Abstract
Objectives
To describe the case mix, resource use and outcomes for adolescents admitted to intensive care units in the UK.
Methods
Analysis of national prospectively collected data for all adolescents aged 12–19 years admitted to UK adult or paediatric intensive care units.
Results
There were 37,320 admissions of adolescents during the eight–year study period. Excluding elective surgery, respiratory diagnoses were the most common reason for paediatric intensive care unit (PICU) admission, with trauma and intoxication the most common reasons for adult intensive care unit (AICU) admission. Intensive care unit mortality was 6.0% and 5.7% for those admitted to PICUs and AICUs, respectively.
Conclusions
Mortality is similar among adolescents admitted to AICUs and PICUs; however, these rates have not been corrected for severity of acute illness or underlying burden of chronic illness, which may be different between AICUs and PICUs. Services planned for the majority of AICU and PICU patients may not be optimal for critically ill adolescents treated in UK intensive care units, who may need special consideration.
Keywords: Adolescent, critical care, critical illness, intensive care units, paediatric, health planning
Introduction
The transition between childhood and adulthood is a time of rapid physical, psychological and behavioural change. Adolescents (aged 12–19 years) requiring intensive care are very different from both the typical paediatric intensive care unit (PICU) population, comprising mainly infants and pre-school children,1 and the typical adult intensive care unit (AICU) population of much older adults.2 Growing numbers of children with childhood-onset chronic illnesses are surviving into adulthood and as a consequence many more adolescents and young adults may require ICU admission.3
In the UK, since the publication of the Department of Health “Framework for the Future” document in 1997,4 PICU services have been centralised such that critically ill patients aged less than 16 years are cared for in dedicated PICUs, and those 16 years and over in AICUs. However, there is little evidence regarding the most appropriate setting (medically or socially) to care for critically ill adolescents, how best to meet their needs and those of their families or even whether a single age cut off can be used to transition adolescents to adult medical settings.
As the first step in a multicentre mixed-methods research project assessing the care of adolescents requiring intensive care in the UK, we aimed to describe the case mix, resource use and outcomes of adolescents admitted to AICUs and PICUs in the UK.
Methods
Data were extracted from databases held by the two existing national intensive care audit programs used in the UK.
The Case Mix Programme (CMP) is the national clinical audit of adult critical care units in England, Wales and Northern Ireland, coordinated by the Intensive Care National Audit & Research Centre (ICNARC). The CMP database contains pooled case mix and outcome data on consecutive admissions to 212 participating units (93.8% of all adults, general critical care units in England, Wales and Northern Ireland).
The Paediatric Intensive Care Audit Network (PICANet) has provided a prospective national audit of case mix and outcomes for all admissions to PICUs in England and Wales since 2002 and now includes admissions to all PICUs in Scotland, Northern Ireland and the Republic of Ireland.
Data quality for both audits is ensured by local and central validation checks. Collection of personally identifiable data has been approved by the Patient Information Advisory Group (now the NHS Health Research Authority Confidentiality Advisory Group, approval numbers PIAG 2–10(f)/2005 and PIAG 4–07(c)/2002) and ethics approval for PICANet has been granted by the Trent Medical Research Ethics Committee (ref. 05/MRE04/17).
Both databases were searched for adolescents (patients aged 12–19 years) admitted to either paediatric or adult intensive care units over the eight–year period between 1 January 2007 and 31 December 2014.
Analyses were stratified by type of admitting unit (AICU or PICU) and by age range (12–15 years, a cohort normally admitted to PICU, and 16–19 years, a cohort routinely admitted to AICU).
Between-group comparisons were made for diagnostic group at admission, reason for admission (elective or emergency surgery, or non-surgical), length of intensive care stay and intensive care unit mortality.
Categorical data are reported as proportions and continuous data are reported as medians and quartiles. All analyses were performed using Microsoft Excel.
Results
Data from 37,320 intensive care admissions of adolescents aged between 12 and 19 years inclusive were included in the analyses (approximately 4600 per year). Patient characteristics and outcomes are summarised in Tables 1 and 2. There were similar numbers of adolescents admitted to AICU (n = 18,438) and PICU (n = 18,882) but after excluding admissions following elective surgery, more were admitted to AICU than PICU (AICU: 16,830, PICU:10,612).
Table 1.
Admissions of adolescents to intensive care units 2007–2014.
| Age | Age 12–15 | Age 16–19 | |||
|---|---|---|---|---|---|
| Type of unit | PICU | AICU | PICU | AICU | |
| Total number of admissions (number of those admissions later transferred to PICU) | 15,423 | 2137 (501) | 3459 | 16,301 (129) | |
| Admission type n (% of admissions) | Elective surgery | 6413 (41.6) | 241 (14.7) | 1857 (53.7) | 1358 (8.4) |
| Emergency surgery | 923 (6.0) | 247 (15.1) | 182 (5.3) | 2389 (14.8) | |
| Non-surgery | 8059 (52.3) | 1148 (70.2) | 1412 (40.8) | 12,425 (76.8) | |
| Not known | 28 (0.2) | 0 | 8 (0.2) | 0 | |
| Death before ICU discharge (n) | 547 | 78 | 119 | 845 | |
| Mortality (%) | 3.5 | 4.8 | 3.4 | 5.2 | |
AICU: adult intensive care unit; PICU: paediatric intensive care unit.
All data for AICU exclude those adolescents transferred to PICU on discharge from AICU except total number of admissions.
Table 2.
Admissions of adolescents to intensive care units 2007–2014 excluding those admitted for elective surgery.
| Age | Age 12–15 | Age 16-19 | ||
|---|---|---|---|---|
| Type of unit | PICU | AICU | PICU | AICU |
| Total number of admissions (number of those admissions later transferred to PICU) | 9010 | 1891 (496) | 1602 | 14,939 (125) |
| Most common diagnoses (% of admissions in this category) | Respiratory (23.9) Trauma (16.1) Neurological (15.5) Cardiovascular (7.4) | Trauma (24.5) Overdose (20.5) Respiratory (15.5) Neurological (14.4) | Respiratory (31.5) Neurological (14.4) Cardiovascular (9.4) Infection (7.2) | Trauma (25.6) Respiratory (17.5) Overdose (13.2 ) Neurological (12.5) |
| LOS (all) – days median (quartiles) | 1.8 (0.9 – 4.9) | 0.9 (0.5 – 1.8) | 2.0 (0.9 – 5.9) | 1.8 (0.9 – 4.0) |
| LOS (survivors) – days median (quartiles) | 1.8 (0.8 – 4.7) | 0.9 (0.5 – 1.8) | 2.0 (0.8 – 5.4) | 1.8 (0.9 – 3.9) |
| LOS (non-survivors) – days median (quartiles) | 2.8 (0.9 – 8.0) | 1.2 (0.5 – 3.4) | 5.0 (1.6 – 12.9) | 1.8 (0.7 – 4.6) |
| Death before ICU discharge (n) | 525 | 77 | 107 | 840 |
| Mortality (%) | 5.8 | 5.5 | 6.7 | 5.7 |
AICU: adult intensive care unit; PICU: paediatric intensive care unit; LOS: length of stay.
All data for AICU exclude those adolescents transferred to PICU on discharge from AICU except total number of admissions.
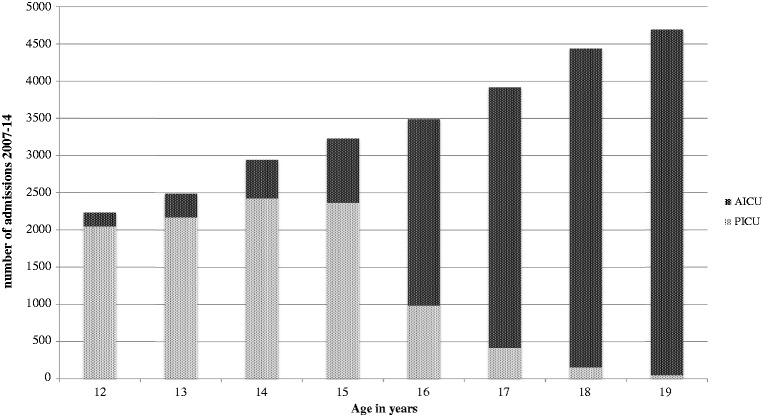
Excluding admissions following elective surgery, 9010/10,901 adolescents (82.7%) aged 12–15 years were treated in a PICU and 14,939/16,541 (90.3%) of those aged 16–19 were treated in AICU. However, these relative proportions do not account for different coverage of the two databases (the sample includes all PICUs in the British Isles but excludes some AICUs) so should be interpreted with caution. The proportion treated in an AICU increased with age, with the greatest increase at the 16th birthday cut-off. Excluding elective surgery, the total number of intensive care admissions increased with increasing age (see Figure 1 and Table 3).
Figure 1.
Number of admissions of adolescents to intensive care units by age, excluding those admitted after elective surgery.
Table 3.
Admissions of adolescents to intensive care units by age excluding elective surgery.
| Age (years) | Admitted to PICU (n) | Admitted to AICU (n) | Total (n) |
|---|---|---|---|
| 12 | 2049 | 186 | 2235 |
| 13 | 2170 | 319 | 2489 |
| 14 | 2424 | 521 | 2945 |
| 15 | 2367 | 865 | 3232 |
| 16 | 985 | 2506 | 3491 |
| 17 | 416 | 3504 | 3920 |
| 18 | 154 | 4282 | 4436 |
| 19 | 47 | 4647 | 4694 |
| Total | 10,612 | 16,830 | 27,442 |
AICU: adult intensive care unit; PICU: paediatric intensive care unit.
Reason for admission
Excluding elective admissions following surgery, but including those later transferred to PICU, the most common reason for adolescent admission to AICU was following trauma, accounting for 25.2% (4243/16,830) of admissions. Poisoning with drugs or alcohol was the cause for 13.5% (2269/16,830) of admissions. Admission diagnostic groups were similar for those AICU admissions aged over and under 16.
One quarter (2661/10,612, 25.1%) of adolescents admitted to PICU had a respiratory diagnostic code while admissions to PICU related to drug or alcohol toxicity were uncommon. In contrast with those treated in AICU, adolescents over 16 in PICU were rarely admitted following trauma.
ICU length of stay
Excluding those admitted for elective surgery, median length of ICU stay was close to 2 days for all groups except 12–15 year olds in AICU, when it was 0.9 days. The length of stay in PICU for non-survivors (3.0 days) was considerably longer than for survivors (1.9 days), but this was not evident among admissions to AICU (1.7 days for both).
Mortality
Excluding elective admissions after surgery, and without adjusting for severity of illness, mortality before unit discharge for both those older and younger than 16 years was similar on PICU (6.0%) and AICU (5.7%).
Discussion
This paper is the first to describe a national picture of the case mix and outcomes of critically ill adolescents admitted to intensive care units. Although the UK policy has been generally to treat those under the age of 16 in PICU and those older in AICU, this practice has only been followed in 87% of cases in this study, with 15 and 16 year olds most likely to be admitted to the “wrong” unit by age criteria. Given that paediatric intensive care is centralised, when clinicians anticipate a short intensive care stay, a nearly adult-sized young person may be more appropriately treated in a local AICU rather than transported to a distant PICU, even if they are not yet 16 years old. Trauma and overdose are more common in the adult population, so physicians in AICU may feel confident managing these patients, even if they are aged less than 16 years (although, with the establishment of Major Trauma Networks,5 children with trauma are now usually managed in hospitals with a PICU). Conversely, it may be felt more appropriate for older adolescents (perhaps with complex needs or learning disabilities) who are still being treated by paediatric teams to receive intensive care in PICU.
Our data suggest that UK clinicians triage adolescents in the way described above; adolescents with “adult” diagnoses are often treated in AICU, and those over 16 treated in PICU commonly have diagnoses requiring tertiary paediatric medical or surgical expertise. The shorter length of stay of 12–15 year olds in AICU may reflect a tendency for adult clinicians to select those adolescents to need a short period of intensive care to be treated locally.6 This includes a significant proportion treated for intoxication or overdose, who are likely recover rapidly. A minority (<4%) are treated briefly in AICU while awaiting transport to PICU, but excluding these patients did not markedly change length of stay or mortality. Those 16–19 year olds who are preferentially managed on PICUs may have more complex underlying problems, which could explain their longer intensive care unit stay.
In this study, we were not able to address the question of whether critically ill adolescents have better outcomes in AICU or PICU as the two databases do not use comparable mortality risk scoring. Three previous studies, restricted to adolescent trauma patients treated in AICU or PICU in the USA, consistently show no difference in mortality but a higher intervention rate in adult centres.7–9 The optimal place of care may also depend on other factors, including age at admission (how far from the age 16 cut-off), co-morbidities, admission diagnosis, and, importantly, the psychological and social suitability of an individual and family for treatment in an adult vs. a paediatric setting.
Critically ill adolescents as a group have previously not been studied specifically. Although they account for over 4600 admissions to intensive care units in the UK annually, this represents a small proportion of total admissions. Any study in the intensive care setting must address age-specific issues in order to ensure that issues relating to the best care for adolescents can be identified. By using comprehensive national datasets we feel confident that our findings are a true reflection of current UK practice; however, this national approach may mask local differences in practice: where distances between units are larger, general intensive care units may more frequently manage younger patients locally. In addition, our data on the absolute numbers admitted to adult and paediatric settings should be interpreted with caution, as our data do not include adolescents admitted to AICUs in Scotland, the Republic of Ireland, and non-participating AICUs elsewhere in the UK.
There is increasing recognition that adolescents need special consideration when planning preventative health-care and access to health services.10 Getting care right for adolescents who are critically ill is at least as important. Having described the group of adolescents receiving intensive care, future studies should aim to identify how our policies and practice can best be adapted to meet the needs of adolescents and their families.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work is supported by a Clinical Research Starter Grant V0015 from the Great Ormond Street Hospital Children's Charity.
References
- 1.UK National Paediatric Intensive Care Audit Network Annual Report 2015, Available from: www.picanet.org.uk/Audit/Annual-Reporting/PICANet_2015_Annual%20Report_Tables_and_Figures_Dec_2015.pdf. Published September 2015, (accessed 28 April 2016).
- 2.Key Statistics from the Case Mix Programme Database 2013–2014. Intensive Care Audit & Research Network, Available from: www.icnarc.org/Our-Audit/Audits/Cmp/Reports/Summary-Statistics, (accessed 28 April 2016).
- 3.Edwards JD, Houtrow AJ, Vasilevskis EE, et al. Multi-institutional profile of adults admitted to pediatric intensive care units. JAMA Pediatr 2013; 167: 436–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.NHS Executive. Paediatric intensive care. “A framework for the future”, London: Department of Health, 1997. [Google Scholar]
- 5.NHS England. NHS Standard Contract for Trauma Service (all ages), Available at: www.england.nhs.uk/wp-content/uploads/2014/04/d15-major-trauma-0414.pdf, (accessed 28 April 28, 2016).
- 6.Ramnarayan P, Patel K, Pappachan J, et al. Characteristics and outcome of children admitted to adult intensive care units in England, Wales and Northern Ireland (1996–2011). Intensive Care Med 2013; 39: 2020–2027. [DOI] [PubMed] [Google Scholar]
- 7.Sanchez JL, Lucas J, Feustel PJ. Outcome of adolescent trauma admitted to an adult surgical intensive care unit versus a pediatric intensive care unit. J Trauma 2001; 51: 478–480. [DOI] [PubMed] [Google Scholar]
- 8.Walther AE, Pritts TA, Falcone RA, et al. Teen trauma without the drama: outcomes of adolescents treated at Ohio adult versus pediatric trauma centers. J Trauma Acute Care Surg 2014; 77: 109–116. [DOI] [PubMed] [Google Scholar]
- 9.Matsushima K1, Schaefer EW, Won EJ, et al. Injured adolescents, not just large children: difference in care and outcome between adult and pediatric trauma centers. Am Surg 2013; 79: 267–273. [PubMed] [Google Scholar]
- 10.Department of Health. You're welcome – Quality criteria for young people friendly health services, Available at: www.gov.uk/government/uploads/system/uploads/attachment_data/file/216350/dh_127632.pdf. Published April 2011, (accessed 28 April 2016).