Abstract
Background: The Boston Carpal Tunnel Questionnaire (BCTQ) is an easy, brief, self-administered questionnaire developed by Levine et al for the assessment of severity of symptoms and functional status of patients with carpal tunnel syndrome. The aim of our study was to develop and validate the Greek version of BCTQ. Methods: We conducted a cross-sectional study of 90 patients with idiopathic carpal tunnel syndrome. The original English version of BCTQ was adapted into Greek using forward and backward translation. Reliability was assessed by internal consistency (Cronbach α and item-total correlation) and reproducibility. Validity was examined by correlating the Boston Questionnaire scores to Canterbury severity scale for electrodiagnostic severity grading. Results: The Greek version showed high reliability (Cronbach α 0.89 for Symptom Severity Scale and 0.93 for Functional Status Scale) and construct validity (Pearson correlation coefficient 0.53 for Symptom Severity Scale and 0.68 for Functional Status Scale). Test-retest were 0.75 for Symptom Severity Scale and 0.79 for Functional Status Scale (P < .05). Receiver operating characteristic curve analysis showed that the optimal cutoff of Symptom Severity Scale for the discrimination of subjects with low electrodiagnostic severity grading than subjects with high electrodiagnostic severity grading was 1.95 with sensitivity equal to 75.5% and specificity equal to 68.3%. Conclusions: The Greek version of the BCTQ is a valid, reliable screening tool for assessment in daily practice of symptoms and functional status in patients with carpal tunnel syndrome.
Keywords: carpal tunnel syndrome, Boston Carpal Tunnel Questionnaire (BCTQ), Canterbury severity scale, validity, Greek
Introduction
Carpal tunnel syndrome (CTS) is the most common entrapment neuropathy of the upper extremities, causing pain, paresthesia, numbness, and weakness in the territory corresponding to the median nerve.19 The prevalence of CTS is estimated to reach 3% of the general population, with higher rates of incidence among women. Carpal tunnel, median nerve decompression is the most common surgery to be performed on the hand.1,7
Because a gold standard for diagnosis has yet to be established, we cannot exclude the possibility that several scheduled surgical procedures may in effect be unnecessary. In 2002, rigorous electrodiagnostic guidelines were proposed by the American Association of Neuromuscular and Electrodiagnostic Medicine8 in order to: (1) confirm diagnosis (particularly prior to surgery); (2) recognize neurogenic mimickers with impact on response to treatment; and (3) develop a grading of neurogenic injury for making treatment decisions. However, there are clinically diagnosed cases of CTS with normal results in electrophysiological (EM) studies.8 Hence, diagnosis remains a synthesis of clinical history, physical examination, and EM studies. Electrodiagnostic severity of CTS may not be associated with clinical severity. Notwithstanding, both are essential in directing treatment recommendations and evaluating outcomes of treatment for CTS from the patient’s perspective. In that sense, disease-specific instruments may be able to do so.
The Boston Carpal Tunnel Questionnaire (BCTQ) is an easy, brief self-administered tool for assessing symptom severity and functional status in CTS.10 Since its introduction, it has been translated into different languages, with high levels of reliability and validity.2,5,6,11,15,17,18 The BCTQ was found to be significantly more responsive to clinical changes after CTS surgery than the commonly performed strength measures or other generic instruments as the 36-Item Short-Form Health Survey (SF-36).2 The most frequently used region-specific questionnaires for CTS are the Disabilities of the Arm, Shoulder and Hand (DASH) and the Manchester-modified version of the region-specific DASH (M2 DASH). However, the DASH and M2 DASH questionnaires are not as responsive as the BCTQ over the initial postoperative recovery period.3
Validating questionnaires in different languages is very important as in other questionnaires the cutoff values may disagree among different languages or among different dialects of the same language. The Greek version of BCTQ may also respond to the need of Greek-speaking individuals. Today, the Greek language is spoken by over 13 million people in Greece, Cyprus, Italy, Albania, Turkey, and the Greek communities throughout the world.14 Our aim is to develop the Greek version of the BCTQ and evaluate its reliability and validity for this patient population.
Materials and Methods
The Adaptation Process
Two of the authors independently translated the original English version of BCTQ into Greek. The independent translations matched absolutely. Subsequently, a third researcher, blind to the initial process, was given the back-translation into English. The back-translation matched the original version (Supplemental Tables 1 and 2). To remove any comprehension barriers, the final Greek version was tested on 10 volunteer patients to guarantee that participants would define each item as originally intended. The final Greek version of the BCTQ was then evaluated to verify its reliability and validity.
Patients
The final Greek version was administered to 90 consecutive patients referred to the electrophysiology laboratory of Department of Neurophysiology of Aeginition Hospital, University of Athens, with symptoms consistent with CTS, between January 2015 and January 2016. The EM diagnosis of CTS was based on the guidelines of the American Association of Neuromuscular and Electrodiagnostic Medicine.8 We used the Canterbury severity scale for CTS, which expresses the modifications of sensory and motor nerve conduction velocities and amplitudes as a numerical scale for the EM grading of severity from 0 (no abnormality) to 6 (extremely severe CTS).4 For the clinical diagnosis, patients were asked about primary symptoms (paresthesia, needling, and nocturnal symptoms) in the median nerve. If only 1 of these symptoms was reported, at least 2 symptoms such as burning or cold, tightness, pain or discomfort, and swelling were explored. All patients had to meet the following inclusion criteria: (1) age equal to or greater than 18 years; (2) first-time visitors not previously diagnosed by the investigators; and (3) absence of severe intellectual disability or cognitive impairment. Exclusion criteria were as follows: (1) symptoms, or signs of polyneuropathy; (2) systemic diseases potentially associated with polyneuropathy, diabetes mellitus, renal failure, hypothyroidism, or amyloidosis; (3) other diseases that cause hand symptoms, such as cervical radiculopathy, or thoracic outlet syndrome; and (4) pregnancy. All participants gave their informed consent. Subsequently, all subjects successfully completed the BCTQ. In the test-retest study, half of the patients repeated the BCTQ within 1 week. The BCTQ has 2 subscales for the measurement of severity of symptoms and functional status, and emerges as a reliable, valid, and responsive instrument for patients with CTS.10 The Symptom Severity Scale (SSS) subscale includes 11 items assessing pain, paresthesia, numbness, weakness, nocturnal symptoms, and overall functional status. The Functional Status Scale (FSS) subscale includes 8 items assessing hand function during common daily activities. Each item is scored on a 5-point scale, from 1 (no symptoms) to 5 (the worst symptoms) for SSS, and from 1 (no difficulty) to 5 (cannot perform the activity at all) for FSS. The overall SSS and FSS scores are calculated as the mean of the scores for 11 and 8 individual items, respectively. The ethical committee of Aeginition Hospital approved the study.
Statistical Analyses
Scale internal consistency reliability was determined by the calculation of Cronbach α coefficient. Scales with reliabilities equal to or greater than 0.70 were consider acceptable. Validity was further examined with the intercorrelations (Pearson r) of scales and the correlation of scales with EM grading (Spearman r). Correlation coefficients between 0.1 and 0.3 are considered low, between 0.31 and 0.5 moderate, and over 0.5 high. The test-retest results were evaluated with the computation of intraclass correlation coefficients (ICC). Association of scales with sex, hand they use, and EM grading (categorized into 2 categories) were investigated by the use of Student t test. In addition, Pearson correlation coefficients were used to explore the association of scales with years of age. The scales were tested for their ability to discriminate subjects with low EM grading than subjects with high EM grading using receiver operating characteristic (ROC) curves. The overall performance of the ROC analysis was quantified by computing area under the curve (AUC). An area of 1 indicated perfect performance, while 0.5 indicated a performance that was not different than chance. Using ROC analysis was determined the optimal sensitivity and specificity of using various cutoff values for the discrimination of high EM grading. P values reported are 2-tailed. Statistical significance level was set at .05 and analysis was conducted using SPSS 19.0 (SPSS Inc, Chicago, Illinois) statistical software.
Results
Sample Characteristics
Data from 90 subjects (15 men and 75 women) were analyzed. Sample characteristics are presented in Table 1. Total sample mean age was 57.3 (SD = 13.8). The age range was 23 to 88 years. About 12.2% of the participants had a surgery for carpal syndrome. Concerning EM grading, 18.9% were at grade 1, 26.7% were at grade 2, 42.2% were at grade 3, and 12.2% were at grade 4 or more.
Table 1.
Sample Characteristics.
| N (%) | |
|---|---|
| Sex | |
| Male | 15 (16.7) |
| Female | 75 (83.3) |
| Age, mean (SD) | 57.3 (13.8) |
| Occupation | |
| Laborer | 25 (27.8) |
| Office worker | 25 (27.8) |
| Housewife | 22 (24.4) |
| Retired | 17 (18.9) |
| Unemployed | 1 (1.1) |
| Dominant hand | |
| Right | 81 (90) |
| Left | 5 (5.6) |
| Bilateral | 4 (4.4) |
| Injured hand | |
| Right | 52 (57.8) |
| Left | 21 (23.3) |
| Both | 17 (18.9) |
| Injured hand same with the dominant one | |
| No | 17 (18.9) |
| Yes | 73 (81.1) |
| Surgery for carpal syndrome | |
| No | 79 (87.8) |
| Yes | 11 (12.2) |
| Electrophysiological grading | |
| Grade 1 | 17 (18.9) |
| Grade 2 | 24 (26.7) |
| Grade 3 | 38 (42.2) |
| Grade 4/5/6 | 11 (12.2) |
Note. SD = standard deviation.
Internal Consistency and Test-Retest Reliability
Mean values, correlations, and Cronbach α coefficients for scales and items are presented in Table 2. All the scales of Boston Questionnaire exceeded the minimum reliability standard of 0.70. Cronbach α was 0.89 for SSS and 0.93 for FSS. The mean value for SSS was 2.17 (SD = 0.78) and for FSS was 1.95 (SD = 0.86). ICCs concerning test-retest were significant (P <.001) and were 0.75 for SSS and 0.79 for FSS.
Table 2.
Mean Values, Correlations, and Cronbach α Coefficients.
| Mean | SD | Corrected item-total correlation | Cronbach α if item deleted | Cronbach α | |
|---|---|---|---|---|---|
| Symptom Severity Scale | 2.17 | 0.78 | 0.89 | ||
| How severe is the hand or wrist pain that you have at night? | 2.06 | 1.27 | 0.74 | 0.87 | |
| How often did hand or wrist pain wake you up during a typical night in the past 2 weeks? | 1.72 | 1.16 | 0.65 | 0.87 | |
| Do you typically have pain in your hand or wrist during the daytime? | 2.16 | 1.11 | 0.62 | 0.87 | |
| How often do you have hand or wrist pain during daytime? | 2.07 | 1.09 | 0.57 | 0.88 | |
| How long on average does an episode of pain last during the daytime? | 2.07 | 1.12 | 0.55 | 0.88 | |
| Do you have numbness (loss of sensation) in your hand? | 2.82 | 1.15 | 0.66 | 0.87 | |
| Do you have weakness in your hand or wrist? | 2.08 | 1.10 | 0.48 | 0.88 | |
| Do you have tingling sensations in your hand? | 2.71 | 1.16 | 0.52 | 0.88 | |
| How severe is numbness (loss of sensation) or tingling at night? | 2.48 | 1.26 | 0.69 | 0.87 | |
| How often did hand numbness or tingling wake you up during a typical night during the past 2 weeks? | 1.96 | 1.16 | 0.62 | 0.87 | |
| Do you have difficulty with the grasping and use of small objects such as keys or pens? | 1.81 | 0.92 | 0.49 | 0.88 | |
| Functional Status Scale | 1.95 | 0.86 | 0.93 | ||
| On a typical day during the past 2 weeks have hand and wrist symptoms caused you to have any difficulty in writing? | 1.80 | 0.99 | 0.73 | 0.93 | |
| On a typical day during the past 2 weeks have hand and wrist symptoms caused you to have any difficulty in buttoning of clothes? | 1.83 | 1.04 | 0.80 | 0.93 | |
| On a typical day during the past 2 weeks have hand and wrist symptoms caused you to have any difficulty in holding a book while reading? | 2.00 | 1.12 | 0.85 | 0.92 | |
| On a typical day during the past 2 weeks have hand and wrist symptoms caused you to have any difficulty in gripping of a telephone handle? | 1.98 | 1.07 | 0.77 | 0.93 | |
| On a typical day during the past 2 weeks have hand and wrist symptoms caused you to have any difficulty in opening of jars? | 1.97 | 0.97 | 0.74 | 0.93 | |
| On a typical day during the past 2 weeks have hand and wrist symptoms caused you to have any difficulty in household chores? | 2.19 | 1.15 | 0.80 | 0.93 | |
| On a typical day during the past 2 weeks have hand and wrist symptoms caused you to have any difficulty in carrying of grocery bags? | 2.13 | 1.06 | 0.81 | 0.93 | |
| On a typical day during the past 2 weeks have hand and wrist symptoms caused you to have any difficulty in bathing and dressing? | 1.67 | 0.90 | 0.71 | 0.93 |
Note. SD = standard deviation.
Construct Validity
The intercorrelation of Boston Questionnaire scales was significant (P < .001) with correlation coefficient equal to 0.64. Also, SSS and FSS were significantly correlated (P < .001) with EM grading with correlation coefficient equal to 0.53 and 0.68, respectively.
Discriminative Ability by Canterbury Severity Scale (EM Grading)
Table 3 presents association of Boston Questionnaire scales with sex, age, and EM grading categorized into 2 categories (low = 1-2 and high = ≥3). A significantly greater score was found for SSS and FSS in women as compared with men. No significant association with age was found, while significantly greater score on both scales were found in those with EM grading ≥3.
Table 3.
Association of Boston Questionnaire Scales With Sex, Age, and EM Grading.
| Symptom Severity Scale |
P | Functional Status Scale |
P | |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | |||
| Sex | ||||
| Males | 1.65 (0.69) | .004a | 1.32 (0.43) | .002a |
| Females | 2.28 (0.75) | 2.07 (0.88) | ||
| Age, rb | −0.01 | .948 | 0.07 | .539 |
| EM grading | ||||
| 1-2 | 1.83 (0.67) | <.001a | 1.44 (0.65) | <.001a |
| ≥3 | 2.47 (0.74) | 2.37 (0.79) | ||
Note. EM = electrophysiological.
Student t test.
Pearson correlation coefficient.
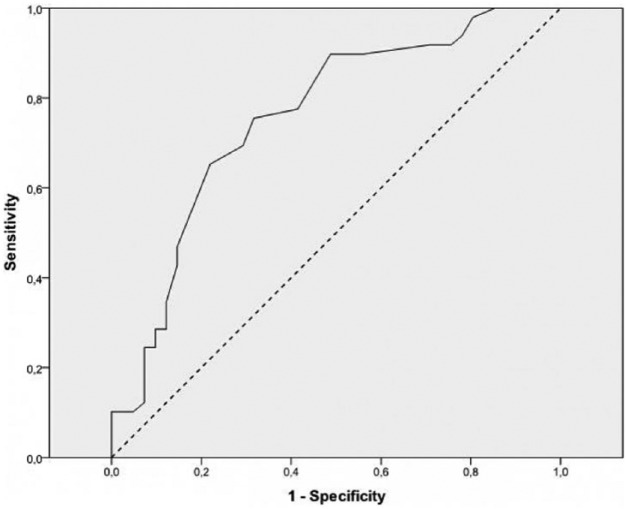
ROC curve analysis showed that the optimal cutoff of SSS for the discrimination of subjects with low EM grading than subjects with high EM grading was 1.95 with sensitivity equal to 75.5% and specificity equal to 68.3% (Figure 1).
Figure 1.
Receiver operating characteristic curve for the prediction of high electrophysiological grading from Symptom Severity Scale.
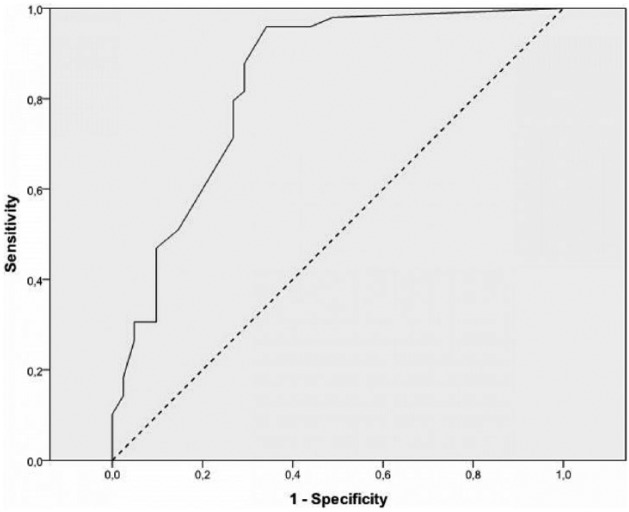
The AUC was 0.76 (SE = 0.05) which significantly differs from 0.5 (P < .001). Also, ROC curve analysis showed that the optimal cutoff of FSS for the discrimination of subjects with low EM grading than subjects with high EM grading was 1.31 with sensitivity equal to 95.9% and specificity equal to 65.9% (Figure 2). The AUC was 0.83 (SE = 0.05) which significantly differs from 0.5 (P < .001).
Figure 2.
Receiver operating characteristic curve for the prediction of high electrophysiological grading from Functional Status Scale.
Discussion
Our study successfully described the Greek translation and cross-cultural adaptation of the BCTQ and provided excellent analyses of the psychometric properties of the translated scale. The results demonstrated that the translated BCTQ has acceptable construct validity while maintaining the factorial structure of the original English version.
The Greek version of the BCTQ has shown a high reliability index expressed through Cronbach α 0.89 (for SSS) and 0.93 (for FSS), comparable to the Spanish version.14 Our results are superior to those of studies in other languages, ranging from 0.81 (for SSS) to 0.87 (for FSS).2,5,6 Furthermore, our test-retest reliability correlations were significant and of a higher order within 1 week with respect to others version. These distinct findings emphasize the importance of analyzing the psychometric properties of the screening questionnaires in different languages in the framework of the linguistic validations.
In previous language versions of BCTQ, the validity of the original version of the Boston Questionnaire was assessed with pinch and grip strength measures with poor to moderate correlations.5,6,15,18 Given the poor cooperation of some patients regarding the usage of the dynamometer, we used the noninvasive method Canterbury severity scale with moderate to high correlation coefficient (r = 0.53 for SSS and 0.68 for FSS). Because there is no agreement in measurement of symptom severity or functional status,9 consensus criteria for standardization in CTS measurement techniques are required; only in this way could further studies be comparable.
With regard to the discriminative ability of the Canterbury severity scale, we found that women had worse scores for symptom severity and functional status compared with men. Other findings, similar to ours, reported higher BQ scores in the surgical and nonsurgical samples.12 A plausible explanation might be that—as in many other syndromes—for a given clinical severity, women with CTS were more sensitive than men in reporting their symptoms.13 Considering also men’s higher tolerance of symptoms, it is possible that the incidence rates of CTS are underestimated in men.16 Even though these sex-related differences were not assessed by previous versions, it is important to consider them when interpreting the BCTQ outcomes.
BCTQ should not be used as an alternative option to clinical, physical, and EM examinations, but as a complementary tool for rapid CTS screening. Other peripheral neuropathies mimicking CTS commonly present in the elderly population; hence, a diagnosis based only on a questionnaire is not recommended.
Using the Greek version of BCTQ with excellent discriminatory properties may simplify daily clinical practice. Given the high rates of undiagnosed cases of CTS,6 such a reliable and easy-to-use disease specific might help in rapid screening.
Limitations
First, the sample was small. Second, we did not follow our patients in order to evaluate clinical changes in CTS.
Conclusions
The Greek BCTQ is a reliable, valid, and responsive disease-specific tool for assessment of symptoms and functional status in patients with CTS.
Supplementary Material
Footnotes
Supplemental material is available in the online version of the article.
Ethical Approval: The ethical committee approved the protocol of the study.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: Informed consent was obtained from all participants, and all procedures were conducted according to the Declaration of Helsinki.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Atroshi I, Gummesson C, Johnsson R, et al. Prevalence of carpal tunnel syndrome in a general population. JAMA. 1999;282:153-158. [DOI] [PubMed] [Google Scholar]
- 2. Atroshi I, Johnsson R, Sprinchorn A. Self-administered outcome instrument in carpal tunnel syndrome reliability, validity and responsiveness evaluated in 102 patients. Acta Orthop Scand. 1998;69:82-88. [DOI] [PubMed] [Google Scholar]
- 3. Bakhsh H, Ibrahim I, Khan WS, et al. Assessment of validity, reliability, responsiveness and bias of three commonly used patient-reported outcome measures in carpal tunnel syndrome. Ortop Traumatol Rehabil. 2012;14(4):335-340. [DOI] [PubMed] [Google Scholar]
- 4. Bland JDP. A neurophysiological grading scale for carpal tunnel syndrome. Muscle Nerve. 2000;23:1280-1283. [DOI] [PubMed] [Google Scholar]
- 5. Correia de, Campos C, Manzano GM, de Andrade LB, et al. [Translation and validation of an instrument for evaluation of severity of symptoms and the functional status in carpal tunnel syndrome] Portuguese. Arq Neuropsiquiatr. 2003;61:51-55. [DOI] [PubMed] [Google Scholar]
- 6. de Krom MC, Knipschild PG, Kester AD, et al. Carpal tunnel syndrome: prevalence in the general population. J Clin Epidemiol. 1992;45(4):373-376. [DOI] [PubMed] [Google Scholar]
- 7. Gelfman R, Melton LJ, III, Yawn BP, et al. Long-term trends in carpal tunnel syndrome. Neurology. 2009;72(1):33-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jablecki CK, Andary MT, Floeter MK, et al. Practice parameter: electrodiagnostic studies in carpal tunnel syndrome. Report of the American association of electrodiagnostic medicine, American academy of neurology, and the American academy of physical medicine and rehabilitation. Neurology. 2002;58:1589-1592. [DOI] [PubMed] [Google Scholar]
- 9. Koran LM. The reliability of clinical methods, data and judgments. N Engl J Med. 1975;293:642-646. [DOI] [PubMed] [Google Scholar]
- 10. Levine DW, Simmons BP, Koris MJ, et al. A self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome. J Bone Joint Surg Am. 1993;75:1585-1592. [DOI] [PubMed] [Google Scholar]
- 11. Lue YJ, Lu YM, Lin GT, et al. Validation of the Chinese version of the Boston Carpal Tunnel Questionnaire. J Occup Rehabil. 2014;24(1):139-145. [DOI] [PubMed] [Google Scholar]
- 12. Mondelli M, Aprile I, Ballerini M, et al. Sex differences in carpal tunnel syndrome: comparison of surgical and non-surgical populations. Eur J Neurol. 2005;12:976-983. [DOI] [PubMed] [Google Scholar]
- 13. Nathan PA, Meadows KD, Doyle LS. Relationship of age and sex to sensory conduction of the median nerve at the carpal tunnel and association of slowed conduction with symptoms. Muscle Nerve. 1988;11:1149-1153. [DOI] [PubMed] [Google Scholar]
- 14. Official languages of the EU—European Commission. Europa: European Union; http://ec.europa.eu/education/official-languages-eu-0_en. Published June 2011. Updated November 25 2016. Accessed February 15 2017. [Google Scholar]
- 15. Otero-Alvaro A, Marín María T, Matas José A, et al. Spanish validation of the Boston Carpal Tunnel Questionnaire. Med Clin (Barc). 2016;146(6):247-253. [DOI] [PubMed] [Google Scholar]
- 16. Padua L, Aprile I, Caliandro P, et al. Is the occurrence of carpal tunnel syndrome in men underestimated? Epidemiology. 2001;12(3):369. [DOI] [PubMed] [Google Scholar]
- 17. Padua R, Padua L, Romanini E, et al. Versione italiana del questionario “Boston Carpal Tunnel”: valutazione preliminare. Giorn Ital Ortop Traumatol. 2000;24:121-129. [Google Scholar]
- 18. Sezqin M, Incel NA, Serhan S, et al. Assessment of symptom severity and functional status in patients with carpal tunnel syndrome: reliability and functionality of the Turkish version of the Boston Questionnaire. Disabil Rehabil. 2006;28(20):1281-1285. [DOI] [PubMed] [Google Scholar]
- 19. Wipperman J, Goerl K. Carpal tunnel syndrome: diagnosis and management. Am Fam Physician. 2016;94(12):993-999. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.