Abstract
Objective/Background
Despite a well-established role of guilt cognitions in the maintenance and treatment of posttraumatic stress disorder (PTSD), relationships of guilt cognitions to nightmares are not well understood. This study investigated the ways in which guilt cognitions related to traumatic events influenced the relationship between combat exposure and trauma-related sleep disturbance in military Veterans with PTSD.
Participants
We recruited a sample of 50 Veterans with PTSD who completed study measures at a screening session.
Methods
Participants completed self-report measures of exposure to potentially traumatic events, trauma-related guilt (hindsight bias, wrongdoing, and lack of justification) and trauma-related sleep disturbance as measured by a self-report scale and clinician ratings of nightmare severity.
Results
Bivariate regression analyses established a relationship of combat exposure to wrongdoing (β = .31, p = .031), and a relationship of wrongdoing with self-reported trauma-related sleep disturbance (β = .27, p = .049) and clinician-rated nightmare severity (β = .36, p = .009). Bootstrapping analysis that included years of education as a covariate found a significant overall indirect effect of combat exposure on clinician-rated nightmare severity exerted through wrongdoing (β = .10, 95% CI [.004, .246]).
Conclusions
Results suggest the association of combat exposure with trauma-related sleep disturbance is significantly influenced by perceived wrongdoing related to a traumatic event. Targeting cognitions related to wrongdoing and moral injury during a traumatic event in PTSD treatment may help ameliorate trauma-related sleep disturbance.
Keywords: nightmares, posttraumatic stress disorder, traumatic stress, guilt, sleep
Introduction
Posttraumatic nightmares are present in up to 80% of individuals within 3 months of trauma exposure and, unlike nightmares associated with other conditions, can emerge from both rapid eye movement (REM) and non-rapid eye movement (NREM) sleep (Aurora et al., 2010). In addition to nightmares, those with trauma exposure also frequently report acting out their dreams (REM without atonia) and disruptive nocturnal behaviors or phenomenon (e.g., screaming or yelling; combative or defensive behaviors during sleep; profuse sweating during sleep) (Mysliwiec et al., 2014). A few prior studies have examined temporal relationships between trauma exposure and subsequent sleep disturbance (Engdahl, Eberly, Hurwitz, Mahowald, & Blake, 2000; Hefez, Metz, & Lavie, 1987; Lavie, Hefez, Halperin, & Enoch, 1979; Seelig et al., 2010). Among 41,225 Millennium Cohort Study participants completing surveys at baseline and follow-up, combat exposure mediated the relationship between deployment status (deployed/not deployed) and both sleep duration and trouble sleeping. Exposure to combat has been linked with sleep disturbance, independent of whether that combat exposure was identified as a PTSD index trauma (Capaldi, Guerrero, & Killgore, 2011; Insana, Hall, Buysse, & Germain, 2013; Mellman, Kulick-Bell, Ashlock, & Nolan, 1995).
The presence of guilt may be especially relevant among combat Veterans who are at increased risk of moral injury. Indeed, killing in combat and participating in atrocities have been associated with higher levels of combat-related guilt (Beckham, Feldman, & Kirby, 1998; Dennis et al., 2017). Furthermore, participation in atrocities has specifically been linked to guilt-related cognitions about perceived responsibility and wrongdoing (Beckham et al., 1998; Stein et al., 2012). Guilt is believed to be a fundamental emotional response to moral injury (Farnsworth, Drescher, Nieuwsma, Walser, & Currier, 2014; Litz et al., 2009). Guilt stems from violating social/moral prohibitions against harming other people (Gilbert, 2004), which makes it particularly relevant among veterans who have experienced combat and/or other morally injurious events in which others were harmed. This violation of standards of behavior (i.e. perceived wrongdoing) could result in moral injury if the Veteran has distress related to unresolved conflicts between actions taken in combat and personal standards drawn from civilian society. Moral injury manifests in a combination of posttraumatic stress disorder-like symptoms (e.g., intrusion, re-experiencing, avoidance), intense feelings of shame, guilt, and demoralization, and self-harm and/or self-handicapping behaviors (Litz et al., 2009).
Guilt following combat exposure could be related to subsequent trauma-related sleep disturbance. For example, examination of nightmare themes discussed during nightmare treatment with Imagery Rehearsal Therapy (IRT) for military Veterans found that war-related disgust and guilt were among the most common themes targeted for treatment (Harb, Thompson, Ross, & Cook, 2012). This finding suggests that guilt-related cognitions are particularly salient among those experiencing chronic nightmares. Prior research has not, however, specifically examined the role of guilt or wrongdoing in trauma-related sleep disturbance. In theory, potentially morally injurious events trigger the individual to have conflict about how to accommodate their pre-trauma assumptions about themselves, others, and the world with their perceived wrongdoing. This conflict drives increased avoidance and intrusions, including sleep disturbance generally and nightmares specifically (Litz et al., 2009).
We analyzed data from a group of treatment-seeking Veterans, approximately half of whom had been exposed to combat. We hypothesized that the association of combat exposures with trauma-related sleep disturbance would be significantly explained by the intervening effects of trauma-related perceived wrongdoing.
2. Method
2.1. Participants and Procedure
Data were derived from screening session assessments of 50 military Veterans who volunteered to participate in a pilot clinical trial on combined treatment for PTSD and smoking cessation. Participants were randomized using an electronic password-protected randomization sequence generated before the trial and only accessed by staff with no other involvement in the conduct of the study. Data presented in this report were collected in the screening session, prior to randomization or treatment initiation. Participants completed self-report and interview measures. Participants could be compensated a maximum of $545 for their time and effort over the course of the study, including incentive payments for completing ecological momentary assessments. The complete randomization sequence was generated prior to the initiation of the study and stored electronically in a password-protected file that was accessed by study staff who had no interactions with study participants. Recruitment methods included flyers, VA clinicians informing patients about the availability of the study, and invitational letters providing a brief description of the study with a phone number to call for more information. One participant who had not been exposed to combat was missing the TRGI and PSQI-A. Another participant who had been exposed to combat was missing the PSQI-A. Otherwise, there were no missing items from any measures used in analyses for the current report. Participants were removed from analyses in which they were missing data on one of the analysis variables. Demographic information for the sample is presented in Table 1.
Table 1.
Sociodemographic Information.
| Sociodemographic Variable | Combat- Exposed (n=26) |
No Combat Exposure (n=24) |
||
|---|---|---|---|---|
|
| ||||
| Frequency (%) |
Frequency (%) |
Test statistic |
p-values | |
| Race/Ethnic Category | ||||
| African American | 13 (50%) | 17 (71%) | Χ2(1)=1.42 | p = .233 |
| White | 8 (31%) | 3 (13%) | ||
| Hispanic | 2 (8%) | 0 (0%) | ||
| Multiple Races | 3 (12%) | 4 (17%) | ||
| Sex (% Male) | 23 (88%) | 18 (75%) | Χ2(1)=1.53 | p = .126 |
| Marital Status | Χ2(4)=6.83 | p = .145 | ||
| Married | 9 (35%) | 6 (26%) | ||
| Separated/Divorced | 9 (35%) | 15 (63%) | ||
| Never Married | 7 (27%) | 1 (4%) | ||
| Widowed | 1 (4%) | 1 (4%) | ||
| Missing | 0 (0%) | 1 (4%) | ||
| Psychiatric Disorders | ||||
| Current Major Depression | 8 (31%) | 11 (46%) | Χ2(1)=1.98 | p = .321 |
| Lifetime Major Depression | 16 (62%) | 11 (46%) | Χ2(1)=1.63 | p = .201 |
| Lifetime Alcohol Use Disorder | 15 (58%) | 17 (71%) | Χ2(1)=0.94 | p = .334 |
| Lifetime Drug Use Disorder | 22 (85%) | 16 (67%) | Χ2(1)=2.20 | p = .138 |
| Index Trauma | ||||
| Combat | 18 (69%) | 0 (0%) | ||
| Child Physical/Sexual Abuse | 2 (8%) | 2 (8%) | ||
| Adult Physical/Sexual Abuse | 1 (4%) | 9 (38%) | ||
| Sudden Medical Crisis | 0 (0%) | 1 (4%) | ||
| Accident | 2 (8%) | 2 (8%) | ||
| Domestic Violence | 1 (4%) | 0 (0%) | ||
| Death of Someone Close | 2 (8%) | 6 (25%) | ||
| Witness/Experience Violence | 0 (0%) | 4 (17%) | ||
| Variable | Mean (SD) | Mean (SD) | ||
| Age (years) | 46.7 (13.4) | 53.6 (8.6) | t(47)=2.09 | p = .042 |
| Education (years) | 13.6 (1.5) | 12.8 (3.0) | t(46)=−1.22 | p = .227 |
| CAPS Total | 40.1 (9.9) | 36.1 (10.2) | t(48)=−1.41 | p = .165 |
| Clinician-rated Nightmare Severity | 2.62 (1.20) | 1.71 (1.52) | t(48)=−2.35 | p = .023 |
| PSQI-A | 10.0 (5.2) | 8.3 (5.8) | t(46)=−1.10 | p = .277 |
| TRGI-Hindsight | 1.57 (1.10) | 1.14 (1.06) | t(47)=−1.39 | p = .172 |
| TRGI-Wrongdoing | 2.09 (0.86) | 1.58 (0.74) | t(47)=−2.22 | p = .031 |
| TRGI-Lack of Justification | 1.96 (1.15) | 2.42 (1.21) | t(47)=1.37 | p = .178 |
SD = Standard Deviation. CAPS = Clinician-Rated PTSD Scale. PSQI-A = Pittsburgh Sleep Quality Index – PTSD Addendum. TRGI = Trauma-Related Guilt Inventory. Clinician-rated Nightmare Severity range: 0–4. PSQI-A range: 0–21.
All study procedures were approved by the institutional review board at the Durham VA Health System, and all participants provided informed consent prior to initiating participation in the study. To be eligible, participants had to a) be military Veterans, b) smoke at least 10 cigarettes a day, c) meet current criteria for PTSD, d) speak and write fluent English, d) be ages 18–75, and e) be willing to attempt smoking cessation. Participants were excluded if they a) had an unstable medication regimen (e.g., scheduled for chemotherapy for cancer or interferon treatment for hepatitis C), b) had a history of myocardial infarction in the previous 6 months, c) medical contraindication that prevented nicotine replacement therapy use, d) used non-cigarette forms of tobacco, e) pregnancy, f) were unable to complete study measures and tasks, g) were currently receiving trauma-focused psychotherapy or behavioral smoking cessation treatment, h) lived in court-ordered residential substance abuse treatment setting, or i) had any of the following psychiatric comorbidities within the previous 3 months: dementia/brain disorder, schizophrenia, current manic syndrome, or other substance use disorder.
2.2. Measures
2.2.1. Traumatic Life Events Questionnaire (TLEQ) (Kubany et al., 2000)
The TLEQ is a 23-item self-report questionnaire assessing potentially traumatic events. Participants are asked to report the number of times they have experienced each event, from never to more than five times. Previous research has found that data from the TLEQ is reliable over time and demonstrates content validity (Kubany et al., 2000). Because we were interested in the effects of combat-related trauma specifically, we used a TLEQ item asking about whether participants had been in a war zone, and whether participants had been exposed to combat. Participants who endorsed both items were coded as having been exposed to combat.
2.2.2. Trauma-Related Guilt Inventory (TRGI) (Kubany et al., 1996)
The 32-item self-report TRGI is a 32-item self-report questionnaire that measures cognitive and emotional facets of guilt related to traumatic stress (Kubany et al., 1996). These items were rated on a scale from 0 to 4, and were averaged to produce a subscale score for each of the cognitive subscales included in this analysis. The TRGI has a 7-item subscale on hindsight bias that includes items assessing cognitions about one’s responsibility for knowing the outcome before it occurred. The TRGI also has a 5-item subscale on perceived wrongdoing that includes items about behaviors, thoughts, cognitions, or feelings during the traumatic event that violated one’s values. Previous research has found this subscale to be related to morally injurious events among active duty service members, supporting the conceptualization of these two variables as overlapping but not identical (Stein et al., 2012). Finally, the TRGI has a 6-item subscale on lack of justification for one’s actions taken during the traumatic event. The TRGI has demonstrated good internal consistency and convergent validity in military Veterans (Kubany et al., 1996).
2.2.3. Clinician Administered PTSD Scale for DSM-5 (CAPS-5) (Weathers et al., 2013)
All participants completed a CAPS interview to determine whether they had current PTSD. The CAPS is a semi-structured interview that specifies an index traumatic event, then asks about the severity of PTSD symptoms on scale of 0 to 4. Using procedures employed to evaluate primary outcomes in studies targeting nightmares as an outcome (Raskind et al., 2007; Raskind et al., 2013), the severity rating of the nightmare item on the CAPS was used as an outcome for this study. The CAPS-5 has demonstrated good interrater reliability (intraclass correlation coefficient = .91), as well as good convergent and discriminant validity (Weathers et al., 2017). Fleiss’ Kappa reliability for CAPS-5 interviewers in this study was .914.
2.2.4. Structured Clinical Interview for Diagnostic and Statistical Manual of Psychiatric Disorders-Version 4 (DSM-4) (First, Spitzer, Gibbon, & Williams, 1994)
All participants completed the SCID-4 semi-structured diagnostic interview to assess psychiatric diagnoses. Diagnostic raters were trained using standardized SCID training, which included review of interview manuals, training videotapes, and co-rating training with an experienced rater. Fleiss’ Kappa reliability for SCID-4 interviewers in this study was .913.
2.2.5. Pittsburgh Sleep Quality Index – PTSD Addendum (PSQI-A) (Germain, Hall, Krakow, Katherine, & Buysse, 2005)
The PSQI is a 10-item self-report measure that assesses aspects of sleep disturbance in the past month. We also administered the 7-item PSQI–A, which measures the frequency of the following specific experiences commonly associated with PTSD that interfered with sleep: a) hot flashes, b) anxiety, c) memories or nightmares of a traumatic experience, d) severe anxiety or panic unrelated to trauma, e) bad dreams unrelated to trauma, f) terror or screaming during sleep without fully awakening, or g) had episodes of acting out dreams, such as kicking, running or screaming. Those 7 items were summed to produce a self-reported trauma-related sleep disturbance score. The PSQI-A items are each rated on a scale of 0 to 3, resulting in a scale range of 0 to 21. Psychometric testing on the PSQI-A has demonstrated satisfactory internal consistency (Cronbach’s α = .85) and a positive predictive value of 93% for discriminating participants with PTSD from those without PTSD (Germain et al., 2005).
2.3. Data Analyses
Analytical Plan
Due to the relatively small sample size, we had limited statistical power to detect indirect effects in this sample. Consequently, we reduced the number of models we ran by screening potential covariates for relationships with outcome variables before testing them in study models. We first examined bivariate correlations of the following variables with the following outcomes in our models: hindsight bias, wrongdoing, lack of justification, self-reported trauma-related sleep disturbance, and clinician-rated nightmare severity. Potential covariates included age, African American race, Caucasian race, years of education, cigarettes smoked per day, breath carbon monoxide level (collected to as a biological indicator of smoking intensity), sex, marital status, employment status, housing status, and level of nicotine dependence. Because both age and African American race were correlated with less hindsight bias, and breath carbon monoxide was correlated with greater hindsight bias, these variables were evaluated as covariates in sensitivity analyses of regression models that specified hindsight bias as the outcome. Being married was correlated with trauma-related sleep disturbance and was evaluated in sensitivity analyses of regression models that specified trauma-related sleep disturbance as the outcome. Years of education was correlated with clinician-rated nightmare severity and was evaluated in sensitivity analyses of regression models that specified clinician-rated nightmare severity as the outcome.
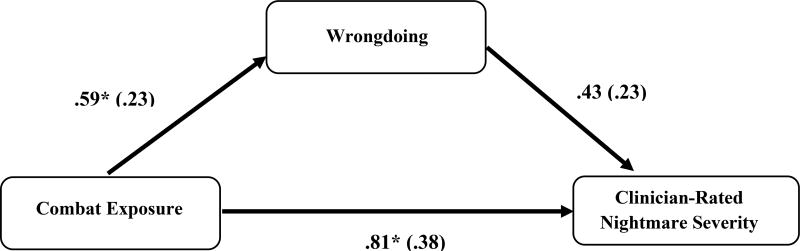
To analyze the indirect pathways by which wrongdoing cognitions might link combat exposure with trauma-related sleep disturbance (illustrated in Figure 1), we first explored the component pathways using bivariate regression equations. These equations specified the relationship of combat exposure with perceived wrongdoing and the association of perceived wrongdoing with trauma-related sleep disturbance. An additional regression equation tested the association of perceived wrongdoing with trauma-related sleep disturbance when combat exposure was included in the model.
Figure 1. Unstandardized Effect Estimates and Standard Errors for Bootstrapped Models of Clinician-Rated Nightmare Severity.
This model adjusted for the influence of years of education. In the overall model, the unstandardized effect of years of education on clinician-rated nightmare severity was −.22** (.08).
Overall unstandardized indirect effect = .25, 95% CI: .01, .71
* p < .05
** p < .01
We followed up this analysis with a bootstrap analysis (5,000 resamples) testing the indirect effects of combat exposure on trauma-related sleep disturbance exerted through perceived wrongdoing. Because bootstrapping generates CIs around the effect estimate, a 95% CI that does not span 0 is statistically significant at the p < .05 level.
3. Results
Participant characteristics are described in Table 1. Intercorrelations among study variables are listed in Table 2. Combat exposure was reported by 26 of the participants (52%). The overall sample had mean PTSD severity in the moderate range on the CAPS (M = 38.2, SD = 10.1). Interviewers rated the CAPS nightmare item at a mean of 2.2 (SD = 1.4). Participants endorsed the PSQI-A self-reported trauma-related sleep disturbance scale at a mean of 9.2 (SD = 5.5). The group with combat exposure was significantly younger, had higher nightmare severity, and had higher perceived wrongdoing on the TRGI.
Table 2.
Intercorrelations Among Major Study Variables.
| Combat Exposure |
Hindsight Bias |
Wrongdoing | Lack of Justification |
Clinician-rated Nightmare Severity (CAPS-5) |
Self-Reported Trauma- Related Sleep Disturbance (PSQI-A) |
|
|---|---|---|---|---|---|---|
| Combat Exposure | --- | |||||
| Hindsight Bias | .19 | --- | ||||
| Wrongdoing | .31* | .40** | --- | |||
| Lack of Justification | −.20 | −.01 | .11 | --- | ||
| Clinician-rated Nightmares | .32* | .15 | .41** | −.09 | --- | |
| Self-Reported Trauma-Related Sleep Disturbance | .16 | −.04 | .35* | .15 | .42** | --- |
CAPS-5 = Clinician-Administered PTSD Scale for DSM-5. PSQI-A = Pittsburgh Sleep Quality Index – PTSD Addendum.
p< .05
p< .01
3.1. Direct Relationship of Combat Exposure to Trauma-Related Sleep Disturbance
Combat exposure was not associated with self-reported trauma-related sleep disturbance in a bivariate regression equation (β = .16, p = .277), or with marital status as a covariate (β = .12, p = .388). In contrast, combat exposure did have direct relationship with clinician-rated nightmare severity in a bivariate regression equation (β = .32, p = .023) that persisted when years of education was included as a covariate (β = .38, p = .005).
3.2. Relationship of Combat Exposure to Guilt Cognitions
Analyses of the relationship of combat exposure to each of the guilt cognition measures found that there was not a statistically significant relationship of combat exposure with hindsight bias in a bivariate regression equation (β = .20, p = .172) or in a regression that included age, African American race, or breath carbon monoxide levels at the screening session as covariates (β = .16, p = .275). There was a statistically significant relationship of combat exposure to wrongdoing in a bivariate regression equation (β = .31, p = .031). A bivariate regression equation of combat exposure predicting lack of justification was not statistically significant (β = −.20, p = .178).
3.3. Relationship of Guilt Cognitions to Trauma-Related Sleep Disturbance
Analyses of the relationship of combat exposure to each of the guilt cognition measures found that there was not a statistically significant relationship of hindsight bias with self-reported trauma-related sleep disturbance in a bivariate regression equation (β = −.04, p = .811), or with marital status as a covariate (β = −.12, p = .340). There was also no statistically significant relationship of hindsight bias to clinician-rated nightmare severity in a bivariate regression equation (β = .15 p = .305), or with years of education as a covariate (β = .19, p = .168). Analyses found that wrongdoing had a statistically significant relationship with self-reported trauma-related sleep disturbance in a bivariate regression equation (β = .35, p = .016), and with marital status as a covariate (β = .27, p = .049). There was also a statistically significant relationship of wrongdoing to clinician-rated nightmare severity in a bivariate regression equation (β = .41 p = .003) that persisted with years of education as a covariate (β = .36, p = .009). The relationship of lack of justification with self-reported trauma-related sleep disturbance was not statistically significant in a bivariate regression equation (β = .15, p = .320), or with marital status as a covariate (β = .08, p = .560). The relationship of lack of justification to clinician-rated nightmare severity was also not statistically significant in a bivariate regression equation (β = −.09 p = .539), or with years of education as a covariate (β = −.19, p = .183).
3.4. Overall Indirect Effects Models
There was a significant indirect effect of combat exposure exerted via wrongdoing on self-reported trauma-related sleep disturbance (β = .101, 95% CI [.010, .255]). With wrongdoing in the model, the remaining direct effect of combat exposure on self-reported trauma-related sleep disturbance was not statistically significant (b = .65, 95% CI: [−2.56, 3.85]). The indirect effects of wrongdoing in the model accounted for 63% of the covariance between combat exposure and self-reported trauma-related sleep disturbance. When marital status was covaried, there was not a statistically significant overall indirect effect of combat exposure exerted via wrongdoing on self-reported trauma-related sleep disturbance (β = .080, 95% CI [−.0005, .238]). The indirect effects of wrongdoing in the model accounted for 62% of the covariance between combat exposure and self-reported trauma-related sleep disturbance.
The bootstrapping model of the indirect association of combat exposure with clinician-rated nightmare severity is illustrated in Figure 1. There was a significant indirect effect of combat exposure exerted via wrongdoing on clinician-rated nightmare severity (β = .109, 95% CI [.017, .271]). With wrongdoing in the model, the remaining direct effect of combat exposure on clinician-rated nightmare severity was not statistically significant (b = .53, 95% CI: [−.25, 1.30]). The indirect effects of wrongdoing accounted for 36% of the covariance between combat exposure and self-reported trauma-related sleep disturbance. With years of education covaried, there was a significant indirect effect of combat exposure exerted via wrongdoing on clinician-rated nightmare severity (β = .095, 95% CI [.004, .246]). With wrongdoing in the model, the remaining direct effect of combat exposure on clinician-rated nightmare severity was statistically significant (b = .81, 95% CI: [.05, 1.58]). The indirect effects of wrongdoing accounted for 24% of the covariance between combat exposure and clinician-rated nightmare severity.
4. Discussion
We found that the association of combat exposure with self-reported trauma-related sleep disturbance was partially exerted through its association with perceived wrongdoing, a measure that conceptually overlaps with moral injury. Similarly, we found that the association of combat exposure with clinician-rated nightmare severity was partially exerted through perceived wrongdoing. Results of our analyses suggest the utility of further research on the role of guilt in trauma-related sleep disturbance in military Veterans. Relatively little research has examined the roles of trauma-related cognitions in nightmares among combat Veterans. However, our results are consistent with previous research noting that guilt is among several themes targeted in IRT aimed at reducing nightmare frequency and severity.
It is noteworthy that wrongdoing cognitions specifically, as opposed to guilt-related cognitions generally, played a role in trauma-related sleep disturbance. Models exploring the roles of hindsight bias and lack of justification did not find the statistically significant relationship that was observed when examining perceived wrongdoing. The importance of perceived wrongdoing in our models of trauma-related sleep disturbance in PTSD could inform existing treatments. For example, PTSD symptoms have been significantly reduced in trials of trauma-focused psychotherapies, including Prolonged Exposure (PE) and Cognitive Processing Therapy (CPT; (Forbes et al., 2010; Kline, Cooper, Rytwinski, & Feeny, 2017). Targeting moral injury and perceived wrongdoing might be a good fit for CPT, which has demonstrated reductions in the moral injury measure used in the current study (Resick, Nishith, Weaver, Astin, & Feuer, 2002) as well as self-blame and the resulting guilt (LoSavio, Dillon, & Resick, 2017). Recent literature has provided guidance and case studies to inform treatment of PTSD and related moral injury using CPT and PE in active duty military personnel and military Veterans (Held, Klassen, Brennan, & Zalta, 2017; Wachen et al., 2016). Reductions in negative trauma-related cognitions have been observed at the conclusion of both CPT and PE (Holliday, Link-Malcolm, Morris, & Suris, 2014; Kumpula et al., 2017; Resick, Nishith, Weaver, Astin, & Feuer, 2002). Alternatively, residual sleep disturbance after successful PTSD treatment by trauma-focused psychotherapy could be addressed through supplementation with sleep-focused treatments (Gutner, Casement, Stavitsky Gilbert, & Resick, 2013). One completed trial using sleep-focused hypnosis preceding CPT has found that combined treatment did not augment the outcomes observed in CPT alone (Galovski et al., 2016), but future research will continue to inform the possible utility of combined PTSD and sleep treatment.
Existing treatments for sleep disturbance among people with PTSD have produced more consistent improvements in insomnia, while results for nightmares have been less consistent across studies (Gehrman, Harb, & Ross, 2016). Evidence for a role of perceived wrongdoing in trauma-related sleep disturbance suggests that interventions such as IRT may be improved by initial assessment of moral injury followed by further discussion of relevance to nightmares that underlie trauma-related sleep disturbance (Bryan et al., 2016). In addition to potentially benefiting from focus on cognitions related to perceived wrongdoing in IRT, Veterans with trauma-related sleep disturbance might also benefit from a combination of IRT and cognitive-behavioral therapy for insomnia (Swanson, Favorite, Horin, & Arnedt, 2009).
The conclusions drawn from this study are limited by several study characteristics, including the limited statistical power provided by this relatively small sample. In addition, it is possible that a tendency to experience guilt-related cognitions and trauma-related nightmares preceded war zone exposure and influenced participants’ risk of experiencing and reporting war zone exposure. Findings from the current study on role of perceived wrongdoing could be complemented by future research utilizing measures of the related construct of moral injury (Bryan et al., 2016). Finally, a continuous measure of combat exposure would likely provide meaningful variance to future studies guilt and trauma-related sleep disturbance.
In conclusion, the present results contributed to limited literature on the role of guilt cognition in trauma-related sleep disturbance among Veterans with PTSD. We found a significant role of wrongdoing cognitions in trauma-related sleep disturbance, including nightmares. This has possible implications for prioritization of guilt-related cognitions, including any perceived wrongdoing, in the treatment of sleep symptoms in Veterans with PTSD.
Acknowledgments
This project was supported by Award Number 1IK2CX000718 to Dr. Dedert from the Clinical Sciences Research & Development Service of the VA Office of Research and Development. This work was supported a Senior Research Scientist Award from VA Clinical Sciences Research and Development, Award Number lK6CX001494. Mr. Hicks was supported by the National Institute of Mental Health of the National Institutes of Health grant T32 MH020030. We would like to thank the Veterans who volunteered to participate in this study and help us gain a better understanding of PTSD and smoking cessation among military Veterans. The authors also wish to thank Angela Kirby, Sarah Wilson, and Elizabeth Van Voorhees, who provided therapy as part of the treatment for this study; as well as Vickie Carpenter, who worked as study coordinator; and Michelle Dennis, who provided laboratory management during conduct of the study. The views expressed in this article are those of the author(s) and do not necessarily represent the views of the Department of Veterans Affairs.
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the VA or the United States government. Since the authors are employees of the United States government and contributed to this work as part of their official duties, the work is not subject to U.S. copyright.
Footnotes
Conflict of Interest
The authors have no conflicts of interest to declare.
References
- Aurora RN, Zak RS, Auerbach SH, Casey KR, Chowdhuri S, Karippot A American Academy of Sleep M. Best practice guide for the treatment of nightmare disorder in adults. Journal of Clinical Sleep Medicine. 2010;6(4):389–401. [PMC free article] [PubMed] [Google Scholar]
- Beckham JC, Feldman ME, Kirby AC. Atrocities exposure in Vietnam combat veterans with chronic posttraumatic stress disorder: Relationship to combat exposure, symptom severity, guilt and interpersonal violence. Journal of Traumatic Stress. 1998;11:777–785. doi: 10.1023/A:1024453618638. [DOI] [PubMed] [Google Scholar]
- Bryan CJ, Bryan AO, Anestis MD, Anestis JC, Green BA, Etienne N, Ray-Sannerud B. Measuring Moral Injury: Psychometric Properties of the Moral Injury Events Scale in Two Military Samples. Assessment. 2016;23(5):557–570. doi: 10.1177/1073191115590855. [DOI] [PubMed] [Google Scholar]
- Capaldi VF, 2nd, Guerrero ML, Killgore WD. Sleep disruptions among returning combat veterans from Iraq and Afghanistan. Military Medicine. 2011;176(8):879–888. doi: 10.7205/milmed-d-10-00440. [DOI] [PubMed] [Google Scholar]
- Dennis PA, Dennis NM, Van Voorhees EE, Calhoun PS, Dennis MF, Beckham JC. Moral transgression during the Vietnam War: a path analysis of the psychological impact of veterans' involvement in wartime atrocities. Anxiety, Stress & Coping. 2017;30(2):188–201. doi: 10.1080/10615806.2016.1230669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engdahl BE, Eberly RE, Hurwitz TD, Mahowald MW, Blake J. Sleep in a community sample of elderly war veterans with and without posttraumatic stress disorder. Biological Psychiatry. 2000;47(6):520–525. doi: 10.1016/s0006-3223(99)00201-2. [DOI] [PubMed] [Google Scholar]
- Farnsworth JK, Drescher KD, Nieuwsma JA, Walser RB, Currier JM. The Role of Moral Emotions in Military Trauma: Implications for the Study and Treatment of Moral Injury. Review of General Psychology. 2014;18(4):249–262. doi: 10.1037/gpr0000018. [DOI] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for Axis I DSM-IV Disorders (Version 2nd) New York, NY: Biometrics Research Department; 1994. [Google Scholar]
- Forbes D, Creamer M, Bisson JI, Cohen JA, Crow BE, Foa EB, Ursano RJ. A guide to guidelines for the treatment of PTSD and related conditions. Journal of Traumatic Stress. 2010;23(5):537–552. doi: 10.1002/jts. [DOI] [PubMed] [Google Scholar]
- Galovski TE, Harik JM, Blain LM, Elwood L, Gloth C, Fletcher TD. Augmenting cognitive processing therapy to improve sleep impairment in PTSD: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2016;84(2):167–177. doi: 10.1037/ccp0000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gehrman P, Harb G, Ross R. PTSD and sleep. PTSD Research Quarterly. 2016;27(4):1–9. [Google Scholar]
- Germain A, Hall M, Krakow B, Katherine SM, Buysse DJ. A brief sleep scale for posttraumatic stress disorder: Pittsburgh sleep quality index addendum for PTSD. Journal of Anxiety Disorders. 2005;19:233–234. doi: 10.1016/j.janxdis.2004.02.001. [DOI] [PubMed] [Google Scholar]
- Gilbert P. Evolution, attractiveness, and the emergence of shame and guilt in a self-aware mind: A reflection on Tracy and Robins. Psychological Inquiry. 2004;15(2):132–135. doi: 10.1037/a0021466. [DOI] [Google Scholar]
- Gutner CA, Casement MD, Stavitsky Gilbert K, Resick PA. Change in sleep symptoms across Cognitive Processing Therapy and Prolonged Exposure: a longitudinal perspective. Behaviour Research Therapy. 2013;51(12):817–822. doi: 10.1016/j.brat.2013.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harb GC, Thompson R, Ross RJ, Cook JM. Combat-related PTSD nightmares and imagery rehearsal: nightmare characteristics and relation to treatment outcome. Journal of Traumatic Stress. 2012;25(5):511–518. doi: 10.1002/jts.21748. [DOI] [PubMed] [Google Scholar]
- Hefez A, Metz L, Lavie P. Long-term effects of extreme situational stress on sleep and dreaming. American Journal of Psychiatry. 1987;144(3):344–347. doi: 10.1176/ajp.144.3.344. [DOI] [PubMed] [Google Scholar]
- Held P, Klassen BJ, Brennan MB, Zalta AK. Using prolonged exposure and cognitive processing therapy to treat veterans with moral injury-based PTSD: Two case examples. Cognitive and Behavioral Practice. 2017 doi: 10.1016/j.cbpra.2017.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holliday R, Link-Malcolm J, Morris EE, Suris A. Effects of cognitive processing therapy on PTSD-related negative cognitions in veterans with military sexual trauma. Military Medicine. 2014;179(10):1077–1082. doi: 10.7205/MILMED-D-13-00309. [DOI] [PubMed] [Google Scholar]
- Insana SP, Hall M, Buysse DJ, Germain A. Validation of the Pittsburgh Sleep Quality Index Addendum for posttraumatic stress disorder (PSQI-A) in U.S. male military veterans. Journal of Trauma Stress. 2013;26(2):192–200. doi: 10.1002/jts.21793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline AC, Cooper AA, Rytwinski NK, Feeny NC. Long-term efficacy of psychotherapy for posttraumatic stress disorder: A meta-analysis of randomized controlled trials. Clinical Psychology Review. 2017 doi: 10.1016/j.cpr.2017.10.009. [DOI] [PMC free article] [PubMed]
- Kubany ES, Haynes SN, Abueg FR, Manke FP, Brennan JM, Stahura C. Development and validation of the trauma-related guilt inventory (TRGI) Psychological Assessment. 1996;8(4):428–444. doi: 10.1037//1040-3590.8.4.428. doi: [DOI] [Google Scholar]
- Kubany ES, Haynes SN, Leisen MB, Owens JA, Kaplan AS, Watson SB, Burns K. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The Traumatic Life Events Questionnaire. Psychological Assessment. 2000;12:210–224. doi: 10.1037//1040-3590.12.2.210. [DOI] [PubMed] [Google Scholar]
- Kumpula MJ, Pentel KZ, Foa EB, LeBlanc NJ, Bui E, McSweeney LB, Rauch SA. Temporal Sequencing of Change in Posttraumatic Cognitions and PTSD Symptom Reduction During Prolonged Exposure Therapy. Behavioral Therapy. 2017;48(2):156–165. doi: 10.1016/j.beth.2016.02.008. [DOI] [PubMed] [Google Scholar]
- Lavie P, Hefez A, Halperin G, Enoch D. Long-term effects of traumatic war-related events on sleep. American Journal of Psychiatry. 1979;136(2):175–178. doi: 10.1176/ajp.136.2.175. [DOI] [PubMed] [Google Scholar]
- Litz BT, Stein N, Delaney E, Lebowitz L, Nash WP, Silva C, Maguen S. Moral injury and moral repair in war veterans: A preliminary model and intervention strategy. Clinical Psychology Review. 2009;29(8):695–706. doi: 10.1016/j.cpr.2009.07.003. [DOI] [PubMed] [Google Scholar]
- LoSavio ST, Dillon KH, Resick PA. Cognitive factors in the development, maintenance, and treatment of post-traumatic stress disorder. Current Opinion in Psychology. 2017;14:18–22. doi: 10.1016/j.copsyc.2016.09.006. [DOI] [PubMed] [Google Scholar]
- Mellman T, Kulick-Bell R, Ashlock LE, Nolan B. Sleep events among veterans with combat-related posttraumatic stress disorder. American Journal of Psychiatry. 1995;152:110–115. doi: 10.1176/ajp.152.1.110. [DOI] [PubMed] [Google Scholar]
- Mysliwiec V, Matsangas P, Baxter T, McGraw L, Bothwell NE, Roth BJ. Comorbid insomnia and obstructive sleep apnea in military personnel: correlation with polysomnographic variables. Military Medicine. 2014;179(3):294–300. doi: 10.7205/MILMED-D-13-00396. [DOI] [PubMed] [Google Scholar]
- Raskind MA, Peskind ER, Hoff DJ, Hart KL, Holmes HA, Warren D, McFall ME. A parallel group placebo controlled study of prazosin for trauma nightmares and sleep disturbance in combat veterans with post-traumatic stress disorder. Biological Psychiatry. 2007;61:928–934. doi: 10.1016/j.biopsych.2006.06.032. [DOI] [PubMed] [Google Scholar]
- Raskind MA, Peterson K, Williams T, Hoff DJ, Hart K, Holmes H, Peskind ER. A trial of prazosin for combat trauma PTSD with nightmares in active-duty soldiers returned from Iraq and Afghanistan. American Journal of Psychiatry. 2013;170(9):1003–1010. doi: 10.1176/appi.ajp.2013.12081133. [DOI] [PubMed] [Google Scholar]
- Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA. A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. Journal of Consulting & Clinical Psychology. 2002;70:867–879. doi: 10.1037//0022-006x.70.4.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA. A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. Journal of Consulting & Clinical Psychology. 2002;70:867–879. doi: 10.1037//0022-006x.70.4.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seelig AD, Jacobson IG, Smith B, Hooper TI, Boyko EJ, Gackstetter GD Millennium Cohort Study, T. Sleep patterns before, during, and after deployment to Iraq and Afghanistan. Sleep. 2010;33(12):1615–1622. doi: 10.1093/sleep/33.12.1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein NR, Mills MA, Arditte K, Mendoza C, Borah AM, Resick PA, Consortium SS. A Scheme for Categorizing Traumatic Military Events. Behavior Modification. 2012;36(6):787–807. doi: 10.1177/0145445512446945. [DOI] [PubMed] [Google Scholar]
- Swanson LM, Favorite TK, Horin E, Arnedt JT. A combined group treatment for nightmares and insomnia in combat veterans: a pilot study. Journal of Traumatic Stress. 2009;22(6):639–642. doi: 10.1002/jts.20468. [DOI] [PubMed] [Google Scholar]
- Wachen JS, Dondanville KA, Pruiksma KE, Molino A, Carson CS, Blankenship AE, Consortium SS. Implementing Cognitive Processing Therapy for posttraumatic stress disorder with active duty U.S. military personnel: Special considerations and case examples. Cognitive and Behavioral Practice. 2016;23:133–147. doi: 10.1016/j.cbpra.2015.08.007. [DOI] [Google Scholar]
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, Keane TM. The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) 2013 doi: 10.1037/pas0000486. Interview available from the National Center for PTSD at www.ptsd.gov. [DOI] [PMC free article] [PubMed]
- Weathers FW, Bovin MJ, Lee DJ, Sloan DM, Schnurr PP, Kaloupek DG, Marx BP. The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5): Development and Initial Psychometric Evaluation in Military Veterans. Psychological Assessment. 2017 doi: 10.1037/pas0000486. [DOI] [PMC free article] [PubMed] [Google Scholar]