Abstract
Background
High rates of tobacco smoking and smoking cessation failure in schizophrenia may be related to pre-frontal cortical dysfunction. Novel treatment options for tobacco use disorder are needed given the limited efficacy of current pharmacotherapies. Preliminary evidence suggests high-frequency repetitive transcranial magnetic stimulation (rTMS) to bilateral dorsolateral prefrontal cortex (DLPFC) may suppress tobacco craving in smokers with schizophrenia. The goal of this study was to determine effects of rTMS for tobacco craving and cognition using a short-term (3-day) human laboratory paradigm.
Methods
Bilateral active (20 Hz) versus sham rTMS stimulation was administered in a counterbalanced, double-blind, cross-over design to thirteen smokers with schizophrenia and n = 14 non-psychiatric smoking controls. Participants were studied at baseline (smoking satiated), after 16 h of smoking abstinence, and after smoking reinstatement. Primary outcome measures included tobacco craving, withdrawal and cognition.
Results
Overnight abstinence produced a significant increase in tobacco craving and withdrawal, and impaired verbal memory and visuospatial working memory in both diagnostic groups; these effects were reversed with smoking reinstatement. However, active rTMS did not modify this pattern of results. Moreover, active versus sham rTMS had no significant effects on cognitive outcomes, and was not associated with significant adverse events.
Conclusions
Our preliminary findings suggest that short-term rTMS administration may not be sufficient enough to modify cognition, craving, and withdrawal outcomes in smokers with schizophrenia (NCT00736710). Longer-term, controlled treatment studies examining effects of rTMS on smoking behaviors and cognition in schizophrenia are warranted.
Keywords: Schizophrenia, Tobacco, rTMS, Cognition, Abstinence, Sham, Craving
Dear Editor
There are higher rates of tobacco smoking and smoking cessation failure amongst smokers with schizophrenia compared to the general population, which may be related to prefrontal cortical dysfunctions (Sacco et al., 2005). Standard tobacco smoking cessation treatments have only been somewhat efficacious, stressing the importance for more effective treatments targeting underlying neurological deficiencies amongst this comorbid population. Repetitive transcranial magnetic stimulation (rTMS) is a non-invasive brain stimulation technique that when targeted to the dorsolateral prefrontal cortex (DLPFC), has shown tremendous promise and tolerability in preliminary research (Sheffer et al. 2018; Wing, 2013). This includes improvements in working memory performance in patients with schizophrenia (Barr et al., 2009), decreased delay discounting in non-psychiatric smokers (Sheffer et al. 2018), and reduced tobacco craving induced by short-term smoking abstinence in schizophrenia smokers (Wing et al., 2012b) and in non-psychiatric smokers (Sheffer et al. 2018). Thus the present study, sought to determine effects of high-frequency rTMS (20 Hz) targeted to the DLPFC, on tobacco craving, withdrawal, and cognition in smokers with schizophrenia and non-psychiatric controls.
A counterbalanced, double-blind, cross-over laboratory study design was employed with a one-month washout period between treatment weeks. rTMS treatment was administered twice daily on days 1–3 of each treatment week, with the resting motor threshold determined using previously published methods (Daskalakis et al. 2006). rTMS treatment targeted the DLPFC at 20 Hz with 25 stimulation trains of 30 pulses per train on a 30-second interval between trains, consistent with previous studies (Wing et al., 2012a) for a total of six treatments. Primary outcome measures included tobacco craving (indexed by the Tiffany Questionnaire for Smoking Urges (TQSU) (Tiffany and Drobes 1991)), withdrawal (Minnesota Nicotine Withdrawal Scale (MNWS) (Hughes and Hatsukami, 1986) and cognition (i.e., Spatial Delayed Response Task (SDR) indexed visuospatial working memory, Hopkins Verbal Learning Task (HVLT) indexed verbal learning and memory (Kozak et al. 2017)), which were assessed under conditions of smoking satiation (Day 2), acute 16-h of smoking abstinence (Day 3 AM), and upon smoking reinstatement (Day 3 PM).
Twenty-seven participants (13 schizophrenia, SZ; 14 non-psychiatric controls, CON) completed the protocol. Both diagnostic groups were demographically and clinically comparable (ps > 0.05; provided in Table 1). Two-way repeated measures ANOVAs across time (Day 2 PM, Day 3 AM, Day 3 PM) and treatment (sham versus active) between diagnoses (SZ versus CON) indicated a significant effect of time on TQSU Factor 1 (SZ = 13; CON = 13; F(2,48) = 23.467, p < 0.001), TQSU Factor 2 (F(1.5,48) = 25.882, p < 0.001) MNWS Craving (SZ = 13; CON = 12; F(1.6,36.8) = 38.9, p < 0.001) and MNWS Total Score (F(1.5,35.1) = 53.5, p < 0.001), and a time by diagnosis interaction on TQSU Factor 1 (F(2,48) = 3.571, p = 0.036), and TQSU Factor 2 (F(2,48) = 3.376, p = 0.042). Moreover, a transient increase appeared in both diagnostic groups in levels of craving and withdrawal after acute abstinence with subsequent reversal of this increase returning to baseline upon reinstatement; however, this affect was not statistically significant and statistical analysis showed no effect of rTMS treatment condition in either group.
ANOVAs indicated a significant effect of time on SDR 30-second delay (SZ = 11; CON = 10) (F(2,38) = 4.4, p = 0.019) (Fig. 1), HVLT-R % Retention (SZ = 12; CON = 12) (F(2,44) = 9.0, p = 0.001) and HVLT-R Discrimination Index (F(2,44) = 6.3, p = 0.004) and a time by diagnosis interaction (F(2,44) = 4.607, p = 0.015) and time by rTMS treatment interaction (F(2,44) = 4.5, p = 0.016) for the latter; however, no three-way interactions were found. There were no significant time, treatment, or diagnostic differences found in any other cognitive outcomes (data not shown).
Fig. 1.
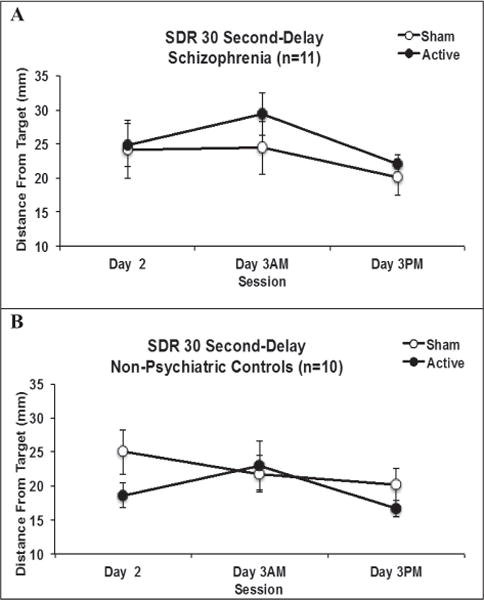
Effects of rTMS on Cognitive Performance. Effects of rTMS treatment (active vs. sham) and time (Day 2 PM, Day 3 AM, Day 3 PM) on Spatial Delayed Response (SDR) 30-second-delay between schizophrenia (Fig. 1A) and control (Fig. 1B) smokers.
Overall, overnight abstinence produced a significant increase in tobacco craving and withdrawal, and impaired verbal memory and visuo-spatial working memory in both diagnostic groups; these effects were reversed with smoking reinstatement consistent with our previous findings (Sacco et al., 2005; Wing et al., 2012a). However, active rTMS did not modify this pattern of results, similar to a recently published report (Kamp et al., 2017). Moreover, active versus sham rTMS was not associated with significant adverse events (data not shown). Study strengths include positive controls of changes in withdrawal and craving with smoking abstinence and reinstatement, the inclusion of both smokers with and without schizophrenia, demonstration of cognitive impairments in visuospatial working memory and verbal learning with smoking abstinence and reversal with smoking reinstatement, and the use of a within-subjects design to minimize between-subject heterogeneity. Study limitations include our relatively small sample sizes of smokers with schizophrenia and non-psychiatric controls.
Our preliminary findings suggest that acute (3 day) administration of rTMS is insufficient to ameliorate such abstinence-induced effects on craving, withdrawal and cognition in smokers with schizophrenia and controls. Longer-term, controlled treatment studies examining effects of rTMS on smoking behaviors and cognition in schizophrenia are warranted.
Supplementary Material
Acknowledgments
This work was supported in part by Canadian Institutes of Health Research Operating Grant MOP#115145, NIH/NIDA grant 1R21-DA-043949, and the Chair in Addiction Psychiatry at the University of Toronto to Dr. George. The authors gratefully acknowledge the assistance of Emily Simpkin, RN, BScN, who provided skilled nursing and technical support towards the successful completion of the study.
Declaration of funding source
• Canadian Institutes of Health Research Operating Grant (MOP#115145) to Dr. George.
• NIDA grant R21-DA-043949 to Dr. George.
Dr. George reports that he has funding support from the Canadian Institutes of Health Research (CIHR) and National Institutes of Health (NIH).
Footnotes
Supported in part by CIHR grant MOP#115145 and NIDA grant R21-DA-043949 to Dr. George.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.schres.2018.02.015.
Contributors
1. Karolina Kozak, M.Sc.1,2,3
2. Maryam Sharif-Razi, M.Sc.1
3. Marya Morozova, M.S.W.1
4. Erin V. Gaudette1
5. Mera S. Barr, Ph.D.2,3
6. Zafiris J. Daskalakis Ph.D., M.D., FRCPC2,3
7. Daniel M. Blumberger, M.D., FRCPC2,3
8. Tony P. George, M.D., FRCPC1,2,3
1 Addictions Division, Centre for Addiction and Mental Health (CAMH).
2 Division of Brain and Therapeutics, Department of Psychiatry, University of Toronto.
3 Institute of Medical Sciences, University of Toronto.
Declaration of conflicts
Ms. Kozak, Ms. Sharif-Razi, Ms. Morozova, Ms. Guadette, Dr. Barr, Dr. Daskalakis, and Dr. Blumberger report no conflicts of interest. The authors alone are responsible for the content and writing of this paper.
References
- Barr MS, Farzan F, Rusjan PM, et al. Potentiation of gamma oscillatory activity through repetitive transcranial magnetic stimulation of the dorsolateral prefrontal cortex. Neuropsychopharmacology. 2009;34:2359–2367. doi: 10.1038/npp.2009.79. [DOI] [PubMed] [Google Scholar]
- Daskalakis ZJ, Moller B, Christensen BK, Fitzgerald PB, Gunraj C, Chen R. The effects of repetitive transcranial magnetic stimulation on cortical inhibition in healthy human subjects. Exp Brain Res. 2006;174(3):403–412. doi: 10.1007/s00221-006-0472-0. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Hatsukami D. Signs and symptoms of tobacco withdrawal. Arch Gen Psychiatry. 1986;43(3):289–294. doi: 10.1001/archpsyc.1986.01800030107013. [DOI] [PubMed] [Google Scholar]
- Kamp D, Engelke C, Wobrock T, Kunze B, Wolwer W, Winterer G, Schmidt-Kraepelin C, Gaebel W, Langguth B, Landgrebe M, Eichhammer P, Frank E, Hajak G, Ohmann C, Verde PE, Rietschel M, Raees A, Honer WG, Malchow B, Schneider-Axmann T, Falkai P, Hasan A, Cordes J. Letter to the Editor: influence of rTMS on smoking in patients with schizophrenia. Schizophr Res. 2017;192:481–484. doi: 10.1016/j.schres.2017.05.036. [DOI] [PubMed] [Google Scholar]
- Kozak K, Dermody SS, Rabin RA, Zack M, Barr MS, Tyndale RF, George TP. Effects of varenicline on cognitive function in non-smokers with schizophrenia. Schizophr Res. 2017;(17):30143–3. doi: 10.1016/j.schres.2017.03.023. pii: S0920–9964. [EPub, ahead of print] [DOI] [PubMed] [Google Scholar]
- Sacco K, Termine A, Seyal A, Dudas MM, Vessicchio JC, Krishnan-Sarin S, Jatlow PI, Wexler BE, George TP. Effects of cigarette smoking on spatial working memory and attentional deficits in schizophrenia: involvement of nicotinic receptor mechanisms. Arch Gen Psychiatry. 2005;62:649–659. doi: 10.1001/archpsyc.62.6.649. [DOI] [PubMed] [Google Scholar]
- Sheffer CE, Bickel WK, Brandon TH, Franck CT, Deen D, Panissidi L, Abdali SA, Pittman JC, Lunden SE, Prashad N, Malhotra R, Mantovani A. Preventing relapse to smoking with transcranial magnetic stimulation: feasibility and potential efficacy. Drug Alcohol Depend. 2018;182:8–18. doi: 10.1016/j.drugalcdep.2017.09.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiffany ST, Drobes DJ. The development and initial validation of a questionnaire on smoking urges. Br J Addict. 1991;86(11):1467–1476. doi: 10.1111/j.1360-0443.1991.tb01732.x. [DOI] [PubMed] [Google Scholar]
- Wing V, Bacher I, Wu BS, Daskalakis ZJ, George TP. High frequency repetitive transcranial magnetic stimulation reduces tobacco craving in schizophrenia. Schizophr Res. 2012a;139:264–266. doi: 10.1016/j.schres.2012.03.006. [DOI] [PubMed] [Google Scholar]
- Wing VC, Moss TG, Rabin RA, George TP. Effects of cigarette smoking status on delay discounting in schizophrenia and healthy controls. Addict Behav. 2012b;37:67–72. doi: 10.1016/j.addbeh.2011.08.012. [DOI] [PubMed] [Google Scholar]
- Wing VC, Barr MS, Wass CE, Lipsman N, Lozano AM, Daskalakis ZJ, George TP. Brain stimulation methods to treat tobacco addiction. Brain Stimulation. 2013;6:221–230. doi: 10.1016/j.brs.2012.06.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


