Abstract
Objective
The primary care (PC) setting provides a unique opportunity to address adolescent alcohol and other drug (AOD) use.
Method
We conducted a randomized controlled trial in four PC clinics from April 2013 to November 2015 to determine whether a 15-minute brief motivational interviewing (MI) AOD intervention, delivered in PC, reduced alcohol and marijuana use and consequences. Adolescents age 12 through 18 that came for an appointment during the 2.5-year study period were asked to be in the study and screened using the NIAAA Screening Guide. Those identified as at-risk were randomized to the intervention, CHAT, or usual care (UC). Adolescents completed four web-based surveys at baseline, 3-, 6- and 12-months post-baseline.
Results
The sample (n=294) was 58% female, 66% Hispanic, 17% Black, 12% white, 5% multiethnic or other, with an average age of 16 years. Compared to UC adolescents, CHAT adolescents reported significantly less perceived peer use of alcohol and marijuana at 3 months (p<0.0001: alcohol; p=.01: marijuana) and 6 months (p=0.04: alcohol; p=0.04: marijuana). CHAT adolescents also reported marginally fewer negative alcohol consequences experienced at 6 months (p=0.08). At 12 months, compared to UC, CHAT adolescents reported less perceived peer alcohol (p =0.04) and marijuana (p <.01) use and fewer negative consequences from alcohol (p =0.03) and marijuana use (p=0.04).
Conclusions
A brief MI intervention delivered in PC reduced negative consequences from alcohol and marijuana use one year later. Findings emphasize that adolescents can benefit from PC interventions that briefly and effectively address both alcohol and marijuana use.
Keywords: Adolescents, primary care, brief motivational intervention, alcohol and marijuana use
Introduction
Alcohol and other drug (AOD) use during adolescence is associated with academic and health problems and a higher likelihood of abuse or dependence in adulthood (Berg et al., 2013; D'Amico, Tucker, et al., 2016; van Gastel et al., 2013). Primary care (PC) settings provide a unique opportunity to address adolescent AOD use through screening and brief intervention, particularly for younger adolescents (Phillips et al., 2014). Despite potential positive effects, rates of both screening and brief interventions for adolescents in medical settings are low (Loheswaran, Soklaridis, Selby, & Le Foll, 2015). Barriers to screening and brief intervention in PC often include provider time constraints, discomfort discussing AOD use, insufficient training, and lack of referral options (Clark & Moss, 2010; Haller et al., 2014; Mitchell, Gryczynski, O'Grady, & Schwartz, 2013; Van Hook et al., 2007). One recent study of 1573 adolescents across four PC clinics found that only 60% of adolescents self-reported being asked by a medical provider in PC about AOD use (screening); of those adolescents that reported being screened, only 37.2% reported receiving any intervention (Meredith et al., 2018). This study cannot address how many adolescents were truly screened and intervened upon by providers given that it is based on self-report. Of note; however, the odds of reported screening/intervention were significantly higher for adolescents with greater AOD risk (Meredith et al., 2018), highlighting that providers are identifying and intervening with adolescents who may be more in need/at-risk.
There have been few randomized controlled trials (RCTs) of screening and brief intervention for adolescents in PC. A 2013 review of screening and brief intervention for adolescent AOD use (Mitchell et al., 2013) found only 8 RCTs that occurred in a medical setting. Seven studies took place in the emergency department (ED), only one study occurred in PC. Six of the ED-based interventions included youth age 12–21; one ED study included teens age 13–17, and the PC study included adolescents age 12–18. Five of the ED studies recruited participants regardless of whether their ED visit was related to drinking (Bernstein et al., 2010; Johnston, Rivara, Droesch, Dunn, & Copass, 2002; Maio et al., 2005; Walton et al., 2010). Two studies included youth regardless of whether they reported any drinking (Johnston et al., 2002; Maio et al., 2005). The PC study (D'Amico, Miles, Stern, & Meredith, 2008) and one ED study (Spirito et al., 2004) screened in adolescents based on being at-risk for drinking or drug use. Most interventions only addressed alcohol use; only two studies addressed marijuana use, and one intervention targeted several behaviors (e.g., seatbelt use, carrying a weapon, heavy drinking).
The majority of these medical setting interventions comprised one individual in-person session ranging from 15 to 60 minutes; one ED intervention also included a one hour videotaped family assessment task in addition to the adolescent session. Some interventions also included a brief 5–10-minute booster call via phone. One ED intervention utilized an interactive computer program (Maio et al., 2005). Several studies reported that intervention delivery utilized motivational interviewing (MI) (Miller & Rollnick, 2012); however, MI fidelity was only reported in some trials. Follow up surveys for these 8 RCTs ranged from 3 to 12 months.
Overall, none of the 8 studies found statistically significant differences in adolescent drinking or heavy drinking at any time point. However, the PC study, with a small sample size (n=42), found a moderate effect size for drinking (Cohen’s d = 0.43) at three month follow up (not significant) (D'Amico et al., 2008). In addition, one ED study that recruited adolescents who either tested positive for blood alcohol or who self-reported drinking just prior to the ED visit found decreased drinking and heavy drinking at the 12-month follow up among the subsample of adolescents reporting more problematic drinking at baseline. They determined problematic drinking by splitting the groups on whether they screened positive for problems on the Adolescent Drinking Inventory (<15) (Spirito et al., 2004). Of the two studies addressing marijuana use, the PC study found decreases in adolescents’ marijuana use at 3-month follow up (D'Amico et al., 2008), and one ED study reported greater reductions in marijuana use and higher rates of abstinence among intervention youth at the one year follow up (Bernstein et al., 2009).
Since 2013, two additional PC-based RCTs were published. One compared a computerized brief intervention (CBI) with an in-person brief intervention, and assessed outcomes for adolescents who reported no substance use and for adolescents who reported substance use at 3, 6 and 12 months. (Walton et al., 2013). They found that the CBI did not reduce the point prevalence of marijuana over the different assessment points for non-using adolescents; however, the cumulative prevalence over 12 months was significantly lower for non-using adolescents in the CBI group as compared to the control. No effects were found for the in-person intervention for non-using adolescents. Among adolescents reporting current marijuana use, there were short term effects on the number of marijuana consequences experienced for the CBI compared to the control group, and a decrease in marijuana DUI in the short term for the in-person intervention compared to the control group. No effects were found for alcohol at any time point, and no effects were found at 12 months on any of the outcomes (Walton et al., 2013). The second study evaluated an intervention for at-risk adolescents focused on reviewing their peer network for risk, such as substance use, influence/offers to use substances, and risky/dangerous activities, and protective behaviors, including support, prosocial activities, and encouragement for healthful behavior. Outcomes were assessed at three and six months (Mason et al., 2015). They found no main intervention effects; however, there was an interaction whereby intervention adolescents who reported more positive networks (e.g., had greater support) were more likely to reduce marijuana use (Mason et al., 2015).
To date, there are only three studies of brief interventions with adolescents in PC; one intervention reduced marijuana use at three months; one found no main effects on alcohol or other drug use; the third found short term effects on marijuana but not alcohol, and no effects at 12 months. One reason for lack of significant findings for brief interventions among adolescents may be due to low levels of AOD use. For example, a 2015 meta-analysis focused on brief alcohol interventions found larger intervention effects for alcohol related problems when adolescents were selected based on their alcohol consumption (Tanner-Smith & Lipsey, 2015).
Given that longer interventions are likely infeasible in PC due to implementation challenges (Ozechowski, Becker, & Hogue, 2016), additional work is needed to better understand whether screening and brief intervention in PC can create long term positive change on adolescent AOD use. Most adolescents see a PC provider at least once a year (CDC/National Center for Health Statistics, 2015), making PC an ideal location to catch potential at-risk adolescents who might otherwise go unnoticed.
The current study builds upon our successful pilot trial (N=42) of a 15-minute brief MI intervention, CHAT, delivered in PC. CHAT was developed based on extensive input from adolescents, parents, and PC providers and staff (Stern, Meredith, Gholson, Gore, & D’Amico, 2007) to ensure it could easily be integrated into a PC appointment and was developmentally appropriate. Specific sociodemographic, social and developmental factors were considered when developing CHAT. CHAT was tested in a PC setting that provided free integrated health care to underserved populations, including the uninsured; the working poor; homeless, runaway, and high-risk youth; and others unable to access affordable health care and human services. Most participants were members of an ethnic minority group; our sample for developing CHAT was 75% Hispanic; the sample in the pilot study was approximately 86% Hispanic and 10% African American. CHAT development emphasized a community-based participatory approach and involved working closely with providers, parents and adolescents to ensure that content was socially and developmentally relevant for this underserved and at-risk population. As part of development, adolescents who received the intervention provided extensive feedback to help develop session content. Some of their themes included: 1) wanting to talk to someone about their AOD use without feeling judged, 2) having the person providing the session be genuine and show he/she cared, 3) confidentiality of information, and 4) wanting strategies to help them make healthier choices and set goals (Stern et al., 2007). CHAT therefore utilized MI, and focused on reducing AOD use and consequences by discussing norms for AOD use, peer AOD use, intentions to use, the pros and cons of use, and willingness and confidence to make changes in use (D'Amico et al., 2008). Brief MI interventions have significant untapped potential to effectively address adolescent AOD use in PC settings (Erickson, Gerstle, & Feldstein, 2007; Williams et al., 2011). They provide an opportunity to engage with teens in a safe setting and help them think about lifestyle choices, such as unhealthy drinking patterns and AOD use, and re-route adolescents towards healthy life choices (D'Amico & Feldstein Ewing, 2016).
In addition to feedback from the community, CHAT content was guided by well-established theories from social psychology, including decision making theory (Kahneman & Tversky, 2000), social learning theory (Bandura, 1977), and self-efficacy theory (Bandura, 1997). For example, when making decisions, adolescents often test out new skills in hypothesis generation and evaluation, which can help them examine situations from different perspectives (D'Amico & Feldstein Ewing, 2016). Thus, content focused on discussing the pros and cons of AOD use and behavior, and among adolescents ready to make a change in AOD behavior, strategies for change. In addition, peer relationships, the behaviors of those around them, and how those behaviors compare with their own become extremely important during adolescence (e.g., Ingersoll & Feldstein Ewing, 2011). Thus, content focused on peer behavior, peer norms, and how behavior and beliefs about peer behavior might influence their own choices. Finally, an important part of successful behavior change is having self-efficacy to make that change. Thus, depending upon each adolescent’s readiness to change, CHAT content addressed how they might change if they were ready to do so, and what that change would look like for them (D'Amico et al., 2008).
In sum, CHAT is one of only three brief interventions available for use in PC settings. It was developed with extensive community input, focuses on underserved and at-risk youth, addresses socially and developmentally relevant content, and can be delivered in 15-minutes. Pilot study results found that adolescents receiving CHAT reported reductions in marijuana use, time spent around peers that used marijuana, perceived prevalence of marijuana use, and intentions to use marijuana compared to control participants at three months. There were no statistically significant effects on alcohol use, likely given the small sample size; however, the effect size for number of days consumed alcohol was moderate (Cohen’s d=.43) (D'Amico et al., 2008).
The current study was based on the pilot and scaled-up to a large randomized controlled trial of CHAT in four PC clinics in Los Angeles and Pittsburgh with a longer follow up period. This study is unique because it 1) focuses exclusively on at-risk adolescents, 2) tests the intervention in different regions of the U.S. with a racially/ethnically diverse sample, and 3) follows these at-risk adolescents over 12 months.
Given CHAT’s focus on AOD cognitions and discussion of peer use, we hypothesized that adolescents who received CHAT would reduce their perceived prevalence of marijuana and alcohol use, report lower intentions to use, and spend less time around peers that use these substances. Further, other intervention work with adolescents has shown that resistance self-efficacy (RSE) typically increases after an intervention (e.g., Robbins, Hong, Engler, & King, 2016; Schwinn, Schinke, Hopkins, Keller, & Liu, 2017; Velasco, Griffin, Botvin, & Corrado Celata and Gruppo LST Lombardia, 2017). We therefore expected RSE to increase among CHAT participants given our focus on planning and preparing for high risk situations. Finally, we expected that adolescents would report decreased use and fewer adverse consequences.
Participants and Methods
Procedures
This study involved four PC clinics (one in Los Angeles; three in Pittsburgh). We obtained a certificate of confidentiality, and all procedures were approved by the institution’s Internal Review Board and each of the four clinics. Every adolescent age 12 through 18 (inclusive) that came for an appointment during the 2.5-year study period (4/13–11/15) was asked to be in the study by survey research group staff (D'Amico, Parast, et al., 2016). Teens and parents were approached while in the clinic waiting room. We obtained parental consent and youth assent (under 18) or consent (18). All materials were provided in English and Spanish, and survey administrators were bilingual. However, youth had to speak English to be in the study. Confidentiality was clearly explained, and as part of the consent process, teens and parents were asked by the survey administrator about the consent process via a checklist to ensure that they understood all aspects of study participation. Adolescents were screened using the NIAAA Screening Guide (SG). Adolescents that screened in as at-risk were randomized to either CHAT or enhanced usual care (both described below). Each adolescent was invited to complete four web surveys: baseline, 3-, 6- and 12-months post-baseline; with the last follow-up completed in January 2017. The survey was written at a 4th grade reading level. Teens completed the baseline survey on the web in a private room in the clinic without their parent present, and with the survey administrator present in case they had questions; they were sent a link via email to complete their 3-, 6- and 12-month follow up surveys. Adolescents randomized to CHAT met the facilitator after they completed their survey and participated in the intervention in a private room without their parent present. Adolescents were paid $25 (baseline), $40 (three month), $50 (six month) and $75 (12 month).
Setting, Participants and Surveys
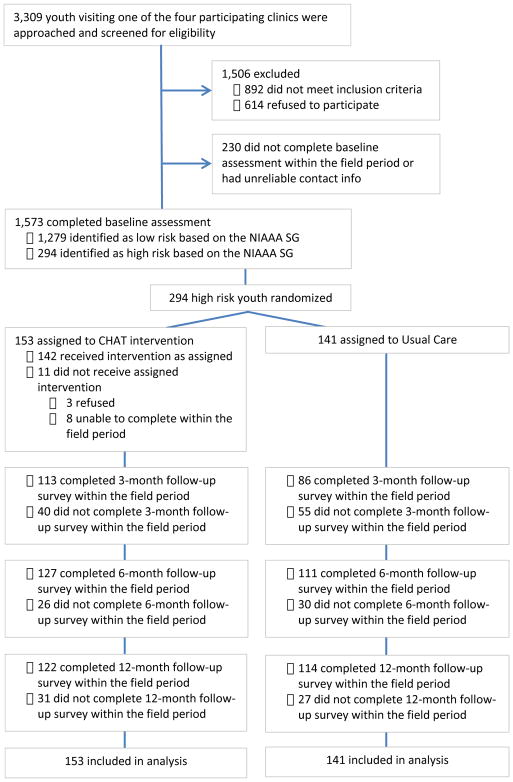
The Pittsburgh and LA area clinics are family-based community health clinics that provide care for ethnically and racially diverse and underserved youth populations. Clinics in both cities serve a high proportion of low-income patients. Approximately 3,309 adolescents were approached to be in the project (see Figure 1 Consort Diagram). Of these adolescents, 27% (n = 892) were ineligible due to age, lack of English language proficiency, being present for an appointment other than their own, or disability status; 18.5% (n = 614) refused to participate, mostly due to time constraints or the teen being at the clinic for family planning (e.g., to obtain birth control) and not wanting their parent(s) to know they were there. This yielded a total sample of 1,803 adolescents who enrolled or provided consent to contact. Of the 1,803 adolescents, 230 did not complete the baseline within the field period or had unreliable contact information. The final enrolled sample included 1,573 adolescents. Screening and baseline surveys were completed in a private clinic space without a parent present. Staff first screened adolescents in person using the NIAAA-SG; adolescents then completed a web-based baseline survey on a laptop. In this paper, we focus on the 294 adolescents identified as at-risk who were part of the randomized controlled trial. These at-risk adolescents were randomized to either usual care (UC) (N=141) or CHAT (N=153); the 1,279 adolescents identified as low-risk were not assigned to any intervention and completed surveys as part of a larger screening study (D'Amico, Parast, et al., 2016). Randomization began with a 1:1 ratio (CHAT:UC) and was implemented by assigning entire days (block randomization) within each clinic to either CHAT or UC. This allocation was adjusted using a random number generator (R Core Team, 2013) over the course of the study to ensure sufficient sample size in each group, given that the number of visits per day fluctuated over time. Initial sample size targets were based on achieving adequate power to detect small-to-medium effects.
Figure 1.
Consort Diagram
Socio-demographic characteristics included age, gender, mother’s education, and race/ethnicity. Mother’s education was categorized as less than high school, high school, some college, college or unknown. Race/ethnicity was categorized as non-Hispanic White, Black, Hispanic, and Other/Multiracial.
NIAAA screening guide (SG) (NIAAA, 2011)
Two screening questions were asked in a different order depending on age: “In the past year, on how many days have you had more than a few sips of beer, wine, or any drink containing alcohol?”, and “Do any of your friends drink alcohol?” Youth age 12–14 were first asked about friend drinking and then self-drinking as a less threatening way to gauge use, whereas youth age 15 and older (and 14 year olds in high school) were first asked about self-drinking and then friend drinking. Adolescents were categorized based solely on the days of use question according to the published NIAAA risk assessment guide, which results in 4 risk categories: no risk, lower risk, moderate risk, and highest risk. For example, youth age 12 to 15 were categorized as moderate risk if they reported 1–5 days of use; adolescents that were 16 years old were categorized as moderate risk if they reported 6–11 days of use (NIAAA, 2011). This screener has been validated for use with adolescents across several studies, and performs well for alcohol related outcomes (Clark et al., 2016; D'Amico, Parast, et al., 2016; Kelly et al., 2014).
Outcomes
Pre-specified outcomes were drinking, heavy drinking, negative alcohol consequences, marijuana use, negative marijuana consequences, perceived peer use (alcohol and marijuana), time spent around peers who use (alcohol and marijuana), and resistance self-efficacy (alcohol and marijuana). We assessed outcomes at 3-, 6-, and 12-months.
Alcohol use, heavy alcohol use, and marijuana use were assessed using well established measures (Ellickson, McCaffrey, Ghosh-Dastidar, & Longshore, 2003; Johnston, O'Malley, Bachman, & Schulenberg, 2013) asking: “During the past [time frame], how many times did you try or use [at least one full drink of alcohol] [drink 5 or more drinks][marijuana]?” At baseline, the time frame was past year; at 3-, 6-, and 12-month follow-up, the time frame was past 3 months. The 6-point frequency response scale (0= “Never” to 5= “More than 20 times”) was rescaled to a pseudo-continuous variable ranging from 0 to 20 using the mid-point of any range as the new value (e.g. 3–10 times was recoded as 6.5 times). We rescaled responses so that the intervention effect estimate could be clinically interpretable in terms of the number of times an adolescent tried or used the substance in the past 3 months. Additionally, to assess maximum quantity of alcohol consumed in the past 30 days, respondents were asked “What is the largest number of drinks that you’ve had on any day in the past 30 days?” at each time point. Responses were capped at 15 drinks. We assessed frequency of marijuana use at each time point by asking “On the days you use marijuana, how many times do you use it?” Response options ranged from “I don’t use marijuana at all” to “3 or more times.” Responses ranged from 0 to 3.
Negative consequences experienced were measured using well-established measures for adolescents (D'Amico, Parast, et al., 2016). Adolescents rated how often they experienced a particular negative consequence in the past year or past three months on a scale from “never” to “20 or more times” using. “Past year” was used at baseline and “past three months” was used at 3-, 6-, and 12-month follow-up. There were six consequences for alcohol (e.g., “doing something they regretted because of drinking”) and four consequences for marijuana (e.g., “had trouble concentrating because of marijuana use”). Items were rescaled to a pseudo-continuous variable ranging from 0 to 20 using the mid-point of any range as the new value (e.g. 3–5 times was recoded as 4 times), and then summed to create a total score indicating the number of negative consequences experienced (alcohol α=0.88; marijuana α=0.88).
Peer influence was assessed by two items of perceived peer use (e.g., how many in a group of 100 students drink alcohol/smoke marijuana at least once a month from 0 to 100) (Pedersen et al., 2013) and two items asking about time spent around peers that use alcohol or marijuana (scored as “Never”=0, “Hardly ever”=1, “Sometimes” =2, “Often”=3) (D'Amico et al., 2008).
Resistance self-efficacy (RSE) (D'Amico et al., 2012) for alcohol and marijuana was defined as the average of four items rated from “I would definitely use” to “I would definitely not use” based on different situations (e.g., if my best friend were using; you were bored at party; your friend gives you a drink). RSE ranged from 1 to 4; higher scores indicated greater RSE (alcohol α=0.92; marijuana α=0.96).
CHAT brief motivational interviewing intervention
Intervention content
CHAT is a 15–20-minute brief MI intervention that first focuses on assessing motivation for change by discussing adolescents’ personal pros and cons of AOD use and determining what their friends think about AOD use and how this might affect their own use. The facilitator then provides normative information for AOD use. Next, adolescents are asked to discuss what they think might happen if they continue to use AOD in the same way. Depending on where adolescents are at in terms of wanting to make changes in their behavior, a discussion follows that addresses willingness and confidence to cut back and/or stop their use. Finally, if the adolescent is willing, he/she discusses a plan to prepare for high risk situations where AOD might be present and how he/she could make a healthy choice in those situations (D'Amico et al., 2008). Facilitators delivered CHAT after adolescents completed their baseline survey.
Fidelity and quality of the CHAT sessions
Across all four clinics over this 2.5-year study, we had 16 different facilitators deliver CHAT. Six had Master’s degrees, and the rest had Bachelor’s degrees. The first author, a member of the Motivational Interviewing Network of Trainers (MINT), trained all facilitators in MI. Each facilitator was subsequently trained on the CHAT protocol through role plays with other project staff, role-playing teens that used alcohol and/or marijuana. When facilitators were confident with the intervention protocol (typically after 4–5 role plays), they conducted a final “check out” role play viewed by both the first and third authors in-person or via Skype, that had to be passed before they could deliver CHAT in the field.
All 153 sessions were digitally recorded and coded for fidelity to CHAT using an adherence checklist (D'Amico, Hunter, Miles, Ewing, & Osilla, 2013). We coded fidelity to MI using the Motivational Interviewing Treatment Integrity scale (MITI) (Moyers, Martin, Manuel, Miller, & Ernst, 2010). Twenty percent of sessions were double coded. Fidelity to the CHAT protocol was 100% across sessions. Supervision was provided weekly by the first and third authors. Average global scores on the MITI for the sessions (evocation, collaboration, autonomy/support, direction, and empathy) were all over 4 (4 is competent), and the percent of complex reflections was 62% (over 50% is competent), indicating facilitators were competent in their delivery of MI.
At the three month follow-up, adolescents reported on their satisfaction with and the quality of the CHAT intervention (Larsen, Atkinson, Hargreaves, & Nguyen, 1979). Adolescents also reported on therapeutic alliance with three items (we worked together to set goals; we respected each other; things we talked about will help me make the changes I want) (Hatcher & Gillaspy, 2006), and on session style (D'Amico et al., 2013) with two items (he/she respected where I was at with my AOD use; he/she valued my opinion). The quality item ranged from 1 (poor) to 4 (excellent); all other items were rated on a 1 to 5 scale from strongly disagree (1) to strongly agree (5). Table 1 shows that 91% of adolescents were satisfied with the CHAT session and 92% thought the quality of the discussion was good or excellent. Eighty-five percent of participants also said that they would recommend this discussion to a friend. Most importantly, 98% of adolescents agreed that the facilitator valued their opinion, and 95% of adolescents indicated that the facilitator respected where they were at with their AOD use and that change was up to them.
Table 1.
Adolescent quality and satisfaction ratings for the CHAT intervention
| % of adolescentsa | |
|---|---|
| Quality | |
| How would you rate the quality of the discussion? | 92% |
|
| |
| Satisfaction | |
| Generally, I am satisfied with the discussion. | 91% |
|
| |
| Therapeutic alliance | |
| We respected each other. | 95% |
| We worked together to set goals. | 72% |
| I feel that the things we talked about will help me make the changes that I want. | 77% |
|
| |
| Session style | |
| I felt that he or she respected where I was at with my AOD use and that change was up to me. | 95% |
| He or she valued my opinion. | 98% |
Note:
For quality, percent reflects adolescents who reported “excellent” or “good”; for satisfaction, therapeutic alliance and session style, percent reflects those who reported “strongly agree” or “agree”.
Overall, MITI scores and adolescents’ ratings clearly emphasize that the session was delivered with fidelity to MI. Adolescents felt respected and listened to during the CHAT intervention, and agreed that during the discussion, it felt like it was their decision whether or not to make changes in their AOD use.
Enhanced Usual Care
To ensure each adolescent received information on AOD use during their PC appointment, adolescents randomized to enhanced usual care (UC) were given a brochure developed by the project team. The brochure included information on the effects of AOD use, how to prepare for risky situations, and online and telephone resources to obtain additional information.
Statistical Analysis
Baseline Differences
We investigated effectiveness of randomization in producing equivalent groups by using two-sample t-tests and chi-squared tests.
Intervention Effect Estimation
To examine intervention effects, we used linear regression models with the outcome value at 3-, 6-, or 12-month follow-up as the dependent variable. We included a CHAT indicator as the primary independent variable, while controlling for the outcome value at baseline. We controlled for standard covariates: age, gender, mother’s education, and race/ethnicity. All models included a fixed effect for site to account for clustering by site. Analyses were performed using intent-to-treat (ITT) (Lachin, 2000) and accounted for missing data due to loss to follow-up and item missingness using multiple imputation. Specifically, 40 imputed datasets were generated using multivariate imputation by chained equations (MICE) using the mi procedure in SAS version 9.4 (Azur, Stuart, Frangakis, & Leaf, 2011; van Buuren & Groothuis-Oudshoorn, 2011; White, Royston, & Wood, 2011). Analyses were performed within each imputed dataset and results were appropriately pooled across datasets (Schafer & Graham, 2002).
Results
Among adolescents assigned to CHAT, 142 received the intervention as intended, 2 refused and 9 did not complete the intervention (Figure 1). Across both conditions, retention was good. Rates of follow up for CHAT were 113 (74%), 127 (83%), and 122 (80%) at 3-, 6- and 12-months, respectively; and for UC, 86 (61%), 111 (79%), and 114 (81%) at 3-, 6- and 12-months, respectively.
Sample information and Baseline Differences
The entire sample was 58% female, 66% Hispanic, 17% Black,12% white, and 5% multiethnic or other, with an average age of 16 years. Overall, 90% of the entire sample reported past year alcohol use, 66% reported heavy drinking, and 77% reported marijuana use. Using DSM-V criteria, 19% of the sample met criteria for an alcohol use disorder (AUD), and 40% met criteria for cannabis use disorder (CUD). Table 2 provides information for all demographic and AOD use variables by group. We did not find any statistically significant differences between groups at baseline. There was one marginal effect whereby the CHAT group had slightly more Black participants compared to UC (p=0.06).
Table 2.
Baseline characteristics stratified by groupa
| CHAT (n=153) | Usual Care (n=141) | P-value | |
|---|---|---|---|
| Mean (SD) or N% | Mean (SD) or % | ||
| Demographics | |||
| Age | 16.16 (1.61) | 15.91 (1.61) | 0.19 |
| Female | 90 (59.6%) | 77 (55.4%) | 0.55 |
| Race | 0.06 | ||
| White | 19 (12.4%) | 15 (10.6%) | |
| Black | 31 (20.3%) | 18 (12.8%) | |
| Hispanic | 99 (64.7%) | 96 (68.1%) | |
| Multi/Other | 4 (2.6%) | 12 (8.5%) | |
| Mom’s education >=Some college | 35 (26.7%) | 30 (25%) | 0.87 |
| Behaviors | |||
| Ever used in lifetime | |||
| Alcohol | 140 (91.5%) | 132 (93.6%) | 0.64 |
| Marijuana | 126 (82.4%) | 116 (82.3%) | 0.99 |
| Past year use (# of times) | |||
| Alcohol | 10.43 (7.93) | 9.46 (7.76) | 0.29 |
| Heavy alcohol | 5.25 (6.23) | 5.51 (7.12) | 0.74 |
| Marijuana | 10.02 (8.51) | 9.51 (8.31) | 0.60 |
| Alcohol max quantity (# drinks) | 3.94 (4.19) | 3.6 (4.46) | 0.50 |
| On days using marijuana, # of times used | 1.54 (1.15) | 1.51 (1.15) | 0.83 |
| Consequences | |||
| Negative consequences (number of consequences experienced) | |||
| Alcohol | 6.59 (14.17) | 7.86 (16.57) | 0.48 |
| Marijuana | 3.58 (10.46) | 4.63 (12.54) | 0.44 |
| Alcohol use disorder | 29 (19.8%) | 24 (17.3%) | 0.57 |
| Cannabis use disorder | 56 (38.6%) | 57 (40.7%) | 0.72 |
| Peer influence and resistance self-efficacy | |||
| Perceived peer use (out of 100 peers) | |||
| Alcohol | 54.38 (26.13) | 53.76 (26.06) | 0.84 |
| Marijuana | 63.92 (27.37) | 65.53 (27.63) | 0.62 |
| Time spent around peers who use (0=never to 3=often) | |||
| Alcohol | 1.93 (0.96) | 1.91 (0.89) | 0.80 |
| Marijuana | 2.07 (0.96) | 2.16 (0.99) | 0.46 |
| Resistance self-efficacy (RSE) (range 1–4b) | |||
| Alcohol | 2.46 (0.91) | 2.46 (0.88) | 0.99 |
| Marijuana | 2.55 (1.12) | 2.57 (1.13) | 0.91 |
| City | 0.37 | ||
| Los Angeles | 100 (65.4%) | 100 (70.9%) | |
| Pittsburgh | 53 (34.6%) | 41 (29.1%) | |
All calculated among non-missing values.
Higher values indicate greater RSE.
Intervention Effect Estimation
Table 3 shows unadjusted mean outcomes at 3 months by group, and results of adjusted regression analyses examining effects of CHAT at 3 months. There were no significant differences at the 3 month assessment in past 3-month alcohol, heavy alcohol or marijuana use or in number of negative consequences experienced. Compared to UC, CHAT participants reported significantly less perceived peer use of alcohol (-15.80, p<0.0001) and marijuana (-8.80, p=.01). There were no significant differences in time spent around peers who use or RSE.
Table 3.
Effect of CHAT on 3-month outcomesa
| CHAT at 3 months Mean (SD) | Usual Care at 3 months Mean (SD) | Coefficient (SE) | CHAT effect b p-value | Effect size | |
|---|---|---|---|---|---|
| Behaviors | |||||
| Past 3 Month Use (# of times) | |||||
| Alcohol | 5.18 (5.59) | 5.64 (5.84) | -0.85 (0.70) | 0.22 | -0.15 |
| Heavy Alcohol | 2.76 (4.56) | 3.04 (4.79) | -0.43 (0.60) | 0.48 | -0.09 |
| Marijuana | 6.38 (8.05) | 5.95 (7.58) | -0.003 (0.95) | 0.99 | 0.00 |
| Alcohol Max Quantity (# drinks) | 3.98 (3.90) | 4.24 (4.25) | -0.42 (0.51) | 0.40 | -0.10 |
| On days using Marijuana, # of times Used Consequences | 1.34 (1.16) | 1.22 (1.10) | 0.10 (0.12) | 0.41 | 0.09 |
| Negative Consequences (Number of consequences experienced) | |||||
| Alcohol | 2.17 (5.05) | 3.39 (9.03) | -1.16 (0.84) | 0.17 | -0.16 |
| Marijuana | 1.67 (5.19) | 1.89 (7.19) | 0.06 (0.71) | 0.93 | 0.01 |
| Peer Influence and Resistance Self-efficacy | |||||
| Perceived Peer Use (out of 100 peers) | |||||
| Alcohol | 45.49 (21.71) | 60.20 (23.63) | -15.80 (2.87) | <0.0001 | -0.70 |
| Marijuana | 53.74 (24.35) | 62.43 (23.62) | -8.80 (3.16) | 0.01 | -0.37 |
| Time Spent Around Peers Who Use (0=Never to 3=Often) | |||||
| Alcohol | 1.79 (0.95) | 1.87 (0.91) | -0.10 (0.11) | 0.37 | -0.11 |
| Marijuana | 2.02 (1.05) | 2.12 (1.01) | -0.06 (0.12) | 0.62 | -0.06 |
| Resistance self-efficacy (RSE) (range 1–4c) | |||||
| Alcohol | 2.54 (0.86) | 2.44 (0.84) | 0.09 (0.10) | 0.37 | 0.11 |
| Marijuana | 2.69 (1.04) | 2.62 (1.06) | 0.06 (0.11) | 0.57 | 0.06 |
All results in table account for missing data using multiple imputation methods;
Regression adjusts for baseline values of all outcomes, race/ethnicity, age, gender, mother’s education, and site;
Higher values indicate greater RSE
Table 4 shows parallel results examining 6-month outcomes. There were no significant differences at the 6 month assessment in past 3-month alcohol, heavy alcohol or marijuana use or in number of negative consequences experienced. Compared to UC, the CHAT group reported less perceived peer alcohol use (-6.37, p=0.04) and marijuana use (-7.71, p=0.04) and marginally fewer negative alcohol consequences experienced (-1.34, p=0.08). There were no significant differences in time spent around peers who use or RSE.
Table 4.
Effect of CHAT on 6-month outcomesa
| CHAT at 6 months | Usual Care at 6 months | CHAT effect b | |||
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Coefficient (SE) | p-value | Effect size | |
| Behaviors | |||||
| Past 3 Month Use (# of times) | |||||
| Alcohol | 4.72 (5.86) | 5.44 (6.45) | -1.20 (0.77) | 0.12 | -0.19 |
| Heavy Alcohol | 2.69 (4.73) | 2.68 (4.66) | -0.08 (0.58) | 0.90 | -0.02 |
| Marijuana | 6.13 (7.90) | 5.07 (6.83) | 0.79 (0.84) | 0.35 | 0.11 |
| Alcohol Max Quantity (# drinks) | 3.64 (3.77) | 4.17 (4.20) | -0.62 (0.49) | 0.21 | -0.16 |
| On days using Marijuana, # of times Used Consequences | 1.14 (1.16) | 1.18 (1.16) | -0.05 (0.13) | 0.73 | -0.04 |
| Negative Consequences (Number of consequences experienced) | |||||
| Alcohol | 2.17 (3.45) | 3.62 (8.54) | -1.34 (0.77) | 0.08 | -0.22 |
| Marijuana | 0.70 (1.54) | 1.46 (5.67) | -0.72 (0.51) | 0.16 | -0.20 |
| Peer Influence and Resistance Self-efficacy | |||||
| Perceived Peer Use (out of 100 peers) | |||||
| Alcohol | 50.25 (20.85) | 55.34 (25.14) | -6.37 (3.16) | 0.04 | -0.28 |
| Marijuana | 56.64 (24.36) | 63.94 (25.73) | -7.71 (3.70) | 0.04 | -0.31 |
| Time Spent Around Peers Who Use (0=Never to 3=Often) | |||||
| Alcohol | 1.82 (1.00) | 1.82 (0.99) | -0.02 (0.12) | 0.84 | -0.02 |
| Marijuana | 2.00 (1.01) | 2.02 (1.02) | 0.02 (0.12) | 0.86 | 0.02 |
| Resistance self-efficacy (RSE) (range 1–4c) | |||||
| Alcohol | 2.48 (0.90) | 2.32 (0.89) | 0.14 (0.11) | 0.21 | 0.16 |
| Marijuana | 2.67 (1.08) | 2.53 (1.11) | 0.14 (0.12) | 0.23 | 0.13 |
All results in table account for missing data using multiple imputation methods;.
Regression adjusts for baseline values of all outcomes, race/ethnicity, age, gender, mother’s education, and site;
Higher values indicate greater RSE
Table 5 shows 12 month outcomes. There were no significant differences at the 12 month assessment in past 3-month alcohol, heavy alcohol or marijuana use. Compared to UC, CHAT participants reported less perceived peer use of alcohol (-6.45. p =0.04) and marijuana (-9.68, p <.01) and fewer negative consequences from both drinking (-2.33, p =0.03) and marijuana use (-1.75, p=0.04). There was a marginal effect whereby CHAT adolescents reported that they spent less time around peers who drank alcohol (-0.21, p =.06). There were no significant differences for RSE.
Table 5.
Effect of CHAT on 12-month outcomesa
| CHAT at 12 months | Usual Care at 12 months | CHAT effect b | |||
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Coefficient (SE) | p-value | Effect size | |
| Behaviors | |||||
| Past 3 Month Use (# of times) | |||||
| Alcohol | 4.54 (5.68) | 5.09 (6.39) | -0.99 (0.70) | 0.15 | -0.16 |
| Heavy Alcohol | 2.44 (4.60) | 2.85 (5.17) | -0.64 (0.59) | 0.28 | -0.13 |
| Marijuana | 6.76 (8.37) | 5.21 (7.35) | 1.08 (0.91) | 0.23 | 0.14 |
| Alcohol Max Quantity (# drinks) | 3.56 (4.15) | 3.50 (4.15) | -0.19 (0.49) | 0.70 | -0.05 |
| On days using Marijuana, # of times Used Consequences | 1.18 (1.20) | 1.06 (1.16) | 0.06 (0.13) | 0.64 | 0.05 |
| Negative Consequences (Number of consequences experienced) | |||||
| Alcohol | 1.99 (4.54) | 4.26 (12.40) | -2.33 (1.10) | 0.03 | -0.28 |
| Marijuana | 0.92 (3.26) | 2.36 (9.29) | -1.75 (0.83) | 0.04 | -0.28 |
| Peer Influence and Resistance Self-efficacy | |||||
| Perceived Peer Use (out of 100 peers) | |||||
| Alcohol | 50.53 (24.23) | 55.88 (26.47) | -6.45 (3.16) | 0.04 | -0.25 |
| Marijuana | 55.11 (25.12) | 64.46 (25.23) | -9.68 (3.27) | <.0.01 | -0.38 |
| Time Spent Around Peers Who Use (0=Never to 3=Often) | |||||
| Alcohol | 1.62 (1.05) | 1.83 (0.94) | -0.21 (0.11) | 0.06 | -0.21 |
| Marijuana | 1.85 (1.11) | 1.98 (1.02) | -0.07 (0.12) | 0.57 | -0.07 |
| Resistance self-efficacy (RSE) (range 1–4c) | |||||
| Alcohol | 2.47 (0.88) | 2.58 (0.90) | -0.07 (0.10) | 0.48 | -0.08 |
| Marijuana | 2.76 (1.13) | 2.69 (1.11) | 0.08 (0.12) | 0.50 | 0.07 |
All results in table account for missing data using multiple imputation methods;
Regression adjusts for baseline values of all outcomes, race/ethnicity, age, gender, mother’s education, and site;
Higher values indicate greater RSE
Discussion
This study examined long term outcomes of a brief MI intervention in PC for a racially/ethnically diverse sample of youth. Adolescents that received CHAT reported lower estimates of peer use for alcohol and marijuana at 3-, 6-, and 12-month follow ups and reduced consequences for both marijuana and alcohol at the 12-month follow up. That we found changes in perceptions of peer use so soon after receiving the intervention is not surprising. CHAT is unique in that cognitive variables are an explicit target of the intervention, and thus, we would expect these cognitions to change before behavior change. For example, adolescents’ opinions about their own individual costs and benefits of AOD use are addressed and their estimates of the number of peers that use (which are routinely higher) are adjusted through collaborative discussion. Actual AOD use is targeted by developing plans for safe or reduced use in the context of these cognitive constructs, adolescents’ personal goals, and their motivation to change their behavior. Given the association between changes in cognitive variables and AOD behavior (Stephens et al., 2009), we would expect behavior change to occur subsequently, and we observed a reduction in both alcohol and marijuana consequences by 12 months. Furthermore, although effects may not persist over time for brief interventions for adolescents generally, Tanner-Smith and Lipsey (2015) note that with high-risk adolescent samples, participants experienced larger beneficial intervention effects on alcohol related consequences. Thus, we may have seen long term effects on consequences given that our sample was at-risk and had more room to improve.
Contrary to our expectations, we did not see a reduction in alcohol or marijuana use for CHAT adolescents. This is not unprecedented as other brief MI interventions have found reductions in consequences for the intervention group with no significant group differences in AOD use, and likened it to the focus of MI on a harm reduction approach (e.g., Monti et al., 1999). Thus, one reason we may have found reductions in consequences but not use could be due to the focus of the session on the pros and cons of use and how to reduce negative experiences. In addition, we may not have found differences in use because our assessment of use had restricted response options that limited our ability to capture smaller and more nuanced changes in adolescents’ alcohol and marijuana use. In contrast, our measure of consequences was more precise and therefore more sensitive to detecting smaller changes. Future work should include smaller response intervals or have youth enter an exact number of times when measuring AOD use to better examine potential change.
Other limitations of this work also need to be considered. First, outcomes were self-reported, which could lead to either under- or overreporting of AOD use. However, the limits of self-report are often exaggerated (Chan, 2008), and recent work with young adults 18–21 has shown that self-reported alcohol use is corroborated by a biochemical measure, transdermal alcohol assessment (Simons, Wills, Emery, & Marks, 2015). In addition, rates of use in the current sample were comparable to national norms (Johnston, O'Malley, Bachman, & Schulenberg, 2012). Third, generalizability may be restricted given that we recruited in PC clinics from two geographic areas. Although we approached every adolescent in the four clinics over a two-and-a-half-year period, and our sample is diverse, our results may not generalize to clinics serving other populations or in other areas in the U.S. Finally, the intervention did not address other potentially relevant sources of drug use norms for adolescents. For example, most study participants were Hispanic, and family norms may have a greater influence than peer norms for teens with this ethnic background (Corbin, Vaughan, & Fromme, 2008). Future research could address this issue when participants are Hispanic.
Clinical implications
Teens that screened into this study were at-risk, as the majority reported alcohol use in the last year (90%), and over two-thirds reported heavy alcohol use (66%) and marijuana use (77%) in the last year. Furthermore, about 1 in 5 (19%) met DSM-V criteria for an AUD, and over one-third (40%) met criteria for CUD. Overall, we found that this 15-minute intervention had long-term positive effects on both alcohol and marijuana consequences for this at-risk sample. Given that many teens report problematic use of both substances (D'Amico, Parast, et al., 2016; Kelly et al., 2014), and that this use can impair functioning across a variety of domains (D'Amico, Tucker, et al., 2016), adolescents can benefit from interventions in PC that briefly and effectively address both alcohol and marijuana use.
CHAT was developed with extensive input from PC providers and staff, and can easily be integrated into a PC appointment given its brevity. Furthermore, adolescents’ ratings of the CHAT intervention highlight that they felt listened to during the discussion and that their opinion was valued. Participants said that they felt respected with where they were at with their AOD use and that any change was up to them. In addition, digital recordings of CHAT sessions suggest that adolescents enjoyed the opportunity to talk about their alcohol and marijuana use, and that many adolescents saw this discussion as a chance to make positive changes.
There are barriers to both screening and brief intervention in PC settings such as time constraints, concerns about confidentiality, and knowing what to do after a positive screen (Committee on Adolescence, 2008; Helitzer, Sussman, Urquieta de Hernandez, & Kong, 2011; Ozechowski et al., 2016). Training can decrease these barriers (Buckelew, Adams, Irwin, Gee, & Ozer, 2008; Committee on Adolescence, 2008; Lustig et al., 2001). Over the course of the study, we trained 16 bachelor and master level people on this protocol, and they were able to implement it with fidelity fairly quickly. We are currently working with the clinics where this study was implemented to train their staff on the CHAT protocol. Given that the majority of adolescents see a PC provider at least once a year (CDC/National Center for Health Statistics, 2015), these visits are a prime opportunity to address adolescents’ AOD use and reach many at-risk youth.
Public Health Significance.
This study suggests that brief motivational intervention in the primary care setting is an effective way to reduce adolescents’ perceptions of alcohol and marijuana use and consequences experienced one year later. Findings emphasize that adolescents can benefit from interventions that briefly and effectively address both alcohol and marijuana use.
Acknowledgments
Work on this article was supported by a grant from the National Institute of Alcohol Abuse and Alcoholism (R01AA021786) to Elizabeth D’Amico.
We would like to thank the four clinics that collaborated with us over the course of the project. We also thank our survey research coordinator, Jennifer Parker, and the survey research group for their hard work recruiting and retaining this sample, and all of the facilitators for implementing CHAT over the course of the project. Work on this project was funded by R01AA021786 (PI D’Amico).
Footnotes
Clinical Trial registry name and registration number: Alcohol Screening in an Ethnically
Diverse Sample of Adolescents in Primary Care; NCT01797835
References
- Azur MJ, Stuart EA, Frangakis C, Leaf PJ. Multiple imputation by chained equations: What is it and how does it work? International Journal of Methods in Psychiatric Research. 2011;20(1):40–49. doi: 10.1002/mpr.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Social learning theory. Englewood Cliffs, NJ: Prentice Hall; 1977. [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. New York, NY: Freeman; 1997. [Google Scholar]
- Berg Noora, Kiviruusu Olli, Karvonen Sakari, Kestilä Laura, Lintonen Tomi, Rahkonen Ossi, Huurre Taina. A 26-year follow-up study of heavy drinking trajectories from adolescence to mid-adulthood and adult disadvantage. Alcohol and Alcoholism. 2013;48(4):452–457. doi: 10.1093/alcalc/agt026. [DOI] [PubMed] [Google Scholar]
- Bernstein E, Edwards E, Dorfman D, Heeren T, Bliss C, Bernstein J. Screening and brief intervention to reduce marijuana use among youth and young adults in a pediatric emergency department. Academic Emergency Medicine. 2009;16:1174–1185. doi: 10.1111/j.1553-2712.2009.00490.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein J, Heeren T, Edward E, Dorfman D, Bliss C, Winter M, Bernstein E. A brief motivational interview in a pediatric emergency department, plus 10-day telephone follow-up,increases attempts to quit drinking among youth and young adults who screen positive for problematic drinking. Academic Emergency Medicine. 2010;17(8):890–902. doi: 10.1111/j.1553-2712.2010.00818.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckelew SM, Adams SH, Irwin CE, Jr, Gee S, Ozer EM. Increasing clinician self-efficacy for screening and counseling adolescents for risky health behaviors: Results of an intervention. Journal of Adolescent health. 2008;43(2):198–200. doi: 10.1016/j.jadohealth.2008.01.018. [DOI] [PubMed] [Google Scholar]
- CDC/National Center for Health Statistics. Summary Health Statistics: National Health Interview Survey, 2015 (Vol. Table C-8a) Center for Disease Control and Prevention; 2015. https://www.cdc.gov/nchs/fastats/physician-visits.htm. [Google Scholar]
- Chan D. So why ask me? Are self-report data really that bad? In: Lance CE, Vandenberg RJ, editors. Statistical and methodological myths and urban legends: Doctrine, verity and fable in the organizational and social sciences. New York: Psychology Press; 2008. pp. 309–336. [Google Scholar]
- Clark DB, Moss HB. Providing alcohol-related screening and brief interventions to adolescents through health care systems: Obstacles and solutions. PLoS Medicine. 2010;7(3):e1000214. doi: 10.1371/journal.pmed.1000214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark Duncan B, Martin Christopher S, Chung Tammy, Gordan Adam J, Fiorentino Lisa, Tootell Mason, Rubio Doris M. Screening for underage drinking and Diagnostic and Statistical Manual of mental disorders, 5th edition alcohol use disorder in rural primary care practice. The Journal of Pediatrics. 2016;173:214–200. doi: 10.1016/j.jpeds.2016.02.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Committee on Adolescence. Achieving quality health services for adolescents. Pediatrics. 2008;121(6):1263–1270. doi: 10.1542/peds.2008-0694. [DOI] [PubMed] [Google Scholar]
- Corbin William R, Vaughan Ellen L, Fromme Kim. Ethnic differences and the closing of the sex gap in alcohol use among college-bound students. Psychology of Addictive Behaviors. 2008;22(2):240–248. doi: 10.1037/0893-164X.22.2.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Amico EJ, Feldstein Ewing SW. The Oxford Handbook of Adolescent Substance Abuse. New York: Oxford University Press; 2016. Prevention in school, primary care, and community based settings. [Google Scholar]
- D'Amico EJ, Hunter SB, Miles JNV, Ewing BA, Osilla KC. A randomized controlled trial of a group motivational interviewing intervention for adolescents with a first time alcohol or drug offense. Journal of Substance Abuse Treatment. 2013;45(5):400–408. doi: 10.1016/j.jsat.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Amico EJ, Miles JNV, Stern SA, Meredith LS. Brief motivational interviewing for teens at risk of substance use consequences: A randomized pilot study in a primary care clinic. Journal of Substance Abuse Treatment. 2008;35:53–61. doi: 10.1016/j.jsat.2007.08.008. [DOI] [PubMed] [Google Scholar]
- D'Amico EJ, Parast L, Meredith LS, Ewing BA, Shadel WG, Stein BS. Screening in primary care: What is the best way to identify at-risk youth for substance use? Pediatrics. 2016;138:1–9. doi: 10.1542/peds.2016-1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Amico EJ, Tucker JS, Miles JNV, Ewing BA, Shih RA, Pedersen ER. Alcohol and marijuana use trajectories in a diverse longitudinal sample of adolescents: Examining use patterns from age 11 to 17. Addiction. 2016;111(10):1825–1835. doi: 10.1111/add.13442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Amico EJ, Tucker JS, Miles JNV, Zhou AJ, Shih RA, Green HD., Jr Preventing alcohol use with a voluntary after school program for middle school students: Results from a cluster randomized controlled trial of CHOICE. Prevention Science. 2012;13(4):415–425. doi: 10.1007/s11121-011-0269-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellickson PL, McCaffrey DF, Ghosh-Dastidar B, Longshore DL. New inroads in preventing adolescent drug use: Results from a large-scale trial of Project ALERT in middle schools. American Journal of Public Health. 2003;93:1830–1836. doi: 10.2105/ajph.93.11.1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erickson SJ, Gerstle M, Feldstein SW. Brief interventions and motivational interviewing with children, adolescents, and their parents in pediatric health care settings: A review. Archives of Pediatric Medicine. 2007;159:1173–1180. doi: 10.1001/archpedi.159.12.1173. [DOI] [PubMed] [Google Scholar]
- Haller DM, Meynard A, Lefebvre D, Ukoumunne OC, Narring F, Broers B. Effectiveness of training family physicians to deliver a brief intervention to address excessive substance use among young patients: A cluster randomized controlled trial. Canadian Medical Association Journal. 2014;186(8):E263–E272. doi: 10.1503/cmaj.131301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatcher RL, Gillaspy JA. Development and validation of a revised short version of the Working Alliance Inventory. Psychotherapy Research. 2006;16(1):12–25. [Google Scholar]
- Helitzer Deborah L, Sussman Andrew L, de Hernandez Urquieta, Brisa, Kong Alberta S. The 'ins' and 'outs' of provider-parent communication: Perspectives from adolescent primary care providers on challenges to forging alliances to reduce adolescent risk. Journal of Adolescent Health. 2011;48(4):404–409. doi: 10.1016/j.jadohealth.2010.07.020. [DOI] [PubMed] [Google Scholar]
- Ingersoll K, Feldstein Ewing SW. Adolescent and young adult substance use and risk taking. In: Johnson BA, editor. Addiction Medicine: Science and Practice. Vol. 2. New York, NY: Springer Press; 2011. pp. 1329–1344. [Google Scholar]
- Johnston BD, Rivara FP, Droesch RM, Dunn C, Copass MK. Behavior change counseling in the emergency department to reduce injury risk: a randomized, controlled trial. Pediatrics. 2002;110(2 Pt 1):267–274. doi: 10.1542/peds.110.2.267. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national results on adolescent drug use: Overview of key findings, 2011. Ann Arbor, Michigan: Institute for Social Research, The University of Michigan; 2012. [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use, 1975–2012. Volume I: Secondary school students. Ann Arbor, Michigan: Institute for Social Research, The University of Michigan; 2013. [Google Scholar]
- Kahneman D, Tversky A. Choices, values, and frames. New York: Cambridge University Press; 2000. [Google Scholar]
- Kelly SM, Gryszynski J, Mitchell SG, Kirk A, O'Grady KE, Schwartz RP. Validity of brief screening instrument for adolescent tobacco, alcohol and drug use. Pediatrics. 2014;133(5):249–257. doi: 10.1542/peds.2013-2346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachin JM. Statistical considerations in the intent-to-treat principle. Controlled clinical trials. 2000;21(3):167–189. doi: 10.1016/s0197-2456(00)00046-5. [DOI] [PubMed] [Google Scholar]
- Larsen DL, Atkinson CC, Hargreaves WA, Nguyen TD. Assessment of client/patient satisfaction: Development of a general scale. Evaluation and Program Planning. 1979;2:197–207. doi: 10.1016/0149-7189(79)90094-6. [DOI] [PubMed] [Google Scholar]
- Loheswaran G, Soklaridis S, Selby P, Le Foll B. Screening and treatment for alcohol, tobacco and opioid use disorders: A survey of family physicians across Ontario. PloS One. 2015;10(4):e0124402. doi: 10.1371/journal.pone.0124402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lustig JL, Ozer EM, Adams SH, Wibbelsman CJ, Fuster CD, Bonar RW, Irwin CE. Improving the delivery of adolescent preventive services through skills based training. Pediatrics. 2001;107:1100–1107. doi: 10.1542/peds.107.5.1100. [DOI] [PubMed] [Google Scholar]
- Maio RF, Shope JT, Blow FC, Gregor MA, Zakrajsek JS, Weber JE, Nypaver MM. A randomized controlled trial of an emergency department-based interactive computer program to prevent alcohol misuse among injured adolescents. Annals of Emergency Medicine. 2005;45(4):420–429. doi: 10.1016/j.annemergmed.2004.10.013. S0196064404015525 [pii] [DOI] [PubMed] [Google Scholar]
- Mason M, Light J, Campbell L, Keyser-Marcus L, Crewe S, Way T, … McHenry BA. Peer network counseling with urban adolescents: A randomized controlled trial with moderate substance users. Journal of Substance Abuse Treatment. 2015;58:16–24. doi: 10.1016/j.jsat.2015.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meredith LS, Ewing BA, Stein BS, Shadel WG, Brooks Holliday S, Parast L, D'Amico EJ. Influence of mental health and alcohol or other drug use risk on adolescent reported care received in primary care settings. BMC Family Practice. 2018;19(1):10. doi: 10.1186/s12875-017-0689-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Helping people change. 3. New York: Guilford Press; 2012. [Google Scholar]
- Mitchell SG, Gryczynski J, O'Grady KE, Schwartz RP. SBIRT for adolescent drug and alcohol use: Current status and future directions. Journal of Substance Abuse Treatment. 2013;44(5):463–472. doi: 10.1016/j.jsat.2012.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monti PM, Colby SM, Barnett NP, Spirito A, Rohsenow DJ, Myers M, … Lewander W. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. Journal of Consulting and Clinical Psychology. 1999;67:989–994. doi: 10.1037//0022-006x.67.6.989. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin T, Manuel JK, Miller WR, Ernst D. Revised Global Scales:Motivational Interviewing Treatment Integrity 3.1.1 (MITI 3.1.1) 2010 http://casaa.unm.edu/mimanuals.html.
- NIAAA. Alcohol screening and brief intervention for youth: A practioners guide. Rockville, MD: NIAAA, DHHS and AAP; 2011. NIH Publication No. 11-7805. [Google Scholar]
- Ozechowski Timothy J, Becker Sara J, Hogue Aaron. Sbirt-a: Adapting sbirt to maximize developmental fit for adolescents in primary care. Journal of Substance Abuse Treatment. 2016;62:28–37. doi: 10.1016/j.jsat.2015.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen ER, Miles JNV, Ewing BA, Tucker JS, Shih RA, D'Amico EJ. A longitudinal examination of alcohol, marijuana, and cigarette perceived norms among middle school adolescents. Drug and Alcohol Dependence. 2013;133(2):647–653. doi: 10.1016/j.drugalcdep.2013.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips NL, Milne B, Silsbury C, Zappia P, Zehetner A, Klineberg E, … Steinbeck K. Addressing adolescent substance use in a paediatric health-care setting. Journal of Paediatrics and Child Health. 2014;50(9):726–731. doi: 10.1111/jpc.12622. [DOI] [PubMed] [Google Scholar]
- R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2013. [Google Scholar]
- Robbins Rockey, Hong Ji, Engler Caroline, King Callie. A study of the effectiveness of the Gifts of the Seven Directions Alcohol Prevention Model for Native Americans: Culturally sustaining education for Native American adolescents. Contemporary Educational Psychology. 2016;47:24–31. [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Schwinn Traci M, Schinke Steven P, Hopkins Jessica, Keller Bryan, Liu Xiang. An online drug abuse prevention program for adolescent girls: Posttest and 1-year outcomes. Journal of Youth and Adolescence. 2017 doi: 10.1007/s10964-10017-10714-10964. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons JS, Wills TA, Emery NN, Marks RM. Quantifying alcohol consumption: Self-report, transdermal assessment, and prediction of dependence symptoms. Addictive Behaviors. 2015;50:205–212. doi: 10.1016/j.addbeh.2015.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spirito A, Monti Peter M, Barnett Nancy P, Colby Suzanne M, Sindelar Holly, Rohsenow Damaris, … Myers M. A randomized clinical trial of a brief motivational intervention for alcohol-positive adolescents treated in an emergency department. Journal of Pediatrics. 2004;145:396–402. doi: 10.1016/j.jpeds.2004.04.057. [DOI] [PubMed] [Google Scholar]
- Stephens PC, Sloboda Z, Stephens RC, Teasdale B, Grey SF, Hawthorne RD, Williams J. Universal school-based substance abuse prevention programs: Modeling targeted mediators and outcomes for adolescent cigarette, alcohol and marijuana use. Drug and Alcohol Dependence. 2009;102(103):19–29. doi: 10.1016/j.drugalcdep.2008.12.016. [DOI] [PubMed] [Google Scholar]
- Stern SA, Meredith LS, Gholson J, Gore P, D’Amico EJ. Project CHAT: A brief motivational substance abuse intervention for teens in primary care. Journal of Substance Abuse Treatment. 2007;32:153–165. doi: 10.1016/j.jsat.2006.07.009. [DOI] [PubMed] [Google Scholar]
- Tanner-Smith EE, Lipsey MW. Brief alcohol interventions for adolescents and young adults: A systematic review and meta-analysis. Journal of Substance Abuse Treatment. 2015;51:1–18. doi: 10.1016/j.jsat.2014.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate imputation by chained equations in R. Journal of Statistical Software. 2011;45(3) [Google Scholar]
- van Gastel WA, Tempelaar W, Bun C, Schubart CD, Kahn RS, Plevier C. Cannabis use as an indicator of risk for mental health problems in adolescents: A population-based study at secondary schools. Psychological Medicine. 2013;43(9):1849–1856. doi: 10.1017/S0033291712002723. [DOI] [PubMed] [Google Scholar]
- Van Hook S, Harris SK, Brooks T, Carey P, Kossack R, Kulig J, Knight JR. The "Six T's": Barriers to screening teens for substance abuse in primary care. Journal of Adolescent Health. 2007;40:456–461. doi: 10.1016/j.jadohealth.2006.12.007. [DOI] [PubMed] [Google Scholar]
- Velasco Veronica, Griffin Kenneth W, Botvin Gilbert J, Celata Corrado, Lombardia Gruppo LST. Preventing adolescent substance use through an evidence-based program: Effects of the Italian adaptation of life skills training. Prevention Science. 2017;18(4):394–405. doi: 10.1007/s11121-017-0776-2. [DOI] [PubMed] [Google Scholar]
- Walton MA, Bohnert K, Resko S, Barry KL, Chermack ST, Zucker RA, … Blow FC. Computer and therapist based brief interventions among cannabis-using adolescents presenting to primary care: One year outcomes. Drug and Alcohol Dependence. 2013;646–653(132):3. doi: 10.1016/j.drugalcdep.2013.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton Maureen A, Chermack Stephen T, Shope Jean T, Bingham C Raymond, Zimmerman Marc A, Blow Frederic C, Cunningham Rebecca M. Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: A randomized controlled trial. JAMA: Journal of the American Medical Association. 2010;304(5):527–535. doi: 10.1001/jama.2010.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Statistics in Medicine. 2011;30(4):377–399. doi: 10.1002/sim.4067. [DOI] [PubMed] [Google Scholar]
- Williams EC, Johnson ML, Lapham GT, Caleiro RM, Chew L, Fletcher GS, … Bradley KA. Strategies to implement alcohol screening and brief intervention in primary care settings: A structured literature review. Psychology of Addictive Behaviors. 2011;25(2):206–214. doi: 10.1037/a0022102. [DOI] [PubMed] [Google Scholar]