Abstract
Background:
Sagittal imbalance is known as the main radiographic driver of disability in adult spinal deformity (ASD). In this study, the association of radiological spinopelvic parameters and clinical outcomes was evaluated following the corrective surgery of sagittal imbalance, in order to explore the predictive ability of each parameter.
Methods:
A total of 23 patients, who underwent corrective osteotomy for restoration of sagittal balance, were included in this study. The mean follow-up period of the patients was 15.5±2.1, ranging from 12 to 18 months. Pre- and postoperative radiological parameters including pelvic tilt (PT), sagittal vertical axis (SVA) and pelvic incidence minus lumbar lordosis (PI-LL) were assessed for each patient. Clinical outcomes were evaluated using Oswestry disability Index (ODI).
Results:
The mean ODI improved 32% following the corrective osteotomy of sagittal imbalance. Postoperative ODI was significantly correlated with all preoperative radiological parameters (r=0.608, P=0.002 for PI-LL; r=0.483, P=0.01 for PT; and r=0.464, P=0.02 for SVA). ODI improvement was significantly correlated with PI-LL and SVA change (r=536, P=0.008 and r=416, P=0.04, respectively), but not with PT change (r=247, P=0.25). The outcome was better in pedicle subtraction osteotomy (PSO) compared to Smith-Petersen Osteotomy (SPO).
Conclusion:
Surgical correction of sagittal imbalance could limit the amount of disability caused by this misalignment. According to our results, while all the spinopelvic parameters could be used in the prediction of the outcomes of corrective surgery of sagittal imbalance, PI-LL was the most informative parameter and more attention should be devoted to this parameter.
Key Words: Outcome, Radiological spinopelvic parameters, Sagittal imbalance, Spinal osteotomy
Introduction
Adult spinal deformity (ASD) includes a broad range of clinical and radiological circumstances that can be associated with substantial disability (1). Sagittal plane imbalance is an increasingly recognized cause of pain and disability. It is afront-to-back imbalance in the spine that has been established as the main radiographic driver of disability in ASD. If one of the spine curves becomes either too pronounced or too flat, the spine balance will be disturbed. Consequently the center of gravity juts too forward (2, 3). This results in the reduction of the quality of life of the affected patients through causing gait disturbances as well aschronic low back and referred leg pain. According to the recent studies, sagittal balance is the most important and reliable radiographic predictor of clinical health status in the adults with a spinal deformity. Affected persons typically experience intractable pain, early fatigue, and a perception of being off-balance.
Conservative nonsurgical management of sagittal imbalance including nonsteroidal and analgesic medications as well as physical therapy plays a limited role. Surgical correction is the main method of alleviating symptoms. Spinal fusion with restored sagittal balance is the primary goal of any reconstructive procedure, which has been shown to be associated with favorable postoperative outcomes and low complication rates at long-term follow-up (4-6). In this setting, adequate balance correction during corrective osteotomyis very important for restoration ofsagittal alignment. Hence, the gravity line must be restored to a normal or near normal location to remove the stress from postural muscles of the back, hips and knees (7-9). Normative values of radiographic parameters includingpelvic tilt (PT), sagittal vertical axis (SVA) andpelvic incidence minus lumbar lordosis (PI-LL) have already been defined to achieve favorable patient-reported outcomes. Even so, restoration of optimal balancemay not always be achievable or even mayincurelevated risk (4). Thus, characterization of parameters that predict the outcome of this surgery is of considerable value.
In this study, the associationof radiological parameters with clinical outcomes was evaluated in a cohort of patients with primary or revision surgery for the correction of sagittal imbalance.
Materials and Methods
In a prospective analysis, a number of 23patients, who were referred to our center during 2010 to 2014 and underwent corrective osteotomy for the restoration of sagittal balance, were included in this study.In total, eight men and 15 women were assessed in this study. The mean age of the patients was 62.4±5.4, ranging from 51 to 71 years. The mean follow-up period of the patients was 15.5±2.1, ranging from 12 to 18 months. Preoperative spinal stenosis was observed in 14 patients. Preoperative instability was also observed in nine patients. Demographic, clinical and surgical characteristics of the patients are demonstrated in detail in Table 1.
Table 1.
Demographic, clinical, and surgical characteristics of the patients
| ID | Sex | Age (year) | UIV | LIV | PLIF | PSO | SPO | IF | Revision | Preop Stenosis | Preop Instability | Follow-up (month) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Male | 51 | T10 | Iliac | - | L4 | - | Iliac | - | - | + | 12 |
| 2 | Male | 69 | T10 | Iliac | - | - | + | Iliac | + | + | - | 13 |
| 3 | Male | 54 | T10 | Iliac | - | - | + | Iliac | - | + | - | 15 |
| 4 | Male | 66 | T10 | Iliac | 2 levels | L3 | - | Iliac | + | - | + | 17 |
| 5 | Male | 56 | T10 | Iliac | - | - | + | S2 (Iliac) | - | + | - | 18 |
| 6 | Male | 58 | T10 | Iliac | - | - | + | Iliac | - | + | - | 18 |
| 7 | Male | 58 | T10 | Iliac | - | L3 | - | Iliac | + | - | + | 18 |
| 8 | Male | 57 | T10 | Iliac | 2 levels | - | + | Iliac | - | - | + | 12 |
| 9 | Female | 63 | T10 | Iliac | - | - | + | S2 (Iliac) | - | + | - | 18 |
| 10 | Female | 63 | T10 | Iliac | - | - | + | Iliac | - | - | + | 12 |
| 11 | Female | 69 | T10 | Iliac | L3 | - | S2 (Iliac) | + | + | - | 14 | |
| 12 | Female | 64 | T9 | Iliac | 1 level | - | + | Iliac | - | + | - | 13 |
| 13 | Female | 67 | T10 | Iliac | - | L4 | - | Iliac | - | - | + | 18 |
| 14 | Female | 64 | T10 | Iliac | - | - | + | S2 (Iliac) | + | + | - | 17 |
| 15 | Female | 59 | T10 | Iliac | 1 level | - | + | Iliac | - | + | - | 16 |
| 16 | Female | 58 | T10 | Iliac | - | L3 | - | Iliac | + | - | + | 18 |
| 17 | Female | 64 | T10 | Iliac | 1 level | - | + | Iliac | - | + | - | 15 |
| 18 | Female | 61 | T10 | Iliac | - | + | S2 (Iliac) | - | + | - | 15 | |
| 19 | Female | 59 | T11 | Iliac | 1 level | - | + | Iliac | - | + | - | 14 |
| 20 | Female | 68 | T10 | Iliac | - | - | + | Iliac | + | - | + | 17 |
| 21 | Female | 69 | T10 | Iliac | - | L3 | - | S2 (Iliac) | + | + | - | 16 |
| 22 | Female | 68 | T10 | Iliac | 1 level | - | + | Iliac | + | + | - | 14 |
| 23 | Female | 71 | T10 | Iliac | - | - | + | Iliac | - | - | + | 17 |
UIV: Upper Instrumented Vertebra; LIV: Lower InstrumentedVertebra(level); PLIF: Posterior Lumbar Interbody Fusion; PSO: Pedicle Subtraction Osteotomy; SPO: Smith-Peterson Osteotomy; IF: Ilium fixation.
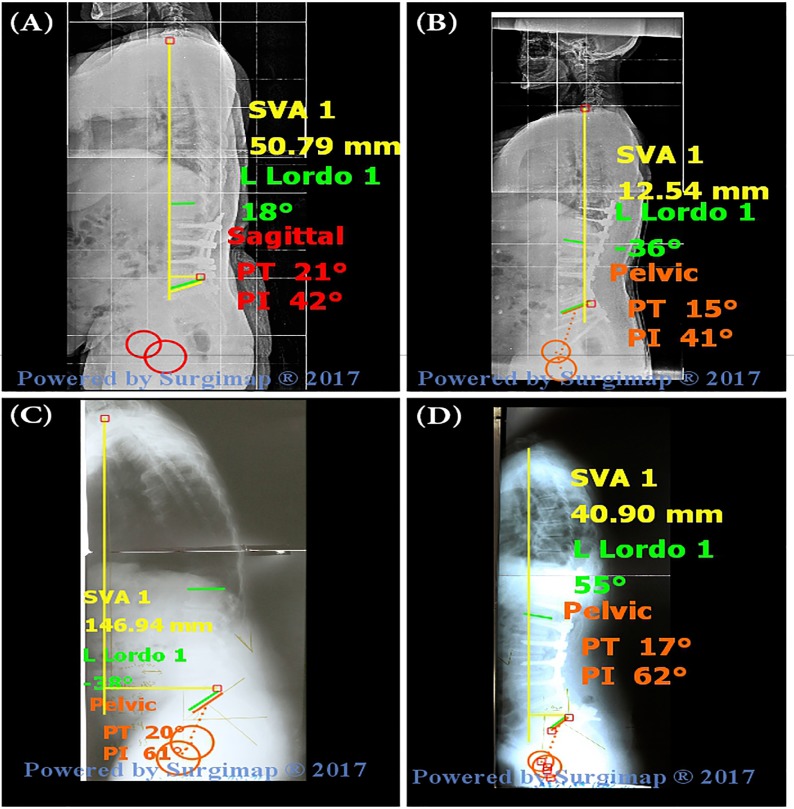
The inclusion criterion was corrective fusion surgery involving more than four intervertebral levels. In order to obtain adequate lumbar lordosis, pedicle subtraction osteotomy (PSO) [Figure 1A, B] or Smith-Peterson osteotomy (SPO) [Figure 1C, D] corrective surgery were performed. In this regard, PSO was used in seven cases and SPO was applied in the remaining 16 cases. Posterior Lumbar Interbody Fusion (PLIF) was implemented in seven cases including one PSO and six SPOs. Upper instrumented level was at T10 (21), T11 (1), and T9 (1). Lower instrumented level was at iliac in all cases. Nine patients had their revision surgery.
Figure 1.
Pre (A) and postoperative (B) lateral view of sagittal imbalance corrected with pedicle subtraction osteotomy (PSO).
Pre (C) and postoperative (D) lateral view of sagittal imbalance corrected with Smith-Petersen Osteotomy (SPO).
Radiologic and clinical parameters were assessed on whole standing X-rays and measured at baseline and at the latest follow-up session. Radiological parameters included PT, SVA and PI-LL. Clinical outcomes were evaluated using Oswestry Disability Index (ODI).
This study was approved by the review board of our institute under the code of IR.BJRC.REC.1396.321 and written consent was obtained from the patients in order to use their medical files.
Statistical analysis
Central tendency and variability for continuous variables were measured using the mean and standard deviation (SD), respectively. Pearson’s correlation coefficient was used for the analysis of the correlations. P-Values less than 0.05 were considered as statistically significant. All statistical analyseswere performed using IBM SPSS for windows, version 21.
Results
The detailed pre-and postoperative radiographic/clinical results of the patients are demonstrated in Table 2.
Table 2.
Pre- and post-operative radiographic/clinical results of the patients
| ID | Preop PT | Postop PT | PT change |
Preop
SVA (cm) |
Postop
SVA (cm) |
SVA change |
Preop
PI-LL |
Postop
PI-LL |
PI-LL
change |
Preop ODI | Postop ODI |
ODI
Change |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 25 | 15 | 10 | 13.8 | 9.8 | 4 | 30 | 10 | 20 | 58 | 50 | 8 |
| 2 | 17 | 13 | 4 | 14.7 | 10.8 | 3.9 | 32 | 11 | 21 | 48 | 32 | 16 |
| 3 | 18 | 11 | 7 | 13.6 | 7.5 | 6.1 | 25 | 5 | 20 | 48 | 28 | 20 |
| 4 | 17 | 11 | 6 | 10.1 | 4.3 | 5.8 | 21 | 9 | 12 | 56 | 32 | 24 |
| 5 | 19 | 12 | 7 | 12.4 | 7 | 5.4 | 28 | 6 | 22 | 64 | 46 | 18 |
| 6 | 18 | 11 | 6 | 13.6 | 6.9 | 7.7 | 26 | 9 | 17 | 64 | 52 | 12 |
| 7 | 23 | 12 | 11 | 13.1 | 6.1 | 8 | 34 | 11 | 23 | 62 | 56 | 6 |
| 8 | 17 | 10 | 7 | 11.3 | 4.6 | 6.7 | 24 | 6 | 18 | 70 | 40 | 30 |
| 9 | 18 | 11 | 7 | 13.6 | 9.5 | 4.1 | 27 | 2 | 25 | 68 | 40 | 28 |
| 10 | 18 | 12 | 6 | 13.3 | 9.5 | 3.8 | 28 | 7 | 21 | 64 | 38 | 26 |
| 11 | 22 | 12 | 10 | 14.2 | 8.1 | 6.1 | 31 | 3 | 28 | 60 | 38 | 22 |
| 12 | 20 | 17 | 3 | 14.6 | 4.1 | 10.5 | 23 | 7 | 16 | 62 | 54 | 8 |
| 13 | 22 | 14 | 6 | 14.4 | 7.6 | 6.8 | 34 | 10 | 24 | 72 | 36 | 36 |
| 14 | 20 | 17 | 3 | 14 | 10.2 | 3.8 | 34 | 17 | 17 | 64 | 58 | 6 |
| 15 | 19 | 12 | 7 | 12.5 | 6.6 | 5.9 | 28 | 4 | 24 | 76 | 40 | 36 |
| 16 | 23 | 10 | 13 | 12.8 | 6.4 | 6.4 | 32 | 4 | 28 | 74 | 40 | 34 |
| 17 | 18 | 14 | 4 | 13 | 9.2 | 3.8 | 30 | 17 | 13 | 58 | 54 | 4 |
| 18 | 19 | 12 | 7 | 13.3 | 6 | 7.3 | 27 | 6 | 21 | 68 | 40 | 28 |
| 19 | 17 | 11 | 6 | 10.2 | 5.5 | 4.7 | 25 | 10 | 15 | 66 | 36 | 30 |
| 20 | 22 | 15 | 7 | 13.7 | 10.7 | 3 | 35 | 21 | 14 | 68 | 68 | 0 |
| 21 | 21 | 13 | 8 | 12 | 6 | 6 | 30 | 7 | 23 | 64 | 36 | 28 |
| 22 | 22 | 16 | 6 | 15.1 | 10.8 | 4.3 | 34 | 19 | 15 | 60 | 60 | 0 |
| 23 | 21 | 15 | 6 | 5.1 | 1.2 | 3.9 | 24 | 6 | 18 | 68 | 38 | 30 |
PI-LL: pelvic incidence minus lumbar lordosis; PT: pelvic tilt; SVA: sagittal vertical axis; ODI: oswestry disability Index
The mean PT changed from 19.82°±2.6° preoperatively to 12.86°±2.6° at the latest follow-up.Accordingly, the meanPT changewas 6.82°±2.4°.The mean PI-LL changed from a preoperative mean of 28.86°±3.94° to 9.04°±5.33° at the latest follow-up. Also, the mean change of PI-LL was 19.82°±44°.The mean SVA changed from 12.8±1.63cm preoperatively to 7.44±2.27cm at the latest follow-up. Accordingly, the mean SVA change was 5.36±1.53cm.The mean ODI also changed from 64±7.5 preoperatively to 43.65±10.78 at the final follow-up.Accordingly, the mean ODI change was 19.56±11.51. The ODI value did not changein two cases (case No 20 and 22) after the operation, while it decreasedin all remaining patients after the surgery. The difference of pre- and postoperative values was statistically different across all parameters (P<0.001) [Table 3].
Table 3.
Descriptive and statistical analysis of spinopelvic parameters before and after surgical correction
| Variable | Minimum | Maximum | Mean | Std. Deviation | P value |
|---|---|---|---|---|---|
| PI-LL preop | 21.00 | 35.00 | 28.86 | 3.94 | <0.001 |
| PI-LL postop | 2.00 | 21.00 | 9.04 | 5.33 | |
| PI-LL change | 12.00 | 28.00 | 19.82 | 4.44 | |
| PT preop | 17.00 | 25.00 | 19.82 | 2.60 | <0.001 |
| PT postop | 10.00 | 17.00 | 12.86 | 2.13 | |
| PT change | 3.00 | 13.00 | 6.82 | 2.40 | |
| SVA preop | 5.10 | 15.10 | 12.80 | 1.63 | <0.001 |
| SVA postop | 1.20 | 10.80 | 7.44 | 2.27 | |
| SVA change | 3.00 | 10.50 | 5.36 | 1.53 | |
| Preop ODI | 48.00 | 74.00 | 64.00 | 7.50 | <0.001 |
| Postop ODI | 28.00 | 68.00 | 43.65 | 10.78 | |
| ODI change | .00 | 36.00 | 19.56 | 11.81 |
PI-LL: pelvic incidence minus lumbar lordosis; PT: pelvic tilt; SVA: sagittal vertical axis; ODI: oswestry disability Index
Preoperative ODI was significantly different between male and females (P=0.02). In this regard, the mean preoperative ODI was 66.8±5.7 in women versus 58.7±7.8 in men. However, postoperative ODI did not show any significant association with gender (P=0.63). In addition, no significant correlation was observed between pre- or postoperative ODI values and age of our cohort (r=-0.057, P=0.79, and r=-0.037, P=0.86, respectively).
Postoperative ODI was significantly correlated to preoperative PI-LL (r=0.608, P=0.002), preoperative PT (r=0.483, P=0.01), and preoperative SVA (r=0.464, P=0.02).
Postoperative ODI was also significantly correlated to all postoperative radiographic parameters in different degrees (r=0.768, P<0.001 for PI-LL; r=0.704, P<0.001 for PT; and r=0.554, P=0.003 for SVA).
The preoperative ODI did not show any significant correlation with preoperative radiographic parameters (P=0.92 for PI-LL, P=0.72 for PT, and P=0.11 for SVA).
The ODI improvement was significantly correlated with PI-LL change (r=536, P=0.008). A significant correlation was also observed between the ODI improvement and SVA change (r=0.416, P=0.04). However, the correlation of the ODI improvement and PT change was not significant (r=0.247, P=0.25).
ODI change was 22.5±11.7 in patients treated with PSO and 18.2±11.9 in SPO group. This difference was not statistically significant (P=0.4). PILL change was 22.2°±5.3° in PSO and 18.7°±3.7 in SPO group. This difference was not statistically significant as well (P=0.07). However, SVA and PT change were significantly different betweenthe PSO and SPO groups (P=0.02 and P=0.01, respectively). In this respect, SVA change was 6.3°±0.8° in PSO and 4.9°±1.6° in SPO group. PT change was 9.1°±2.6° in PSO and 5.8°±1.5° in SPO group.
Postoperative complications
Deep infection was seen in two patients after the surgery (Cases No 4 and 12). It was managed by irrigation and debridement followed by the graft removal.The patients received intravenous antibiotics until normalization of ESR, followed byoral antibiotic for six weeks afterwards. Subsequently, the infection was completely resolved. No other postoperative complications were observed in our patients
Discussion
Although surgical management of ASD has been reported to result in better outcomes in comparison with nonoperative treatments, management of specific ASD patterns has not been clearly codified and remainschallenging. In spite of our current understanding of normative values for sagittalplane alignment, little is known regardingthe most relevant amounts of correction necessary to achieve a favorable outcome (3, 10, 11). Thus, more clarification is needed to adequately address this challenge and predict the outcome of the surgery. In this respect, finding an association between radiologicalparameters and clinical outcomes could in principle help the prediction of outcomes and patients who most benefit from the surgery.
We evaluated the clinical and radiological outcomes of surgical correction of sagittal imbalance in 23 patients with ASD. Our results showeda significant improvement in post operative radiographic and clinical parameters following surgical correction of sagittal balance.
Our study also contains some limitations. The limited number of patients that might have affected the power of the study could be regarded as the biggest limitation of our study. Therefore, future studies with larger patients’ number could result in more favorable results.
According to the report of Schwab et al., corrective osteotomy for ASD leads to a good sagittal balance if the range of correction is within sagittal vertical axis (SVA) of less than 47 mm, pelvic tilt (PT) of less than 22°, and pelvic incidence minus lumbar lordosis ( PI – LL) of 11° or less (4). The mean postoperative PT,SVA and PI-LL of our patients were 12.86°, 7.39cm and 9.04°, respectively. While the mean PT and PI-LL of our patients were acceptable according to the normative range introduced by Schwab et al.,the mean SVA of our patients was considerably different from the desired point.Individual evaluation of the parameters demonstrated that postoperative PT was less than 22° in all patients. Postoperative PI-LL was 11° or less in the majority of cases (18 out of 23 patients). However, postoperative SVA was less than 4.7cm in only four patients.
Clinical outcomes of patients showed different degrees of improvement inall patients, but two (No.20 and 22). Interestingly, the lowest SVA and PI-LL corrections were observed in these patients as well. ODI improvement was more correlated to PI-LL change compared to the other spinopelvic parameters. Moreover, a significant positive correlation was observed between clinical outcome and perioperative radiographic parameters. This correlation was most prominent with PI-LL. Altogether, these resultsshows the importance of PI-LL in the clinical outcomes of the corrective surgeries of sagittal imbalance and suggest devoting more attention to this parameter.
The association of spinopelvic radiographic parameters with clinical outcome of patients has been examined in other investigations as well.Schwab et al. evaluated the potential correlations between spinopelvic parameters and clinical outcomes in patients with ASD in a prospective multicenter analysis. According to their results, among all parameters, PT, SVA, and PI-LL correlated most strongly with disability of patients (4).
Coutinho et al. aimed to explore which sagittal and spinopelvic radiographic parameters more influences the clinical and functional outcomesof patients undergoing spinal fusion. According to their results, patients’ satisfaction was significantly correlated with SVA, but not PT and PI-LL (12). This inconsistency with our results could be attributed to the different follow-up periods of the studies. While the minimum follow-up period of our patients was 12 months, the minimum follow-up period of the study of Coutinho et al was 3 months.
Berjano et al. evaluated the reasons of failures and revisions in surgery for sagittal imbalance.Regarding the spinopelvic parameters, patients undergoing revision surgery for failure after sagittal realignment had a mean PT of 28°, and a mean SVA of 11.8 cm (13). However, PI-LL was not evaluated in their study. Their results also confirm an association between spinopelvicradiographic parameters and clinical outcome of sagittal balance restoration.
Surgical correction of sagittal imbalance could limit the amount of disability caused by this misalignment. An acceptable clinical outcome would be expected when the correction is in certain range of spinopelvic parameters. According to our results, PI-LL was the most relevant spinopelvic parameters in determination of the clinical outcome of the patients.
References
- 1.Good CR, Auerbach JD, O’Leary PT, Schuler TC. Adult spine deformity. Curr Rev Musculoskelet Med. 2011;4(4):159–67. doi: 10.1007/s12178-011-9101-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lu DC, Chou D. Flatback syndrome. Neurosurg Clin North Am. 2007;18(2):289–94. doi: 10.1016/j.nec.2007.01.007. [DOI] [PubMed] [Google Scholar]
- 3.Blondel B, Schwab F, Ungar B, Smith J, Bridwell K, Glassman S, et al. Impact of magnitude and percentage of global sagittal plane correction on health-related quality of life at 2-years follow-up. Neurosurgery. 2012;71(2):341–8. doi: 10.1227/NEU.0b013e31825d20c0. [DOI] [PubMed] [Google Scholar]
- 4.Schwab FJ, Blondel B, Bess S, Hostin R, Shaffrey CI, Smith JS, et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine. 2013;38(13):E803–12. doi: 10.1097/BRS.0b013e318292b7b9. [DOI] [PubMed] [Google Scholar]
- 5.Hyun SJ, Rhim SC. Clinical outcomes and complications after pedicle subtraction osteotomy for fixed sagittal imbalance patients: a long-term follow-up data. J Korean Neurosurg Soc. 2010;47(2):95–101. doi: 10.3340/jkns.2010.47.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim YJ, Bridwell KH, Lenke LG, Cheh G, Baldus C. Results of lumbar pedicle subtraction osteotomies for fixed sagittal imbalance: a minimum 5-year follow-up study. Spine. 2007;32(20):2189–97. doi: 10.1097/BRS.0b013e31814b8371. [DOI] [PubMed] [Google Scholar]
- 7.Roussouly P, Nnadi C. Sagittal plane deformity: an overview of interpretation and management. Eur Spine J. 2010;19(11):1824–36. doi: 10.1007/s00586-010-1476-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Le Huec JC, Faundez A, Dominguez D, Hoffmeyer P, Aunoble S. Evidence showing the relationship between sagittal balance and clinical outcomes in surgical treatment of degenerative spinal diseases: a literature review. Int Orthop. 2015;39(1):87–95. doi: 10.1007/s00264-014-2516-6. [DOI] [PubMed] [Google Scholar]
- 9.Jang JS, Lee SH, Min JH, Maeng DH. Changes in sagittal alignment after restoration of lower lumbar lordosis in patients with degenerative flat back syndrome. J Neurosurg Spine. 2007;7(4):387–92. doi: 10.3171/SPI-07/10/387. [DOI] [PubMed] [Google Scholar]
- 10.Smith JS, Shaffrey CI, Berven S, Glassman S, Hamill C, Horton W, et al. Operative versus nonoperative treatment of leg pain in adults with scoliosis: a retrospective review of a prospective multicenter database with two-year follow-up. Spine. 2009;34(16):1693–8. doi: 10.1097/BRS.0b013e3181ac5fcd. [DOI] [PubMed] [Google Scholar]
- 11.Smith JS, Shaffrey CI, Berven S, Glassman S, Hamill C, Horton W, et al. Improvement of back pain with operative and nonoperative treatment in adults with scoliosis. Neurosurgery. 2009;65(1):86–93. doi: 10.1227/01.NEU.0000347005.35282.6C. [DOI] [PubMed] [Google Scholar]
- 12.Coutinho MA, Pratali RD, Motta MM, Hoffman CB, Barsotti CE, Santos FP, et al. Influence of the sagittal balance on the clinical outcome in spinal fusion. Coluna/Columna. 2016;15(1):52–6. [Google Scholar]
- 13.Berjano P, Bassani R, Casero G, Sinigaglia A, Cecchinato R, Lamartina C. Failures and revisions in surgery for sagittal imbalance: analysis of factors influencing failure. Eur Spine J. 2013;22(6):853–8. doi: 10.1007/s00586-013-3024-x. [DOI] [PMC free article] [PubMed] [Google Scholar]