah H, Azzam H, Elsayed R. Correlates of parental stress and psychopathology in pediatric epilepsy. Ann Indian Acad Neurol. 2012;2526(14) doi: 10.4103/0972-2327.91938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nachshen SJ, Minnes P. Empowerment in parents of school-aged children with and without developmental disabilities. JIDR. 2005;12(49):889–904. doi: 10.1111/j.1365-2788.2005.00721.x. https://doi.org/10.1111/j.1365-2788.2005.00721.x PMid:162∫8. [DOI] [PubMed] [Google Scholar]
- 36.Estes A, Munson J, Dawson G, Koehler E, Zhou XH, Abbott R. Parenting Stress and Psychological Functioning among Mothers of Preschool Children with Developmental Delay:Autism. International journal of research and practice. 2009;13(4):375–87. doi: 10.1177/1362361309105658. https://doi.org/10.1177/1362361309105658 PMid:19535467 PMCid:PMC2965631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Minjarez MB, Mercier EM, Williams SE, Hardan AY. Impact of Pivotal Response Training Group Therapy on Stress and Empowerment in Parents of Children with Autism. Journal of Positive Behavior Intervention. 2013;15:71–78. https://doi.org/10.1177/1098300712449055. [Google Scholar]
- 38.Dempsey I, Dunst C. Help giving styles and parent empowerment in families with a young child with a disability. Journal of Intellectual and Developmental Disability. 2004;29(1):40–51. https://doi.org/10.1080/13668250410001662874. [Google Scholar]
- 39.Gatta M, Balottin L, Mannarini S, Birocchi V, Del Col L, Battistella PA. Parental Stress and psychopathological traits in children and adolescents. A controlled study. Riv Psichiatr. 2016;51(6):251–259. doi: 10.1708/2596.26726. PMid:27996985. [DOI] [PubMed] [Google Scholar]


