Background
In 2015, prescription opioids and heroin overdoses resulted in more than 30,000 fatalities in the United States (US).1 The preventable deaths in these young and relatively healthy victims have contributed to the expansion of a scarce donor organ pool for critically ill patients waitlisted for solid organ transplantation due to single/multi-organ failure refractory to medical treatment options.2 The aim of this study was to evaluate the contribution and outcomes associated with the utilization of drug overdose (DO) donors on solid organ transplantation in the US.
Methods
We performed a retrospective analysis using the United Network for Organ Sharing (UNOS) database from January 1, 2000, to December 31, 2016, to study the annual trends in the etiology of death leading to organ donation for kidney, liver, heart, and lung transplantation in the US. In addition, we compared donor demographics and characteristics of DO organ donors versus all other causes of organ donation. Kaplan-Meir survival analyses were performed to determine post-transplant patient survival rates among liver and kidney transplant recipients. Due to the small sample size, post-transplant outcomes in heart and lung transplant recipients were not analyzed. Using the Center for Disease Control (CDC) WONDER database, crude cause-specific mortality rates (per 100,000 persons) due to DO were determined.3 SAS statistical software version 9.4 (SAS Institute Inc., Cary, NC, USA) was used.
Results
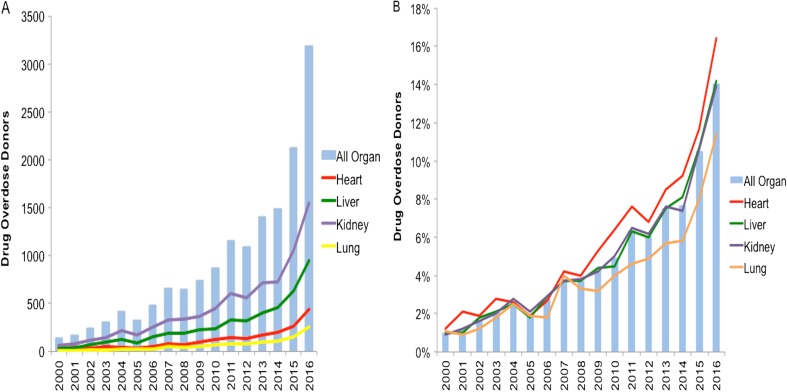
From 2000 to 2016, a total of 290,102 adult deceased donor-related kidney (50.6%), liver (29.8%), heart (11.2%), and lung (8.4%) transplant surgeries were performed in the US. Of these, 15,359 (5.3%) donors died from DO. The annual number and proportion of solid organ transplants utilizing DO donors have rapidly increased since 2012 as depicted in Fig. 1a, b. Compared to all other causes of organ donation, donors due to DO were significantly younger with a higher prevalence of Caucasians and hepatitis C virus (HCV) seropositivity (Table 1). More importantly, DO-related liver and kidney donor organs were associated with a significantly higher 1-year patient survival rate (Table 1). In 2016, over 25% of solid organ transplants in UNOS regions spanning the Northeast and Mid-Atlantic states (UNOS regions 1, 2, and 9) utilized DO donors. These geographic areas in the US also demonstrated the highest cause-specific mortality rates from DO (34.9 per 100,000 persons) in 2016. Among HCV seropositive donor organ pool, allografts procured from DO donors increased by 24% annually, accounted for nearly 50% of all HCV seropositive donor organs in 2016, and were noted to have a lower liver donor risk and kidney donor profile indices compared to all other allografts. In a sub-analysis, observed 1-year survival rates in liver transplant recipients with HCV seropositive DO organs were statistically comparable to non-HCV DO organs (HCV seropositive 92.5% vs. non-HCV DO 91.8%, P = 0.34) following the introduction of direct-acting antiviral (DAA) therapy in late 2013.
Fig. 1.
Annual trends in donors from drug overdose utilized in solid organ transplantation in the United States from 2000 to 2016. a Annual trend in the number of drug overdose donors. b Annual trend in the percentage of donors utilized from drug overdose.
Table 1.
Comparison of Demographics, Characteristics and Post-Transplant Survival Among Donors from Drug Overdose Versus All Other Causes
| Drug overdose (n = 15,359) | All other causes (n = 274,743) | P value | |
|---|---|---|---|
| Mean age (SD), year | 31.4 (10.1) | 38.5 (16.5) | < 0.001 |
| Ethnicity (%) | < 0.001 | ||
| Caucasian | 13,086 (85.2) | 184,730 (67.2) | < 0.001 |
| African-American | 853 (2.6) | 41,657 (15.2) | < 0.001 |
| Hispanic | 1127 (7.3) | 37,962 (13.8) | < 0.001 |
| Asian | 135 (0.9) | 6353 (2.3) | < 0.001 |
| Other | 158 (1.0) | 3998 (1.5) | < 0.001 |
| Gender (%) | < 0.001 | ||
| Female | 6475 (42.2) | 106,381 (38.7) | |
| Male | 8884 (57.8) | 168,361 (61.3) | |
| PHS/CDC high risk* (%) | 7602 (49.5) | 22,747 (8.3) | < 0.001 |
| HCV seropositive† (%) | 1584 (10.3) | 5827 (2.1) | < 0.001 |
| Mean cold ischemia time (SD), h | 3.9 (1.7) | 4.0 (1.7) | 0.156 |
| Donor organ type‡ (%) | |||
| Liver | 4541 (5.3%) | 81,798 (94.7%) | < 0.001 |
| Kidney | 7728 (5.3%) | 138,951 (94.7%) | < 0.001 |
| Heart | 1938 (6.1%) | 30,692 (93.9%) | < 0.001 |
| Lung | 1107 (4.5%) | 23,302 (95.5%) | < 0.001 |
| Liver | |||
| Liver donor risk index§ (SD) | 1.2 (0.3) | 1.4 (0.4) | < 0.001 |
| 1-year patient survival (95% CI), % | 91.4% (90.6–92.3) | 89.1 (88.9–89.3) | < 0.001 |
| Kidney | |||
| Kidney donor profile index‖ (SD) | 32.7 (19.9) | 48.7 (28.1) | < 0.001 |
| 1-year patient survival (95% CI), % | 96.4% (95.9–96.8) | 94.5% (94.9–95.1) | < 0.001 |
*Public Health Service/Center for Disease Control (PHS/CDC) high-risk donor for hepatitis C virus, human immunodeficiency virus, and hepatitis B virus infection
†Hepatitis C virus (HCV) antibody seropositive
‡Percentage of drug overdose or all other donors calculated by donor organ type
§Liver donor risk index (LDRI) score is a quantitative assessment of the risk of donor liver graft failure based on donor age, ethnicity, height, cause of death split or partial graft, cold ischemia time, and location of organs based on donor service area. LDRI score was provided by the United Network of Organ Sharing
‖Kidney donor profile index (KDPI) score is a quantitative assessment of the risk of donor kidney graft failure based on donor age, height, weight, ethnicity, cause of death, HCV serologic status, history of hypertension and diabetes, and serum creatinine. KDPI score was provided by the United Network of Organ Sharing
Discussion
Deaths related to DO have now become a significant contributor to the expansion of the deceased donor organ pool for solid organ transplantation in the US. Noted limitations of this study include details related to drug exposure—type/dosage/duration/timing and the retrospective design of the study. The unfortunate reality is that DO has led to the tragic loss of our nation’s youth. However, these young, otherwise healthy, donors have lower donor risk indices, leading to higher liver and kidney transplant survival rates compared to all other donors. With the availability of efficacious DAA agents for the treatment of HCV in the post-transplant setting,4 the utilization rate of DO organs is steadily rising despite the increased risk for disease transmission as the transplant community recognizes the true life-saving impact from this untimely loss of life.
Acknowledgements
We would like to acknowledge the United Network for Organ Sharing, a non-profit organization that administrates the Organ Procurement and Transplantation Network, from which our data was collected.
Abbreviations
- DAA
Direct-acting antiviral
- DO
Drug overdose
- CDC
Center for Disease Control
- CIT
Cold ischemia time
- HCV
Hepatitis C virus
- UNOS
United Network for Organ Sharing
- US
United States
Author Contributions
G.C and A.A.—study concept and design, acquisition of data, analysis and interpretation of data, drafting and critical revision of the manuscript, and study supervision.
A.A.L., R.C., A.E.T, and J.S.G.—study concept and design, interpretation of data, drafting of the manuscript, and critical revision of the manuscript.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
References
- 1.Goldberg DS, Blumberg E, McCauley M, Abt P, Levine M. Improving organ utilization to help overcome the tragedies of the opioid epidemic. Am J Transplant. 2016;16(10):2836–2841. doi: 10.1111/ajt.13971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Drug overdose death data. https://www.cdc.gov/drugoverdose/data/statedeaths.html; 2018. Accessed on April 12, 2018.
- 3.Centers for Disease Control (CDC). Wide-ranging Online Data for Epidemiological Research (CDC WONDER) Database. Available from www.wonder.cdc.gov; 2018. Accessed on April 12, 2018.
- 4.Cholankeril George, Li Andrew A., March Katherine L., Yoo Eric R., Kim Donghee, Snyder Heather, Gonzalez Stevan A., Younossi Zobair M., Ahmed Aijaz. Improved Outcomes in HCV Patients Following Liver Transplantation During the Era of Direct-Acting Antiviral Agents. Clinical Gastroenterology and Hepatology. 2018;16(3):452–453. doi: 10.1016/j.cgh.2017.08.020. [DOI] [PubMed] [Google Scholar]