Abstract
BACKGROUND:
Asthma is the most prevalent chronic disease in the pediatric age group. The disease affects different aspects of the children’s lives, such as physical, emotional, social and educational aspects. Thus, more focus has been on the quality of life in these patients rather than the duration of their illness in recent years.
AIM:
This study examined the different aspects of quality of life in asthmatic children for the first time in this geographic area.
METHODS:
The study was cross-sectional conducted in 2015-2016. The asthmatic group was 100 patients aged 8 to 12 admitted to the Asthma and Allergy Clinic of Ghaem Hospital (as) in Mashhad with the control group composed of 100 healthy children of the same age and gender. The standard questionnaire pedsQLTM was used for comparing the quality of life of children in the two groups. Statistical analysis was SPSS23 with P-value less than 0.05, which was statistically significant.
RESULTS:
In each group, 58 patients were boys, and 42 were girls. In a comparison of the quality of life of children, the asthma group with a mean total score of Peds QL 20.99 ± 12.54 compared to the healthy children with a mean total score of Peds QL of 8.8 ± 5.41 had a lower quality of life (P < 0.001). Moreover, regarding various aspects of quality of life asthma group had a lower quality of life in physical performance, emotional performance and performance in school (P < 0.001). Nonetheless, there was no significant difference between the two groups considering social function (P = 0.267). Examining the relationship between Peds QL score of patients with asthma with various variables was indicative of the fact that Peds QL scores were significantly correlated with the gender of the patients, showing better quality of life in the girls (P = 0.001).
CONCLUSION:
The results indicated that children with asthma have a significantly lower quality of life compared with healthy children of the same age. Also, in examining the different aspects of quality of life, these children had a lower quality of life in physical performance, emotional performance, and performance at school, and were at the level as that of healthy children only in social performance.
Keywords: Asthma, Children, Physical Function, Emotional Function, Social Function
Introduction
Asthma is a respiratory condition marked by attacks of spasm in the bronchi of the lungs, causing difficulty in breathing. It is usually connected to an allergic reaction or other forms of hypersensitivity [1].
Asthma management for reducing inflammation of the air passage is through minimising pre-inflammatory environmental contacts using daily anti-inflammatory drugs and controlling the condition of the onset of the condition that makes asthma worse [2]. Less inflammation usually leads to better control of asthma, with fewer attacks, and reduction of the need for fast-paced asthma medications, but the attacks keep happening yet [3]. Early intervention with systemic corticosteroids greatly reduces the severity of such attacks [4]. The progress in asthma management, especially in pharmacotherapy, enables everyone, except the child with severe asthma, to live naturally [5].
Even though the reason behind childhood asthma is not known, concurrent research showed a combination of environmental contacts and inherited biological, genetic talents [6]. Pulmonary contacts of its environmental causes are inhaled allergens, viral respiratory infections and chemical contaminants, viral respiratory infections and chemical and biological air pollutants like tobacco smoke in the environment [7]. In a prone host, immune responses to these common contacts can be a stimulant for pathogenic, long-term inflammation and undesired repair of damaged airways. In the early life of the growing lung, these pathological trends cause adverse effects on the growth and differentiation of airways, resulting in altered adult paths [5].
Asthma is a common chronic disease with significant pathogenesis. In 2011, more than 10 million children (14% of American children) had been diagnosed with asthma throughout their lives, 70% of the group had asthma in 2015. Being a male and life in poverty are the risk factors for childhood asthma: 15% of boys had asthma compared to 13% of girls, and 18% of all children living in low-income families compared to 12% of children who were not poor [5].
Childhood asthma is among the commonest causes of emergency admission, hospitalisation and absenteeism from school [8]. The high prevalence of hospitalisation and death from asthma has to do with poverty, ethnic minority and urban living [9]. In the past two decades, admission to emergency rooms, hospitalisation, and death from asthma were 2 to 7 times higher in African American children compared with white children. For ethnic minority asthmatic patients living in low-income urban communities, it is believed that a combination of biological, environmental, economic and psychosocial risk factors increases the likelihood of severe asthma attacks [10].
Several studies in many countries have shown a prevalence of around 50% for childhood asthma. Overall, the prevalence of childhood asthma varies greatly from one area to another. A major international study on the prevalence of Childhood Asthma, 233 centres from 97 countries (International Study on Asthma and Allergies in Childhood, Phase 3) revealed a wide range of current outbreaks at 6-7-year-old (2.4 to 27.6%) and 13-14-year-old children (from 0.8 to 32.6%) [11].
Almost 80% of all asthmatic patients report the disease onset before age 6. However, from among all young children with recurrent wheeze, only a few have stable asthma at the end of their childhood. Early childhood asthma risk factors are defined for stable asthma. Asthma prognosis includes major (parent asthma, eczema, inhaler allergy) and minor risk factors (allergic rhinitis, cold wheeze, more than 4% eosinophil, food allergen allergy). Allergies in young children with a frequent cough or wheeze are the strongest risk factor for childhood asthma. The prevalence of asthma is well-connected with the incidence of allergic rhinoconjunctivitis and atopic eczema [5] [12].
Various studies have shown that quality of life varies in chronic diseases, and as asthma is considered as one of the common chronic diseases, it is important to study the quality of life of these patients. Additionally, the prevalence, symptoms, complications and effects of asthma on growth and development and other aspects of the life of school-age children point to the importance of research in this age group [13]. Thus, by determining the quality of life of these patients, one can ease decision making in treatment and propose new solutions to the treatment team.
Considering this, we can determine the different aspects of quality of life in asthmatic children for the first time in this geographic area and designed interventional plans to improve the quality of life of these children according to the results.
Methods
This cross-sectional study was conducted in 2015-2016 to evaluate the quality of life of asthma patients aged 8-12. One part of the population was the patients aged 8-12 admitted to childhood asthma and Allergy Clinics of Ghaem Hospital (as) Mashhad diagnosed with asthma by their children’s allergy specialist. The purpose and content of the questionnaires were described to the parents of the child by the GP present at the clinic, and they were given a questionnaire to complete in case of agreement. The questionnaire was given to the control group as well, selected from the two parts of the city and various schools, completed by children and their parents. Finally, the data was collected with statistical analysis was performed on them.
The study used a pedsQLTM standard questionnaire to assess the quality of life of children with asthma. The questionnaire examines the quality of life of children in four aspects including physical, emotional, social and educational performance, whose validity and reliability are confirmed in various studies.
In addition to the standard questionnaire, a questionnaire prepared by the researchers containing information such as age, gender, parental education, family income, etc. was also provided to parents and completed.
Considering the professors’ opinions and the paper by Jafari et al., [14], with an alpha of 0.05 and a beta of 0.2, the sample size in each group was considered 100. Thus, 100 children were selected with asthma and 100 healthy children as the sample size.
Data analysis was done after data collection and initial processing in two parts. First, all observations were performed using descriptive statistics method including frequency tables, frequency distribution and columnar graphs, and statistical indices. Central tendency and dispersion were described.
Examining the goals and hypotheses of the plan, the Kolmogorov-Smirnov test was used to test the normality of the data. For comparison of quantitative variables between groups, a t-test was used in the case of normal distribution of data, and Mann-Whitney-U test was used in the case of a normal distribution. The relationship between qualitative variables was also evaluated using chi-square and Fisher’s exact test. Statistical analysis was performed using SPSS22, with a P value less than 0.05 was considered statistically significant.
In this study, no intervention was performed for patients, but prior to entering the study, the goals and method of the study, as well as the contents of the questionnaires were completely explained to patients and their parents, and then informed consent form was given to the participants, so that in case of consent to be completed. Information about each patient was recorded using the code assigned to the patient, and access to information was only available to project implementers to provide the complete safety and patient information protection.
Results
This study examined 100 children aged 8-12 years with asthma and 100 healthy children, compared in this age range. Fifty-eight patients were boys, and 42 were girls. The mean age of the patients was 9.37 ± 1.34 in the asthmatic group and 9.29 ± 1.24 years in the control group. Mann-Whitney test showed no significant differences between the two groups (P = 0.781). Moreover, children in asthmatic and control groups were divided and compared according to different living conditions like parenting life (P = 0.304), living with parents (P = 0.234), father’s education (P = 0.957), maternal education (P = 0.87), maternal occupation (P = 0.508), family income level (P = 0.953), parental smoking (P = 0.852) and the mean number of family members (P = 0.307). None of these cases showed a significant difference between the two groups. Chi-square test was used to compare the two groups.
Comparison of children’s quality of life using Peds QL questionnaire in two groups showed that the asthmatic group with a mean total score of Peds QL was 20.99 ± 15.54 compared with healthy children with a mean total score of Peds QL of 8.8 ± 5.41% had a lower quality of life (P < 0.001).
Moreover, compared with different aspects of life quality in these two groups, asthmatic patients showed a lower level of quality of life in physical performance, emotional performance and performance in school (P < 0.001). However, in the case of social performance, the difference in score from the questionnaires was insignificant groups (P = 0.267) (Table 1).
Table 1.
Comparison of the life quality of the subjects in the control and asthma groups
| Characteristics | Control group N = 100 | Asthma group N = 100 | p-value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Physical performance | 2.12 | 2.11 | 7.63 | 4.82 | <0.001 |
| Emotional performance | 2.43 | 2.39 | 5.62 | 4.09 | <0.001 |
| Social Performance | 2.13 | 1.84 | 3.57 | 4.08 | 0.267 |
| Performance at school | 2.12 | 2.5 | 4.17 | 3.75 | <0.001 |
| Total score of Peds QL | 8.8 | 5.41 | 20.99 | 12.54 | <0.001 |
*Mann-Whitney test was used to compare the two groups.
Comparing the quality of life between the two genders showed the group observed had no significant differences between boys and girls genders in the control group (P > 0.05) neither in the overall Peds QL score nor any of the aspects of quality of life. However, in the group of children with asthma, the physical function (P < 0.001) and social function (P = 0.015) had a higher quality of life than boys. Moreover, the mean total score of Peds QL in boys with asthma was 24.57 ± 13.32 and in girls was 16.23 ± 9.68, which shows the higher quality of life in asthmatic girls (P < 0.001) (Table 2).
Table 2.
Comparison of quality of life between boys and girls in two groups: control and asthma
| Characteristics | Control group N = 100 | P value | Asthma group N = 100 | P value | ||
|---|---|---|---|---|---|---|
| Boy | Girl | Boy | Girl | |||
| Physical performance | 2.05±1.75 | 2.21±2.55 | 0.952 | 9.19±4.96 | 5.55±3.76 | <0.001 |
| Emotional performance | 2.36±2.07 | 2.52±2.8 | 0.907 | 6.21±4.24 | 4.83±3.79 | 0.104 |
| Social Performance | 1.91±1.51 | 2.42±2.21 | 0.421 | 4.45±4.5 | 2.39±3.12 | 0.015 |
| Performance at school | 1.56±1.41 | 2.88±3.36 | 0.16 | 4.71±4.11 | 3.44±3.11 | 0.174 |
| Total score of Peds QL | 7.89±3.34 | 10.04±7.25 | 0.673 | 24.57±13.32 | 16.23±9.68 | 0.001 |
*Mann-Whitney test was used to compare the two groups.
As shown in Table 3, comparing different aspects of quality of life in patients based on the severity of the disease using Kruskal-Wallis statistical test showed that only physical function (P = 0.01) was affected by the severity of the disease. Patients with a higher grade of step had a higher average score in this aspect of quality of life and a lower quality of life later on. However, there were no significant differences between the different stages of the disease (P > 0.05) (Table 3 and Figure 1).
Table 3.
Comparison of the life quality of patients with asthma according to the severity of the disease
| Step I N = 28 | Step II N = 35 | Step III N = 33 | Step IV N = 4 | P-value | |
|---|---|---|---|---|---|
| Physical performance | 6.17±5.23 | 7.3±5.55 | 8.88±3.56 | 9.5±1.73 | 0.01 |
| Emotional performance | 5.17±3.84 | 5.72±4.59 | 6.08±3.94 | 3.75±2.87 | 0.5 |
| Social Performance | 5.1±4.87 | 2.93±4.28 | 2.77±2.93 | 5±2.44 | 0.065 |
| Performance at school | 4.17±4.58 | 3.75±3.4 | 4.37±3.39 | 5.75±3.94 | 0.616 |
| Total score of Peds QL | 20.64±14.79 | 19.72±14.12 | 22.11±9.5 | 24±5.09 | 0.263 |
*Mann-Whitney test was used to compare the two groups.
Figure 1.
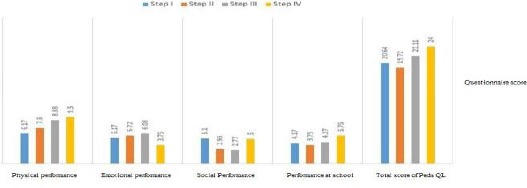
Comparison of the life quality of patients with asthma according to the severity of the disease
The relationship between Peds QL scores of patients with asthma with different variables related to the characteristics of the patients as well as the severity of their disease was examined using statistical regression test.
In this evaluation, it was found that Peds QL scores were significantly correlated with the gender of the patients (B = -0.928; standard error 2.58 and P = 0.001). Girls with asthma have a better quality of life compared to boys with asthma (Table 4).
Table 4.
The relationship between Peds QL score and different characteristics of patients with asthma in the regression test
| Independent variable | B | Standard error | P-value* |
|---|---|---|---|
| Age | -0.246 | 1.16 | 0.833 |
| Gender | -9.28 | 2.58 | 0.001 |
| Number of children | 2.27 | 1.32 | 0.091 |
| The parents being alive | -1.78 | 9.71 | 0.855 |
| Life with parents | 2.64 | 8.43 | 0.755 |
| Father’s education | -3.09 | 2.71 | 0.257 |
| Mother’s education | 5.85 | 2.55 | 0.025 |
| Mother’s employment | -7.41 | 3.78 | 0.053 |
| Income | -0.51 | 2.68 | 0.85 |
| The onset of the disease | 0.552 | 1.56 | 0.726 |
| History of asthma | -0.29 | 1.63 | 0.859 |
| Parental smoking | 1.69 | 3.75 | 0.653 |
| Infant eczema | 4.33 | 3.98 | 0.281 |
| Allergic rhinitis | -4.67 | 2.91 | 0.112 |
| Hospitalization | -5.42 | 3.9 | 0.168 |
| Disease step | 1.27 | 1.51 | 0.402 |
Discussion
Asthma is an allergic disease affecting air passage (bronchus). When an allergic reaction occurs, the bronchial are constricted, narrowed, and blocked by the mucus, making it difficult to breathe. An asthma attack can be very frightening for a child as the feeling of choking makes fears more difficult to breathe [15]. Life quality in patients with asthma is a process affected by the interaction between different physiological and psychological variables. Psychological variables directly affect the life quality of patients, whereas physiological variables indirectly affect the life quality of these patients due to psychological variables [16].
In this study, compared with children’s quality of life, the asthma group with a mean total score of Peds QL 20.99 ± 12.54 compared to healthy children with a mean total score of Peds QL of 8.8 ± 5.41 had a lower quality of life. Moreover, comparing the different aspects of quality of life shows that in these two groups, asthmatic patients showed a lower level of quality of life in physical performance, emotional performance, and performance in school. However, in the case of social performance, the difference in scores obtained from the questionnaire was insignificant between the two groups. Comparing different aspects of patients’ quality of life-based on the severity of the disease, only the physical function of the patients significantly decreased with increasing severity of the disease. The relationship between Peds QL score of patients with asthma with different variables using regression analysis showed that Peds QL scores had a significant relationship only with the patients’ gender so that girls with asthma had a better quality of life than boys
The study found that children with asthma had a lower quality of life compared to healthy children of the same age. Previous studies have shown that due to the chronicity of asthma, this disease can have a profound effect on the lifestyle and function of the affected patients, and negatively affects group activities, social functioning, mental performance, and academic achievement [17].
In previous studies, the drop of quality of life of patients with asthma of different ages has been reported, including Miadich et al., 2015 [18] who examined the quality of life associated with asthma using a questionnaire and eventually reported asthma as a chronic disease affecting the quality of life of children with asthma greatly influences asthma.
Kiotseridis et al., 2018 [19] reviewed the quality of life of 399 patients (236 adults and 163 children) with asthma using HRQL questionnaire and reported that children with asthma have the significantly lower quality of life than the other communities of children.
Annett et al., 2001 examined 339 children aged 4-8 with asthma in a study. In this study, the life quality of children with asthma and their relationship with the symptoms of patients has evaluated: 63% of these children had moderate asthma, and 37% had mild asthma. The study stressed the negative effects of asthma on children’s quality of life [20].
Reichenberg et al., 2000 [21] examined 61 children aged 7-9 with asthma in Sweden, of whom 36 were boys and 25 were girls, 11 had mild asthma, 40 moderate asthma and 10 severe asthma. Asthma showed a significant negative effect on the quality of life of these patients using the PAQLQ questionnaire, which wears more pronounced in young children. The study reported that gender, eczema and rhinoconjunctivitis had no significant effects on the life quality of these patients. However, our study showed that gender affects the quality of life of children, this difference can be due to the type of attitude in both genders, girls and boys are different from the limitations of the disease and how to deal with the disease as well as the attitudes of others in this regard. Another point is the difference in the type of independence and access to academic goals. Hence, the physical and mental differences between the two genders change their view of the disease, its acceptance, and its treatment.
Hallstrand et al., 2003 [22] studied the life quality of 160 adolescents with mild asthma using Peds QL questionnaire. They reported that these patients have a lower quality of life than healthy children regarding their life quality related to health. Also, these patients had lower levels of physical, emotional and school performance than the healthy children of the same age did. These results are totally in line with these results because in our study, in addition to the overall quality of life of these patients, in examining different aspects of quality of life similar to this study, the quality of life was lower in physical, emotional, and school performance. However, there were no significant differences in social function in healthy children.
Everhart et al., 2008 [23] examined 14 review studies for the relationship between the quality of life of children with asthma and their severity, reporting that 9 out of 14 studies showed that the severity of asthma had a significant effect on the quality of life of patients. They also stated that the type of questionnaire used to assess life quality affected the outcomes of these studies. The study showed that factors like the economic level of the family and the number of children in the family affected the life quality of children with asthma. However, in the study by Salman Yazdi et al., [24], there was a significant relationship between the number of children in the family and the quality of life of two-year-old children. Moreover, it was reported that an increase in the number of children in the family reduced the quality of life of children. This is probably because although the number of family members increases the level of independence in children and adolescents, due to the possibility of reducing family health care and increasing the risk factors for asthma (e.g. allergens, infections, inappropriate nutrition, stress and competition among children) quality of life in children decreases.
However, childhood asthma leads to different problems and suffering for the child and his family, so determining the quality of life of these patients can help identify the specific needs of these patients and their families. After this, the adoption of suitable therapeutic and educational methods for these patients and their families, because of difficulty in many aspects of life quality, could be related to the reduction of illness and its harm, the improvement of the physical and psychological health of children. Finally, they helped improve their quality of life.
In conclusion, the results indicated that Peds QL questionnaire score for children aged 8-12 with asthma was significantly higher than that of healthy children matched by age and gender.
Hence, children with asthma had the significantly lower quality of life than their peers. Also, in an exclusive study of different aspects of life quality, these children had lower levels of quality of life in physical performance, emotional performance, and performance in school and had the same level of quality to that of healthy children only in social performance. Another important issue was that of children with asthma, girls have a higher quality of life than boys that may be due to the cultural issues of society.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Hirano T, Matsunaga K. Late-onset asthma: current perspectives. J Asthma Allergy. 2018;11:19–27. doi: 10.2147/JAA.S125948. https://doi.org/10.2147/JAA.S125948 PMid:29445292 PMCid: PMC5810515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rowe BH, Sevcik W, Villa-Roel C. Management of severe acute asthma in the emergency department. Curr Opin Crit Care. 2011;17(4):335–41. doi: 10.1097/MCC.0b013e328348bf09. https://doi.org/10.1097/MCC.0b013e328348bf09 PMid:21716106. [DOI] [PubMed] [Google Scholar]
- 3.Zhu D, Zhang C, Shen H, Ying S. Breaking through Restricting Bottleneck for Better Asthma Control. J Transl Int Med. 2017;5(4):192–193. doi: 10.1515/jtim-2017-0032. https://doi.org/10.1515/jtim-2017-0032 PMid:29340274 PMCid: PMC5767707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.An TJ, Rhee CK, Kim JH, Lee YR, Chon JY, Park CK, Yoon HK. Effects of Macrolide and Corticosteroid in Neutrophilic Asthma Mouse Model. Tuberc Respir Dis (Seoul) 2018;81(1):80–87. doi: 10.4046/trd.2017.0108. https://doi.org/10.4046/trd.2017.0108 PMid:29332324 PMCid: PMC5771750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gahagan S, Kliegman RM, Stanton BF, Geme JWS, Schor NF. Nelson textbook of pediatrics. 20th ed. Philadelphia: Saunders; 2016. pp. 1650–77. [Google Scholar]
- 6.Duong-Thi-Ly H, Nguyen-Thi-Thu H, Nguyen-Hoang L, Nguyen-Thi-Bich H, Craig TJ, Duong-Quy S. Effects of genetic factors to inhaled corticosteroid response in children with asthma: a literature review. J Int Med Res. 2017;45(6):1818–1830. doi: 10.1177/0300060516683877. https://doi.org/10.1177/0300060516683877 PMid:29251255 PMCid: PMC5805193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pawankar R, Canonica GW, Holgate ST, Lockey RF. Allergic diseases and asthma: a major global health concern. Current opinion in allergy and clinical immunology. 2012;12(1):39–41. doi: 10.1097/ACI.0b013e32834ec13b. https://doi.org/10.1097/ACI.0b013e32834ec13b PMid:22157151. [DOI] [PubMed] [Google Scholar]
- 8.Rust G, Zhang S, Holloway K, Tyler-Hill Y. Timing of emergency department visits for childhood asthma after initial inhaled corticosteroid use. Popul Health Manag. 2015;18(1):54–60. doi: 10.1089/pop.2013.0126. https://doi.org/10.1089/pop.2013.0126 PMid:25046059 PMCid: PMC4346601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mitchell DK, Adams SK, Murdock KK. Associations among risk factors, individual resources, and indices of school-related asthma morbidity in urban, school-aged children: a pilot study. J Sch Health. 2005;75(10):375–83. doi: 10.1111/j.1746-1561.2005.00052.x. https://doi.org/10.1111/j.1746-1561.2005.tb06640.x PMid:16313508. [DOI] [PubMed] [Google Scholar]
- 10.Forno E, Celedon JC. Asthma and ethnic minorities: socioeconomic status and beyond. Curr Opin Allergy Clin Immunol. 2009;9(2):154–60. doi: 10.1097/aci.0b013e3283292207. https://doi.org/10.1097/ACI.0b013e3283292207 PMid:19326508 PMCid: PMC3920741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Asher MI, Weiland SK. The International Study of Asthma and Allergies in Childhood (ISAAC) ISAAC Steering Committee. Clinical and experimental allergy: Journal of the British Society for Allergy and Clinical Immunology. 1998;28:52–66. doi: 10.1046/j.1365-2222.1998.028s5052.x. https://doi.org/10.1046/j.1365-2222.1998.028s5052.x PMid:9988448. [DOI] [PubMed] [Google Scholar]
- 12.Szentpetery SS, Gruzieva O, Forno E, Han YY, Bergström A, Kull I, et al. Combined effects of multiple risk factors on asthma in school-aged children. Respir Med. 2017;133:16–21. doi: 10.1016/j.rmed.2017.11.002. https://doi.org/10.1016/j.rmed.2017.11.002 PMid:29173444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Howell CR, Thompson LA, Gross HE, Reeve BB, Huang SW, DeWalt DA, et al. Association of consistently suboptimal quality of life with consistently poor asthma control in children with asthma. Ann Allergy Asthma Immunol. 2017;119(6):562–564. doi: 10.1016/j.anai.2017.09.053. https://doi.org/10.1016/j.anai.2017.09.053 PMid:29107463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jafari P, Forouzandeh E, Bagheri Z, Karamizadeh Z, Shalileh K. Health related quality of life of Iranian children with type 1 diabetes: reliability and validity of the Persian version of the PedsQL8482Generic Core Scales and Diabetes Module. Health and quality of life outcomes. 2011;9(1):104. doi: 10.1186/1477-7525-9-104. https://doi.org/10.1186/1477-7525-9-104 PMid:22112006 PMCid: PMC3280935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mahemuti G, Zhang H, Li J, Tieliwaerdi N, Ren L. Efficacy and side effects of intravenous theophylline in acute asthma: a systematic review and meta-analysis. Drug Des Devel Ther. 2018;12:99–120. doi: 10.2147/DDDT.S156509. https://doi.org/10.2147/DDDT.S156509 PMid:29391776 PMCid: PMC5768195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baiardini I, Sicuro F, Balbi F, Canonica GW, Braido F. Psychological aspects in asthma: do psychological factors affect asthma management? Asthma research and practice. 2015;1(1):7. doi: 10.1186/s40733-015-0007-1. https://doi.org/10.1186/s40733-015-0007-1 PMid:27965761 PMCid: PMC5142316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Valizadeh L, Bilan N, Zarei S, Sharifi A. Effect of education and controlling Asthma triggers on quality of life among adolescents with asthma: a randomized clinical trial. Journal of Mazandaran University of Medical Sciences. 2013;23(98):49–57. [Google Scholar]
- 18.Miadich SA, Everhart RS, Borschuk AP, Winter MA, Fiese BH. Quality of Life in Children with Asthma: A Developmental Perspective. J Pediatr Psychol. 2015;40(7):672–9. doi: 10.1093/jpepsy/jsv002. https://doi.org/10.1093/jpepsy/jsv002 PMid:25680363 PMCid: PMC4505073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kiotseridis H, Arvidsson P, Backer V, Braendholt V, Tunsäter A. Adherence and quality of life in adults and children during 3-years of SLIT treatment with Grazax-a real life study. NPJ Prim Care Respir Med. 2018;28(1):4. doi: 10.1038/s41533-018-0072-z. https://doi.org/10.1038/s41533-018-0072-z PMid:29434271 PMCid: PMC5809499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Annett RD, Bender BG, Lapidus J, DuHamel TR, Lincoln A. Predicting children's quality of life in an asthma clinical trial: what do children's reports tell us? The Journal of pediatrics. 2001;139(6):854–61. doi: 10.1067/mpd.2001.119444. https://doi.org/10.1067/mpd.2001.119444 PMid:11743513. [DOI] [PubMed] [Google Scholar]
- 21.Reichenberg K, Broberg AG. Quality of life in childhood asthma: use of the Paediatric Asthma Quality of Life Questionnaire in a Swedish sample of children 7 to 9 years old. Acta paediatrica. 2000;89(8):989–95. doi: 10.1080/080352500750043495. https://doi.org/10.1111/j.1651-2227.2000.tb00423.x PMid:10976845. [DOI] [PubMed] [Google Scholar]
- 22.Hallstrand TS, Curtis JR, Aitken ML, Sullivan SD. Quality of life in adolescents with mild asthma. Pediatric pulmonology. 2003;36(6):536–43. doi: 10.1002/ppul.10395. https://doi.org/10.1002/ppul.10395 PMid:14618647PMCid: PMC2002508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Everhart RS, Fiese BH. Asthma severity and child quality of life in pediatric asthma: a systematic review. Patient education and counseling. 2009;75(2):162–8. doi: 10.1016/j.pec.2008.10.001. https://doi.org/10.1016/j.pec.2008.10.001 PMid:19036553. [DOI] [PubMed] [Google Scholar]
- 24.Salman-Yazdi N, Ghasemi I, Salahshourian A, Haghani H. Comparative study on the quality of life amongst asthmatic boys and girls aged between 7-17 in Zanjan. Iranian Journal of Cardiovascular Nursing. 2012;1(1):24–9. [Google Scholar]


