Abstract
A 17-year-old man initially presented to his primary care physician with throat pain for 1 week and was started on amoxicillin. After four additional days of ongoing pain and difficulty swallowing with decreased oral intake, he presented to the emergency department. Exam showed fullness to the right posterior oropharynx and palpable mass in the right neck without stridor. Initial imaging was soft tissue neck CT with contrast, which showed cystic 8 cm mass in the parapharyngeal space. Patient additionally underwent MRI, which showed an 8.6 cm mass in the right posterior oropharynx with obliteration of the vallecula. Differential diagnosis included abscess; therefore, ear, nose, and throat (ENT) specialist was consulted for possible drainage. Intraoperatively, there was no abscess; alternatively a biopsy was obtained, which was identified by pathology as a ganglioneuroma. Patient was referred to paediatric ENT specialist, underwent extensive resection confirming diagnosis of ganglioneuroma and did well postoperatively.
Keywords: ear, nose and throat/otolaryngology; paediatrics
Background
Neck mass in the paediatric population has a wide differential with common diagnoses including infection or malignancy.1 Ganglioneuroma is a rare finding as it is a benign member of the family of neuroblastic tumours, most of which are malignant.2 Other case reports show significantly longer duration of symptoms, predominantly female patients or much younger or older ages at presentation. This patient reported very brief course of illness, which was initially misleading and makes his case unique, as does his demographics. The extensive bulk of this patient’s parapharyngeal tumour causes resection to be increasingly dangerous as the mass grows due to proximity of vital anatomy. Early recognition and definitive care can help improve outcomes.
Case presentation
This is a 17-year-old fully immunised man who presented with throat pain, difficulty swallowing and right throat mass. He was first seen by his primary care physician as an outpatient where he received oral antibiotics for possible strep throat. Over the next 4 days he had worsening symptoms, and he reported significantly decreased oral intake for 1 week prior to admission secondary to throat pain and trouble swallowing. On exam, he had obvious fullness of the right posterior oropharynx (figure 1) and a palpable mass in the right neck, which was non-tender to palpation. He had no stridor and was tolerating his saliva although he stated swallowing was painful. He was tachycardic with heart rate ranging from 110 to 140 with otherwise normal vital signs. His review of systems was negative except throat pain and dysphagia.
Figure 1.

Intraoral photo demonstrating mass in the right parapharyngeal space.
He has a medical history of well-controlled asthma and anxiety.
His surgical history is remarkable for tonsillectomy approximately 8 years ago.
He denies any use of tobacco, alcohol and illicit substances.
Family history is unremarkable for any childhood cancers, paternal grandfather died from oesophageal cancer at age 58 years and maternal grandfather died from lung cancer at age 58 years.
Investigations
Soft tissue CT neck with contrast remarkable for well-defined cystic mass centred within the right posterior pharynx (figure 2).
Figure 2.
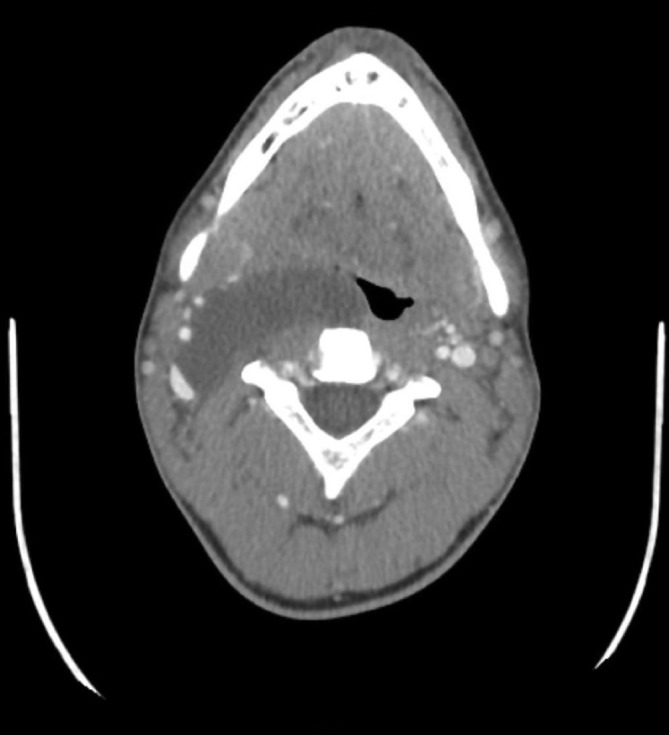
CT soft tissue neck with contrast demonstrates a large right parapharyngeal mass.
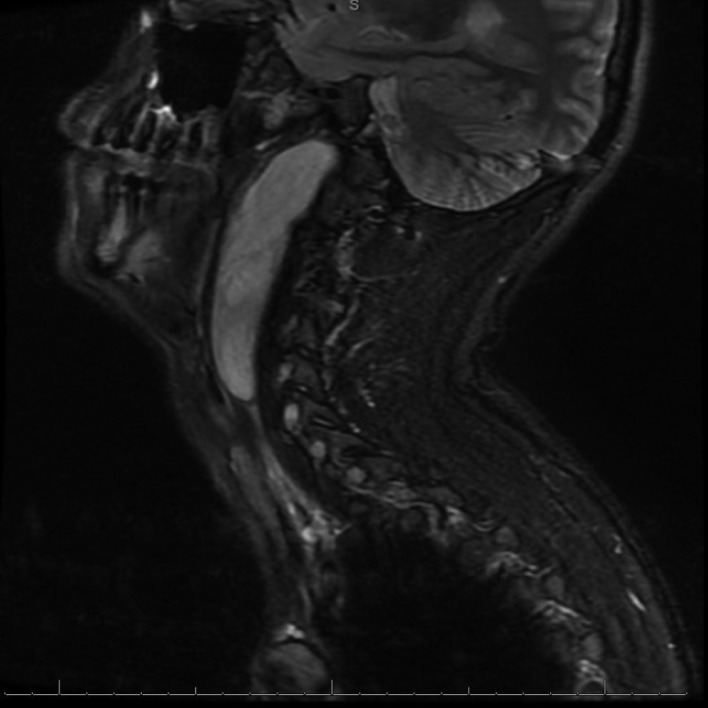
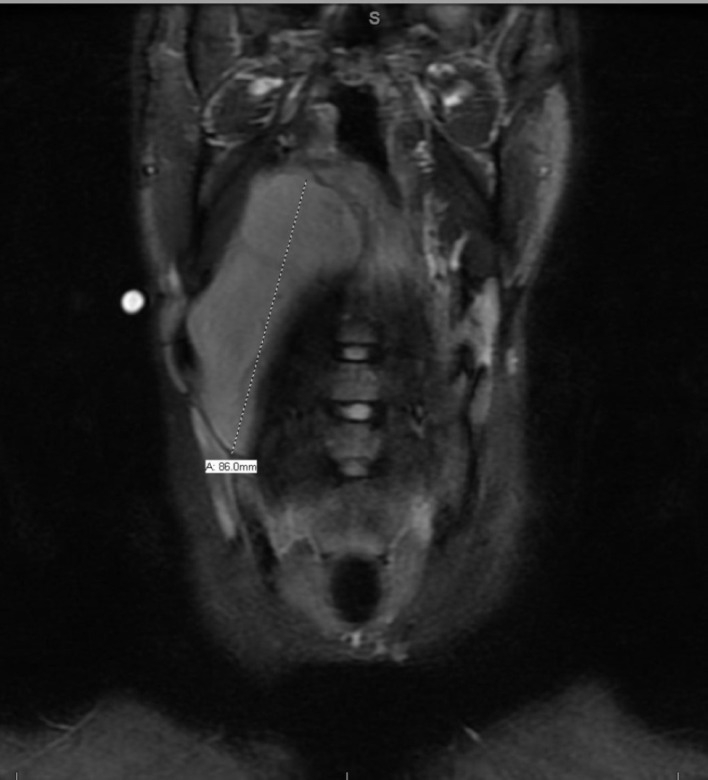
MRI with and without contrast of neck showing large thin-walled non-enhancing mass centred in the posterior right pharynx with maximum diameter 8.6 cm, obliteration of the vallecula, compression of the right parapharyngeal space in sagittal (figure 3) and coronal (figure 4) views.
Figure 3.
MRI with and without contrast of neck demonstrating 8.6 cm mass in the right parapharyngeal space: sagittal view.
Figure 4.
MRI with and without contrast of neck demonstrating 8.6 cm mass in the right parapharyngeal space: coronal view.
Biopsy of parapharyngeal mass showing spindly cells with wavy nuclei in a myxoid background initially stained with H&E at 10× magnification and 40× magnification (figure 5), positive for S-100 immunostain (figure 6). The initial pathology findings were reported as most consistent with a Schwannoma; however, additional slides and staining techniques such as calretinin stain (figure 7) showed further characteristics that were more consistent with ganglioneuroma.
Figure 5.
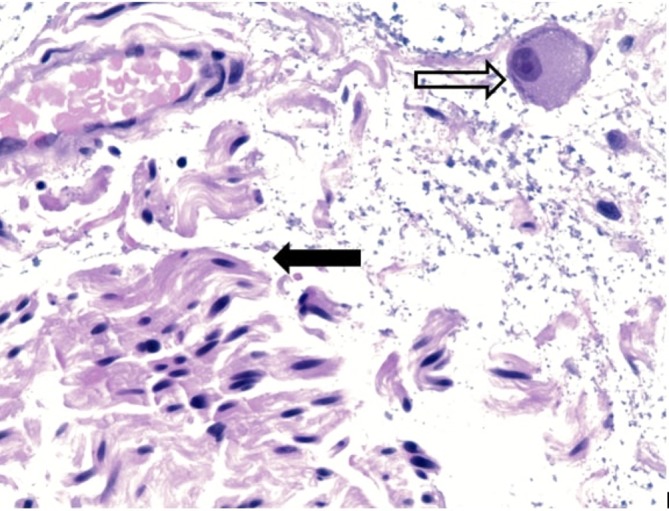
H&E stain original magnification 40×. Higher magnification showing ganglion cell (open arrow) and Schwannoma cells (black arrow).
Figure 6.
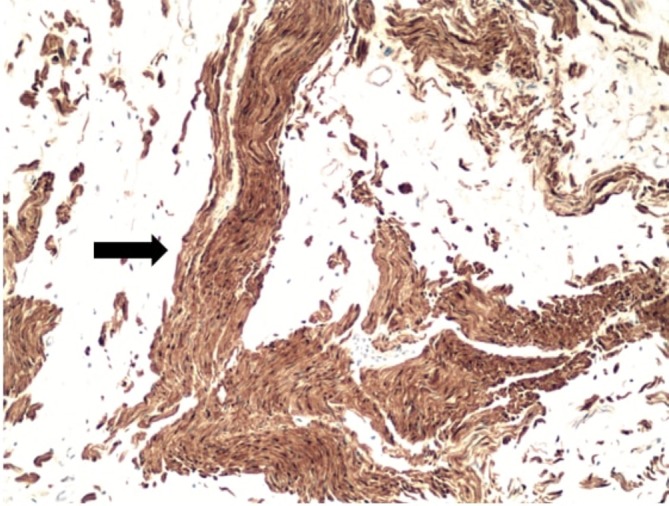
Immunohistochemical stain with S-100 staining the Schwannoma cells at original magnification 10×.
Figure 7.
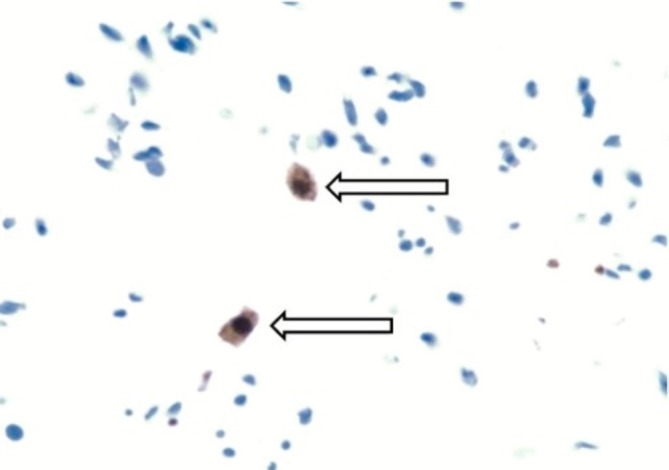
Immunohistochemical stain for calretinin showing positive ganglion cell at 40× original magnification.
Lab work obtained during his initial presentation included complete blood count, basic metabolic panel, and thyroid studies which were all unremarkable. Although there are reports of metabolic studies such catecholamine secretion measuring or radionucleotide metaiodobenzylguanidine scans being used to help differentiate among different types of neuroblastic tumours, our patient did not undergo such studies, and his diagnosis and treatment plan were developed based on his biopsy and histology results.3
Differential diagnosis
Differential diagnosis included retropharyngeal abscess, peritonsillar abscess, branchial cleft cyst and malignancy. The initial differential directed the early treatment options including steroids, antibiotics, and attempted incision and drainage of the mass.
Treatment
As an outpatient, he had been started on amoxicillin for possible strep throat after reporting 1 week of throat pain; however, he had four additional days of worsening dysphagia and pharyngodynia and went to the emergency department. After his evaluation there showed the CT findings as reported above, he was treated with dexamethasone and admitted to the paediatric intensive care unit as there was concern for impending airway compromise. The differential included infection that could have progressed rapidly, and he required close monitoring. Patient was initially started on clindamycin with concern for retropharyngeal abscess, which was discontinued after the attempted incision and drainage. Ibuprofen and benzocaine lozenges were the only therapies that helped his throat pain. He was ultimately discharged to follow up with specialty surgery as an outpatient at another facility. He underwent transoral resection of the mass from the pharyngeal mucosa, transoral repair of pharyngotomy and suprahyoid neck dissection, which all confirmed diagnosis of ganglioneuroma on surgical pathology reports.
Outcome and follow-up
Patient was monitored in the paediatric intensive care unit for 4 days; he had improvement in his ability to tolerate oral intake using topical therapies, acetaminophen and ibuprofen. He maintained a stable airway and never had stridor or dyspnoea during his admission. He was referred for follow-up within 2 days to a paediatric ear nose and throat specialist at a university hospital for definitive care with resection. A few weeks later, he underwent an extensive surgery with transoral and transcutaneous resection of the mass, which confirmed the diagnosis. He did well postoperatively with the exception of persistent pain at the surgical sites. He will be monitored for any recurrence with no additional surgeries or therapies planned at the time of publication.
Discussion
There is a case report of a 2.5-year-old girl with a parapharyngeal space ganglioneuroma; however, her initial symptoms persisted for around 1 year prior to diagnosis.4 Another case was reported of a 5-year-old girl with 4 months of enlarging neck mass who was also treated initially with outpatient antibiotics, although her mass was not causing any symptoms.5 The most similar case report is an 18 year old who had a gradually growing neck mass, which eventually caused obstructive sleep apnoea symptoms.6 One publication outlines 49 patients studied between 1981 and 1999 with proven ganglioneuroma on histology studies, and of these, the median age at diagnosis was 6 years and 7 months, and only one of these patients had any cervical involvement.3
Our patient is unique due to demographics and his presentation as he is older than most of the reported cases and his symptoms were present for less than 2 weeks prior to initial presentation. The cervical location of his tumour also makes his case more rare.
Learning points.
Ganglioneuroma is a rare but benign variant tumour within the family of neuroblastic tumours, of which the intermediate and malignant varieties include ganglioneuroblastoma and neuroblastoma.2
Cervical region accounts for about 8% of ganglioneuromas, with more common sites including mediastinum or retroperitoneum.7
Histological examination will show ganglion cells and Schwann cells.2
Ganglioneuromas typically present with longer duration of symptoms (when mass effect becomes relevant) or as an incidental radiographic finding; however, in this case the history of 10 days of symptoms was misleading.
Definitive treatment includes surgical resection, which can be complicated by proximity to major vessels and airway.
Footnotes
Contributors: JB was responsible for drafting the manuscript, obtaining radiology and clinical photos with descriptions and final editing. QA was responsible for obtaining pathology slides, drafting the slide descriptions and final editing. AS was responsible for drafting pathology slide descriptions and editing the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Meier JD, Grimmer JF. Evaluation and management of neck masses in children. Am Fam Physician 2014;89:353–8. [PubMed] [Google Scholar]
- 2.Longergan GJ, Schwab CM, Suarez ES, et al. From the Archives of the AFIP - Neuroblastoma, Ganglioneuroblastoma, and Ganglioneuroma: Radiologic – Pathologic Correlation. RadioGraphics 2002;22:911–34. [DOI] [PubMed] [Google Scholar]
- 3.Geoerger B, Hero B, Harms D, et al. Metabolic activity and clinical features of primary ganglioneuromas. Cancer 2001;91:1905–13. [DOI] [PubMed] [Google Scholar]
- 4.Kaufman MR, Rhee JS, Fuegelman LJ, et al. Ganglioneuroma of the Parapharyngeal Space in a Pediatric Patient. Otolaryngology-Head and Neck Surgery 2001;124:702–4. 10.1177/019459980112400625 [DOI] [PubMed] [Google Scholar]
- 5.Albuquerque BS, Farias TP, Dias FL, et al. Surgical management of parapharyngeal ganglioneuroma: case report and review of the literature. ORL J Otorhinolaryngol Relat Spec 2013;75:240–4. 10.1159/000353550 [DOI] [PubMed] [Google Scholar]
- 6.Urata S, Yoshida M, Ebihara Y, et al. Surgical management of a giant cervical ganglioneuroma. Auris Nasus Larynx 2013;40:577–80. 10.1016/j.anl.2013.01.005 [DOI] [PubMed] [Google Scholar]
- 7.Rodriguez FJ, Folpe AL, Giannini C, et al. Pathology of peripheral nerve sheath tumors: diagnostic overview and update on selected diagnostic problems. Acta Neuropathol 2012;123:295–319. 10.1007/s00401-012-0954-z [DOI] [PMC free article] [PubMed] [Google Scholar]