Abstract
Meniscal root tears are defined as radial tears located within 1 cm from the meniscal attachment or a bony root avulsion. This injury is biomechanically comparable to a total meniscectomy, leading to compromised hoop stresses resulting in decreased tibiofemoral contact area and increased contact pressures in the involved compartment. These changes are detrimental to the articular cartilage and ultimately lead to the development of early osteoarthritis. Surgical repair is the treatment of choice in patients without significant osteoarthritis (Outerbridge grades 3 or 4). Root repairs have been reported to improve clinical outcomes, decrease meniscal extrusion and slow the onset of degenerative changes. Here we describe the anatomy, biomechanics, clinical evaluation, treatment methods, outcomes, and post-operative rehabilitation for posterior meniscal root tears.
Key Words: Lateral meniscus, Medial meniscus, Meniscus root tear, Outcomes, Root repair
Introduction
Meniscal root tears are defined as bony or soft tissue root avulsion injuries or radial tears within 1 cm of meniscus root attachment (1–4). These tears are increasingly being recognized as a cause of morbidity, development of early osteoarthritis (OA), and altered joint kinematics when not surgically repaired (3, 5–9). The prevalence of a complete meniscus root tear in patients with a documented meniscus root tear has been reported to be 9.1 % overall in patients who had arthroscopic knee surgery (10). Moreover, lateral meniscus posterior root tears (LPRT) were 10.3 times more likely to occur with an ACL tear than medial meniscus posterior root tears (MPRT), which were 5.8 times more likely to have concomitant knee chondral defects than LPRTs (11). Medial meniscus posterior root tears are commonly degenerative and seen in middle aged women and may represent up to 21.5% of posterior horn medial meniscus tears (11). Iatrogenic MPRT have also been reported after non-anatomic tibial tunnel placement in posterior cruciate ligament (PCL) reconstructions (12). Injuries to the anterior horns of the menisci are less common and frequently occur iatrogenically, such as during ACL tibial tunnel reaming and tibial nailing on tibial shaft fractures (12–14).
Historically, meniscal root tears were treated with total or partial meniscectomy to achieve short-term benefits. Recent anatomic, biomechanical, and patient reported outcome studies have elucidated this pathology, substantiated the necessity of repair, and have led to improved treatment methods. Currently, repair of meniscal root injuries is the treatment of choice with the aim of restoring joint kinematics, contact pressures, and delaying the development of OA (15, 16). This review will focus mainly on posterior meniscal root tears including the anatomy, biomechanics, clinical evaluation, treatment methods, outcomes, and post-operative rehabilitation.
Anatomy
The meniscal roots exhibit main and supplemental fiber attachment sites, which significantly contribute to the native attachment areas and root attachment forces. Therefore, previous anatomic studies need to be interpreted based upon whether or not they have included the supplemental fibers (17–21).
Medial meniscus posterior root attachment (MPRA)
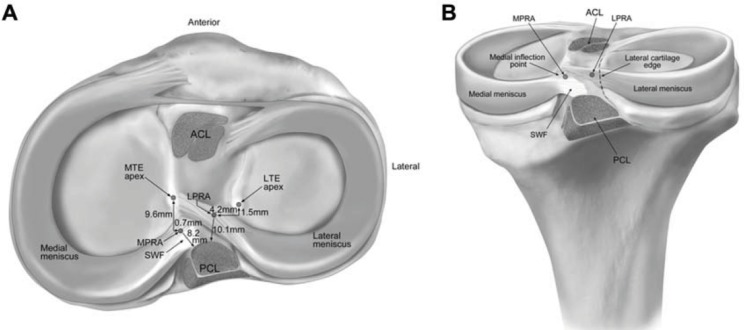
The MPRA is 9.6 mm posterior and 0.7 mm lateral to the medial tibial eminence (MTE), which is the most reproducible osseous landmark (17). Additionally, the center point of the MPRA can be found 3.5 mm lateral to the medial cartilage inflection point and 8.2 mm directly anterior to the most proximal aspect of the PCL tibial attachment point, which represent two other consistent landmarks [Figure 1] (17).
Figure 1.
Medial and lateral meniscal posterior root attachments and relevant arthroscopic bony landmarks. (A) Superior view and (B) posterior view. ACL, anterior cruciate ligament; LPRA, lateral meniscus posterior root attachment; LTE, lateral tibial eminence; MPRA, medial meniscus posterior root attachment; MTE, medial tibial eminence; PCL, posterior cruciate ligament bundle attachments; SWF, shiny white fibers of posterior horn of medial meniscus. (Reproduced with permission from: Johannsen M, Civitarese DM, Padalecki JR, Goldsmith MT, Wijdicks CA, LaPrade RF. Qualitative and quantitative anatomic analysis of the posterior root attachments of the medial and lateral menisci. Am J Sport Med. 2012;40(10):2342–7).
Lateral meniscus posterior root attachment (LPRA)
The LPRA is 1.5 mm posterior and 4.2 mm medial to the lateral tibial eminence (LTE) (17). Additionally, the center point of the LPRA is 4.3 mm medial to the lateral cartilage inflection point and 12.7 mm directly anterior to the most proximal aspect of the PCL tibial attachment (17).
Medial meniscus anterior root attachment (MARA)
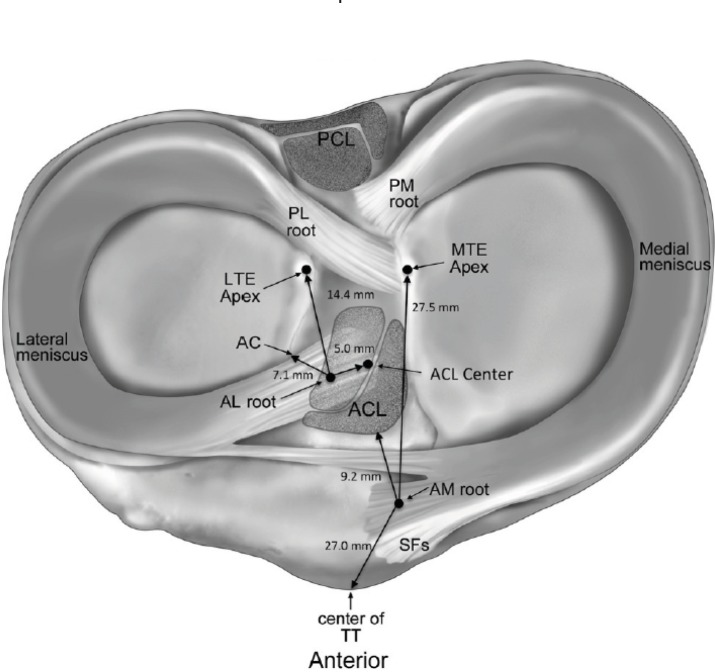
The MARA inserts along the anterior intercondylar crest of the anterior slope of the tibia (5). The center of the MARA was reported to be 18.2 mm anteromedial from the center of the anterior cruciate ligament (ACL) tibial footprint and 27.5 mm anterolateral from the medial tibial eminence apex [Figure 2] (22). The MARA is at risk during intramedullary nailing of tibial fractures (14).
Figure 2.
The anterior lateral (AL) meniscal root is shown to run deeply beneath and overlap with the anterior cruciate ligament (ACL), as observed in all knees. The anterior medial (AM) meniscal root is depicted with supplemental fibers (SFs) that were observed to be anterior and distal to the central root. Anterior meniscal root structure is also described in relation to pertinent bony and soft tissue landmarks. AC, articular cartilage; LTE, lateral tibial eminence; MTE, medial tibial eminence; PL root, posterior lateral meniscal root; PM root, posterior medial meniscal root; TT, tibial tuberosity. (Reproduced with permission from: LaPrade CM, Ellman MB, Rasmussen MT, James EW, Wijdicks CA, Engebretsen L, et al. Anatomy of the anterior root attachments of the medial and lateral menisci: a quantitative analysis. Am J Sport Med. 2014;42(10):2386–92.)
Lateral meniscus anterior root attachment (LARA)
LaPrade et al reported that the area of the LARA averaged 140.7 mm2, given the considerable overlap with the ACL footprint (22). Furthermore, the LARA site was 5.0 mm anterolateral from the center of the ACL footprint, 14.4 mm from the lateral tibial eminence apex and 7.1 mm from the nearest edge of the lateral articular cartilage. Therefore, the LARA is at high risk for iatrogenic injury during ACL tibial tunnel reaming [Figure 2] (12, 22).
Biomechanics
The meniscal roots have an important function for the meniscus to convert axial tibiofemoral loads into hoop stresses (8). The loss of meniscal anchoring to the tibial plateau results in loss of normal meniscus function, meniscal extrusion, and altered knee kinematics. This leads to unequal and abnormal distribution of knee loading, thereby decreasing tibiofemoral contact area and increasing peak contact pressures (8). Allaire et al reported that sectioning of the MPRA resulted in a 25% increase in medial peak contact pressure when compared to the native state, comparable to that of a total meniscectomy (8). Similar changes in the loading profile of the knee have been reported for avulsions of the LPRA (2, 9). The increased contact pressures due to meniscal root tears are detrimental to the articular cartilage, and can lead to the development of early OA if not treated adequately (23, 24).
In cases of ACL deficiency, the LM posterior root plays an important role in stabilizing the knee in both anterior tibial translation (ATT) and during pivoting activities (25). Therefore, in patients who exhibit a grade 3 Lachman and a 3+ pivot shift, a possible LPRT should be suspected. The LPRA has also been reported to act as the primary stabilizer for internal rotation at higher flexion angles (25). Based on these biomechanical findings, a repair of a LPRT should be performed concurrently with an ACL reconstruction to avoid persistent instability and increased forces on the ACL graft.
Although speculation still exists on whether or not the shiny white fibers (SWF) and supplemental fibers should be considered as part of the meniscal root attachment, biomechanical investigations have reported that they impart significant contributions to their ultimate failure strengths for the posteromedial, posterolateral and anteromedial roots (19). Therefore, Ellman et al suggested that failure to incorporate these fibers during repair might be why some surgical techniques do not adequately restore knee biomechanics (19). Likewise, a non-anatomic repair has been reported to have significant consequences for the long-term health of the tibiofemoral joint (26, 27). In porcine and human models, recent studies have reported that a non-anatomic transtibial pull-out repair of the medial meniscal roots, anchored only 3-5 mm medial from the native site, substantially increased mean contact pressure and decreased contact area during tibiofemoral loading (26, 27). Therefore, anatomic repair is necessary to decrease the detrimental factors contributing to the progression of osteoarthritis.
The two-tunnel transtibial pull-out repair technique has become popular among clinicians because of its ability to restore tibiofemoral contact pressures and contact area at time zero (3, 8, 28–30). The transtibial pull-out technique has also been proposed to have the added benefit of enhanced meniscal healing due to the biological effect provided by tunnel drilling allowing the egression of growth factors and progenitor cells from bone marrow (31). However, micromotion of the meniscal root, or “bungee effect” as described by Feucht et al (2014), caused by long length suture construct has been an area of concern, but Cerminara et al. reported that the main cause of root displacement was the meniscus-suture interface failure, rather than a “bungee effect” (28, 31).
Diagnosis
Clinical Evaluation
Meniscal root tears can occur during traumatic events, but most cases (around 70% of MPRT) occur in degenerative knees without a specific injury event or following minor traumatic movement, such as squatting (32,33). The MPRA is the least mobile of the meniscal roots and, consequently, has a highest incidence of tears. The incidence of MPRT reportedly varies from 10-21% of medial meniscus tears (34–38). In the setting of a multiligament injury, the incidence of MPRT is reported to be around 3% (6, 33, 39, 40). Additionally, 80% of patients with spontaneous osteonecrosis of the knee (SONK), typically involving the medial femoral condyle, have an associated MPRT, which argues against the “spontaneous” etiology of this overload syndrome (41). The risk factors for MPRT are varus alignment, increased age, high body mass index and female sex (35–37, 42).
Most meniscus root tears have no history of inciting trauma; therefore, a high degree of suspicion is required in the presence of risk factors. Patients can report joint line pain, but meniscal mechanical symptoms (locking, catching and giving way) are not common (43). A popping sound can be heard when the patient performs light activities like rising from a chair or squatting (44). The onset of pain may be subtle and severe with a minor or no evident trauma (45). The most common findings on physical examination are pain with full knee flexion (66.7%), joint line tenderness (61.9%) and a positive McMurray test (57.1%) (45). A MPRT can result in an extruded meniscus palpable along the anteromedial joint line when a varus stress is applied to the knee in full extension. This extrusion disappears when normal knee alignment is restored (46).
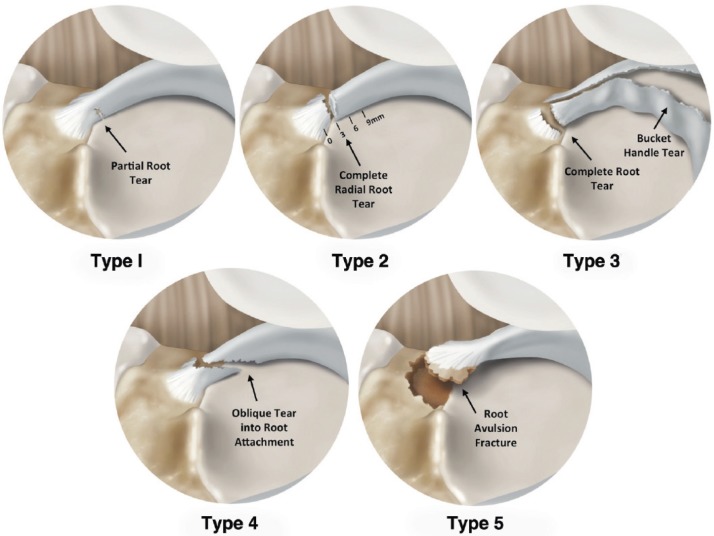
LaPrade et al. (2015) classified posterior root tears according to morphology based on an arthroscopic assessment. Type 1 (7%) is a partial and stable root tear; Type 2 (68%) a complete radial tear within 9 mm of the root attachment. A Type 2 tear can be subclassified in 2a (38%), within 0 to <3 mm, 2b (17%), between 3 and <6 mm and 2c (12%), between 6 and 9 mm from the root attachment. Type 3 (6%) is a bucket-handle tear with complete root detachment, Type 4 (10%) is a complex oblique or longitudinal tear with complete root detachment and Type 5 is a root bony avulsion [Figure 3] (47). Forkel et al. have described another classification for LPRT according to localization and compromise of meniscofemoral ligaments (48).
Figure 3.
Meniscal root tear classification system illustrated in posterior medial meniscal root. Type 1: partial stable tear. Type 2: Complete radial tear within 9 mm from attachment. Type 3: Bucket-handle tear with complete root detachment. Type 4: Complex oblique or longitudinal tear with complete root detachment. Type 5: Bony avulsion fracture of the root attachment. (Reproduced with permission from: LaPrade CM, James EW, Cram TR, Feagin JA, Engebretsen L, LaPrade RF. Meniscal Root Tears. Am J Sports Med. 2015;43(2):363-9
Imaging
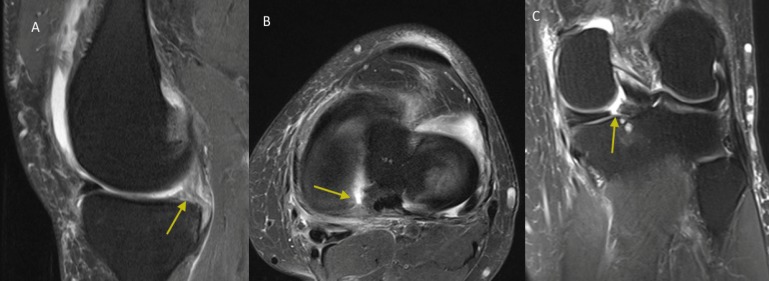
Magnetic resonance imaging (MRI) is the imaging modality of choice to diagnose meniscal root tears and concomitant pathologies (32, 35, 49–51). In a recent prospective level II study LaPrade and Ho reported a diagnostic sensitivity of 77%, a specificity of 73%, a positive predictive value (PPV) of 22%, and a negative predictive value (NPV) of 97% using 3.0 T MRI, with a higher sensitivity for MPRT (10). To assess for a meniscal root injury, T2-weighted sequences are typically utilized with coronal, sagittal and axial images (49, 52). Three main signs should be evaluated on MRI when a MPRT is suspected: 1) linear high signal intensity perpendicular to the meniscus (radial tear) at the meniscal root in the axial plane; 2) a vertical linear defect on the meniscal root (truncation sign), which is associated with medial meniscal extrusion >3 mm; and 3) the ghost sign, which is absence of normal meniscus signal in the sagittal plane [Figure 4] (50). These three signs when used together have been reported to have a high sensitivity and specificity (10). Moreover, near perfect intra- and interobserver reliability were reported for MPRT diagnosis on axial, coronal and sagittal MRI planes (50).
Figure 4.
Left knee MRI showing a medial meniscus posterior root tear (MPRT) (White arrow). A: Sagittal plane view. Ghost sign; B: Axial plane view; C: Coronal plane view
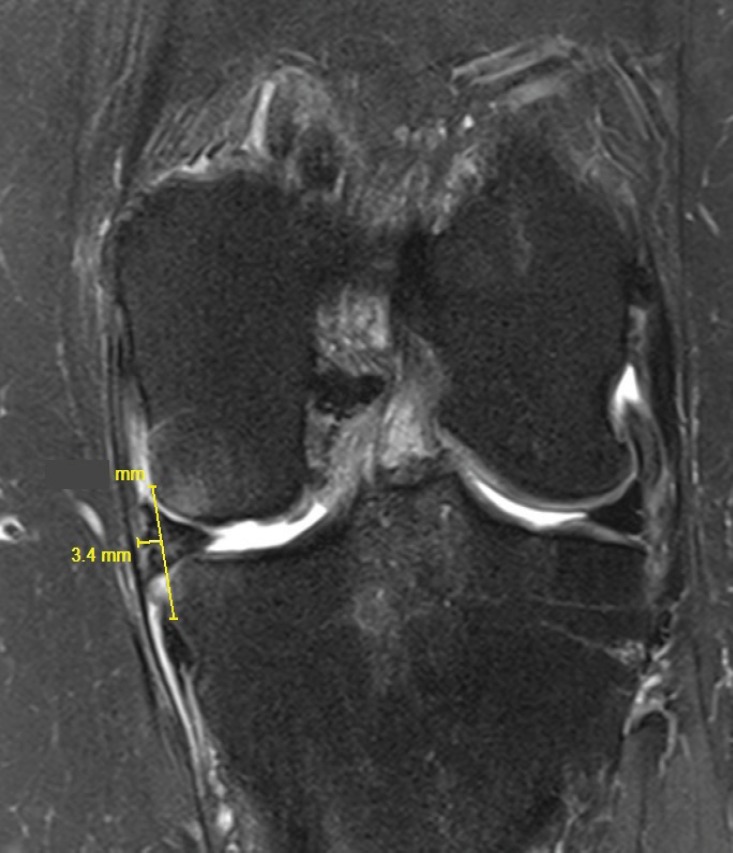
Extrusions of greater than 3 mm on mid-coronal imaging are significantly associated with articular cartilage degeneration, severe meniscal degeneration, and meniscal root tears [Figure 5] (53, 54). Ipsilateral tibiofemoral compartment bone marrow edema and insufficiency fractures are commonly noted in the presence of posterior meniscal tears (32).
Figure 5.
Left knee MRI showing a medial meniscus extrusion on the coronal plane views.
Treatment Rationale
Treatment of meniscal root tears is variable based upon the severity of the injury, timing of injury to surgical intervention and the condition of the articular cartilage. The goal of surgical repair is to restore joint contact pressures, joint kinematics and delay the development of OA. Therefore, surgical repair is not indicated for patients with diffuse Outerbridge grades 3-4; however, it may be considered in those with focal chondral deficits to relieve symptoms. The most commonly utilized treatments for posterior meniscal root tears include non-operative treatment, partial meniscectomy, or repair.
Non-Operative Treatment
With recent evidence on the importance of the posterior meniscal roots on maintaining hoop stresses, normal knee kinematics and normal contact loading; as well as excellent post-operative patient reported outcomes and established surgical techniques; there are few scenarios not to treat a root tear with a surgical repair. Elderly patients with high grade and diffuse OA (Outerbridge 3-4) are usually candidates for non-operative treatment. Symptomatic treatment with use of analgesics, (oral or topical), activity modification and/or an unloader brace can relieve some of the symptoms.
Meniscectomy
Patients with advanced degenerative changes and persistent mechanical symptoms such as locking and who have failed conservative treatment may benefit from a partial or subtotal meniscectomy (42). However, development of further OA reliably occurs, making symptom relief often short-lived in contrast to meniscal root surgical repair.
Posterior Meniscal Root Repair
Anatomic repair of the meniscal root should be attempted whenever possible to prevent meniscus damage and OA, except in cases in which the patient is a poor surgical candidate (significant comorbidities or advanced age), diffuse Outerbridge grade 3 or 4 OA of the ipsilateral compartment, non-symptomatic chronic meniscal root tears, and/or significant limb malalignment unless concurrently corrected (32, 55). The two most commonly used repair techniques are suture anchor repair and transtibial meniscal root repair.
Suture anchor repair
Medial meniscal root tears can be treated with suture anchor repair, utilizing one suture anchor with two sutures via an all-inside technique. For a MPRT, an anchor is inserted at the meniscal root anatomic footprint by using a high posteromedial portal. Then, the root is reattached with two vertical sutures (56–58). This technique is technically demanding and has mainly been reported in patients with grade 3 medial collateral ligament tears.
Transtibial pull-out repair
Many techniques describing transosseous suture fixation for medial and lateral posterior root tears have been described. Treatment can slightly differ depending on the type of meniscal root tear pattern. This particular technique involves passing sutures through the meniscal root, retrieving them through tunnels drilled in the proximal tibia and subsequently tying them over a post, button or anterior tibia bone bridge (40, 59–61). Many meniscal suture configurations have been proposed with different biomechanical properties including two simple stiches, horizontal mattress stitch, modified Mason-Allen (MMA), and two modified loop stiches (62). However, two simple sutures have been reported to result in the least root displacement, have increased stiffness, and reportedly not significantly different to the more complex (MMA) suture (28, 62). Single tunnel and double tunnel techniques have been described in attempt to better reproduce the anatomical footprint and enhance biologic healing (30). Fixation with a button is advantageous given that it is less invasive and reduces risk of soft tissue irritation compared with screw and washer fixation (40).
Senior author’s preferred technique
The senior author´s preferred technique is a two-tunnel transtibial pull-out repair using two simple sutures tied over a cortical button. Standard anterolateral (AL) and anteromedial (AM) parapatellar portals directly adjacent to the patellar tendon are made together with accessory AM or AL portals as needed. A curette is used to decorticate the planned root reattachment site on the tibial plateau. An ACL or meniscal root guide is used to position a drill pin with a cannulated sleeve in the posterior aspect of the footprint followed by another drill hole with cannula placed approximately 5 mm anterior to the first. Once the tunnel placements are verified to be correct, the drill pins are removed and two simple sutures are passed, one anterior and one posterior, into the meniscus root using a suture passing device through an anterior or posteromedial portal depending on the device. The sutures are then retrieved through the corresponding tunnels and tied over a button on the AM or AL aspect of the tibia [Figure 6] (55).
Figure 6.
Transtibial pull-out repair of a medial meniscal posterior root tear in a right knee. (Reproduced with permission from: LaPrade CM, LaPrade MD, Turnbull TL, Wijdicks CA, LaPrade RF. Biomechanical evaluation of the transtibial pull-out technique for posterior medial meniscal root repairs using 1 and 2 transtibial bone tunnels. Am J Sports Med. 2015;43(4):899–904).
Outcomes
Partial meniscectomy vs meniscal root repair
Partial meniscectomy for MPRT has been reported to significantly improve subjective outcome scores; however, degenerative changes on the Kellgren-Lawrence scale (KL) increased significantly postoperatively at 5 years’ follow-up (35, 63). In a recent retrospective study by Krych et al. comparing a partial medial meniscectomy with nonoperative treatment, no significant difference in final Tegner scores, IKDC, or KL grades, was found between both groups. However, 54% of the partial medial meniscectomy group progressed to a total knee arthroplasy (TKA) at a mean of 4.5 years (63).
Meniscal root repairs have been reported to improve subjective patient outcomes. In a recent meta-analysis Chung et al. reported significant improvements in postoperative clinical scores after operative repair (23, 24). Similar results were reported in a recent systematic review by Feucht et al. (64). Feucht et al. reported an improvement of the Lysholm score (52 to 86) after MPRT repair by arthroscopic transtibial pull-out technique (64). In a retrospective study comparing transtibial pull-out meniscal root repair to partial meniscectomy at minimum 5-year follow-up, Chung et al., reported significantly better clinical and radiological outcomes in the repair group (24). The rate of conversion to a TKA was 34% in the partial meniscectomy group and none in the root repair group (24). In a retrospective study, Kim et al. compared partial meniscectomy (28 patients) to meniscal root repair with pull-out technique (30 patients) with a mean follow up of 46 months. Significantly better clinical and radiologic results were found in the repair group (65).
LaPrade et al performed a retrospective Level III study of 50 knees and reported improved subjective outcomes (Lysholm, IKDC, WOMAC) with posterior meniscal root repairs with an anatomic two-tunnel transtibial pull-out technique (66). There was no significant differences in the failure rate according to age (<50 vs >50 years) and laterality (MPRT vs LPRT). Patient satisfaction was high with a significant improvement in pain, function and activity level (66). Therefore, they suggested that other factors such as OA grade, high BMI, or the ability to comply with the postoperative rehabilitation protocol may be more useful when assessing the appropriate management rather than age as a sole factor (66, 67).
Meniscal root repair and arthritis
In a meta-analysis by Chung et al, it was reported that progression of arthrosis was observed in only 10% of patients at a mean follow-up of 30.3 months and mean age of 54 years after meniscal root repair (23). Therefore, it was concluded that a minimum of 79.7% of patients with MPRT could avoid degenerative changes with surgical repair. In a systematic review by Feucht et al, it was reported that 84% of the patients had no progression of OA on the Kellgren-Lawrence grading scale after meniscal root repair (64). These studies suggest that meniscus root repair can slow down the progression of osteoarthritis.
Meniscal root repair and meniscal extrusion
One of the challenges with meniscal root repairs is the presence of meniscal extrusion during follow-up. Chung et al reported that meniscal extrusion was not reduced in the evaluation of 117 patients of four studies, while Feutch et al. found a 56% rate of medial meniscus extrusion (23, 64). Kim et al found a decrease in meniscal extrusion in 86.7% of patients (24). The biomechanical consequences of extrusion are not fully understood; however, increased joint loading can be expected with increasing meniscus extrusion. Therefore, anatomic reduction and fixation of the meniscus root to the anatomic footprint is important.
Postoperative Rehabilitation
The patient should remain non-weight-bearing for a minimum of 6 weeks following a transtibial pull-out meniscus root repair. Passive range of motion exercises in a safe zone of 0º to 90º of flexion is initiated postoperative day 1. After 2 weeks, the patient can be advanced in their knee flexion as tolerated. Progressive advancement to full weight-bearing begins at 6 weeks. Deep leg presses and squats with greater than 70º of knee flexion should be avoided for at least 4 months following surgery. Different postoperative rehabilitation protocols have been described in the literature; however, no comparison study has been performed (32, 33, 67, 68).
Although the management of meniscal root tears is evolving and improved subjective outcomes are being observed, no long randomized controlled studies have been published to date. However, with an adequate diagnosis such as a correct clinical and imaging assessment, followed by a correct indication, meniscal root tears should be repaired. This will result in improved clinical and radiological outcomes compared to a partial meniscectomy.
References
- 1.Choi CJ, Choi YJ, Lee JJ, Choi CH. Magnetic resonance imaging evidence of meniscal extrusion in medial meniscus posterior root tear. Arthroscopy. 2010;26(12):1602–6. doi: 10.1016/j.arthro.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 2.Laprade CM, Jansson KS, Dornan G, Smith SD, Wijdicks CA, Laprade RF. Altered tibiofemoral contact mechanics due to lateral meniscus posterior horn root avulsions and radial tears can be restored with in situ pull-out suture repairs. J Bone Joint Surg Am. 2014;96(6):471–9. doi: 10.2106/JBJS.L.01252. [DOI] [PubMed] [Google Scholar]
- 3.Padalecki JR, Jansson KS, Smith SD, Dornan GJ, Pierce CM, Wijdicks CA, et al. Biomechanical consequences of a complete radial tear adjacent to the medial meniscus posterior root attachment site: in situ pull-out repair restores derangement of joint mechanics. Am J Sports Med. 2014;42(3):699–707. doi: 10.1177/0363546513499314. [DOI] [PubMed] [Google Scholar]
- 4.Marzo JM, Gurske-DePerio J. Effects of medial meniscus posterior horn avulsion and repair on tibiofemoral contact area and peak contact pressure with clinical implications. Am J Sports Med. 2009;37(1):124–9. doi: 10.1177/0363546508323254. [DOI] [PubMed] [Google Scholar]
- 5.Koenig JH, Ranawat AS, Umans HR, Difelice GS. Meniscal root tears: diagnosis and treatment. Arthroscopy. 2009;25(9):1025–32. doi: 10.1016/j.arthro.2009.03.015. [DOI] [PubMed] [Google Scholar]
- 6.Pagnani MJ, Cooper DE, Warren RF. Extrusion of the medial meniscus. Arthroscopy. 1991;7(3):297–300. doi: 10.1016/0749-8063(91)90131-g. [DOI] [PubMed] [Google Scholar]
- 7.Papalia R, Vasta S, Franceschi F, D’Adamio S, Maffulli N, Denaro V. Meniscal root tears: from basic science to ultimate surgery. Br Med Bull. 2013;106(2):91–115. doi: 10.1093/bmb/ldt002. [DOI] [PubMed] [Google Scholar]
- 8.Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus. J Bone Joint Surg Am. 2008;90(9):1922–31. doi: 10.2106/JBJS.G.00748. [DOI] [PubMed] [Google Scholar]
- 9.Schillhammer CK, Werner FW, Scuderi MG, Cannizzaro JP. Repair of lateral meniscus posterior horn detachment lesions: a biomechanical evaluation. Am J Sports Med. 2012;40(11):2604–9. doi: 10.1177/0363546512458574. [DOI] [PubMed] [Google Scholar]
- 10.LaPrade RF, Ho CP, James E, Crespo B, LaPrade CM, Matheny LM. Diagnostic accuracy of 30 T magnetic resonance imaging for the detection of meniscus posterior root pathology. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):152–7. doi: 10.1007/s00167-014-3395-5. [DOI] [PubMed] [Google Scholar]
- 11.Matheny LM, Ockuly AC, Steadman JR, LaPrade RF. Posterior meniscus root tears: associated pathologies to assist as diagnostic tools. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):3127–31. doi: 10.1007/s00167-014-3073-7. [DOI] [PubMed] [Google Scholar]
- 12.LaPrade CM, Smith SD, Rasmussen MT, Hamming MG, Wijdicks CA, Engebretsen L, et al. Consequences of tibial tunnel reaming on the meniscal roots during cruciate ligament reconstruction in a cadaveric model, Part 2: The posterior cruciate ligament. Am J Sports Med. 2015;43(1):207–12. doi: 10.1177/0363546514554771. [DOI] [PubMed] [Google Scholar]
- 13.Ellman MB, James EW, LaPrade CM, LaPrade RF. Anterior meniscus root avulsion following intramedullary nailing for a tibial shaft fracture. Knee Surg Sports Traumatol Arthrosc. 2015;23(4):1188–91. doi: 10.1007/s00167-014-2941-5. [DOI] [PubMed] [Google Scholar]
- 14.LaPrade MD, LaPrade CM, Hamming MG, Ellman MB, Turnbull TL, Rasmussen MT, et al. Intramedullary tibial nailing reduces the attachment area and ultimate load of the anterior medial meniscal root: a potential explanation for anterior knee pain in female patients and smaller patients. Am J Sport Med. 2015;43(7):1670–5. doi: 10.1177/0363546515580296. [DOI] [PubMed] [Google Scholar]
- 15.Hoser C, Fink C, Brown C, Reichkendler M, Hackl W, Bartlett J. Long-term results of arthroscopic partial lateral meniscectomy in knees without associated damage. J Bone Joint Surg Br. 2001;83(4):513–6. doi: 10.1302/0301-620x.83b4.11364. [DOI] [PubMed] [Google Scholar]
- 16.Stein T, Mehling AP, Welsch F, von Eisenhart-Rothe R, Jäger A. Long-term outcome after arthroscopic meniscal repair versus arthroscopic partial meniscectomy for traumatic meniscal tears. Am J Sports Med. 2010;38(8):1542–8. doi: 10.1177/0363546510364052. [DOI] [PubMed] [Google Scholar]
- 17.Johannsen AM, Civitarese DM, Padalecki JR, Goldsmith MT, Wijdicks CA, LaPrade RF. Qualitative and quantitative anatomic analysis of the posterior root attachments of the medial and lateral menisci. Am J Sport Med. 2012;40(10):2342–7. doi: 10.1177/0363546512457642. [DOI] [PubMed] [Google Scholar]
- 18.Anderson CJ, Ziegler CG, Wijdicks CA, Engebretsen L, LaPrade RF. Arthroscopically pertinent anatomy of the anterolateral and posteromedial bundles of the posterior cruciate ligament. J Bone Joint Surg Am. 2012;94(21):1936–45. doi: 10.2106/JBJS.K.01710. [DOI] [PubMed] [Google Scholar]
- 19.Ellman MB, LaPrade CM, Smith SD, Rasmussen MT, Engebretsen L, Wijdicks CA, et al. Structural properties of the meniscal roots. Am J Sports Med. 2014;42(8):1881–7. doi: 10.1177/0363546514531730. [DOI] [PubMed] [Google Scholar]
- 20.Kohn D, Moreno B. Meniscus insertion anatomy as a basis for meniscus replacement: a morphological cadaveric study. Arthroscopy. 1995;11(1):96–103. doi: 10.1016/0749-8063(95)90095-0. [DOI] [PubMed] [Google Scholar]
- 21.Johnson DL, Swenson TM, Livesay GA, Aizawa H, Fu FH, Harner CD. Insertion-site anatomy of the human menisci: gross, arthroscopic, and topographical anatomy as a basis for meniscal transplantation. Arthroscopy. 1995;11(4):386–94. doi: 10.1016/0749-8063(95)90188-4. [DOI] [PubMed] [Google Scholar]
- 22.LaPrade CM, Ellman MB, Rasmussen MT, James EW, Wijdicks CA, Engebretsen L, et al. Anatomy of the anterior root attachments of the medial and lateral menisci: a quantitative analysis. Am J Sport Med. 2014;42(10):2386–92. doi: 10.1177/0363546514544678. [DOI] [PubMed] [Google Scholar]
- 23.Chung KS, Ha JK, Ra HJ, Kim JG. A meta-analysis of clinical and radiographic outcomes of posterior horn medial meniscus root repairs. Knee Surg Sports Traumatol Arthrosc. 2016;24(5):1455–68. doi: 10.1007/s00167-015-3832-0. [DOI] [PubMed] [Google Scholar]
- 24.Chung KS, Ha JK, Yeom CH, Ra HJ, Jang HS, Choi SH, et al. Comparison of clinical and radiologic results between partial meniscectomy and refixation of medial meniscus posterior root tears: a minimum 5-year follow-up. Arthroscopy. 2015;31(10):1941–50. doi: 10.1016/j.arthro.2015.03.035. [DOI] [PubMed] [Google Scholar]
- 25.Frank JM, Moatshe G, Brady AW, Dornan GJ, Coggins A, Muckenhirn KJ, et al. Lateral meniscus posterior root and meniscofemoral ligaments as stabilizing structures in the ACL-deficient knee: a biomechanical study. Orthop J Sport Med. 2017;5(6):232596711769575. doi: 10.1177/2325967117695756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.LaPrade CM, Foad A, Smith SD, Turnbull TL, Dornan GJ, Engebretsen L, et al. Biomechanical consequences of a nonanatomic posterior medial meniscal root repair. Am J Sport Med. 2015;43(4):912–20. doi: 10.1177/0363546514566191. [DOI] [PubMed] [Google Scholar]
- 27.Stärke C, Kopf S, Gröbel KH, Becker R. The effect of a nonanatomic repair of the meniscal horn attachment on meniscal tension: a biomechanical study. Arthroscopy. 2010;26(3):358–65. doi: 10.1016/j.arthro.2009.08.013. [DOI] [PubMed] [Google Scholar]
- 28.Cerminara AJ, LaPrade CM, Smith SD, Ellman MB, Wijdicks CA, LaPrade RF. Biomechanical evaluation of a transtibial pull-out meniscal root repair: challenging the bungee effect. Am J Sports Med. 2014;42(12):2988–95. doi: 10.1177/0363546514549447. [DOI] [PubMed] [Google Scholar]
- 29.Harner CD, Mauro CS, Lesniak BP, Romanowski JR. Biomechanical consequences of a tear of the posterior root of the medial meniscus Surgical technique. J Bone Joint Surg Am. 2009;91(Suppl 2):257–70. doi: 10.2106/JBJS.I.00500. [DOI] [PubMed] [Google Scholar]
- 30.LaPrade CM, LaPrade MD, Turnbull TL, Wijdicks CA, LaPrade RF. Biomechanical evaluation of the transtibial pull-out technique for posterior medial meniscal root repairs using 1 and 2 transtibial bone tunnels. Am J Sports Med. 2015;43(4):899–904. doi: 10.1177/0363546514563278. [DOI] [PubMed] [Google Scholar]
- 31.Feucht MJ, Grande E, Brunhuber J, Rosenstiel N, Burgkart R, Imhoff AB, et al. Biomechanical comparison between suture anchor and transtibial pull-out repair for posterior medial meniscus root tears. Am J Sports Med. 2014;42(1):187–93. doi: 10.1177/0363546513502946. [DOI] [PubMed] [Google Scholar]
- 32.Bhatia S, LaPrade CM, Ellman MB, LaPrade RF. Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med. 2014;42(12):3016–30. doi: 10.1177/0363546514524162. [DOI] [PubMed] [Google Scholar]
- 33.Kim YJ, Kim JG, Chang SH, Shim JC, Kim SB, Lee MY. Posterior root tear of the medial meniscus in multiple knee ligament injuries. Knee. 2010;17(5):324–8. doi: 10.1016/j.knee.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 34.Jones AO, Houang MT, Low RS, Wood DG. Medial meniscus posterior root attachment injury and degeneration: MRI findings. Australas Radiol. 2006;50(4):306–13. doi: 10.1111/j.1440-1673.2006.01586.x. [DOI] [PubMed] [Google Scholar]
- 35.Ozkoc G, Circi E, Gonc U, Irgit K, Pourbagher A, Tandogan RN. Radial tears in the root of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc. 2008;16(9):849–54. doi: 10.1007/s00167-008-0569-z. [DOI] [PubMed] [Google Scholar]
- 36.Bin SI, Kim JM, Shin SJ. Radial tears of the posterior horn of the medial meniscus. Arthroscopy. 2004;20(4):373–8. doi: 10.1016/j.arthro.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 37.Hwang BY, Kim SJ, Lee SW, Lee HE, Lee CK, Hunter DJ, et al. Risk factors for medial meniscus posterior root tear. Am J Sports Med. 2012;40(7):1606–10. doi: 10.1177/0363546512447792. [DOI] [PubMed] [Google Scholar]
- 38.Thompson WO, Thaete FL, Fu FH, Dye SF. Tibial meniscal dynamics using three-dimensional reconstruction of magnetic resonance images. Am J Sports Med. 1991;19(3):210–5. doi: 10.1177/036354659101900302. [DOI] [PubMed] [Google Scholar]
- 39.Brody JM, Lin HM, Hulstyn MJ, Tung GA. Lateral meniscus root tear and meniscus extrusion with anterior cruciate ligament tear. Radiology. 2006;239(3):805–10. doi: 10.1148/radiol.2393050559. [DOI] [PubMed] [Google Scholar]
- 40.Kim YM, Rhee KJ, Lee JK, Hwang DS, Yang JY, Kim SJ. Arthroscopic pullout repair of a complete radial tear of the tibial attachment site of the medial meniscus posterior horn. Arthroscopy. 2006;22(7):e1–4. doi: 10.1016/j.arthro.2005.12.040. [DOI] [PubMed] [Google Scholar]
- 41.Robertson DD, Armfield DR, Towers JD, Irrgang JJ, Maloney WJ, Harner CD. Meniscal root injury and spontaneous osteonecrosis of the knee: an observation. J Bone Joint Surg Br. 2009;91(2):190–5. doi: 10.1302/0301-620X.91B2.21097. [DOI] [PubMed] [Google Scholar]
- 42.LaPrade RF, Arendt EA, Getgood A, Faucett SC. The menisci. Berlin, Heidelberg: Springer Berlin Heidelberg; 2017. [Google Scholar]
- 43.Lee JH, Lim YJ, Kim KB, Kim KH, Song JH. Arthroscopic pullout suture repair of posterior root tear of the medial meniscus: radiographic and clinical results with a 2-year follow-up. Arthroscopy. 2009;25(9):951–8. doi: 10.1016/j.arthro.2009.03.018. [DOI] [PubMed] [Google Scholar]
- 44.Lee DW, Ha JK, Kim JG. Medial meniscus posterior root tear: a comprehensive review. Knee Surg Relat Res. 2014;26(3):125–34. doi: 10.5792/ksrr.2014.26.3.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kim JH, Chung JH, Lee DH, Lee YS, Kim JR, Ryu KJ. Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: A prospective comparison study. Arthroscopy. 2011;27(12):1644–53. doi: 10.1016/j.arthro.2011.06.033. [DOI] [PubMed] [Google Scholar]
- 46.Seil R, Dück K, Pape D. A clinical sign to detect root avulsions of the posterior horn of the medial meniscus. Knee Sports Surg Traumatol Arthrosc. 2011;19(12):2072–5. doi: 10.1007/s00167-011-1550-9. [DOI] [PubMed] [Google Scholar]
- 47.LaPrade CM, James EW, Cram TR, Feagin JA, Engebretsen L, LaPrade RF. Meniscal root tears: a classification system based on tear morphology. Am J Sports Med. 2015;43(2):363–9. doi: 10.1177/0363546514559684. [DOI] [PubMed] [Google Scholar]
- 48.Forkel P, Foehr P, Meyer JC, Herbst E, Petersen W, Brucker PU, et al. Biomechanical and viscoelastic properties of different posterior meniscal root fixation techniques. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):403–10. doi: 10.1007/s00167-016-4237-4. [DOI] [PubMed] [Google Scholar]
- 49.De Smet AA, Blankenbaker DG, Kijowski R, Graf BK, Shinki K. MR diagnosis of posterior root tears of the lateral meniscus using arthroscopy as the reference standard. AJR Am J Roentgenol. 2009;192(2):480–6. doi: 10.2214/AJR.08.1300. [DOI] [PubMed] [Google Scholar]
- 50.Harper KW, Helms CA, Lambert HS, Higgins LD. Radial meniscal tears: significance, incidence, and MR appearance. AJR Am J Roentgenol. 2005;185(6):1429–34. doi: 10.2214/AJR.04.1024. [DOI] [PubMed] [Google Scholar]
- 51.Choi SH, Bae S, Ji SK, Chang MJ. The MRI findings of meniscal root tear of the medial meniscus: emphasis on coronal, sagittal and axial images. Knee Surg Sports Traumatol Arthrosc. 2012;20(10):2098–103. doi: 10.1007/s00167-011-1794-4. [DOI] [PubMed] [Google Scholar]
- 52.Lee SY, Jee WH, Kim JM. Radial tear of the medial meniscal root: reliability and accuracy of MRI for diagnosis. AJR Am J Roentgenol. 2008;191(1):81–5. doi: 10.2214/AJR.07.2945. [DOI] [PubMed] [Google Scholar]
- 53.Lerer DB, Umans HR, Hu MX, Jones MH. The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol. 2004;33(10):569–74. doi: 10.1007/s00256-004-0761-2. [DOI] [PubMed] [Google Scholar]
- 54.Costa CR, Morrison WB, Carrino JA. Medial meniscus extrusion on knee MRI: is extent associated with severity of degeneration or type of tear? AJR Am J Roentgenol. 2004;183(1):17–23. doi: 10.2214/ajr.183.1.1830017. [DOI] [PubMed] [Google Scholar]
- 55.Chahla J, Moulton SG, LaPrade CM, Dean CS, LaPrade RF. Posterior meniscal root repair: the transtibial double tunnel pullout technique. Arthrosc Tech. 2016;5(2):e291–6. doi: 10.1016/j.eats.2016.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Choi NH, Son KM, Victoroff BN. Arthroscopic all-inside repair for a tear of posterior root of the medial meniscus: a technical note. Knee Surg Sports Traumatol Arthrosc. 2008;16(9):891–3. doi: 10.1007/s00167-008-0581-3. [DOI] [PubMed] [Google Scholar]
- 57.Kim JH, Shin DE, Dan JM, Nam KS, Ahn TK, Lee DH. Arthroscopic suture anchor repair of posterior root attachment injury in medial meniscus: technical note. Arch Orthop Trauma Surg. 2009;129(8):1085–8. doi: 10.1007/s00402-008-0810-8. [DOI] [PubMed] [Google Scholar]
- 58.Jung YH, Choi NH, Oh JS, Victoroff BN. All-Inside repair for a root tear of the medial meniscus using a suture anchor. Am J Sports Med. 2012;40(6):1406–11. doi: 10.1177/0363546512439181. [DOI] [PubMed] [Google Scholar]
- 59.Raustol OA, Poelstra KA, Chhabra A, Diduch DR. The meniscal ossicle revisited: etiology and an arthroscopic technique for treatment. Arthroscopy. 2006;22(6):e1–3. doi: 10.1016/j.arthro.2005.12.022. [DOI] [PubMed] [Google Scholar]
- 60.Ahn JH, Wang JH, Yoo JC, Noh HK, Park JH. A pull out suture for transection of the posterior horn of the medial meniscus: using a posterior trans-septal portal. Knee Surg Sports Traumatol Arthrosc. 2007;15(12):1510–3. doi: 10.1007/s00167-007-0310-3. [DOI] [PubMed] [Google Scholar]
- 61.Nicholas SJ, Golant A, Schachter AK, Lee SJ. A new surgical technique for arthroscopic repair of the meniscus root tear. Knee Surg Sports Traumatol Arthrosc. 2009;17(12):1433–6. doi: 10.1007/s00167-009-0874-1. [DOI] [PubMed] [Google Scholar]
- 62.Feucht MJ, Grande E, Brunhuber J, Rosenstiel N, Burgkart R, Imhoff AB, et al. Biomechanical evaluation of different suture materials for arthroscopic transtibial pull-out repair of posterior meniscus root tears. Knee Surg Sport Traumatol Arthrosc. 2013;23(1):132–9. doi: 10.1007/s00167-013-2656-z. [DOI] [PubMed] [Google Scholar]
- 63.Krych AJ, Johnson NR, Mohan R, Dahm DL, Levy BA, Stuart MJ. Partial meniscectomy provides no benefit for symptomatic degenerative medial meniscus posterior root tears. Knee Surg Sports Traumatol Arthrosc. 2017;26(4):1117–22. doi: 10.1007/s00167-017-4454-5. [DOI] [PubMed] [Google Scholar]
- 64.Feucht MJ, Kühle J, Bode G, Mehl J, Schmal H, Südkamp NP, et al. Arthroscopic transtibial pullout repair for posterior medial meniscus root tears: a systematic review of clinical, radiographic, and second-look arthroscopic results. Arthroscopy. 2015;31(9):1808–16. doi: 10.1016/j.arthro.2015.03.022. [DOI] [PubMed] [Google Scholar]
- 65.Kim SB, Ha JK, Lee SW, Kim DW, Shim JC, Kim JG, et al. Medial meniscus root tear refixation: Comparison of clinical, radiologic, and arthroscopic findings with medial meniscectomy. Arthroscopy. 2011;27(3):346–54. doi: 10.1016/j.arthro.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 66.LaPrade RF, Matheny LM, Moulton SG, James EW, Dean CS. Posterior meniscal root repairs: outcomes of an anatomic transtibial pull-out technique. Am J Sports Med. 2017;45(4):884–91. doi: 10.1177/0363546516673996. [DOI] [PubMed] [Google Scholar]
- 67.Moon HK, Koh YG, Kim YC, Park YS, Jo SB, Kwon SK. Prognostic factors of arthroscopic pull-out repair for a posterior root tear of the medial meniscus. Am J Sports Med. 2012;40(5):1138–43. doi: 10.1177/0363546511435622. [DOI] [PubMed] [Google Scholar]
- 68.Seo HS, Lee SC, Jung KA. Second-look arthroscopic findings after repairs of posterior root tears of the medial meniscus. Am J Sports Med. 2011;39(1):99–107. doi: 10.1177/0363546510382225. [DOI] [PubMed] [Google Scholar]