Abstract
This study assessed the association between community savings group participation and consistent condom use (CCU) among female sex workers (FSW) in Iringa, Tanzania. Using cross-sectional data from a survey of venue-based FSW (n = 496), logistic regression was used to examine the associations between financial indicators including community savings group participation and CCU. Over one-third (35%) of the women participated in a savings group. Multivariable regression results indicated that participating in a savings group was significantly associated with nearly two times greater odds of CCU with new clients in the last 30 days (aOR = 1.77, 95% CI 1.10–2.86). Exploratory mediation analysis indicated that the relationship between savings group participation and CCU was partially mediated by financial security, as measured by monthly income. Findings indicate that community savings groups may play an important role in reducing sexual risk behaviors of FSW and hold promise as part of comprehensive, community-led HIV prevention strategies among FSW.
Keywords: HIV, Female sex workers, Community savings groups, Economic strengthening interventions, Financial security, Tanzania
Background
Female sex workers (FSW) bear a disproportionately high burden of HIV. Globally, it is estimated that they have 13.5 times greater odds of having HIV than other adult women [1]. HIV prevalence among FSW in sub-Saharan African countries is significantly higher than in other geographic regions, with an estimated pooled prevalence of 36.9% [2]. Tanzania has a national HIV prevalence of 5.1% however, the Iringa region in the southwest highlands has a notably higher prevalence of 9.1% [3]. Iringa is characterized by high levels of trade, transport and migration of seasonal workers, dynamics that create and sustain demand for sex work [4]. Sex work in Iringa occurs mostly in venues such as bars, guesthouses and truck stops along the major transport and trucking route that traverses the region. HIV prevalence among FSW in Iringa is estimated to be 32.9% [5].
There is an established literature indicating the importance of financial insecurity as a driver of HIV risk behaviors such as unprotected sex among FSW [6–14]. Studies in diverse settings indicate that financial insecurity places sex workers in a position of limited power to negotiate condom use and to refuse unsafe sex with clients [15–19]. The impact of condom use on FSW earnings has been quantified in multiple and diverse settings indicating marked price differences between sex with and without a condom [20–23]. Higher premiums for unprotected sex are particularly compelling when additional pay can help cover basic needs such as food, housing or health care for one’s family, underscoring the role of financial incentive in decision-making around condom use for economically vulnerable FSW.
Economic strengthening interventions for HIV prevention among FSW include strategies for addressing the material vulnerability that affects FSW condom negotiating capacities with clients. Such approaches acknowledge the role of economic factors in sexual decision-making for FSW and aim to promote financial security, thereby reducing the risk of unprotected sex with clients. The literature on such approaches with FSW is limited [24, 25]. However, there are a number of promising examples of programs that have successfully implemented economic strengthening interventions such as cooperative banking and group lending within the context of a broader community empowerment approach—one in which the community takes collective ownership of strategies to address structural barriers to their health [26].
Durbar (the Sonagachi Project), the widely-recognized community empowerment intervention among FSW in Kol-kata, India, was among the first to document a peer-run cooperative bank and address financial insecurity by increasing savings among brothel-based FSW [27]. This model has been associated with reduced economic vulnerability and increased consistent condom use (CCU) among FSW [28–30]. The Karnataka Health Promotion Trust among FSW in Karnataka, India has shown that FSW participating in savings activities within the program’s cooperative bank structures were more likely to report condom use at last sex with clients [31]. A savings-focused intervention among FSW in Mongolia demonstrated that women receiving the savings component were more likely to report CCU with clients at follow-up than those receiving the HIV prevention component alone [32]. While the literature provides models from a handful of settings, other examples and further evaluation of savings-led approaches aimed at improving the financial security of FSW are needed, particularly in the context of sub-Saharan Africa.
Prior formative work conducted in Iringa identified organically formed community savings groups [locally called michezo (singular: mchezo)] among FSW [4]. Mich-ezo are widespread among non-FSW in Tanzania as well and used for general financial security and social support. Similar to group lending strategies and informal local savings cooperatives seen throughout Tanzania and in other parts of the world, members of michezo in Iringa regularly contribute a set amount and receive the lump sum of the members’ contributions in a rotating payout as well as have access to loans for emergency funds. These groups may have the potential to increase savings, improve financial security and better position FSW who participate in them to refuse unsafe sex and negotiate condom use. This study sought to assess the association between participating in a community savings group and CCU among FSW in Iringa, Tanzania.
Methods
Study Sample and Recruitment
This analysis utilized baseline survey data from Project Shikamana, a phase II community-based combination HIV prevention trial being conducted in two distinct communities within the Iringa region of Tanzania [33]. The study enrolled venue-based FSW who were consented, tested for HIV, and completed an interviewer-administered baseline survey. Eligibility criteria included being 18 years or older, having exchanged sex for money in the last 30 days, and working at a sex work venue in one of the two study communities. The study communities were matched on demographics and HIV prevalence among the general population. The sample (n = 496) recruited from the two communities included both HIV-uninfected (n = 293) and HIV-infected (n = 203) women. FSW were recruited from venues using time-location sampling to approximate a representative sample. The combination HIV prevention intervention includes the following biomedical, behavioral, and structural components: (1) peer education, condom distribution, and HIV counseling and testing in entertainment venues, (2) peer navigation to facilitate linkage to and retention in care and on antiretroviral therapy (ART), (3) sensitivity training for HIV clinical care providers, (4) text messages to promote awareness, solidarity, and adherence to care and ART, and (5) a community-led drop-in center for activities to promote social cohesion and community mobilization [33]. This analysis was conducted on baseline data which was collected prior to initiation of intervention activities.
Measures
Dependent Variables
The primary outcome measure of CCU in the last 30 days was assessed by asking about condom use behaviors with new clients, regular clients and steady, non-paying partners, respectively. Participants were asked if they had always, almost always, sometimes, almost never, or never used a condom during vaginal sex in the last 30 days with each partner type. This variable was then dichotomized into consistent (always) and inconsistent (anything less than always) condom use for each partner type. New clients were defined as clients the respondent had sex with only once or twice in her life, regular clients were defined as those whom she had sex with at least three times in her life and who pay her for sex, and steady, non-paying partners were defined as partners she had sex with at least three times in her life and who do not pay her for sex acts.
Independent Variables
Community savings group participation was the primary independent variable of interest and was assessed by a survey question asking participants if they currently participate in a savings group. Our main hypothesis was that participating in a savings group has a protective effect on HIV risk behaviors. Financial indicators were chosen for inclusion in the analysis as independent variables based on existing literature and conceptual relevance. Monthly total income and monthly sex work income were each dichotomized using the median as the cut-point to create higher and lower income groups to serve as proxies for financial security. Ten quan-tiles were also created for total income to assess changes in effect across finer groupings of income categories. Percentage of income from sex work was created by dividing sex work income by total income and multiplying by 100 and was then dichotomized at the median (above 50% of income from sex work vs. below 50% of income from sex work). Other financial indicators included in the analysis were: having financial dependents, having someone to help cover basic needs at times when income alone was not enough, and participants’ self-perceived financial security dichotomized as poor/fair versus good/very good.
Due to non-normal distribution of the data, dichotomous variables were created, using the median for age (> 25), education (no schooling or some primary school vs. some secondary school or higher) and marital status (currently married vs. not married). Number of children was categorized as no children, 1–2 children, and 3 or more children. Length of time in sex work was calculated by subtracting the age when first engaged in sex work from the respondent’s age at the time of the survey. Participants were asked to report the number of sex work clients they had in the past week and the average pay they received per sexual encounter with a client. Participant’s recruitment community was also included. HIV status was determined through serological testing including parallel rapid HIV-1 antibody tests (Determine and Unigold), followed by repeat parallel testing in the case of discordant results. A categorical variable was created to distinguish between HIV positive women who knew their HIV status versus those who did not (with HIV negative women as the reference group) to examine if knowledge of HIV status affected condom use behaviors.
Data Analysis
Exploratory data analysis was conducted to examine frequencies and percentages for the sample, specifically demographics, financial security indicators and sex work and sexual risk behavior characteristics. Bivariate logistic regression was conducted to determine odds ratios (ORs) and confidence intervals (CIs) for each independent variable against the outcome. Independent variables that had a p value of ≤ 0.10 in bivariate analysis were included in multivariable logistic regression models as well as important confounders such as HIV infection and age. Multivariable analysis was conducted through an iterative backward stepwise process dropping the least significant variable with each iteration. The generalized estimating equation approach [34] was used to adjust for intra-class correlation among venues from which participants were recruited. Akaike information criterion was used to compare the nested models and determine model selection. Multi-collinearity was assessed by examining variance inflation factors of the independent variables, and a Hosmer–Lemeshow goodness of fit test was conducted on the final model. We posited that increased CCU may be associated with savings group participation through improved financial security, and thus, financial security was examined as a potential mediator. Exploratory mediation analysis was conducted in an attempt to better understand whether financial security (e.g., higher individual monthly income) has a role in the mechanism through which community savings group participation affects CCU. We applied a bootstrapping test of the indirect effect when financial security was added to the model. All analyses were conducted using Stata® version 13.1.
Ethics
This study received Human Subjects Research Approval from the Institutional Review Boards of the Johns Hopkins Bloomberg School of Public Health, Muhimbili University of Health and Allied Sciences, and the National Institute for Medical Research of Tanzania.
Results
Demographic, Sex Work, and Financial Characteristics
Table 1 shows demographic, sex work, and financial characteristics of the study sample. The cohort had a median age of 25 years (range 18–55) and the median number of children among the participants was 2 (range 0–10). The majority of participants were unmarried (82%) and had primary level schooling or no schooling (71%). Roughly a quarter of the sample lived either with fellow workers (27%); a sexual partner or spouse (24%); their children, parents, extended family or others (26%); or alone (23%). A total of 203 women (41%) were HIV-infected, only 31% (63/203) of whom were previously aware of their status. Of women who were aware of their status, 68% of them were on ART (43/63); and for those on ART, 70% (30/43) were virally suppressed. The median number of years in sex work among the women was 5, median number of clients per week was 2, and median pay per sexual encounter was 15,000 Tanzanian shillings (Tsh) (~ 7 USD). Among women reporting sex with new clients in the past 30 days, 40% reported CCU, among those reporting sex with regular clients, 34% reported CCU, and among those reporting sex with steady, non-paying partners, 21% reported CCU. Being aware of HIV status was not signifi-cantly associated with CCU.
Table 1.
Demographic, sex work, and financial characteristics of venue-based FSW in Iringa, Tanzania (n = 496)
| Variable | Median [range] or N (%) |
|---|---|
| Demographic characteristics | |
| Age (years) | 25 [18, 55] |
| Education | |
| Some primary school or no education | 352 (71.0) |
| Some secondary school or higher | 144 (29.0) |
| Marital status | |
| Married (legal, traditional or common law) | 89 (17.9) |
| Not married (single, separated, divorced, widowed) | 407 (82.1) |
| Number of children | 2 [0,10] |
| No children | 81 (16.3) |
| 1–2 children | 259 (50.2) |
| 3 or more children | 166 (33.5) |
| Living situation (lives with) | |
| Fellow workers | 135 (27.2) |
| Sexual partner/spouse | 118 (23.7) |
| Children/parents/extended family/other | 131 (26.4) |
| Alone | 112 (22.5) |
| HIV infected | 203 (40.9) |
| Sex work characteristics | |
| Length of time in sex work (years) | 5 [0, 31] |
| Number of clients per week | 2 [0, 40] |
| Pay received per sexual encounter | 15,000 Tsh [2000, 250,000] (~ $7 USD) |
| CCU with new clients in last 30 days (n = 366) | 147 (40.2%) |
| CCU with regular clients in last 30 days (n = 385) | 131 (34.0%) |
| CCU with steady non-paying partners in last 30 days (n = 415) | 88 (21.2%) |
| Financial characteristics | |
| Participates in a community savings group | 175 (35.3) |
| Monthly total income (sex work and other sources) | 120,000 Tsh [0, 3,500,000] (~ $54 USD) |
| Monthly sex work income | 50,000 Tsh [0, 620,000] (~ $23 USD) |
| Percentage of income from sex work income | 50 [0.5, 100] |
| Has financial dependents | 353 (71.2) |
| Has help covering basic needs when income is not enough | 190 (38.3) |
| Has a bank account | 37 (7.5) |
| Self-perceived financial security | |
| Poor/fair | 435 (87.7) |
| Good/very good | 61 (12.3) |
Over one third of the sample (35%) participated in a community savings group. Median monthly income from sex work and other sources was 120,000 Tsh (~ 54 USD), median monthly income from sex work alone was 50,000 Tsh (~ 23 USD) and median percentage of income from sex work was 50%. The majority of participants (71%) had one or more financial dependents while over a third (38%) reported having someone to help cover basic needs in a month when their own income was not enough. Only 8% of participants had a bank account and the majority (88%) perceived their own financial security as fair or poor.
Factors Associated with Savings Group Participation
Table 2 shows odds ratios (ORs) with associated 95% con-fidence intervals (CIs) for characteristics associated with participating in a community savings group. In terms of demographic characteristics, older women (OR = 1.54, 95% CI 1.07–2.24) and married women (OR = 1.84, 95% CI 1.16–2.93) were more likely to be in a savings group. We also found statistically significant associations between the following financial indicators and group participation: higher pay per sexual encounter (OR = 1.86, 95% CI 1.27–2.72), higher total income (OR = 2.40, 95% CI 1.64–3.51) and higher sex work income (OR = 1.81, 95% CI 1.24–2.74), having one or more financial dependents (OR = 2.03, 95% CI 1.31–3.14), and having someone who can help in a financial emergency (OR = 1.74, 95% CI 1.19–2.53).
Table 2.
Characteristics associated with participating in a community savings group (N = 496)
| Variables | Odds ratio | 95% CI | p-value |
|---|---|---|---|
| Older age | 1.54 | 1.07–2.24 | 0.022 |
| Married | 1.84 | 1.16–2.93 | 0.010 |
| Higher pay per sex act | 1.86 | 1.27–2.72 | 0.001 |
| Higher total income | 2.40 | 1.64–3.51 | 0.000 |
| Higher sex work income | 1.81 | 1.24–2.74 | 0.002 |
| Has one or more dependents | 2.03 | 1.31–3.14 | 0.002 |
| Has emergency financial help | 1.74 | 1.19–2.53 | 0.004 |
Factors Associated with Consistent Condom Use
Bivariate logistic regression results of factors associated with CCU at p ≤ 0.10 significance level with any partner type are shown in Table 3. Community savings group participation was significantly associated with CCU with new clients (OR = 2.43, 95% CI 1.56–3.79) and regular clients (OR = 1.65, 95% CI 1.07–2.54) but not with steady, non-paying partners. Higher total income (OR = 2.31, 95% CI 1.50–3.55), higher sex work income (OR = 2.81, 95% CI 1.82–4.34), higher pay per sex act (OR = 2.67, 95% CI 1.71–4.15), having one or more financial dependents (OR = 2.52, 95% CI 1.51–4.21), and higher self-perceived financial security (OR = 1.71, 95% CI 0.92–3.19) were all positively associated with CCU with new clients. In a sub-analysis examining CCU across the ten categories of total income, there was a steady increase in new client CCU with increasing income. Older age (OR = 0.70, 95% CI 0.46–1.06) and longer time in sex work (OR = 0.55, 95% CI 0.36–0.84) were negatively associated with CCU with new clients. All factors (savings group participation, higher total monthly income, higher monthly sex work income, higher pay per sex act, older age, longer time in sex work, and having financial dependents) except for higher self-perceived financial security were significantly associated with CCU with regular clients. With steady, non-paying partners, higher sex work income (OR = 1.56, 95% CI 0.98–2.49), higher pay per sex act (OR = 1.49, 95% CI 0.93–2.39), and higher self-perceived financial security (OR = 1.79, 95% CI 0.94–3.40) were positively associated with CCU and longer time in sex work (OR = 0.57, 95% CI 0.35–0.91) was negatively associated with CCU.
Table 3.
Bivariate analysis for financial security and sex work characteristics associated with consistent condom use (CCU) in the last 30 days by partner type
| Variables | CCU with NEW clients | CCU with REGULAR clients | CCU with NON-PAYING partners | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Odds ratio | 95% CI | p-value | Odds ratio | 95% CI | p-value | Odds ratio | 95% CI | p-value | |
| Participates in a community savings group | 2.43 | 1.56–3.79 | 0.000 | 1.65 | 1.07–2.54 | 0.023 | 1.42 | 0.88–2.29 | 0.155 |
| Higher total monthly income | 2.31 | 1.50–3.55 | 0.000 | 1.54 | 1.01–2.37 | 0.046 | 1.40 | 0.87–2.24 | 0.164 |
| Higher monthly sex work income | 2.81 | 1.82–4.34 | 0.000 | 2.11 | 1.38–3.22 | 0.001 | 1.56 | 0.98–2.49 | 0.060 |
| Higher pay per sex act | 2.67 | 1.71–4.15 | 0.000 | 2.58 | 1.68–3.96 | 0.000 | 1.49 | 0.93–2.39 | 0.099 |
| Age (> 25) | 0.70 | 0.46–1.06 | 0.095 | 0.69 | 0.45–1.06 | 0.091 | 0.77 | 0.48–1.23 | 0.278 |
| Length of time in sex work (≥ 5 years) | 0.55 | 0.36–0.84 | 0.006 | 0.60 | 0.39–0.91 | 0.018 | 0.57 | 0.35–0.91 | 0.019 |
| Has one or more dependents | 2.52 | 1.51–4.21 | 0.000 | 1.82 | 1.10–3.02 | 0.020 | 1.53 | 0.87–2.67 | 0.138 |
| Higher self-perceived financial security | 1.71 | 0.92–3.19 | 0.090 | 1.36 | 0.73–2.54 | 0.335 | 1.79 | 0.94–3.40 | 0.076 |
The final multivariable logistic regression models of factors associated with CCU by partner type are presented in Table 4. Potentially confounding variables that were not significant and had a negligible effect on the estimated associations of the other covariates with the outcome were omitted from the final model, which was determined to be the most parsimonious fit for the data. When controlling for other characteristics, participating in a community savings group was significantly associated with nearly two times greater odds of CCU with new clients in the past 30 days (aOR = 1.77, 95% CI 1.10–2.86). Participating in a community savings group was not significantly associated with CCU with regular clients or with steady, non-paying partners in multivariable models. Other factors significantly associated with CCU with new clients in multivariable analysis were receiving higher pay per sex act (aOR = 1.78, 95% CI 1.09–2.43) and having one or more dependents (aOR = 2.04, 95% CI 1.18–3.53). Receiving higher pay per sex act was also significantly associated with condom use with regular clients (aOR = 2.25, 95% CI 1.36–3.70).
Table 4.
Multivariable logistic regression model for factors associated with consistent condom use (CCU) in past 30 days by partner type
| Variables | CCU with NEW clients | CCU with REGULAR clients | CCU with NON-PAYING partners | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Adjusted ORa | 95% CI | p-value | Adjusted ORa | 95% CI | p-value | Adjusted ORa | 95% CI | p-value | |
| Participates in a community savings group | 1.77 | 1.10–2.86 | 0.019 | 1.40 | 0.89–2.21 | 0.148 | 1.33 | 0.81–2.19 | 0.264 |
| Higher total income | 1.52 | 0.94–2.43 | 0.085 | 0.99 | 0.61–1.60 | 0.943 | 1.08 | 0.64–1.81 | 0.780 |
| Higher pay per sex act | 1.78 | 1.09–2.43 | 0.022 | 2.25 | 1.36–3.70 | 0.001 | 1.11 | 0.65–1.90 | 0.701 |
| Has one or more dependents | 2.04 | 1.18–3.53 | 0.011 | 1.68 | 0.98–2.88 | 0.060 | 1.36 | 0.76–2.42 | 0.306 |
| Length of time in sex work | 0.64 | 0.40–1.03 | 0.064 | 0.79 | 0.50–1.27 | 0.336 | 0.60 | 0.36–1.00 | 0.050 |
Adjusted for intra-class correlation due to clustering in venues
Exploratory mediation analysis indicated that the relationship between savings group participation and CCU with new clients was partially mediated by financial security, as measured by total monthly income (Fig. 1). The strength of the direct relationship between savings group participation and CCU with new clients was reduced after controlling for monthly income in the model, and the standardized regression coefficients of both the direct effect (βc′ = 0.18, 95% CI 0.06–0.30) and the indirect effect (βb = 0.05, 95% CI 0.02–0.10) were statistically significant with approximately 23% of the total effect of savings groups on CCU being mediated by financial security. Thus, there remained a substantial direct effect of savings group participation and CCU with new clients, after accounting for the mediation effect of financial security.
Fig. 1.
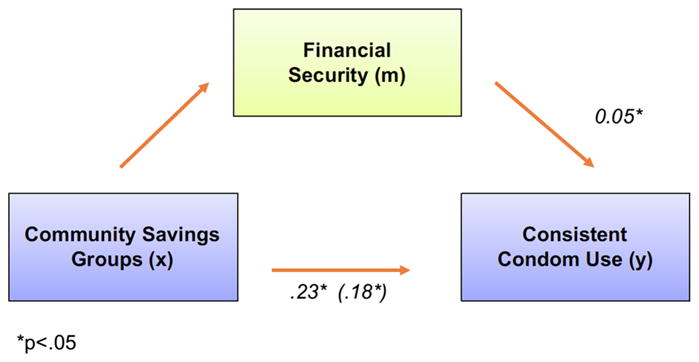
Mediation analysis examining the role of financial security in the effect of community savings group participation on CCU with new clients
Discussion
This study found that FSW in Iringa, Tanzania who participate in community savings groups had nearly two times greater odds of CCU with new clients in the last 30 days compared to their peers who do not participate in the groups. Results indicate that savings groups may alter economic vulnerability, a critical structural barrier impeding condom use among FSW. These findings have implications for the promising role of such groups as a sustainable, community-established and community-led effort to improve financial security and reduce economic vulnerability to sexual risk with clients among this high-risk population.
Examining characteristics associated with savings group participation among the sample allowed us to understand demographic characteristics of group members. However, with regards to the associated financial indicators (e.g., higher income associated with community savings group participation), it is unclear from this cross-sectional analysis whether these characteristics are the effects of being in the groups or factors facilitating women being able to join and participate in the groups. Longitudinal research is needed to address the issue of temporality and further our understanding of the underlying mechanisms at play in these relationships. Noting our finding that FSW participating in savings groups tend to be older, future studies should consider examining the role of savings in condom use behavior with clients from a life-course perspective. Particularly given the focus on young women in sub-Saharan Africa who have exceptionally high rates of new HIV infections [35], future research should explore both why younger women may not be as likely to participate in such groups and the potential of broadening the appeal of these groups to younger women.
Our finding that the relationship between savings group participation and CCU is strongest with new clients is particularly important given that new clients are often “gateway clients,” meaning that a new client can become a future regular client or steady partner [36]. Hence, establishing a norm of CCU with new clients may allow for greater CCU with these other partner types over time, if such transitions occur. Our findings that savings group participation was not associated with CCU with regular clients or steady, non-paying partners in multivariable analysis are consistent with prior research showing that relationship intimacy between FSW and their sexual partners impacts safer sex decision-making; specifically, condom use decreases with increasing relationship intimacy [36–39]. Reliable income from regular clients and finan-cial support from steady partners also complicate condom negotiations as requesting condom use could mean losing a client who regularly provides income or losing financial support from a partner. Interventions intended to impact condom use among FSW must examine the socioeconomic dynamics of their relationships with clients and partners.
Exploratory mediation analysis suggests that financial security, as measured by monthly income, may partially mediate the association between savings group participation and condom use with new clients. Furthermore, the signifi-cant direct effect detected suggests that beyond the effect of savings group participation on CCU through improved financial security, there is a residual positive effect, a benefit beyond financial security alone that contributes to reduced risk behaviors. For example, the groups may be providing other support mechanisms that empower women with a sense of agency to take control of their sexual risk. Similarly, the association between CCU and receiving higher pay per sex act may indicate that group participation provides a financial cushion allowing women to accept only clients offering higher pay for sex or it may be revealing a sense of empowerment among FSW in the groups enabling them to engage in price negotiations with clients.
Our findings are consistent with studies from other settings indicating that access to savings can mitigate economic vulnerability to engage in unsafe sex among FSW [27, 32]. Determining what the groups may be providing beyond financial security requires further examination but our results certainly resonate with prior research on the promising role of collectivization among FSW to address financial vulnerabilities [40] and the compelling evidence on the role of community empowerment in reducing HIV risk behaviors among FSW [26]. Future longitudinal analysis will allow us to assess how these groups function as an empowerment intervention, including changes in social cohesion and leadership among the FSW community that occur as part of the parent study’s combination prevention intervention.
There are several limitations to this study. Our primary study outcome of condom use and financial indicators such as income were self-reported which are subject to both recall bias and social desirability bias [41]. The use of cross-sectional data limits our ability to make causal inferences regarding the relationship between participating in a community savings group and condom use with clients. Future research should include utilizing longitudinal data to allow for observation prior to and following FSW joining and participating in savings groups and the groups’ effects on sexual risk behaviors as well as changes in HIV infection over time. Additionally, the mediation analysis should be considered preliminary; while a mediating relationship can be hypothesized, the mechanisms through which savings group participation may impact safer sex practices with clients remain unknown. Thus, future analysis should further investigate mediation and explore pathways among these relationships.
This study was unique in that it focused on organically formed community savings groups established for the purposes of improving financial security and specifically examined the potential for group participation to serve as an HIV-protective behavior among FSW. Community savings groups are an accepted element of Tanzanian society and thus may offer a valuable platform for engagement in HIV prevention. Such groups are commonplace in other sub-Saharan African countries and around the world. Utilizing an existing and culturally accepted activity within the community offers a sustainable mechanism for reaching people, particularly those who are socioeconomically disadvantaged, with HIV prevention programming. Future research should further explore the potential of such groups in combating the HIV epidemic among women at high risk in other settings including among women living with HIV.
Conclusions
Programmatic strategies for HIV prevention with FSW must address the economic realities of sex workers’ lives that impede safer sex behaviors. Community savings groups may serve as an HIV prevention strategy to support a basic level of economic security for FSW, better positioning them to engage in condom negotiation with clients. Our study findings suggest the promising role of community savings groups as a structural intervention to promote financial security and reduce HIV risk among FSW. The community savings groups that are the subject of this study should be considered one component of a comprehensive prevention package. Our findings indicate that different risk reduction strategies are needed to address the distinct dynamics present between FSW and their steady partners versus new or regular clients. As a community-led effort, savings groups are most appropriately situated within a community-empowerment approach to HIV prevention through which FSW design and implement programs to address structural barriers to their health within their own community. Further research on this topic across diverse settings will enhance our understanding of how savings groups can best be implemented and potentially taken to scale as part of comprehensive, community-led HIV prevention efforts among FSW.
Acknowledgments
Funding This work was supported by the National Institute of Mental Health through R01MH104044 and the National Institute of Allergy and Infectious Disease of the National Institutes of Health through T32AI050056. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Compliance with Ethical Standards
Conflict of interest The authors declare that they have no conflict of interest.
Ethical Approval All procedures performed in studies involving human participants were in accordance with the Ethical Standards of the Institutional and/or National Research Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent Informed consent was obtained from all individual participants included in the study.
References
- 1.Baral S, Beyrer C, Muessig K, Poteat T, Wirtz AL, Decker MR, et al. Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12(7):538–49. doi: 10.1016/S1473-3099(12)70066-X. [DOI] [PubMed] [Google Scholar]
- 2.Kerrigan D, Wirtz A, Baral S, Decker M, Murray L, Poteat T, et al. The global HIV epidemics among sex workers. Washington, DC: World Bank; 2013. [Google Scholar]
- 3.Tanzania Commission for AIDS (TACAIDS), Zanzibar AIDS Commission (ZAC), National Bureau of Statistics (NBS), Office of Chief Government Statistician (OCGS), ICF International. Tan-zania HIV/AIDS and Malaria Indicator Survey 2011–12. Dar es Salaam; 2013. [Google Scholar]
- 4.Beckham S, Kennedy C, Brahmbhatt H, et al. Research brief: female sex workers. Baltimore: 2013. Strategic assessment to define a comprehensive response to HIV in Iringa, Tanzania. [Google Scholar]
- 5.Tanzania National AIDS Control Program, PSI Tanzania. Female sex workers in seven regions. Dar es Salaam; Iringa, Mbeya, Mwanza, Tabora, Shinyanga and Mara: 2013. HIV biological and behavioral surveys: Tanzania 2013. [Google Scholar]
- 6.Tsai LC, Witte SS, Aira T, Riedel M, Hwang HG, Ssewamala F. There is no other option; we have to feed our families…who else would do it?”: the financial lives of women engaging in sex work in Ulaanbaatar, Mongolia. Glob J Health Sci. 2013;5(5):41–50. doi: 10.5539/gjhs.v5n5p41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fitzgerald-Husek A, Martiniuk AL, Hinchcliff R, Aochamus CE, Lee RB. I do what I have to do to survive”: an investigation into the perceptions, experiences and economic considerations of women engaged in sex work in Northern Namibia. BMC Women’s Health. 2011;11:35. doi: 10.1186/1472-6874-11-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reed E, Gupta J, Biradavolu M, Devireddy V, Blankenship KM. The context of economic insecurity and its relation to violence and risk factors for HIV among female sex workers in Andhra Pradesh, India. Public Health Rep. 2010;125(Suppl 4):81–9. doi: 10.1177/00333549101250S412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ngo AD, McCurdy SA, Ross MW, Markham C, Ratliff EA, Pham HT. The lives of female sex workers in Vietnam: findings from a qualitative study. Cult Health Sex. 2007;9(6):555–70. doi: 10.1080/13691050701380018. [DOI] [PubMed] [Google Scholar]
- 10.Saggurti N, Jain AK, Sebastian MP, Singh R, Modugu HR, Halli SS, et al. Indicators of mobility, socio-economic vulnerabilities and HIV risk behaviours among mobile female sex workers in India. AIDS Behav. 2012;16(4):952–9. doi: 10.1007/s10461-011-9937-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Phrasisombath K, Faxelid E, Sychareun V, Thomsen S. Risks, benefits and survival strategies—views from female sex workers in Savannakhet, Laos. BMC Public Health. 2012;12:1004. doi: 10.1186/1471-2458-12-1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agha S, Chulu Nchima M. Life-circumstances, working conditions and HIV risk among street and nightclub-based sex workers in Lusaka, Zambia. Cult Health Sex. 2004;6(4):283–99. doi: 10.1080/13691050410001680474. [DOI] [PubMed] [Google Scholar]
- 13.Onyeneho NG. HIV/AIDS risk factors and economic empower-ment needs of female sex workers in Enugu Urban, Nigeria. Tan-zan J Health Res. 2009;11(3):126–35. doi: 10.4314/thrb.v11i3.47698. [DOI] [PubMed] [Google Scholar]
- 14.USAID Project Search. HIV among female sex workers and men who have sex with men in Swaziland. Baltimore: USAID | Project Search: Research to Prevention; 2013. [Google Scholar]
- 15.Wojcicki JM, Malala J. Condom use, power and HIV/AIDS risk: sex-workers bargain for survival in Hillbrow/Joubert Park/Berea, Johannesburg. Soc Sci Med (1982) 2001;53(1):99–121. doi: 10.1016/s0277-9536(00)00315-4. [DOI] [PubMed] [Google Scholar]
- 16.Urada LA, Morisky DE, Pimentel-Simbulan N, Silverman JG, Strathdee SA. Condom negotiations among female sex workers in the Philippines: environmental influences. PLoS ONE. 2012;7(3):e33282. doi: 10.1371/journal.pone.0033282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Adu-Oppong A, Grimes RM, Ross MW, Risser J, Kessie G. Social and behavioral determinants of consistent condom use among female commercial sex workers in Ghana. AIDS Educ Prev Off Publ Int Soc AIDS Educ. 2007;19(2):160–72. doi: 10.1521/aeap.2007.19.2.160. [DOI] [PubMed] [Google Scholar]
- 18.Umar US, Adekunle AO, Bakare RA. Pattern of condom use among commercial sex workers in Ibadan, Nigeria. Afr J Med Med Sci. 2001;30(4):285–90. [PubMed] [Google Scholar]
- 19.Bharat S, Mahapatra B, Roy S, Saggurti N. Are female sex workers able to negotiate condom use with male clients? The case of mobile FSWs in four high HIV prevalence states of India. PLoS ONE. 2013;8(6):e68043. doi: 10.1371/journal.pone.0068043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rao V, Gupta I, Lokshin M, Jana S. Sex workers and the cost of safe sex: the compensating differential for condom use among Calcutta prostitutes. J Dev Econ. 2003;71(2):585–603. [Google Scholar]
- 21.Elmes J, Nhongo K, Ward H, Hallett T, Nyamukapa C, White PJ, et al. The price of sex: condom use and the determinants of the price of sex among female sex workers in eastern Zimbabwe. J Infect Dis. 2014;210(Suppl 2):S569–78. doi: 10.1093/infdis/jiu493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gertler P, Shah M, Bertozzi S. Sex sells, but risky sex sell for more. 2003 [Google Scholar]
- 23.Ntumbanzondo M, Dubrow R, Niccolai LM, Mwandagalirwa K, Merson MH. Unprotected intercourse for extra money among commercial sex workers in Kinshasa, Democratic Republic of Congo. AIDS Care. 2006;18(7):777–85. doi: 10.1080/09540120500412824. [DOI] [PubMed] [Google Scholar]
- 24.Moret W. Economic strengthening for female sex workers: a review of the literature. USA: ASPIRES, FHI; 2014. p. 360. [Google Scholar]
- 25.Global Network of Sex Work Projects (NSWP) Economic empowerment programmes for sex workers—regional report: Africa. 2015 [Google Scholar]
- 26.Kerrigan D, Kennedy CE, Morgan-Thomas R, Reza-Paul S, Mwangi P, Win KT, et al. A community empowerment approach to the HIV response among sex workers: effectiveness, challenges, and considerations for implementation and scale-up. Lancet. 2015;385(9963) doi: 10.1016/S0140-6736(14)60973-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Swendeman D, Basu I, Das S, Jana S, Rotheram-Borus MJ. Empowering sex workers in India to reduce vulnerability to HIV and sexually transmitted diseases. Soc Sci Med. 1982;69(8):1157–66. doi: 10.1016/j.socscimed.2009.07.035. 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ghose T, Swendeman D, George S, Chowdhury D. Mobilizing collective identity to reduce HIV risk among sex workers in Sona-gachi, India: the boundaries, consciousness, negotiation framework. Soc Sci Med. 1982;67(2):311–20. doi: 10.1016/j.socscimed.2008.03.045. 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Basu I, Jana S, Rotheram-Borus MJ, Swendeman D, Lee S-J, Newman P, et al. HIV prevention among sex workers in India. J Acquir Immune Defic Syndr. 1999;36(3):845–52. doi: 10.1097/00126334-200407010-00012. 2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fehrenbacher AE, Chowdhury D, Ghose T, Swendeman D. Consistent condom use by female sex workers in Kolkata, India: testing theories of economic insecurity, behavior change, life course vulnerability and empowerment. AIDS Behav. 2016;20(10):2332–45. doi: 10.1007/s10461-016-1412-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pillai P, Bhattacharjee P, Ramesh BM, Isac S. Impact of two vulnerability reduction strategies—collectivisation and participation in savings activities—on HIV risk reduction among female sex workers. Karnataka Health Promotion Trust (KHPT); 2012. [Google Scholar]
- 32.Witte SS, Aira T, Tsai LC, Riedel M, Offringa R, Chang M, et al. Efficacy of a savings-led microfinance intervention to reduce sexual risk for HIV among women engaged in sex work: a randomized clinical trial. Am J Public Health. 2015;105(3):e95–102. doi: 10.2105/AJPH.2014.302291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kerrigan D, Mbwambo J, Likindikoki S, Beckham S, Mwampashi A, Shembilu C, et al. Project Shikamana: baseline findings from a community empowerment-based combination HIV prevention trial among female sex workers in Iringa, Tanzania. J Acquir Immune Defic Syndr. 2017;74(Suppl 1):S60–8. doi: 10.1097/QAI.0000000000001203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zeger S, Liang K, Albert PS. Models for longitudinal data: a generalized estimating equation approach. Biometrics. 1988;44(4):1049–60. [PubMed] [Google Scholar]
- 35.Joint United Nations Programme on HIV/AIDS (UNAIDS) HIV prevention among adolescent girls and young women. Geneva: 2016. [Google Scholar]
- 36.Robertson AM, Syvertsen JL, Amaro H, Martinez G, Rangel MG, Patterson TL, et al. Can’t buy my love: a typology of female sex workers’ commercial relationships in the Mexico–U.S. Border Region. J Sex Res. 2014;51(6):711–20. doi: 10.1080/00224499.2012.757283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Murray L, Moreno L, Rosario S, Ellen J, Sweat M, Kerrigan D. The role of relationship intimacy in consistent condom use among female sex workers and their regular paying partners in the Dominican Republic. AIDS Behav. 2007;11(3):463–70. doi: 10.1007/s10461-006-9184-5. [DOI] [PubMed] [Google Scholar]
- 38.Andrews CH, Faxelid E, Sychaerun V, Phrasisombath K. Determinants of consistent condom use among female sex workers in Savannakhet, Lao PDR. BMC Women’s Health. 2015;15:63. doi: 10.1186/s12905-015-0215-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Le MN, D’Onofrio CN, Rogers JD. HIV risk behaviors among three classes of female sex workers in Vietnam. J Sex Res. 2010;47(1):38–48. doi: 10.1080/00224490902999278. [DOI] [PubMed] [Google Scholar]
- 40.Patel SK, Prabhakar P, Jain AK, Saggurti N, Adhikary R. Relationship between community collectivization and financial vulnerability of female sex workers in Southern India. PLoS ONE. 2016;11(5):e0156060. doi: 10.1371/journal.pone.0156060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hanck SE, Blankenship KM, Irwin KS, West BS, Kershaw T. Assessment of self-reported sexual behavior and condom use among female sex workers in India using a polling box approach: a preliminary report. Sex Transm Dis. 2008;35(5):489–94. doi: 10.1097/OLQ.0b013e3181653433. [DOI] [PubMed] [Google Scholar]


