Abstract
There is a pressing need for safe and highly effective Plasmodium falciparum (Pf) malaria vaccines. The circumsporozoite protein (CS), expressed on sporozoites and during early hepatic stages, is a leading target vaccine candidate, but clinical efficacy has been modest so far. Conversely, whole-sporozoite (WSp) vaccines have consistently shown high levels of sterilizing immunity and constitute a promising approach to effective immunization against malaria. Here, we describe a novel WSp malaria vaccine that employs transgenic sporozoites of rodent P. berghei (Pb) parasites as cross-species immunizing agents and as platforms for expression and delivery of PfCS (PbVac). We show that both wild-type Pb and PbVac sporozoites unabatedly infect and develop in human hepatocytes while unable to establish an infection in human red blood cells. In a rabbit model, similarly susceptible to Pb hepatic but not blood infection, we show that PbVac elicits cross-species cellular immune responses, as well as PfCS-specific antibodies that efficiently inhibit Pf sporozoite liver invasion in human hepatocytes and in mice with humanized livers. Thus, PbVac is safe and induces functional immune responses in preclinical studies, warranting clinical testing and development.
Malaria: Programming non-pathogenic parasites as vaccine candidates
A genetically engineered parasite, related to malaria-causing Plasmodium falciparum, excels as a vaccine in preclinical tests. A team led by Miguel Prudêncio, of the University of Lisbon, Portugal, developed a genetically altered vaccine candidate based on Plasmodium berghei, which is pathogenic to rodents but, in humans, fails to progress from a harmless, transient liver infection to causing full, blood-borne malaria. The candidate expresses a human form of ‘circumsporozoite protein,’ a known antigen, and is designed to provoke a more comprehensive immune response as it presents a whole pathogen to the host. In preclinical tests, the candidate generated antibodies able to neutralize infection in human hepatocytes and also provoked a cellular immune response in rabbits. The team’s candidate proved safe and efficacious, warranting further trials and clinical testing.
Introduction
The long-standing goal of an effective vaccine against malaria constitutes a crucial component of efforts to prevent a disease that continues to kill nearly half a million people per year.1 During a natural malaria infection, Plasmodium sporozoites are injected into the skin and skin vasculature by an infected mosquito and travel to the liver of their vertebrate host. An asymptomatic parasite maturation and replication phase inside hepatocytes ensues, leading to the generation of Plasmodium exoerythrocytic forms (EEFs) and preceding the release of erythrocyte-infectious merozoites, which can establish a blood infection and lead to disease symptoms [reviewed in2].
So far, vaccines against the early pre-erythrocytic stages of Plasmodium parasites have shown most success among current vaccine candidates,3 including the most advanced subunit vaccine against the human malaria parasite P. falciparum (Pf), RTS,S, that targets the circumsporozoite (CS) protein,4 the predominant antigen on the surface of sporozoites and a major vaccine candidate. While the ability of CS-based vaccination to partially limit clinical malaria infection in the field is a major achievement, the modest and rapidly waning efficacy of RTS,S stresses the urgency to develop vaccines with higher and more durable protection.5 An alternative to subunit vaccines is the use of whole-sporozoite (WSp) approaches, based on the generation of immunity against Plasmodium pre-erythrocytic stages following immunisation with infective sporozoites under conditions that prevent the appearance of clinical symptoms, including radiation-attenuated sporozoites (RAS),6–8 genetically attenuated parasites (GAP),9–13 and immunisation with non-attenuated sporozoites in combination with chemoprophylaxis (CPS).14–16 Although CS has been proposed to play an important protective role in WSp vaccines, complete protection following P. yoelii RAS immunization has been shown to occur in transgenic mice that are T-cell tolerant to CS and cannot produce antibodies.17 Therefore, protection induced by WSp is likely mediated by a plethora of hitherto unidentified liver stage antigens presented to the immune system during liver stage parasite development (reviewed in18). Accordingly, later liver stage-arresting parasites, such as some GAP parasites, and those completing liver stage development, such as the CPS approach, seem to trigger antimalarial immunity superior to that elicited by early-arresting variants.11,19 Nonetheless, the most advanced WSp approach to human vaccination relies on the intravenous administration of the PfSPZ Vaccine, composed of aseptic, purified, cryopreserved PfRAS.20–23 While all current WSp human vaccination strategies rely on the use of Pf sporozoites, alternative WSp vaccines can also be envisaged. In this context, a rodent Plasmodium-based immunization platform constitutes an inherently safe and hitherto unexplored approach to WSp vaccination that is worth investigating.
The paradigm of immunizing with non-pathogenic microorganisms to protect against the disease caused by their human-infective counterparts was pioneered by Edward Jenner using a bovine poxvirus to prevent smallpox. This concept of vaccination has since been employed for various other human diseases, through the development of the bovine bacillus Calmette–Guérin (BCG) vaccine against human TB or the selection of rhesus and bovine rotavirus strains to create human rotavirus vaccines (reviewed in24). Vaccine development has also benefitted from advances in genetic manipulation, which have allowed for isolation, modification, and optimization of vaccine antigen delivery and facilitated smart vaccine design. The first genetically modified (GM) human vaccine, against hepatitis B, was approved in 1986,25 followed by vaccines targeting influenza26 and Japanese encephalitis.27 However, the combination of cross-species immunity and genetic modification has never been applied to the field of malaria vaccination.
We propose to use GM rodent Plasmodium sporozoites expressing human Plasmodium antigens as a safe “naturally attenuated” WSp vaccination platform that can elicit cross-species immune responses against Pf as well as deliver specific immunogens, such as PfCS, and that may protect against a subsequent infection by human malaria parasites. Rodent P. berghei (Pb) parasites efficiently infect human hepatocytes in vivo, a requirement for optimal antigen presentation, while remaining unable to cause a blood-stage infection, in agreement with the widely accepted notion that they are non-pathogenic to humans. We establish the proof-of-principle of this vaccination approach by demonstrating that immunisation of rabbits with transgenic Pb sporozoites expressing PfCS (PbVac) induces robust immunity against Pf, including cross-species cellular immune responses, as well as PfCS-dependent humoral responses that functionally block Pf infection of liver-humanized mice. These results identify a new Pb-based WSp immunizing agent and antigen delivery platform for malaria vaccination and pave the way for the design of rodent parasites that can induce optimal protective immune responses against human malaria.
Results
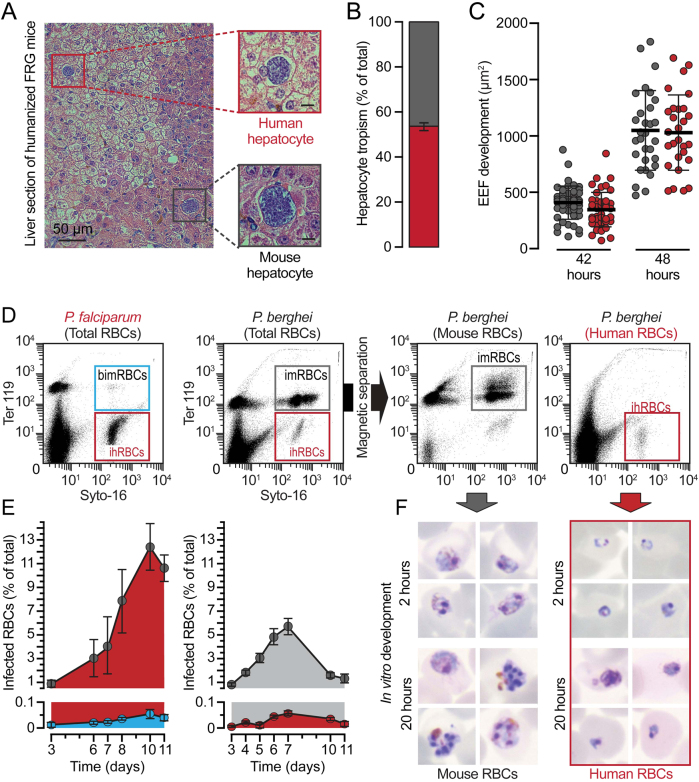
P. berghei can infect human hepatocytes but is unable to develop in human erythrocytes
It is well known that the sporozoite stage of Pb is able to infect hepatic cells from different hosts, including several human-derived and mouse-derived hepatoma cell lines and human primary hepatocytes (PH) cultured ex vivo [reviewed in28]. We confirmed and extended these findings by monitoring in parallel the in vitro infection of one mouse and two human hepatoma cell lines (Hepa 1-6, HepG2, and Huh7, respectively), and one human immortalized hepatocyte line (HC-04), as well as the ex vivo infection of human PH/fibroblast co-cultures by Pb. Infection assessed by immunofluorescence microscopy showed that sporozoites invade and develop to similar extents in all in vitro systems studied (Fig. S1A-C) and that these parasites are able to invade and develop inside human PH ex vivo (Fig. S1D-F). We further ascertained Pb infectivity of human hepatocytes in vivo, in liver-humanized FRG mice. Our results show that Pb can effectively infect human hepatocytes engrafted in liver-humanized FRG mice (Fig. 1a and Fig. S1G, H), displaying similar tropism to mouse and human hepatocytes (Fig. 1b), and similar development inside either type of cell (Fig. 1c and Fig. S1H).
Fig. 1.
Rodent P. berghei parasites successfully develop within human hepatocytes but not within human RBCs. a Representative images of developing rodent PbWT parasites in mouse (black square) and human (red square) hepatic cells of liver-humanized FRG mice 48 h post infection (hpi) by iv injection of freshly isolated sporozoites. b Relative proportion of Pb-infected mouse (grey) and human (red) hepatocytes in humanized FRG mice, normalized to the total humanization of the chimeric liver. c PbWT development in mouse (grey) and human (red) hepatocytes 42 and 48 hpi of liver-humanized FRG mice. d Representative flow cytometry plots of peripheral blood from blood-humanized NSG mice infected by iv injection of Pf-infected (left) or Pb-infected RBCs (middle-left) before and after magnetic separation (middle-right and right); Syto-16 for nucleic acids; TER-119 for murine erythroid lineage; imRBCs/ihRBCs: infected mouse or human RBCs; bimRBCs: background signal for infected murine erythroid lineage. e Relative proportion of mouse and human RBCs infected with Pf (left) or Pb (right) parasites; bars indicate standard error. f Representative pictures of Pb parasite forms observed within magnetically separated imRBCs and ihRBCs from the total blood of infected blood-humanized NSG mice after 2 and 20 h of in vitro culture
We subsequently assessed Pb infectivity of human red blood cells (RBC) employing blood-humanized mice, engrafted with defined proportions of human RBC,29 infected by transfusion of infected RBC. Coupled use of nuclear SYTO-16 and mouse erythroid line-specific TER-119 dyes allowed the distinction between infected and non-infected cells and between human and rodent RBC, respectively, and thereby enabling monitoring of infection by flow cytometry (Fig. 1d). Our results show that while the SYTO-16+/TER-119+ population, indicative of infection of the mouse RBC population, increased steadily, the SYTO-16+/TER-119− population, corresponding to infected human RBC, remained below 0.1%, similar to the background signal observed for mouse RBCs in Pf-infected blood-humanized mice (Fig. 1d and e). Fluorescence microscopy analysis of these samples revealed very few SYTO-16+/TER-119− cells indicating the rare occurrence of invasion of human RBCs by Pb (data not shown). We could not find any human RBC bearing a parasite with more than a single nucleus, suggesting that the parasite degenerates into unviable cryptic forms. To ascertain this, infected human and mouse RBC were isolated by TER-119-based magnetic activated cell sorting and the isolated cells were cultured in vitro for up to 20 h. Our in vitro results show that while parasites in infected mouse RBC were able to develop as expected, parasites in the infected human RBC population remained single-nucleated and unable to multiply (Fig. 1f). Similar results were obtained when infection of blood-humanized mice was initiated by sporozoite injection (data not shown). Overall, these results clearly show that Pb is capable of infecting human hepatocytes whereas it is unable to develop inside human RBC.
The PbVac vaccination platform
In order to assess the potential of Pb to elicit cross-species immune responses against Pf, a comprehensive, in silico prediction of CD8+ T cell epitopes in the proteomes of Pf and Pb was carried out. Our results show that 24171 in silico-predicted epitopes are shared between species. These are encoded in 61% (3371/5548) of the Pf proteins and 66% (3332/5059) Pb proteins, of which 3223 are orthologous pairs in the two species. This includes several antigens expressed during pre-erythrocytic stages (e.g., SLARP, SIAP1, LISP1, and MB2), and substantiates the potential for cross-protection between the two species (Fig. S2, Tables S1, S2). Notably absent from the set of Pf proteins containing shared epitopes with Pb is CS.
Given the established value of PfCS as a leading vaccine candidate antigen, we generated a transgenic Pb line, PbVac, that expresses PfCS, using ‘gene insertion/marker out’ (GIMO) methods of transfection.30 The gene encoding PfCS was inserted into the neutral 230p locus of the Pb genome under the control of the 5′- and 3′ regulatory sequences of Pb’s upregulated in infective sporozoites 4 (uis4) gene (Fig. S3A), which is expressed exclusively in sporozoites and developing liver stages.31 The GIMO transfection method employed ensures the stable insertion of the gene encoding the heterologous PfCS and flanking regions in the Pb genome, resulting in a drug-selectable marker-free transgenic parasite.30 Genotyping of PbVac showed correct integration of the PfCS expression cassette (Fig. S3B and C).
We next sought to assess the impact of genetic manipulation on the overall fitness of PbVac. To this end, we started by evaluating PbVac’s sporogonic development and showed that it was indistinguishable from that of the parental wild-type Pb (PbWT), contrary to what was observed in previous attempts at expressing PfCS as a replacement of the endogenous PbCS gene.32 The two parasite lines formed similar numbers of oocysts in the mosquito host’s midgut (Fig. S4A), as well as of sporozoites in oocysts (Fig. S4B), in the hemolymph (Fig. S4C), and in salivary glands (Fig. S4D). We then analyzed the expression of the endogenous PbCS and heterologous PfCS proteins, in PbVac and PbWT parasites. Immunofluorescence microscopy analysis clearly shows that only PbCS is expressed and shed by PbWT sporozoites (data not shown), while the PbVac sporozoites express and shed both the PbCS and the PfCS proteins during gliding (Fig. 2a). Our results further show that both proteins are expressed by developing PbVac parasites during hepatic development and are present at the parasite membrane both in in vivo (Fig. 2b) and ex vivo (Fig. S4E and F). We then compared the hepatic infectivity of PbVac and PbWT sporozoites in mice. Immunofluorescence microscopy analysis of ex vivo-infected mouse PH revealed that both parasites yield equivalent numbers of EEFs (Fig. S4G), which have comparable development (Fig. S4H). Subsequent qRT-PCR and immunofluorescence microscopy analyses of infected mouse livers further confirmed that PbVac and PbWT sporozoites lead to similar total hepatic parasite loads (Fig. S4I), with identical numbers of EEFs formed (Fig. S4J) and similar in vivo development (Fig. S4K). Additionally, we showed that, like PbWT, the PbVac parasites readily infect human hepatocytes in liver-humanized FRG mice (Fig. S5A and B) but, unlike Pf parasites, are unable to multiply in human RBC, degenerating into unviable cryptic forms (Fig. S5C and D). Finally, we compared the infectivity of PbVac and Pf sporozoites to freshly isolated human PH ex vivo. Our data showed that the number of resulting EEFs in human PH, as determined by microscopy 48 h after sporozoite addition, can be up to 50-fold higher for PbVac than for Pf (Fig. 2c). Collectively, we show that PbVac parasites display similar fitness to PbWT and that the engineered PfCS protein is correctly expressed, localizing to the surface of PbVac sporozoites. Our results further show that PbVac parasites are unable to develop inside human erythrocytes and, most importantly, are able to infect human hepatocytes with even greater efficiency than Pf.
Fig. 2.
PfCS expression and human hepatic infectivity of PbVac pre-erythrocytic stages. a, b Representative Immunofluorescence microscopy images of PbCS (grey) and PfCS (purple) expressed by PbVac sporozoites a and exoerythrocytic forms in the livers of mice infected by iv injection of freshly isolated sporozoites b. c Comparative infection rates of PbVac and Pf parasites in ex vivo cultures of human hepatocytes assessed by immunofluorescence microscopy. The shading of dots indicates distinct biological replicates obtained employing human hepatocytes from different donors. The boxes correspond to the 25th and 75th percentiles; the lines and bars indicate mean of infection and standard error of the mean, respectively; ***p < 0.001, as determined by Mann–Whitney U test. Scale bars: 10 µm
An innovative animal model for evaluation of PbVac immunogenicity
Having constructed and characterized the PbVac vaccine candidate, we then sought to assess its ability to elicit immune responses against human-infective Pf parasites. Rodents do not constitute an appropriate animal model in that respect, as they are susceptible to blood-stage infection by PbVac. To overcome this limitation, we evaluated New Zealand White (NZW) rabbits as an alternative model that mimics Pb’s pattern of infectivity in humans. To this end, we started by infecting NZW rabbit PH with Pb sporozoites and assessed infection at different time points after sporozoite addition by immunofluorescence microscopy. The results show that Pb effectively invades and develops inside rabbit PH (Fig. 3a and Fig. S6A) and is capable of completing its hepatic developmental process and forming infectious merozoites ex vivo (Fig. 3b and Fig. S6B). To ascertain Pb’s ability to infect rabbit hepatocytes in vivo, NZW rabbits were exposed to infected mosquito bites or increasing numbers of Pb sporozoites injected intravenously. qRT-PCR and detailed immunofluorescence microscopy analyses of rabbit livers showed that Pb readily infects rabbit hepatocytes in an in vivo context (Fig. 3c) developing for a longer period than the 58–62 h of development observed in highly susceptible hosts such as BALB/c or C57BL/6 mice. Our results further indicate that larger EEFs disappear from the rabbit livers earlier than less developed parasites, which can be observed up to 96 h after infection (Fig. 3d and Fig. S6C and D), therefore appearing to persist longer than irradiated parasites do in the liver of susceptible hosts (data not shown). Finally, to investigate rabbit RBC infectivity by Pb, NZW rabbits were infected with luciferase-expressing Pb sporozoites and blood samples were collected daily and analyzed by Giemsa staining and luminescence. As controls, mice were infected with similar numbers of Pb sporozoites and blood samples were collected at the same time points. Our results show that whereas parasitemia increased steadily in the blood of infected mice, no parasites were detected in the NZW rabbit blood up to 7 days after parasite administration (Fig. 3e). To fully establish the inability of Pb to infect NZW rabbit RBC, rabbits and mice were also infected by blood transfusion with 1 × 108 Pb-infected mouse erythrocytes. Again, while parasitemia developed as expected in the blood of infected mice, no parasites were detected in rabbit blood (Fig. S6E) even following prolonged treatment with phenylhydrazine to increase reticulocytemia (Fig. S6F).
Fig. 3.
Infection of NZW rabbit hepatocytes with P. berghei sporozoites. a Rodent Pb parasite development 24 and 48 hpi in ex vivo cultures of rabbit primary hepatocytes. b Representative immunofluorescence microscopy image of a Pb merosomes developing ex vivo within rabbit primary hepatocytes 60 hpi and presenting typical markers of late exoerythrocytic development. c qRT-PCR quantification of hepatic infection of rabbits following iv injection of increasing amounts of freshly isolated Pb sporozoites (1 × 105, 5 × 105, and 1 × 106). d Representative immunofluorescence microscopy images of rodent Pb parasites developing in the livers of NZW rabbits at different hpi. e Parasitemia in the peripheral blood of rabbits (orange) or mice (grey) following iv injection of freshly isolated Pb sporozoites. Scale bars: 10 µm
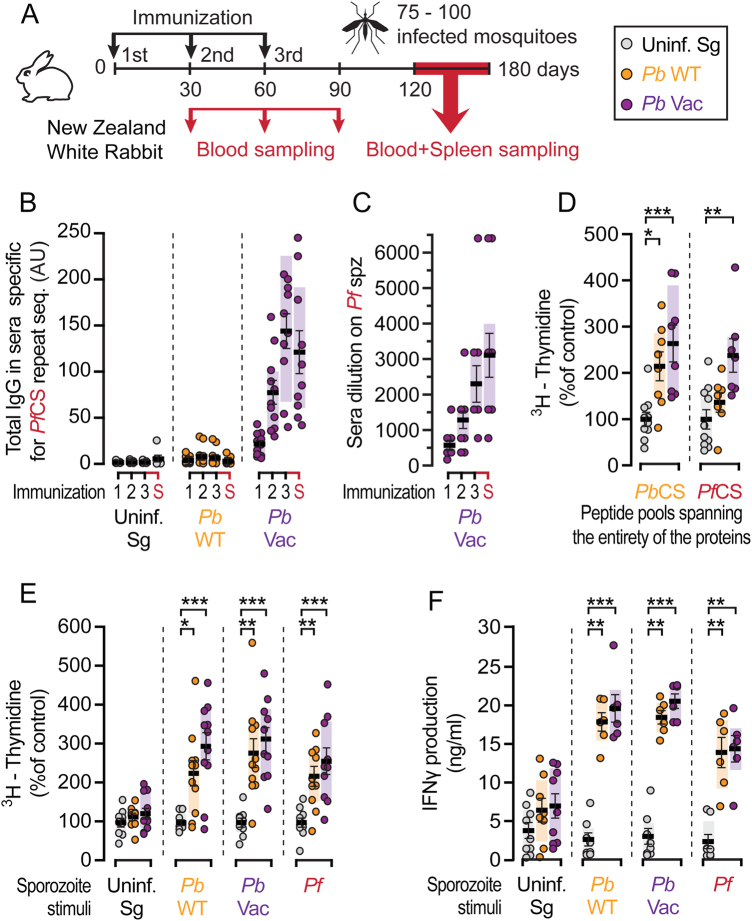
Immune responses elicited by immunization with PbVac parasites
Having shown that they constitute a model of Pb hepatic infection that can be employed in immunization studies with Pb-based sporozoite vaccines, NZW rabbits were immunized by repeated mosquito bite delivery of PbWT or PbVac sporozoites for immune response assessment. In parallel, non-infected mosquitoes were allowed to feed on mock-immunized controls. Blood samples were collected at the time of the 2nd and 3rd immunizations, as well as one month after the 3rd and last immunization. Two to four months after the last of three immunizations, rabbit blood and splenocytes samples were collected for processing and subsequent analysis (Fig. 4a). We started by quantifying total IgGs in the serum of immunized animals by ELISA, employing peptides spanning the PfCS repeat region. Anti-PfCS antibody titers in the serum of PbVac-immunized animals steadily increased after each of the three immunizations, confirming “vaccine take” in these animals and successful delivery of the heterologous PfCS antigen by PbVac (Fig. 4b). Anti-PbCS antibody titers measured as controls in these experiments were also found to increase after each immunization with either PbWT or PbVac, whereas neither anti-Pf CS nor anti-PbCS antibodies were detected in mock-immunized animals (Fig. S7A). Having shown that PfCS transgene presentation upon immunization with PbVac leads to a strong humoral response, we then investigated the responses elicited against whole Pf sporozoites. Indirect fluorescence antibody test (IFAT) analyses of immune sera collected at various time points revealed the presence of increasing amounts of antibodies that recognize and bind to immobilized Pf sporozoites in the serum of PbVac-immunized (Fig. 4c), but not in that of mock-immunized or PbWT-immunized (Fig. S7B), rabbits. We then asked whether a CS-specific cellular immune response was also induced by immunization. To this end, rabbit splenic lymphocyte proliferation was assessed by a 3H-thymidine incorporation assay following stimulation with peptide pools spanning the entire amino acid sequence of either the PbCS or the PfCS proteins. A marked proliferation of lymphocytes of PbWT-immunized rabbits was only observed in response to a PbCS stimulus, whereas those of PbVac-immunized animals significantly proliferated upon stimulation with either PbCS or PfCS (Fig. 4d and Fig. S8). Of note, proliferation was not observed when the cells were stimulated with peptides spanning only the conserved repeat regions of the PbCS or PfCS proteins (Fig. S8). Concomitantly, proliferation of lymphocytes from immunized animals was assessed upon stimulation with uninfected salivary gland material, PbWT, PbVac and Pf sporozoites. Our data showed that lymphocytes from either PbWT-immunized or PbVac-immunized rabbits significantly responded to both PbWT and PbVac sporozoite stimuli, whereas stimulation with non-infected salivary gland material induced only basal levels of thymidine incorporation (Fig. 4e and Fig. S8). As expected, stimulations with sporozoites consistently induced more marked lymphocyte proliferation than peptide-based stimulation. Lymphocytes from either group of immunized animals also incorporated significantly more 3H-thymidine than those of mock-immunized animals in response to a stimulus with Pf sporozoites, indicating not only that immunization with PbVac elicits a strong cellular response against Pf but also that this response occurs likewise upon immunization with PbWT (Fig. 4e). These results are in complete agreement with our flow cytometry investigation of cell proliferation in the presence of the different sporozoite stimuli (Fig. S9 A-C). Furthermore, our results show that the cellular immune responses observed in PbWT-immunized and PbVac-immunized animals upon sporozoite stimulation contained a major CD4+ T cell component (Fig. S9C). Finally, augmented lymphocyte proliferation capacity is concomitant with increased IFNɣ production, as our results show that the amount of IFNɣ produced upon stimulation of cells from sporozoite-immunized animals, but not from mock-immunized animals, with any of the sporozoite stimuli employed, was significantly enhanced compared to that of cells stimulated with non-infected salivary gland material (Fig. 4f). Overall, these data indicate not only the existence of cross-species cellular responses between Pb and Pf but also that the PfCS protein engineered on the Pb background contributes to the cellular, and mediates the humoral, immune responses observed upon immunization with the PbVac parasite.
Fig. 4.
Immune responses in NZW rabbits after PbVac sporozoite immunization. a Diagram of the immunization protocol. Immunizations were performed by exposure to the bites of 75-100 mosquitoes. b Total IgG titers against PfCS repeat sequence in serum after 1, 2, and 3 mock immunizations (grey), or immunization with PbWT (orange) and PbVac (purple), or at the time of animal sacrifice (S) 60–90 days after last immunization. c Serum binding capacity to Pf sporozoites after PbVac immunization. d Spleen cell proliferation upon stimulation with peptide pools spanning the entire PbCS or PfCS proteins in immunized rabbits, as indicated by assessment of 3H-thymidine incorporation. e Spleen cell proliferation upon stimulation with PbWT, PbVac or Pf sporozoites, as indicated by assessment of 3H-thymidine incorporation. Stimulation with an extract of uninfected mosquito salivary gland material was used as control. f IFNy production in rabbit spleen cell supernatant after stimulation with PbWT, PbVac or Pf sporozoites. Measurements were taken from distinct samples. The boxes correspond to the 25th and 75th percentiles; the line and bars indicate mean of infection and standard error of the mean, respectively; *p < 0.05; **p < 0.01; ***p < 0.001, as determined by Kruskal–Wallis test, corrected with Dunn’s multiple comparisons test
Functional capacity of PbVac-induced humoral immune responses
We next evaluated the ability of the observed immune responses to inhibit infection by Pf. Since the protective capacity of the cellular immune responses cannot be directly assessed because the rabbit model employed is not susceptible to Pf infection, we focused our analysis on the functionality of the humoral immune responses elicited upon immunization. To this end, we performed both in vitro inhibition assays and in vivo Pf challenge assays of liver-humanized FRG mice employing IgGs isolated from the serum of mock-, PbWT-immunized and PbVac-immunized rabbits (Fig. 5a). Incubation of sporozoites with ~0.2 mg/ml post PbVac-immunization IgGs led to a ~40% decrease in Pf infection of HC04 cells compared with IgGs from mock-immunized animals (Fig. 5b). This effect is more pronounced than the impairment observed on Pf sporozoite traversal following incubation with 10 mg/ml total IgGs from CPS-immunized volunteers.33 Finally, 10 mg total IgGs purified from the serum of mock-, PbWT-immunized and PbVac-immunized rabbits were injected into liver-humanized FRG mice. Twenty-four hours after IgG passive transfer, these mice were challenged by an equal number of Pf-infected mosquito bites. The Pf load in the chimeric livers of humanized FRG mice was assessed five days later by qRT-PCR. The results show that passive transfer of 10 mg IgGs from PbVac-immunized rabbits, but not from PbWT-immunized or mock-immunized animals, conveyed near complete protection against a subsequent Pf hepatic infection (Fig. 5c). This decrease in liver parasite load is more marked than that observed under similar experimental conditions following passive transfer of 10 mg of IgGs from CPS-immunized volunteers, which is equivalent to the typical IgG concentration in human plasma.33 Collectively, these data show that immunization with PbVac elicits the production of high titers of functional antibodies, mostly targeting the PfCS antigen, capable of preventing a subsequent infection by human-infective parasites.
Fig. 5.

PbVac-mediated protection against Pf challenge. a Diagram of the experimental protocol. b Pf sporozoite infection of HC-04 human immortalized hepatocyte cultures incubated with purified IgG from mock- (grey), PbWT- (yellow) or PbVac (purple)-immunized rabbits. c qRT-PCR quantification of Pf hepatic infection inhibition in liver-humanized FRG mice following passive transfer of purified IgGs from mock (grey)-, PbWT (orange)- or PbVac (purple)-immunized rabbits and challenge by the bites of 20 Pf-infected mosquitoes (n = 3 mice per group). Measurements were taken from distinct samples. The boxes correspond to the 25th and 75th percentiles in B), and the minimum and maximum data range in C); the lines and bars indicate mean of infection and standard error of the mean, respectively; *p < 0.05; **p < 0.01, as determined by one-way ANOVA, corrected with Dunnett’s multiple comparisons test
Discussion
Despite being known for more than 100 years that attenuated pathogens can induce protective immunity,24 the present study introduces for the first time a practical approach to developing a human vaccine based on the concept of employing an avirulent non-human Plasmodium parasite as a versatile platform of WSp-based antigen delivery for vaccination against human malaria. Although transgenic rodent malaria parasites where endogenous antigens were replaced by those of their human-infective counterparts have previously been described, they served exclusively as tools for assessment of functional immunogenicity of malaria vaccines rather than as antigen delivery platforms.32,34,35 We now propose to use Pb as a safe, genetically modifiable vaccination platform that can be engineered to express multiple antigens of human malaria parasites capable of inducing functional immune responses against different Plasmodium species or various stages of the parasite’s life cycle.
We generated a new transgenic Pb parasite, PbVac, capable of expressing and delivering the Pf immunodominant protective antigen, PfCS.17,36 In a pre-clinical proof-of-principle study, we show that immunisation with PbVac is effective against Pf through a combination of cellular immune responses and antibody-based responses. Consistent with the distribution of in silico-predicted epitopes shared between the Pf and Pb proteomes, the induction of T cell-mediated immunity by PbVac appears to be largely PfCS-independent and arise from the vaccine’s Pb background. This is in agreement with a recent study, in which peripheral blood T cell responses to CS peptides were not detected following CPS immunization of rhesus monkeys with P. knowlesi,37 as well as with previous literature on cross-species immune responses in WSp vaccination. In fact, the first report of pre-erythrocytic cross-species protection between Plasmodium species dates back to 1969, when mice immunized by injection of X-irradiated Pb sporozoites were shown to be protected against a challenge with viable sporozoites of P. vinckei.38 Protection was also observed when Pb-immunized animals were challenged with rodent P. chabaudi sporozoites and vice versa.39 In other studies, mice immunized by irradiated or genetically attenuated (p36p−) Pb sporozoites were shown to provide partial protection against challenge by P. yoelii (Py) sporozoites,40 and 100% sterilizing cross-species protection was observed when mice were immunized with a late liver stage-arresting genetically attenuated Py parasite (Py-abb/f) and challenged with Pb sporozoites.11 Sedegah et al.41 reported T cell-mediated protection of mice immunized with attenuated Pb or Py sporozoites against heterologous challenge with Py or Pb, respectively. The requirement for T cells to provide protection against heterologous parasites was consistent with the previous observation that a PyCS CD8+ T cell clone was protective against challenge with the heterologous Pb sporozoites.42 Most relevant in the context of the present study, immunization of mice with Pf sporozoites protected the animals from infection with Pb.43 Protection was proposed to be mediated, at least in part, by antibody cross-reaction between antigens other than PfCS and PbCS, in agreement with the high genetic sequence similarity between the two parasite species.44 However, it should be noted that several examples of cross-species protective immune responses induced by parasite components other than CS following immunization with irradiated Plasmodium sporozoites are available in the literature.45,46 Such protective antigens may include, for instance, cell-traversal protein for ookinetes and sporozoites (CelTOS),47 a protein that is highly conserved among the Plasmodium species. Indeed, immunization of mice with PfCelTOS has been shown to elicit cross-species protection against a heterologous challenge with Pb.48 In humans, CS-specific cellular immune responses were described in RAS-immunized volunteers as determined by the proliferation of peripheral blood mononuclear cells (PBMCs) upon in vitro stimulation with recombinant Pf CS.49,50 Nevertheless, the reports of human immunization with Pf sporozoites available so far do not show a correlation between long-term protection afforded by WSp vaccines and CS-targeted cellular immune responses, and correlations identified between long-term protection and CS-targeted antibody responses20,21 have been interpreted as biomarkers of vaccine take rather than mechanistic correlates. Thus, it is thought that long-term protection induced by WSp is complex and likely mediated by multiple liver stage antigens, whose identification has been a matter of previous research.47,51
Although protection by WSp immunisation may result from the combined activities of induced T cells and antibodies against a variety of antigens [reviewed in18], the presentation of a key Pf antigen by the Pb vaccination platform may provide an additional means of inducing targeted and effective immune responses. Accordingly, our results show that immunization with PbVac elicits a potent PfCS antibody response, capable of functionally inhibiting infection of hepatocytes by Pf sporozoites. Humoral responses induced by immunization with PbWT lack inhibitory activity against Pf sporozoites, indicating a pivotal role of the PfCS protein in the antibody-based protection conferred by vaccination with PbVac. Unlike subunit approaches, a major advantage of the expression of Pf antigens in Pb is that the latter is more likely to generate full length Pf proteins that are correctly folded and post-translationally modified, inducing a greater array of inhibitory antibody responses against Pf sporozoites. Our findings are in agreement with the fact that RAS immunization of human volunteers leads to the production of high titers of antibodies against the CS protein,49,52 which parallel the serum inhibitory activity of sporozoite invasion of hepatoma cells in vitro.52 Moreover, antibodies against the immunodominant B-cell epitope of PfCS were also shown to inhibit sporozoite infection in vitro53,54 and in vivo.55 Our results further indicate that the PfCS component of the PbVac parasite may induce not only humoral responses but also contribute to the overall cellular responses observed after immunisation. In fact, CS-specific cellular immune responses have been described in RAS-immunized volunteers as determined by the proliferation of peripheral blood mononuclear cells upon in vitro stimulation with recombinant PfCS.49,50 Additionally, an epitope mapping to the 5′ repeat region of PfCS was identified in T cell lines and clones obtained from a sporozoite-immunized human volunteer,56 and another PfCS epitope was shown to be recognized by human cytolytic class II-restricted CD4+ T cells.57
It is clear that WSp immunization offers several benefits over subunit vaccines, including the presentation of a wider range of antigens, correctly folded and optimally delivered to their target location. However, the success of Pf-based WSp vaccination depends on the strict absence of breakthrough episodes, a concern that is eliminated by Pb-based WSp antigen delivery systems. Since Pb develops into maturing liver schizonts in human hepatocytes, immunisation with Pb WSp vaccines is likely to result in increased antigen exposure relative to early-arresting Pf-based variants such as RAS or early-arresting GAP. We further observed that PbVac sporozoites are 20–50 times more infectious than Pf, likely increasing the effective dose of vaccination, and potentially inducing robust immune responses with relatively few immunizing parasites. Moreover, Pb is highly amenable to genetic manipulation, and several neutral loci have already been identified in its genome. This raises the possibility of introducing multiple antigens in the Pb platform, including those from different human-infective Plasmodium spp., as well as blood-stage or transmission-blocking antigens, placed under the control of a strict pre-erythrocytic stage promoter.
The manufacturing of a PbVac vaccine suitable for future human use can be envisaged to employ parenteral injection of sporozoites obtained from mosquitoes that fed on PbVac-infected, specific-pathogen free (SPF) rodents, previously infected with a master cell bank of PbVac parasites that is fully certified as free of human pathogens or other microbiological contaminants. A single SPF rat can be used to infect more than one thousand mosquitoes, potentially generating hundreds of vaccine doses. Importantly, the production of a Pb-based vaccine can be achieved in the absence of high-containment mosquito infection and handling facilities or, possibly, in vitro, as suggested by previous proof-of-principle studies.58,59
The data presented here employing the PbVac parasite provides the proof-of-concept that immunisation with GM rodent malaria parasites can potentially be used to protect against human malaria. Given the limitations of available animal models to predict the protective efficacy of such a vaccination approach, this can only be fully ascertained in clinical trials performed upon addressing all relevant safety and regulatory issues.
Materials and methods
Animal experimental procedures
Male C57BL/6 and Balb/cByJ mice, aged six to eight weeks, as well as NZW rabbits, aged four to six weeks, were purchased from Charles River and housed in the animal facilities of Instituto de Medicina Molecular, Faculdade de Medicina, Universidade de Lisboa, Portugal (iMM Lisboa). Experimental procedures were performed according to the Federation of European Laboratory Animal Science Associations (FELASA) guidelines and iMM Lisboa regulations. Blood-humanized NSG mice were produced and housed at the AAALAC-accredited GlaxoSmithKline Laboratory Animal Science facility in Tres Cantos (Madrid, Spain). All the experiments were approved by the GlaxoSmithKline Diseases of the Developing World Group Ethical Committee and complied with Spanish and European Union legislation on animal research and GlaxoSmithKline policy on the care and use of animals. Liver humanized FRG mice were produced by Yecuris (Tualatin, Oregon USA), and housed in the animal facilities of the Faculty of Medicine and Health Sciences of the Ghent University or at iMM Lisboa. The experimental protocol for Pf or Pb infection of these mice was approved by the animal ethics committees of the Faculty of Medicine and Health Sciences of the Ghent University and of iMM Lisboa (DGV-AWB-2015-09-MP-Malaria). All facilities were kept under a 12 h light/dark period at a temperature of 22 ± 2 °C and 40–70% relative humidity. Filtered tap water and a γ-irradiated pelleted diet were provided ad libitum. In experiments involving blood-stage infections, animals were euthanized at the first behavioral signs of onset of experimental cerebral malaria (ECM), and this was considered the experimental endpoint, with all efforts made to minimize animal suffering.
P. berghei and P. falciparum reference parasite lines
The following reference lines of the ANKA strain of Pb were used: line cl15cy1, line 676m1cl1 (PbGFP-Luccon; see RMgm-29 in www.Pberghei.eu) and line 1596cl1 (GIMOPbANKA mother line; see RMgm-687 in in www.Pberghei.eu). PbGFP-Luccon expresses a fusion protein of GFP and luciferase from the eef1a promoter60 and the GIMO-mutant contains the hdhfr::yfcu positive–negative selection marker in the silent 230p locus.30 For Pf experiments, Pf NF54 asexual and sexual blood stages were cultured in a semi-automated culture system. Sporozoites were obtained by dissection of salivary glands from infected female Anopheles stephensi mosquitoes, reared at iMM-Lisboa or at the Radboud University (Nijmegen, Netherlands), and which had previously fed on gametocyte-carrying infected mice for Pb infections or cultured gametocytes through standard membrane feeding for Pf infections. Mosquito salivary glands were kept on ice in D-MEM culture medium and homogenized with a grinder to release the sporozoites, which were subsequently counted on a Neubauer chamber.
Generation and genotyping of transgenic P. berghei parasite, PbVac
A transgenic Pb parasite line containing a Pfcs expression cassette in the neutral 230p locus was generated using the ‘gene insertion/marker out’ (GIMO) technology as previously described.30,61 The Pfcs expression cassette was introduced into the neutral 230p locus of the GIMO mother line 1596cl1,30,61 using construct pL1988 (Fig. S3A). The pL1988 construct contains the Pfcs coding sequence (CDS) under the control of the Pbuis4 5′ and 3′ UTR regulatory sequences flanked by the 5′ and 3′ targeting sequences for the 230p locus. This construct integrates by double crossover homologous recombination and replaces the positive–negative selectable marker (SM) (human dihydrofolate reductase:: yeast cytosine deaminase and uridyl phosphoribosyl transferase (hdhfr::yfcu)) cassette in the GIMO mother line 1596cl1 with the Pfcs expression cassette. The expression cassette contains the Pfcs CDS, which was amplified by PCR from Pf NF54 genomic DNA.62 The CDS is flanked by the 5′ and 3′ promoter and transcription terminator sequences of Pb UIS4, which were amplified from Pb ANKA WT genomic DNA. The coding sequence of the Pfcs gene was confirmed by sequencing. The construct pL1988 was linearized by digestion with by SacII before introduction into parasites of the GIMO mother line 1596cl1 using standard methods of GIMO transfection.30 Transfected parasites were selected in mice by applying negative selection by providing 5-fluorocytosine (5-FC) in the drinking water of mice. Negative selection results in selection of chimeric parasites where the hdhfr::yfcu SM in the 230p locus is replaced by the Pfcs expression cassette (Fig. S3A). Selected transgenic parasites (line 2266) were cloned by the method of limiting dilution. Clone line 2266cl1 (PbANKA-PfCSPPbuis4) was selected for further analysis. Correct integration of the construct into the genome of transgenic parasites was analysed by diagnostic PCR analysis of gDNA and Southern analysis of pulsed field gel (PFG)-separated chromosomes (Fig. S3B,C). Primer sequences are listed in Supplementary Tables S3 and S4.
In vitro infection of human and mouse hepatoma cell lines
Human (Huh7, HepG2, and HC-04) and mouse (Hepa1-6) hepatoma or immortalized hepatocyte cell lines were cultured in RPMI medium supplemented with fetal bovine serum (FBS), 50 µg/mL Penicillin/Streptomycin, 2 mM Glutamine 0.1 mM non-essential amino acids (Gibco) at 37 °C with 5% CO2. Cells were infected 24 h after seeding, by adding 5 × 104 freshly dissected sporozoites in supplemented RPMI medium containing Fungizone (1 µg/mL, Gibco), followed by a 5-min centrifugation at 3000 rpm. The number of infected hepatocytes was assessed by staining for Plasmodium Hsp-70 (mAb 2E6) and indirect immuno-fluorescence analysis, as previously described.63
In vitro infection of mouse and rabbit PH
Mouse PH were isolated from livers of adult C57BL/6 male mice following an adaptation of a previously described perfusion method.64 Briefly, mouse livers were initially perfused with 30–40 mL of liver perfusion medium (LPM, Gibco) at 37 °C and a controlled flow rate of 7–9 mL/min, through a cannula inserted in the portal vein, followed by digestion with 30–40 mL of liver digest medium (LDM, Gibco). The liver was then transferred to a cell culture dish containing 10 mL of LDM, its capsule membrane removed and shaken to release loose cells. The cell suspension was then serially passed through 100 and 70 µm cell strainers, washed twice with 30 mL 4% (v/v) FBS supplemented William’s E Medium (Gibco) at 30 g for 3 min at 20 °C and purified by layering over a 60% Percoll gradient (GE Healthcare), followed by centrifugation for 20 min at 750 g, 20 °C, with no break. Purified viable hepatocytes were counted with Trypan blue and plated on collagen-coated plates before infection with freshly dissected Pb sporozoites (1 × 105 hepatocytes infected with 7 × 104 sporozoites). An adaptation of the mouse PH isolation protocol described above was applied for isolation of rabbit PH. Briefly, animals were euthanized by injection of 150 mg/kg IV Sodium Pentobarbital (Eutasil, CEVA), exsanguinated by direct heart puncture and immediately opened to begin the process of liver perfusion. The portal vein was cannulated with a 21G needle and the inferior vena cava cute for outflow. Perfused occurred with 400–500 mL of liver perfusion medium (LPM, Gibco) at 37 °C followed by digestion with 400–500 mL of liver digest medium (LDM, Gibco) at a flow rate of 18 mL/min, controlled by a peristaltic pump. The liver was carefully removed, cut in small pieces and gently shaken to release loose cells. The cell suspension was then treated identically to mouse PH to isolate purified viable hepatocytes which were plated on collagen-coated plates and allowed to settle and attach overnight. Pb infection and development was assessed by immunofluorescence using mouse anti-Plasmodium Hsp-70 (mAb 2E6), rabbit anti-Pb MSP1, goat anti-Pb UIS4, mouse anti-Pb CS (mAb 3D11) and mouse anti-Pf CS (mAb 2A10) and appropriate secondary antibodies, as previously described.63
In vitro infection of human PH
Pb and Pf infection of human PH was performed on either micropatterned co-culture (MPCC) preparations as previously described65 or on cultures of fresh primary human hepatocytes isolated from patients undergoing partial hepatectomy. Briefly, for micropatterned co-cultures, 1 × 104 cryopreserved primary human hepatocytes (Life Technologies) were seeded on collagen-micropatterned plates softlithographically patterned with 500 µm islands together with 7 × 103 3T3-J2 murine embryonic fibroblasts. One day after seeding, 7 × 104 freshly dissected Pb sporozoites were added to each well and subsequently, cells were fixed at various time points post infection for immunofluorescence microscopy analysis. For fresh primary human hepatocyte culture, viable hepatocytes were seeded into collagen-coated 96-well flat-bottom plates (5 × 104 hepatocytes/well) in complete William’s B medium and cultured at 37 °C in an atmosphere of 5% CO2. Two days after seeding, a batch of 5 × 104 freshly dissected Pf or Pb sporozoites were added to each well. Cells were fixed 2 and 5 days after infection for Pb and for Pf, respectively. The number of infected hepatocytes was assessed by staining for Plasmodium Hsp-70 (mAb 2E6) and indirect immunofluorescence analysis.
In vivo infection of liver humanized FRG mice
Highly repopulated FRG mice were obtained from Yecuris (Tualatin, Oregon, USA), as previously described.66 Briefly, six-to-eight weeks old mice received an injection in the spleen of cryopreserved human hepatocytes from a single donor. The mice were then subjected to standardized NTBC (2-(2-nitro-4-trifluoromethylbenzoyl)-1,3-cyclohexanedione) withdrawal regimen. Starting eight weeks post transplantation, human albumin levels are monitored using the Bethyl Laboratory Quantitative Human Albumin ELISA Kit (Catalog #E90-134) according to the manufacturer’s protocol. Mice with albumin levels above 5 mg/mL, corresponding to <95% repopulation, were included in the study. For Pb infection, liver chimeric FRG humanized mice were injected respectively with 2 × 106 sporozoites or uninfected mosquito salivary glands as control. Mice were euthanized 48 h post infection and parts of the liver were either preserved in RNAlater, or placed in 4% paraformaldehyde for 24 h, after which they were stored in PBS and further processed to paraffin blocks. For microscopy analyses of Pb-infected livers, liver sections were either stained with hematoxylin and eosin following standard procedures or a combination of anti-PbUIS4 antibody and anti-fumarylacetoacetate hydrolase (Yecuris®) and/or by anti-hepatocyte specific antigen antibody (OCH1E5, Santa Cruz®). For Pf challenge, mice received an intraperitoneal injection of either 10 mg rabbit IgG purified from immunized rabbits, or PBS, in an adaptation of a previously established methodology.33 Briefly, IgG purification from 3–8 ml plasma samples was performed using Ab SpinTrap columns (GE Healthcare Life Sciences), according to the manufacturer’s instructions and purified IgGs were further concentrated to 200 µl using Amicon Ultra-0.5 Centrifugal Filter Units with Ultracel-30 membrane (Millipore) also according to the manufacturer’s instructions. Twenty-four hours after injection, animals were exposed to the bites of 20 Pf-infected mosquitoes for 20 min. Successful blood feeding and sporozoite presence was confirmed by mosquito dissection after the challenge experiment. Five days later, mice were euthanized and liver parasite burden (ring stage equivalent parasites (Pf) per 106 human hepatocytes) was determined as previously described.67 Each liver was divided into 12 sections, of which 25 mg tissue was weighed and DNA was extracted into 100 µL elution buffer with the High Pure PCR Template Preparation Kit (Roche, Zaventem Belgium). Pf DNA levels were quantified using a highly sensitive qPCR assay. qPCR was also employed to assess the degree of repopulation with human hepatocytes of the chimeric livers, and to normalize the Pf copy numbers.
In vivo infection of blood-chimeric humanized mice
Highly engrafted mice with human erythrocytes (hE) were obtained and infected as previously described.29 Briefly, NOD-scid IL-2Rγnull mice (NSG) obtained from Charles River laboratories were injected i.p. daily throughout the experiment with hE. When 60–70% chimerism in peripheral blood was reached (7–10 days after initiation of injections), the mice were infected by iv injection of 1 × 107 parasites obtained from infected donors or 5 × 105 freshly dissected sporozoites (not shown). Parasitemia was measured during the following days by flow cytometry analysis of 2 µl of blood collected from the tail lateral vein of infected mice as previously described.68 Blood was rapidly transferred into 0.1 ml of saline containing 2.5 or 5 µM SYTO-16 (for Pb) and 10 µg/ml TER119-PE (for murine erythroid lineage), and incubated for 20 min at room temperature in the dark. Ten microliter of saline containing 0.25% (w/v) glutaraldehyde was then added to each sample and incubated for an additional 5 min for complete Plasmodium inactivation. The samples were then analysed on FACScalibur or LSRII flow cytometers (Becton Dickinson). Erythrocytes were gated based on side scatter and forward scatter analysis, followed by a key compensation step for SYTO-16 to accurately define the region of infected events by comparison of the effect of increasing compensation of the emission of SYTO-16 in samples from uninfected and Plasmodium-infected mice. Results were analyzed using either CellQuest-Pro or BD FACSDiva 5.0 (Becton Dickinson) software. Microscopic analysis of samples of peripheral blood from infected mice was simultaneously performed in blood smears stained with 10% (v/v) Giemsa in saline buffer (0.015 M NaCl, 0.001 M phosphate buffer, pH 7.0).
In silico identification of CD8+ T cell epitopes in the Pf and Pb proteomes
The complete proteomes of Pf and Pb, consisting of 5548 and 5076 annotated proteins, respectively, were downloaded from PlasmoDB (v36).69 CD8+ T cell epitope prediction was performed with the package NetMHCpan (v4.0),70 and was based on ten alleles representative of the HLA-A and HLA-B supertypes, with allele frequencies as described in the Allele Frequency Net Database,71 accessed on 22 February 2018. Peptide lengths of 9, 10, and 11 residues were used to search for 9 residue-long core epitopes. Reported results are based only on strong binders, which are defined as those in the top 0.5% of affinity binding prediction scores, according to best practices.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Electronic supplementary material
Acknowledgements
The authors would like to acknowledge Ana Filipa Teixeira, Ana Parreira, and Geert-Jan van Gemert for mosquito production and infection, the bioimaging, rodent, and flow cytometry facilities of Instituto de Medicina Molecular for technical support, and Thomas Hanscheid and Bruno Silva-Santos for insightful discussions. This project was funded by Bill & Melinda Gates Foundation’s grant OPP1025364 and Fundação para a Ciência e Tecnologia (FCT-Portugal)’s grant PTDC/BBB-BMD/2695/2014. K.A.M., A.D., and J.C.S. were supported by the National Institute of Allergy and Infectious Diseases, National Institutes of Health (U19AI110820). A.M.M. and M.P. would like to acknowledge FCT-Portugal for grants SFRH/BPD/80693/2011 and Investigador FCT 2013, respectively.
Author contributions
A.M.M. contributed to the experimental design, carried out and co-supervised the experimental work, produced the figures, and co-wrote the manuscript. I.R., M.M., N.G.R., L.F., C.M., A.M.S., A.S.P.Y., K.A.M., A.D., C.C.H., B.J.D., S.V., J.M.S., and I.A. carried out experimental work and analysis. S.N.B. and J.B. provided crucial biological materials. I.A.B., J.C.S., G.L.R., C.J.J., S.M.K., M.M.M., and R.W.S. contributed to the experimental design, provided intellectual input, and supervised researchers. M.P. coordinated the study, contributed to the experimental design, supervised the experimental work, and wrote the manuscript. All authors read and approved the final manuscript.
Competing interests
A.M.M., M.M.M., and M.P. are inventors on a patent or patent application issued, allowed or filed internationally, covering parts of this work. All other authors declare no competing interests.
Footnotes
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary information accompanies the paper on the npj Vaccines website (10.1038/s41541-018-0068-2).
References
- 1.Malaria vaccine: WHO position paper-January 2016. Wkly Epidemiol Rec91, 33–51 (2016). [PubMed]
- 2.Prudencio M, Rodriguez A, Mota MM. The silent path to thousands of merozoites: the Plasmodium liver stage. Nat. Rev. Microbiol. 2006;4:849–856. doi: 10.1038/nrmicro1529. [DOI] [PubMed] [Google Scholar]
- 3.Hill AV. Vaccines against malaria. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2011;366:2806–2814. doi: 10.1098/rstb.2011.0091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gordon DM, et al. Safety, immunogenicity, and efficacy of a recombinantly produced Plasmodium falciparum circumsporozoite protein-hepatitis B surface antigen subunit vaccine. J. Infect. Dis. 1995;171:1576–1585. doi: 10.1093/infdis/171.6.1576. [DOI] [PubMed] [Google Scholar]
- 5.Olotu A, et al. Seven-year efficacy of RTS,S/AS01 malaria vaccine among young African children. N. Engl. J. Med. 2016;374:2519–2529. doi: 10.1056/NEJMoa1515257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hoffman SL, et al. Protection of humans against malaria by immunization with radiation-attenuated Plasmodium falciparum sporozoites. J. Infect. Dis. 2002;185:1155–1164. doi: 10.1086/339409. [DOI] [PubMed] [Google Scholar]
- 7.Nussenzweig RS, Vanderberg J, Most H, Orton C. Protective immunity produced by the injection of x-irradiated sporozoites of plasmodium berghei. Nature. 1967;216:160–162. doi: 10.1038/216160a0. [DOI] [PubMed] [Google Scholar]
- 8.Seder RA, et al. Protection against malaria by intravenous immunization with a nonreplicating sporozoite vaccine. Science. 2013;341:1359–1365. doi: 10.1126/science.1241800. [DOI] [PubMed] [Google Scholar]
- 9.Mueller AK, Labaied M, Kappe SH, Matuschewski K. Genetically modified Plasmodium parasites as a protective experimental malaria vaccine. Nature. 2005;433:164–167. doi: 10.1038/nature03188. [DOI] [PubMed] [Google Scholar]
- 10.van Dijk MR, et al. Genetically attenuated, P36p-deficient malarial sporozoites induce protective immunity and apoptosis of infected liver cells. Proc. Natl Acad. Sci. USA. 2005;102:12194–12199. doi: 10.1073/pnas.0500925102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Butler NS, et al. Superior antimalarial immunity after vaccination with late liver stage-arresting genetically attenuated parasites. Cell Host Microbe. 2011;9:451–462. doi: 10.1016/j.chom.2011.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van Schaijk, B. C. et al. A genetically attenuated malaria vaccine candidate based on P. falciparum b9/slarp gene-deficient sporozoites. Elife 3, 10.7554/eLife.03582 (2014).. [DOI] [PMC free article] [PubMed]
- 13.Kublin, J. G. et al. Complete attenuation of genetically engineered Plasmodium falciparum sporozoites in human subjects. Sci Transl Med9, 9/371/eaad9099 (2017). [DOI] [PubMed]
- 14.Roestenberg M, et al. Protection against a malaria challenge by sporozoite inoculation. N. Engl. J. Med. 2009;361:468–477. doi: 10.1056/NEJMoa0805832. [DOI] [PubMed] [Google Scholar]
- 15.Mordmuller, B. et al. Sterile protection against human malaria by chemoattenuated PfSPZ vaccine. Nature, 10.1038/nature21060 (2017).. [DOI] [PMC free article] [PubMed]
- 16.Beaudoin RL, Strome CP, Mitchell F, Tubergen TA. Plasmodium berghei: immunization of mice against the ANKA strain using the unaltered sporozoite as an antigen. Exp. Parasitol. 1977;42:1–5. doi: 10.1016/0014-4894(77)90054-6. [DOI] [PubMed] [Google Scholar]
- 17.Kumar KA, et al. The circumsporozoite protein is an immunodominant protective antigen in irradiated sporozoites. Nature. 2006;444:937–940. doi: 10.1038/nature05361. [DOI] [PubMed] [Google Scholar]
- 18.Mendes, A. M. et al. in Malaria (eds Maria M. Mota & Ana Rodriguez) (Springer, 2017).
- 19.Borrmann S, Matuschewski K. Targeting Plasmodium liver stages: better late than never. Trends Mol. Med. 2011;17:527–536. doi: 10.1016/j.molmed.2011.05.008. [DOI] [PubMed] [Google Scholar]
- 20.Ishizuka AS, et al. Protection against malaria at 1 year and immune correlates following PfSPZ vaccination. Nat. Med. 2016;22:614–623. doi: 10.1038/nm.4110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sissoko, M. S. et al. Safety and efficacy of PfSPZ Vaccine against Plasmodium falciparum via direct venous inoculation in healthy malaria-exposed adults in Mali: a randomised, double-blind phase 1 trial. Lancet Infect Dis, 10.1016/S1473-3099(17)30104-4 (2017). [DOI] [PMC free article] [PubMed]
- 22.Lyke, K. E. et al. Attenuated PfSPZ Vaccine induces strain-transcending T cells and durable protection against heterologous controlled human malaria infection. Proceedings of the National Academy of Sciences of the United States of America, 10.1073/pnas.1615324114 (2017). [DOI] [PMC free article] [PubMed]
- 23.Epstein JE, et al. Protection against Plasmodium falciparum malaria by PfSPZ Vaccine. JCI Insight. 2017;2:e89154. doi: 10.1172/jci.insight.89154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Plotkin S. History of vaccination. Proc. Natl Acad. Sci. USA. 2014;111:12283–12287. doi: 10.1073/pnas.1400472111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zajac BA, West DJ, McAleer WJ, Scolnick EM. Overview of clinical studies with hepatitis B vaccine made by recombinant DNA. J. Infect. 1986;13(Suppl A):39–45. doi: 10.1016/S0163-4453(86)92668-X. [DOI] [PubMed] [Google Scholar]
- 26.Belshe RB, et al. The efficacy of live attenuated, cold-adapted, trivalent, intranasal influenzavirus vaccine in children. N. Engl. J. Med. 1998;338:1405–1412. doi: 10.1056/NEJM199805143382002. [DOI] [PubMed] [Google Scholar]
- 27.Guirakhoo F, et al. Immunogenicity, genetic stability, and protective efficacy of a recombinant, chimeric yellow fever-Japanese encephalitis virus (ChimeriVax-JE) as a live, attenuated vaccine candidate against Japanese encephalitis. Virology. 1999;257:363–372. doi: 10.1006/viro.1999.9695. [DOI] [PubMed] [Google Scholar]
- 28.Prudencio M, Mota MM, Mendes AM. A toolbox to study liver stage malaria. Trends Parasitol. 2011;27:565–574. doi: 10.1016/j.pt.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 29.Angulo-Barturen I, et al. A murine model of falciparum-malaria by in vivo selection of competent strains in non-myelodepleted mice engrafted with human erythrocytes. PLoS ONE. 2008;3:e2252. doi: 10.1371/journal.pone.0002252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lin JW, et al. A novel ‘gene insertion/marker out’ (GIMO) method for transgene expression and gene complementation in rodent malaria parasites. PLoS ONE. 2011;6:e29289. doi: 10.1371/journal.pone.0029289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mueller AK, et al. Plasmodium liver stage developmental arrest by depletion of a protein at the parasite-host interface. Proc. Natl Acad. Sci. USA. 2005;102:3022–3027. doi: 10.1073/pnas.0408442102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tewari R, Spaccapelo R, Bistoni F, Holder AA, Crisanti A. Function of region I and II adhesive motifs of Plasmodium falciparum circumsporozoite protein in sporozoite motility and infectivity. J. Biol. Chem. 2002;277:47613–47618. doi: 10.1074/jbc.M208453200. [DOI] [PubMed] [Google Scholar]
- 33.Behet MC, et al. Sporozoite immunization of human volunteers under chemoprophylaxis induces functional antibodies against pre-erythrocytic stages of Plasmodium falciparum. Malar. J. 2014;13:136. doi: 10.1186/1475-2875-13-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Persson C, et al. Cutting edge: a new tool to evaluate human pre-erythrocytic malaria vaccines: rodent parasites bearing a hybrid Plasmodium falciparum circumsporozoite protein. J. Immunol. 2002;169:6681–6685. doi: 10.4049/jimmunol.169.12.6681. [DOI] [PubMed] [Google Scholar]
- 35.Zhang M, et al. A highly infectious Plasmodium yoelii parasite, bearing Plasmodium falciparum circumsporozoite protein. Malar. J. 2016;15:201. doi: 10.1186/s12936-016-1248-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kumar KA, Baxter P, Tarun AS, Kappe SH, Nussenzweig V. Conserved protective mechanisms in radiation and genetically attenuateduis3(-) and uis4(-) Plasmodium sporozoites. PLoS O. 2009;4:e4480. doi: 10.1371/journal.pone.0004480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pichyangkul S, et al. Chemoprophylaxis with sporozoite immunization in P. knowlesi rhesus monkeys confers protection and elicits sporozoite-specific memory T cells in the liver. PLoS ONE. 2017;12:e0171826. doi: 10.1371/journal.pone.0171826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nussenzweig RS, Vanderberg JP, Most H, Orton C. Specificity of protective immunity produced by x-irradiated Plasmodium berghei sporozoites. Nature. 1969;222:488–489. doi: 10.1038/222488a0. [DOI] [PubMed] [Google Scholar]
- 39.Nussenzweig RS, et al. Sporozoite-induced immunity in mammalian malaria. A review. Am. J. Trop. Med. Hyg. 1972;21:722–728. doi: 10.4269/ajtmh.1972.21.722. [DOI] [PubMed] [Google Scholar]
- 40.Douradinha B, et al. Genetically attenuated P36p-deficient Plasmodium berghei sporozoites confer long-lasting and partial cross-species protection. Int. J. Parasitol. 2007;37:1511–1519. doi: 10.1016/j.ijpara.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 41.Sedegah M, Weiss WW, Hoffman SL. Cross-protection between attenuated Plasmodium berghei and P. yoelii sporozoites. Parasite Immunol. 2007;29:559–565. doi: 10.1111/j.1365-3024.2007.00976.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Weiss WR, et al. A T cell clone directed at the circumsporozoite protein which protects mice against both Plasmodium yoelii and Plasmodium berghei. J. Immunol. 1992;149:2103–2109. [PubMed] [Google Scholar]
- 43.Sina BJ, do Rosario VE, Woollett G, Sakhuja K, Hollingdale MR. Plasmodium falciparum sporozoite immunization protects against Plasmodium berghei sporozoite infection. Exp. Parasitol. 1993;77:129–135. doi: 10.1006/expr.1993.1069. [DOI] [PubMed] [Google Scholar]
- 44.Blanquart S, Gascuel O. Mitochondrial genes support a common origin of rodent malaria parasites and Plasmodium falciparum’s relatives infecting great apes. BMC Evol. Biol. 2011;11:70. doi: 10.1186/1471-2148-11-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mauduit M, et al. A role for immune responses against non-CS components in the cross-species protection induced by immunization with irradiated malaria sporozoites. PLoS ONE. 2009;4:e7717. doi: 10.1371/journal.pone.0007717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gruner AC, et al. Sterile protection against malaria is independent of immune responses to the circumsporozoite protein. PLoS One. 2007;2:e1371. doi: 10.1371/journal.pone.0001371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Doolan DL, et al. Identification of Plasmodium falciparum antigens by antigenic analysis of genomic and proteomic data. Proc. Natl Acad. Sci. USA. 2003;100:9952–9957. doi: 10.1073/pnas.1633254100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bergmann-Leitner ES, et al. Immunization with pre-erythrocytic antigen CelTOS from Plasmodium falciparum elicits cross-species protection against heterologous challenge with Plasmodium berghei. PLoS ONE. 2010;5:e12294. doi: 10.1371/journal.pone.0012294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Herrington D, et al. Successful immunization of humans with irradiated malaria sporozoites: humoral and cellular responses of the protected individuals. Am. J. Trop. Med. Hyg. 1991;45:539–547. doi: 10.4269/ajtmh.1991.45.539. [DOI] [PubMed] [Google Scholar]
- 50.Nardin EH, et al. Cellular and humoral immune responses to a recombinant P. falciparum CS protein in sporozoite-immunized rodents and human volunteers. Bull. World Health Organ. 1990;68(Suppl):85–87. [PMC free article] [PubMed] [Google Scholar]
- 51.Trieu A, et al. Sterile protective immunity to malaria is associated with a panel of novel P. falciparum antigens. Mol. Cell Proteom. 2011;10:007948. doi: 10.1074/mcp.M111.007948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Egan JE, et al. Humoral immune responses in volunteers immunized with irradiated Plasmodium falciparum sporozoites. Am. J. Trop. Med. Hyg. 1993;49:166–173. doi: 10.4269/ajtmh.1993.49.166. [DOI] [PubMed] [Google Scholar]
- 53.Enea V, et al. DNA cloning of Plasmodium falciparum circumsporozoite gene: amino acid sequence of repetitive epitope. Science. 1984;225:628–630. doi: 10.1126/science.6204384. [DOI] [PubMed] [Google Scholar]
- 54.Nardin EH, et al. Circumsporozoite proteins of human malaria parasites Plasmodium falciparum and Plasmodium vivax. J. Exp. Med. 1982;156:20–30. doi: 10.1084/jem.156.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Herrington DA, et al. Safety and immunogenicity in man of a synthetic peptide malaria vaccine against Plasmodium falciparum sporozoites. Nature. 1987;328:257–259. doi: 10.1038/328257a0. [DOI] [PubMed] [Google Scholar]
- 56.Nardin EH. T cell responses in a sporozoite-immunized human volunteer and a chimpanzee. Immunol. Lett. 1990;25:43–47. doi: 10.1016/0165-2478(90)90089-9. [DOI] [PubMed] [Google Scholar]
- 57.Moreno A, et al. Cytotoxic CD4+ T cells from a sporozoite-immunized volunteer recognize the Plasmodium falciparum CS protein. Int. Immunol. 1991;3:997–1003. doi: 10.1093/intimm/3.10.997. [DOI] [PubMed] [Google Scholar]
- 58.Azevedo, R. et al. Bioluminescence Method for In Vitro Screening of Plasmodium Transmission-Blocking Compounds. Antimicrob Agents Chemother61, 10.1128/AAC.02699-16 (2017). [DOI] [PMC free article] [PubMed]
- 59.Al-Olayan EM, Beetsma AL, Butcher GA, Sinden RE, Hurd H. Complete development of mosquito phases of the malaria parasite in vitro. Science. 2002;295:677–679. doi: 10.1126/science.1067159. [DOI] [PubMed] [Google Scholar]
- 60.Janse CJ, et al. High efficiency transfection of Plasmodium berghei facilitates novel selection procedures. Mol. Biochem Parasitol. 2006;145:60–70. doi: 10.1016/j.molbiopara.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 61.Salman AM, et al. Generation of transgenic rodent malaria parasites expressing human malaria parasite proteins. Methods Mol. Biol. 2015;1325:257–286. doi: 10.1007/978-1-4939-2815-6_21. [DOI] [PubMed] [Google Scholar]
- 62.Ponnudurai T, Leeuwenberg AD, Meuwissen JH. Chloroquine sensitivity of isolates of Plasmodium falciparum adapted to in vitro culture. Trop. Geogr. Med. 1981;33:50–54. [PubMed] [Google Scholar]
- 63.Meireles, P. et al. GLUT1-mediated glucose uptake plays a crucial role during Plasmodium hepatic infection. Cell. Microbiol.19(2), e12646, (2017). [DOI] [PMC free article] [PubMed]
- 64.Goncalves LA, Vigario AM, Penha-Goncalves C. Improved isolation of murine hepatocytes for in vitro malaria liver stage studies. Malar. J. 2007;6:169. doi: 10.1186/1475-2875-6-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.March S, et al. A microscale human liver platform that supports the hepatic stages of Plasmodium falciparum and vivax. Cell Host Microbe. 2013;14:104–115. doi: 10.1016/j.chom.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Foquet L, et al. Successful engraftment of human hepatocytes in uPA-SCID and FRG(R) KO mice. Methods Mol. Biol. 2017;1506:117–130. doi: 10.1007/978-1-4939-6506-9_8. [DOI] [PubMed] [Google Scholar]
- 67.Foquet L, et al. Molecular detection and quantification of Plasmodium falciparum-infected human hepatocytes in chimeric immune-deficient mice. Malar. J. 2013;12:430. doi: 10.1186/1475-2875-12-430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jimenez-Diaz MB, et al. Quantitative measurement of Plasmodium-infected erythrocytes in mliver digest mediumurine models of malaria by flow cytometry using bidimensional assessment of SYTO-16 fluorescence. Cytom. A. 2009;75:225–235. doi: 10.1002/cyto.a.20647. [DOI] [PubMed] [Google Scholar]
- 69.Aurrecoechea C, et al. PlasmoDB: a functional genomic database for malaria parasites. Nucleic Acids Res. 2009;37:D539–D543. doi: 10.1093/nar/gkn814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Jurtz V, et al. NetMHCpan-4.0: improved peptide-MHC class I interaction predictions integrating eluted ligand and peptide binding affinity data. J. Immunol. 2017;199:3360–3368. doi: 10.4049/jimmunol.1700893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gonzalez-Galarza FF, et al. Allele frequency net 2015 update: new features for HLA epitopes, KIR and disease and HLA adverse drug reaction associations. Nucleic Acids Res. 2015;43:D784–D788. doi: 10.1093/nar/gku1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.