Abstract
[Purpose] This study aimed to investigate the effects of McKenzie exercise, Kinesio taping, and myofascial release (MFR) on forward head posture (FHP). [Participants and Methods] Twenty-eight individuals with an FHP were enrolled. participants were randomly assigned to one of three groups: Group A, Group B and Group C. Group A underwent McKenzie exercise and MFR. Group B underwent McKenzie exercise and Kinesio taping. Group C underwent McKenzie exercise, MFR, and Kinesio taping. Interventions for all three groups were provided three times per week for four weeks. The acromion and tragus of ear (A-T length), craniovertebral angle (CVA), Cranial rotation angle (CRA), and neck disability index (NDI) were measured. [Results] The A-T length significantly differed after intervention in all three groups. CVA only significantly differed after intervention in group C. All three groups showed an increase in CRA after intervention; however, these increases were not statistically significant. [Conclusion] Considering these results, these three types of exercise may be recommended as effective exercises to improve posture in adults with FHP.
Key words: Forward head posture, Kinesio taping, Myofacial release
INTRODUCTION
Excessive use of smartphones and display devices in modern societies have generated a variety of problems1, 2), one of which is forward head posture (FHP), recognized as an excessive extension between the atlanto-occipital joint and superior cervical spine and elevated flexion between the inferior cervical spine and superior chest3). Cho et al.4) showed that individuals with persistent FHP had elevated fatigue of the neck muscles compared to that of normal people5). Quek et al.6) reported that FHP increases retroversion of the thoracic spine while reducing range of motion in the cervical spinal area6).
The McKenzie exercise encourages self-care treatment through repeated exercises and focuses on extension, including ROM exercise, manipulation, and patient education7). In a study on men and women with FMP in their 20s, Kim8) reported that McKenzie exercises significantly ameliorated the cervical posture of people with FHP.
Myofascial release (MFR) is widely used to control pain associated with musculoskeletal lesions, and its series of therapeutic effects are maximized by relaxing muscles at the lesion as much as possible9). Furthermore, MFR is generally the physical therapy of choice to stimulate blood circulation for patients with cervical pain10).
Kinesio taping is a type of natural therapy that involves the use of a non-medicated adhesive tape on human muscles for pain control purposes. It utilizes the homeostatic properties of muscles to improve symptoms and control pain, as an application of the Kinesio tape normalizes reduced muscle strength, spasms, and tension while facilitating blood, tissue fluid, and lymphatic circulation11).With elasticity and increased tension, Kinesio taping may also provide mechanical effects by inhibiting the FHP12).
Although changes of the FHP because of McKenzie exercises, MFR, and Kinesio taping have been extensively studied in the literature, hardly any studies compared the efficacies of the three techniques combined.
Therefore, this study aimed to compare the efficacy of these three interventions on adults with a FHP.
PARTICIPANTS AND METHODS
Twenty-eight undergraduate students of K University who had a FHP were enrolled in this study. Only students who voluntarily provided informed consent were enrolled. The present study was conducted with the approval from the Institutional Review Board of Department of Physical Therapy at Kangwon National University. Group A underwent the McKenzie exercise and MFR. Group B underwent the McKenzie exercise and Kinesio taping, and group C underwent McKenzie exercise, MFR, and Kinesio taping. None of the three groups underwent any other preservative treatment.
The inclusion and exclusion criteria were as follows. 1) Inclusion criteria: (1) The center of the ears is positioned more than 2.5 cm anterior to the center of the shoulders. (2) Neck disability index (NDI) of 14 or lower. (3) No cervical fracture. (4) No history of surgery within three months. (5) No vascular diseases. (6) No psychiatric problems that would hinder the comprehension of the survey content. 2) Exclusion criteria: (1) Bone fracture. (2) Neuromyopathy. (3) Inflammatory disease. (4) History of disc surgery.
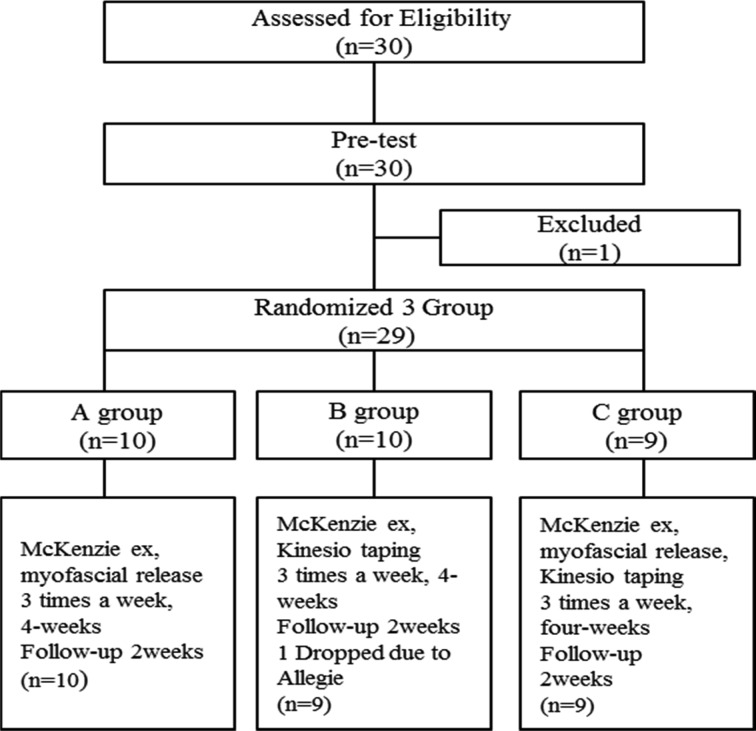
Twenty-nine out of the initial 30 candidates who provided an informed consent were determined to be eligible and enrolled in the study (Fig. 1). The pre-test was carried out three to five days prior to the experiment, and the post-test was carried out on the day of study completion via the same method.
Fig. 1.
Frame of study.
All interventions were administered three times a week for four weeks. We measured the distance between the acromion and tragus of the ear (A-T length), craniovertebral angle (CVA), cranial rotation angle (CRA), and Neck disability index (NDI).
For each motion, participants in McKenzie exercise group maintained peak isometric force for seven seconds for a total of 15 reps, and took a break after completing the motion (Table 1).
Table 1. McKenzie exercise program.
| Exercise program |
| 1. Retraction for neck from sitting position |
| 2. Extension for neck from sitting position |
| 3. Lateral bending in head |
| 4. Rotation in head |
| 5. Flexion for neck from sitting position |
| 6. Chin tuck neck from supine position |
| 7. Extension for neck from supine position |
Myofascial release group was performed using a lacrosse ball. Three sets of 15 reps were performed for each muscle. Upper trapezius, neck extensor, and levator scapulae releases were performed in the prone position, while pectoralis major and pectoralis minor muscle releases were performed in the supine position. The therapist stood on the side of the patient and used a lacrosse ball to perform myofascial release from the origin to insertion of muscles. Each session comprised three sets of fifteen rounds, and the same was performed on the opposite side.
In Kinesiology taping group, two elastic I tapes were used (5 cm wide, 11 cm long). Intervention was performed three times a week, and participants were instructed to leave the tape for eight hours after each intervention. Taping was applied with the participants sitting on a chair with a neutral position and gazing forward. The tape was applied in a V shape around the C7–T1 junction.
A lacrosse ball and Kinesio tape were used for this study, and measurements were taken with a tape measure. The horizontal distance between the center of the ear and center of the shoulder (AT length), CVA, CRA, and NDI were measured. 1) Changes of A-T length: To measure posture, participants were photographed from 1 m away at the same location after placing a sticker on the acromion. The distance between the central line of the external auditory canal and a vertical line through the acromion was measured. 2) Changes of CRA and CVA: Participants were instructed to maintain a natural head posture and relax their arms next to their trunk. Photographs were taken with a digital camera from a position 60-cm away from the participants after placing stickers on the center of the acromion and external auditory canal. After marking the C7, external auditory canal, and lateral angle of eye, the angle formed by a line connecting these points was defined as the CRA. The angle formed by external auditory canal and C7 and a horizontal line passing through C7 was defined as the CVA.
The NDI questionnaire is used to assess neck functional disability and neck pain, and is the most effective means for self-assessment of neck pain13). Lee et al.14) established the reliability and validity of the Korean version of the questionnaire, which consists of ten items. Each item is rated on a six-point scale (0–5 points), and the maximum score is 50 points for the entire questionnaire. A higher score reflects a more severe neck functional disability. A total score of 0–4 indicates no disability, 5–14 a mild disability, 15–24 a moderate disability, and 25–34 a complete disability.
Data were analyzed using SPSS ver. 19.0 for Windows. participants’ general characteristics were analyzed with descriptive statistics, and intergroup differences were analyzed with repeated measures ANOVA. Statistical significance was set at p<0.05.
RESULTS
The general characteristics of the participants are as follows (Table 2). A total of 28 participants were enrolled, 15 of whom were men and 13 of whom were women. Pre-intervention homogeneity among groups A, B, and C was confirmed, as there were no significant differences among the groups. With regard to changes in the changes of A-T length, groups A (p<0.00), B (p<0.00), and C (p<0.01) showed significant changes of A-T length after a six-week intervention period (p<0.05) (Table 3). Regarding changes in the CVA, groups A and B showed changes of CVA, but not to a statistically significant extent; group C showed a significant change of CVA after a six-week intervention (p<0.05) (Table 3). All three groups showed changes of CRA after a six-week intervention, but not to a statistically significant extent (Table 3).
Table 2. General characteristics of participants.
| A group (n=10) | B group (n=9) | C group (n=9) | |
| Gender (M/F) | 7/3 | 4/5 | 4/5 |
| Age (yrs) | 21.6 ± 1.6 | 21.3 ± 2.1 | 20.3 ± 1.5 |
| Weight (kg) | 69.9 ± 18.3 | 59.1 ± 7.8 | 68.4 ± 11.7 |
| Height (cm) | 169.8 ± 6.3 | 170.2 ± 10.8 | 169.2 ± 7.9 |
M ± SD: Mean ± standard deviation.
A group: McKenzie exercise and myofascial release.
B group: McKenzie exercise and Kinesio taping.
C group: McKenzie exercise, myofascial release and Kinesio taping.
Table 3. Comparison according to the period in A-T length, CVA and CRA (unit: cm).
| A-T length | CVA | CRA | ||
| M ± SD | M ± SD | M ± SD | ||
| A group | Pre-test | 8.4 ± 1.8 | 52.8 ± 7.7 | 141.5 ± 9.3 |
| Post-test | 4.5 ± 1.5* | 57.0 ± 2.7 | 142.8 ± 5.7 | |
| B group | Pre-test | 6.8 ± 2.6 | 55.6 ± 3.9 | 139.8 ± 6.7 |
| Post-test | 2.8 ± 1.5* | 58.5 ± 3.8 | 143.2 ± 5.6 | |
| C group | Pre-test | 8.3 ± 4.3 | 50.6 ± 5.2 | 141.4 ± 8.5 |
| Post-test | 3.6 ± 2.6* | 56.4 ± 3.9* | 143.7 ± 5.5 | |
M ± SD: Mean ± Standard Deviation. *p<0.05.
CVA: craniovertebral angle; CRA: cranial rotation angle; A-T length: acromion-tragus length.
A group: McKenzie exercise and myofascial release.
B group: McKenzie exercise and Kinesio taping.
C group: McKenzie exercise, myofascial release and Kinesio taping.
DISCUSSION
FHP, characterized by an excessive anterior protrusion of the neck, is quite prevalent in modern society due to driving and the prolonged use of smartphones and computers. According to Jang15), prolonged muscular stress in the head and cervical spine results in muscular spasms with localized pain in the trapezius and suboccipital muscles.
Myofascial release16), which is an advanced stretching technique to promote maximum relaxation of tense tissues, is widely used in mainly controlling pain from musculoskeletal lesions like myofascial trigger points and myofibrosis and maximizes a therapeutic effect by relaxing muscles of related lesions17).
Kinesio taping is a natural therapy11) to provide a mechanical effect for inhibiting forward head posture with extended and increased tension18) and to control pain by normalizing reduced muscle strength, muscle cramps and tension, and balancing muscles, based on the muscle homeostasis principle11).
Therefore, this study aimed to investigate the effects of three types of intervention (McKenzie exercise, myofascial release, Kinesio taping; three times a week for four weeks) in 28 individuals with a FHP.
Our findings showed that A-T length changed from 8.41 cm before intervention to 4.51 cm after intervention in group A, 6.87 cm before intervention to 2.66 cm after intervention in group B, and 8.34 cm before intervention to 3.53 cm after intervention in group C. All three groups showed significant changes in A-T length after the intervention (p<0.05). These results are in line with the results of Kwon18), where the experimental group with neck pain and control group significantly differed in their neck posture.
All three groups showed increases of CVA after the intervention. Groups A and B showed clinical elevation of CVA, but not to statistically significant degrees. On the other hand, group C showed a significant change of CVA after the intervention (p<0.05). Kim8) and Jeong19) confirmed that McKenzie exercise increases CVA in patients with a FHP. It has been said that the increase in CVA led to the relaxation of forward head posture and the reduction in pain and NDI20). It has also been said that the reason why NDI in forward head posture patients decreased was because the reduction in muscle imbalance around the neck and the surrounding tissues led to the relaxation of forward head posture and the reduction of loads on the surrounding muscles of the neck and joints and eventually, this reduced neck pain21).
Furthermore, according to Jeong19) study on the effects of McKenzie exercise on functional recovery and FHP in patients with chronic neck pain, McKenzie exercise led to significant changes of CVA and NDI, but a statistically insignificant increase of CRA, which are in line with our findings. McKenzie exercise, Kinesio taping, and MFR improved participants’ FHP, and the effects were significantly greater on the group that underwent all three interventions. This result suggests that applying all three interventions would be more effective on FHP than applying any one of the interventions.
The limitations of this study are as follows. First, it is difficult to generalize our findings due to the small sample size and the study population, which was limited to undergraduate college students. Second, it is possible that the therapeutic effects were not fully evident due to a short intervention period. Third, we had difficulty controlling the potential variables that may have affected the outcome. Thus, we suggest a future study that includes a larger population with a longer intervention period. Our findings showed that all three types of interventions improved FHP, but applying all three interventions was the most effective to improve FHP.
Funding
This study was supported by 2015 Research Grant from Kangwon National University (No. 201510106).
Conflict of interest
None.
REFERENCES
- 1.Szeto GP, Lee R: An ergonomic evaluation comparing desktop, notebook, and subnotebook computers. Arch Phys Med Rehabil, 2002, 83: 527–532. [DOI] [PubMed] [Google Scholar]
- 2.Janwantanakul P, Sitthipornvorakul E, Paksaichol A: Risk factors for the onset of nonspecific low back pain in office workers: a systematic review of prospective cohort studies. J Manipulative Physiol Ther, 2012, 35: 568–577. [DOI] [PubMed] [Google Scholar]
- 3.Hanten WP, Olson SL, Russell JL, et al. : Total head excursion and resting head posture: normal and patient comparisons. Arch Phys Med Rehabil, 2000, 81: 62–66. [DOI] [PubMed] [Google Scholar]
- 4.Cho WH, Lee WY, Choi HK: An investigation on the biomechanical effects of turtle neck syndrome through EMG analysis. KSPE, 2008, 1: 195–196. [Google Scholar]
- 5.Shin DC: The effects of a deep cervical flexion exercise on neck-shoulder pain, muscle strengthening, and cervical alignment in sedentary workers. Graduate School, Sahmyook University, 2008. [Google Scholar]
- 6.Quek J, Pua YH, Clark RA, et al. : Effects of thoracic kyphosis and forward head posture on cervical range of motion in older adults. Man Ther, 2013, 18: 65–71. [DOI] [PubMed] [Google Scholar]
- 7.McKenzie RA: Treat your own neck. Lower Hutt: Spinal Publication, 1983. [Google Scholar]
- 8.Kim SY: The effect of Mckenzie exercise on forward head posture and respiratory function. Department of Physical Therapy, Graduate School, Catholic University of Pusan, 2014. [Google Scholar]
- 9.John RJ, Wright V: Relative importance of various tissues in joint stiffness. J Physiol, 1962, 17: 824–828. [Google Scholar]
- 10.Park YK, Hyun SW, Seo HK: The effectiveness of joint mobilization and myofascial release on the neck. Journal of Korean Academy of Orthopaedic Manual Therapy, 2009, 15: 69–79. [Google Scholar]
- 11.Go DI: Easy kinesio taping therapy. Seoul: Pureunsol, 2000. [Google Scholar]
- 12.Yoo WG: Effect of the Neck Retraction Taping (NRT) on forward head posture and the upper trapezius muscle during computer work. J Phys Ther Sci, 2013, 25: 581–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Song KJ, Choi BW, Kim SJ, et al.: Cross-cultural adaptation and validation of the Korean version of the neck disability index. Journal of Korean Academy of Orthopaedic Manual Therapy, 2009, 44: 350–359. [Google Scholar]
- 14.Lee EW: Reliability and validity of the neck disability index in neck pain patients. Korean Res Soc Phys Ther, 2007, 14: 97–106. [Google Scholar]
- 15.Jang JW: The effects of sling exercise and Mckenzie exercise on forward head posture. Graduate School, Sahmyook University, 2017. [Google Scholar]
- 16.Jeon JG: The approch to myofascial release for plantarfascitis of foot. J Korean Academy of Orthopaedic Manual Therapy, 2003, 9: 93–95. [Google Scholar]
- 17.Seo HG, Gong WT, Lee SY: The effect of myofacial release and transcutaneous electrical nerve stimulation on the range of motion and pain in patient with chronic cervical neck pain. Journal Korean Academy Orthopaedic Manual Therapy, 2005, 11: 1–12. [Google Scholar]
- 18.Yoo WG: Effect of the neck retraction taping on forward head posture and the upper trapezius muscle during computer work. J Phys Ther Sci, 2013, 25: 581–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kwon MH: A comparing of strength and cervical posture between people with and without cervical pain. Graduate School, Dankook University, 2004. [Google Scholar]
- 20.Jeong YW: Effects of Mckenzie exercise on the functional recovery and forward head posture of chronic neck pain patients. J Korean Soc Phys Med, 2006, 1: 93–108. [Google Scholar]
- 21.Yoon HK: The effect of push up plus exercise in sling by forward head posture muscle activity and function of lung. Dongshin University. Master’s Thesis, 2016.