INTRODUCTION
As noted in prior wars such as the 1991 Gulf War, increasing evidence indicates that, chronic multisystem medically unexplained symptoms, referred to as chronic multisymptom illness (CMI), are commonly experienced by Veterans returning from Operations Enduring Freedom, Iraqi Freedom, and New Dawn (OEF/OIF/OND) 1, 2. Females may be at higher risk for CMI based on evidence among civilian populations and veterans from prior conflicts 3–5. Little is known regarding the sex-specific CMI prevalence among OEF/OIF/OND deployed veterans or related healthcare utilization. Among OEF/OIF/OND veterans nationwide and stratified by sex, we sought to estimate the prevalence of CMI-related diagnoses (hereafter referred to as CMI) and to explore trends in CMI-related (versus non-CMI-related) outpatient healthcare utilization in the Veterans Health Administration (VHA).
METHODS
Our serial cross-sectional study included 501,996 males and 69,611 females from the OEF/OIF/OND Roster provided by the Department of Defense who had encounters in any VHA facility nationwide after their last deployment end date from fiscal years 2002–2011 6. We defined CMI as one or more International Classification of Diseases, 9th edition, Clinical Modification (ICD-9-CM) coded diagnosis of chronic fatigue syndrome (CFS, 780.71), fibromyalgia (FMS, 729.1), or irritable bowel syndrome (IBS, 564.1). We estimated adjusted prevalence ratios (PR) for demographic and military service characteristics associated with CMI by fitting generalized linear “Log Poisson” regression models, and robust standard errors (STATA v 14.2, College Station Tx), with two-sided p values < 0.05. We identified the settings of outpatient encounters including primary care and specialty care clinics such as gastrointestinal, pain, and rheumatology/arthritis. We defined CMI-related outpatient utilization as VHA encounters with a documented ICD-9-CM code for CMI and calculated the yearly mean number. This study was approved by our Institutional Review Board.
RESULTS
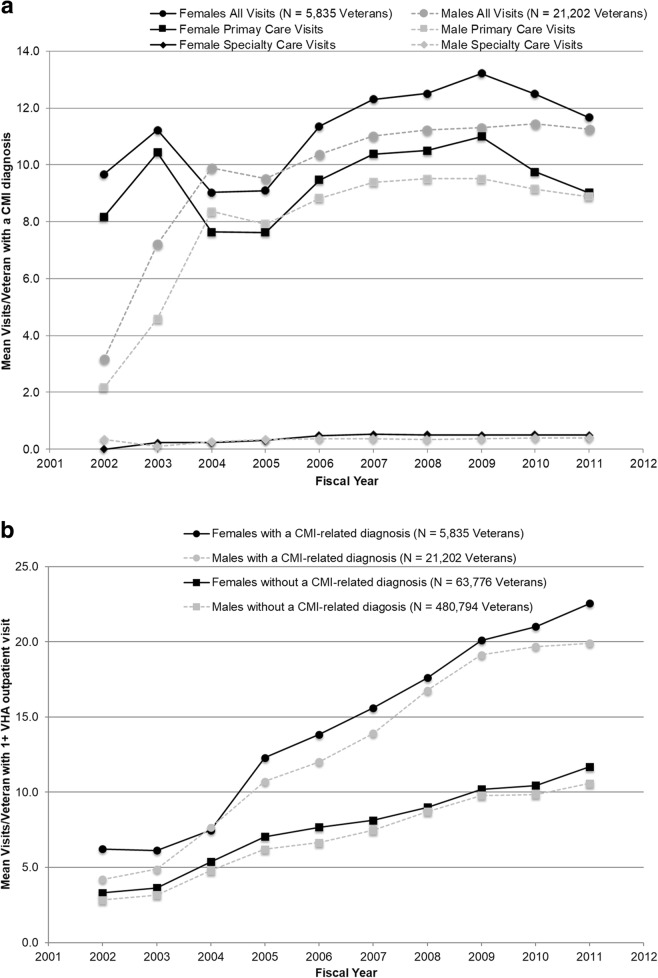
The prevalence of CMI was 4.2% in males and 8.4% in females. The higher prevalence in females versus males was consistent for CFS (3.3% versus 1.7%), FMS (9.2% versus 2.6%), and IBS (3.5% versus 1.6%). Age ≥ 30 years (PR 1.14, 95% CI 1.11–1.17) and being married (PR 1.13, 95% CI 1.10–1.16) were associated with CMI (Table 1). Enlisted rank (PR 1.35, 95% CI 1.28–1.42) and Army military branch (PR: 1.22, 95% CI 1.18–1.25) were also associated with CMI in our fully adjusted models. Over the 10-year period, the mean yearly average number of CMI-related outpatient encounters was 11.3 in females and 9.6 in males; visit counts/veteran were higher among females across all years and care settings (Fig. 1a). Total outpatient utilization was higher among veterans with CMI compared to those without CMI (13.2 versus 7.1 yearly mean visits), regardless of sex (Fig. 1b). Among veterans with CMI, total outpatient utilization was higher in females versus males (14.3 versus 12.9 yearly mean visits). Among OEF/OIF/OND veterans without CMI, total outpatient utilization was higher among females versus males (7.7 versus 7.0 yearly mean visits).
Table 1.
Demographic and Military Service Characteristics Associated with Chronic Multisymptom Illness-Related Diagnoses
| Demographic characteristics | CMI dx/No CMI dx N = 27,037/544,570 |
Prevalence ratio (95% confidence interval) | ||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | ||
| Male sex | 5835/63,776 | 1 (ref) | 1 (ref) | 1 (ref) |
| Female sex | 21,202/480,794 | 1.98 (1.93, 2.04) | 2.02 (1.96, 2.07) | 2.05 (1.99, 2.11) |
| Age at first VHA visit | ||||
| 18–24 years | 6705/149,455 | 1 (ref) | 1 (ref) | 1 (ref) |
| 25–29 years | 6134/130,649 | 1.04 (1.01, 1.08) | 1.03 (1.00, 1.07) | 1.02 (0.98, 1.05) |
| 30–39 years | 7829/139,540 | 1.24 (1.20, 1.28) | 1.24 (1.20, 1.28) | 1.18 (1.13, 1.22) |
| 40+ years | 6364/124,856 | 1.13 (1.09, 1.17) | 1.16 (1.12, 1.20) | 1.10 (1.06, 1.15) |
| Race/ethnicity | ||||
| White | 12,713/272,580 | 1 (ref) | 1 (ref) | 1 (ref) |
| Black | 2877/59,153 | 1.04 (1.00, 1.08) | 0.91 (0.88, 0.95) | 0.90 (0.87, 0.94) |
| Hispanic | 3042/57,849 | 1.12 (1.08, 1.17) | 1.09 (1.05, 1.14) | 1.11 (1.06, 1.15) |
| Other | 1301/26,877 | 1.04 (0.98, 1.10) | 0.97 (0.91, 1.02) | 1.02 (0.96, 1.08) |
| Missing | 7104/128,111 | 1.18 (1.15, 1.21) | 1.13 (1.10, 1.17) | 1.21 (1.18, 1.25) |
| Marital status | ||||
| Not currently married | 14,374/307,192 | 1 (ref) | 1 (ref) | 1 (ref) |
| Married | 12,647/237,106 | 1.13 (1.11, 1.16) | 1.14 (1.11, 1.17) | 1.13 (1.10, 1.16) |
| Education | ||||
| High school or less | 20,899/425,082 | 1 (ref) | 1 (ref) | 1 (ref) |
| Greater than high school | 5791/112,449 | 1.05 (1.02, 1.08) | 0.95 (0.92, 0.98) | 1.02 (0.98, 1.05) |
| Military service characteristics | ||||
| Component | ||||
| Active duty | 15,265/315,391 | 1 (ref) | 1 (ref) | 1 (ref) |
| National Guard/reserve | 11,772/229,171 | 1.06 (1.03, 1.08) | 1.09 (1.07, 1.12) | 1.02 (1.00, 1.05) |
| Rank | ||||
| Enlisted | 25,256/501,990 | 1 (ref) | 1 (ref) | 1 (ref) |
| Officer | 1527/37,355 | 0.82 (0.78, 0.86) | 0.74 (0.70, 0.78) | 0.72 (0.68, 0.77) |
| Warrant | 254/5217 | 0.97 (0.86, 1.09) | 0.92 (0.81, 1.04) | 0.87 (0.77, 0.98) |
| Branch of service | ||||
| Army | 17,840/335,547 | 1 (ref) | 1 (ref) | 1 (ref) |
| Airforce | 3175/60,547 | 0.99 (0.95, 1.02) | 0.90 (0.87, 0.93) | 0.90 (0.87, 0.94) |
| Navy | 2953/70,546 | 0.80 (0.77, 0.83) | 0.73 (0.70, 0.76) | 0.74 (0.71, 0.77) |
| Marines | 3048/77,309 | 0.75 (0.72, 0.78) | 0.83 (0.80, 0.86) | 0.84 (0.81, 0.87) |
| Coast guard | 21/621 | 0.65 (0.43, 0.99) | 0.64 (0.42, 0.97) | 0.31 (0.12, 0.81) |
Model 1 unadjusted
Model 2 includes age, sex, and race/ethnicity
Model 3 includes age, sex, race/ethnicity, marital status, education and military characteristics
CMI chronic multisymptom illness
Fig. 1.
Veterans Health Administration outpatient care utilization by OEF/OIF/OND veterans after their last deployment end date, fiscal years 2002–2011. a CMI-related visits/veteran by setting and sex*†. b All outpatient visits/veteran by CMI-related diagnosis status and sex. a *CMI-related visits defined as VHA outpatient encounters associated with one or more ICD-9-CM code of chronic fatigue (780.71), fibromyalgia (729.1), or irritable bowel (564.1) syndrome. †Primary care visits defined by primary stop codes: primary care (342, 348, 350, and 323) and women’s primary care (322, 339, 404, 525, 704). Specialty care visits defined by primary stop codes: gastrointestinal (307, 321, 337); pain clinic (420); rheumatology/arthritis (314). All CMI-related encounters are counted in the numerator, including those occurring on the same day. Denominator includes veterans with ≥ 1 CMI-related ICD-9-CM code in the corresponding fiscal year. b Outpatient encounters counted as no more than one/day. Denominator includes all veterans with ≥ 1 VHA outpatient encounter during the corresponding fiscal year. CMI, chronic multisymptom illness; ICD-9-CM, International Classification of Diseases, 9th revision, Clinical Modification; OEF, Operation Enduring Freedom; OIF, Operation Iraqi Freedom; OND, Operation New Dawn; VHA, Veterans Health Administration.
DISCUSSION
Among 571,607 OEF/OIF/OND veterans who accessed VHA services from fiscal years 2002–2011, 4.7% veterans had CMI. Results from our cross-sectional study of demographic and military characteristics associated with CMI were generally consistent with prior research, including prospective studies, and extend these findings to one of the largest nationwide populations of OEF/OIF/OND veterans studied to date 2, 3. The finding that females have a higher prevalence of CMI is also supported by other studies 4, 5. A secondary analysis of yearly prevalence of CMI, stratified by gender, showed that the prevalence increased over the 10-year period (data not shown). The extent to which more frequent healthcare utilization by females versus males overall, as observed in our study, provides more opportunities for females to receive a CMI diagnosis needs additional investigation. The finding that VHA outpatient care utilization was nearly twice as high for OEF/OIF/OND veterans with versus without CMI underscores the significant burden related to CMI both to patients and the healthcare system. Further work is needed to understand the timing or incidence and severity of symptoms, patterns of healthcare utilization within and outside the VHA, and quality of care received by male and female OEF/OIF/OND veterans with CMI. Such work may help inform updated patient-centered evidence-based guidelines and identify opportunities to improve the care of deployed veterans with CMI, a phenomenon that is being noted with regularity after major military deployments.
Contributors
Resources and administrative support were provided by VA Salt Lake City Health Care System (IDEAS 2.0 Center). The authors would like to acknowledge our research team members and the Veterans Informatics and Computing Infrastructure (VINCI) team in Salt Lake City.
Funders
This work was supported by the U.S. Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Health Services Research and Development Project No. HIR 10-001 (PI: Samore). A.F.M. was supported by the VA Advanced Fellowship Program in Medical Informatics of the Office of Academic Affiliations, Department of Veterans Affairs, and a VA CDA 1 IK2 RX002324-01A1; and L.M.M. was supported by CDA-13-017. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the US government.
Compliance with Ethical Standards
Prior Presentation
Chronic Multisymptom Illness among Iraq/Afghanistan-Deployed Veterans and their Healthcare Utilization. Mohanty AF, McAndrew LM, Helmer D, Samore MH, Gundlapalli A. (Veterans Affairs 2017 HSR&D/QUERI National Annual Conference, Crystal City, VA, July 2017).
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- 1.McAndrew LM, Phillips LA, Helmer DA, Maestro K, Engel CC, Greenberg LM, et al. High healthcare utilization near the onset of medically unexplained symptoms. J Psychosom Res. 2017;98:98–105. doi: 10.1016/j.jpsychores.2017.05.001. [DOI] [PubMed] [Google Scholar]
- 2.Smith TC, Powell TM, Jacobson IG, Smith B, Hooper TI, Boyko EJ, et al. Chronic multisymptom illness: a comparison of Iraq and Afghanistan deployers with veterans of the 1991 Gulf War. American journal of epidemiology. 2014;180(12):1176–87. doi: 10.1093/aje/kwu240. [DOI] [PubMed] [Google Scholar]
- 3.VA/DoD Clinical Practice Guideline for the Management of Chronic Multisymptom Illness. Version 2.0 ed: Department of Veterans Affairs and the Departoment of Defense; 2014.
- 4.Vincent A, Lahr BD, Wolfe F, Clauw DJ, Whipple MO, Oh TH, et al. Prevalence of fibromyalgia: a population-based study in Olmsted County, Minnesota, utilizing the Rochester Epidemiology Project. Arthritis Care Res (Hoboken). 2013;65(5):786–92. doi: 10.1002/acr.21896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vincent A, Brimmer DJ, Whipple MO, Jones JF, Boneva R, Lahr BD, et al. Prevalence, incidence, and classification of chronic fatigue syndrome in Olmsted County, Minnesota, as estimated using the Rochester Epidemiology Project. Mayo Clin Proc. 2012;87(12):1145–52. doi: 10.1016/j.mayocp.2012.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mohanty AF, Muthukutty A, Carter ME, Palmer MN, Judd J, Helmer D, et al. Chronic multisymptom illness among female Veterans deployed to Iraq and Afghanistan. Med Care. 2015;53(4 Suppl 1):S143–8. doi: 10.1097/MLR.0000000000000314. [DOI] [PubMed] [Google Scholar]