Abstract
Background:
Silicone breast implants have been used for decades for cosmetic breast augmentation or reconstruction after mastectomy. In selected cases, postmastectomy adjuvant radiotherapy is given with the breast implants in situ. Previous clinical studies have shown that radiotherapy may lead to complications such as capsular contracture and infection and that removal of the implant may be required. Yet, the effect of radiotherapy on silicone breast implants themselves is unknown. The aim of this study was to investigate if irradiation of breast implants influences their mechanical properties.
Methods:
This was an ex vivo study on 32 ready-to-use silicone breast implants (Mentor and Silimed). Half of the implants of each brand were irradiated with 1 × 60 Gy, the other half were not irradiated. Tensile, mechanical hysteresis, and rheology tests were performed. Differences in mechanical properties between the irradiated and nonirradiated implants were determined.
Results:
No significant differences were found in tensile strength, mechanical hysteresis, and rheological properties between irradiated and nonirradiated implants.
Conclusions:
Breast implants’ mechanical properties for these 2 brands were not significantly affected after single-dose irradiation in an ex vivo setting.
INTRODUCTION
Implant-based breast reconstruction is 1 of the most frequently performed operations in breast cancer patients who undergo a mastectomy and adjuvant radiotherapy.1–4 Patients who choose to undergo an immediate breast reconstruction might receive adjuvant radiotherapy with an implant in situ.1 The latter strategy may lead to several clinical complications. For example, capsular contracture, hematoma, infection, necrosis, or extrusion,5–10 inferior cosmetic results of the breast reconstruction6,8,10 but also a significantly higher reconstruction failure compared with the nonirradiated patients.8,9,11
It is unknown if such complications are caused by tissue reactions, by a damaged implant due to radiotherapy, or by a combination of the 2. Multiple studies have shown that ionizing irradiation can affect the mechanical properties of silicone materials on both a microscopic (eg, scission and crosslinking reactions), and a macroscopic level (eg, increase of hardness and reduced tear strength).12–14
However, such studies have been performed with sterilizing doses (eg, several kGy). In clinical practice, breast implants may typically receive total doses of up to about 60 Gy only. Although the chemical environment of the implant in-vivo, combined with radiotherapy, may influence the mechanical properties, we cannot simulate this. We therefore studied the effect of radiation on macroscopic mechanical properties of silicone breast implants in an ex vivo setting.
MATERIALS AND METHODS
Implants
An ex vivo study was performed on 32 ready-to-use silicone breast implants. Implants were kindly provided by Mentor (Mentor, CPG331 Gel Breast Implant, Cohesive III, Leiden, The Netherlands) and Silimed (Silimed, Polyurethane, Rio de Janeiro, Brazil). Implants from each manufacturer were equally distributed into 2 groups (n = 8): 1 group was irradiated and the other remained untreated (Fig. 1). Subsequently, all implants underwent mechanical testing consisting of tensile and mechanical hysteresis tests on the shell and a rheometric test on the gel filling.
Fig. 1.
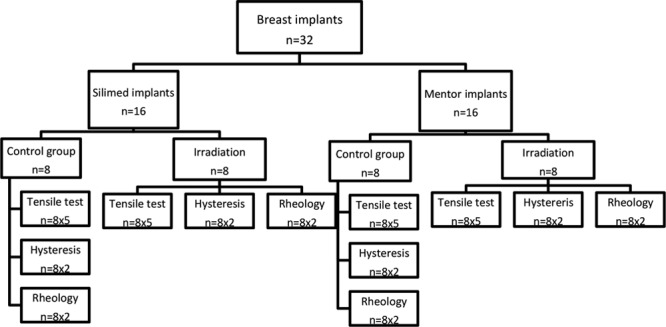
Overview of experiments and number of samples used in each test. n, number of implants tested.
Irradiation
Irradiation took place in a 30 × 30 × 30 cm3 water phantom at room temperature (about 25°C). A Varian TrueBeam linear accelerator delivered 2 opposing 15 MV beams of equal weight and 40 × 30 cm2 field size with the isocenter set to the geometrical center of the phantom. A homogeneous dose of 60 Gy ± 5% was delivered in a single fraction. Clinically, such a dose is delivered in 16 fractions to facilitate normal tissue repair after radiation. But because silicone implants consist of nonliving gel material, repair mechanisms are not present, allowing a single fraction rather than fractionated irradiation, to be used.
Sample Preparation
After irradiation, the implants were disassembled, the gel was removed from the shell, and put in labeled air-tight bags. The gel was minimally disturbed to prevent air entrapment, and care was taken to avoid stretching or compression of the shell. Ethanol (70%) was used to clean the shell before it was transferred to similarly labeled bags.
Mechanical Tests
The mechanical tests were performed according to the Organization for Standardization (ISO) 37 and ISO 14607 standards (ISO 37 for rubber, vulcanized or thermoplastic-Determination of tensile stress-strain properties15 and ISO 14607 for nonactive surgical implants- Mammary implants- Particular requirements).16 To assess unambiguously measured radiation-induced effects on the shell and the gel, appropriate tests were selected for each of these components.
Shell Tests
Tensile Test
Dumb bell–shaped test samples were cut from the shells using a cutting press according to ISO 37.15 For each implant brand 8 irradiated and 8 nonirradiated shells were evaluated with 5 samples randomly selected and tested from each shell. All specimens were cut at ± 20°C. The thickness of the specimens was determined using a digital thickness meter. The tensile tests were performed using the Zwick/Roell BZ 1.0/TH1S tensile testing frame (Zwick/Roell, Ulm, Germany). Samples were tested up to failure, while recording force and elongation. A force-elongation curve was subsequently plotted for each test. The breaking force (N), elongation at break (mm), strain (%), and the elastic modulus (N/mm) were calculated for each specimen. Data from all 5 samples of each implant were averaged.
Mechanical Hysteresis Test
Specimens were again cut in accordance with ISO 37 (type 2).15 For each implant brand, 8 irradiated and 8 nonirradiated shells were evaluated with 2 samples randomly selected and tested from each shell. The test was performed under the same conditions as the tensile test. After measuring the thickness, each specimen was marked with 2 black dots that allowed accurate tracking of the strain. The elongation of the sample was performed using an Instron 3343 video extensometer. A mechanical hysteresis test with 10%, 30%, and 50% elongation of the sample was performed, and each level was tested 3 times. The position of the black marks on the sample was recorded with a digital camera and analyzed with approximately 10 data points/sample. Strain was calculated from the difference between mark separation at the start of the test (gauge length) and at 10%, 30%, and 50% elongation. Tracking the center of the mark eliminated possible errors caused by stretching of the marks at high elongations. Maximum force (N) was derived at 10%, 30%, and 50% elongation, and the work (N·mm) needed was calculated using the area under the curve (AUC). Stretch speed was 0.5 mm/s. Force after specimen insertion was between −1 and 0 N. Preload was 0.001 N. After reaching the desired strain at each level, the tensile tester decreased the strain until the force reached 0 N.
Gel Test
Rheology
To test the silicone gel cohesion, an ISO-standards test is used by the manufacturer. This test involves filling a funnel-like apparatus with silicone gel.16 The specimen meets the requirements of the test if there is no separation of the gel, and the projection length is ≤ 30 mm. We found no projection at all after 24 hours for both brands of irradiated and nonirradiated implants. To obtain a quantitative comparison on the effect of irradiation on the silicone gel, we performed a rheology test to test gel cohesion. This test provides more information than the test proposed by the ISO-standard, as it quantifies the silicone gel stiffness and its viscous behavior at a range of physiologically relevant frequencies, rather than a flow test at zero frequency. Rheology measurements were performed on a rheometer (Anton Paar, Physica MCR501, Graz, Austria) using a stainless steel cone-plate measurement geometry consisting of a circular bottom plate and a concentric top plate with a 30 mm radius and 1°-cone angle. For each brand, 8 irradiated and 8 nonirradiated breast implants were assessed, and for every implant, 2 random samples were tested. Samples were placed in the center of the bottom plate and the cone was lowered into position. The normal force was subsequently allowed to relax to a constant value. The mechanical properties [the storage modulus (G’), indicating the elasticity of the material and the loss modulus (G’’) indicating its viscous behavior] were measured by applying a small oscillatory shear strain with an amplitude of 0.5%. The frequency of the oscillation was logarithmically varied from 0.01–10 Hz to probe the time-dependence of the viscoelastic properties. To reduce the effect of sample-to-sample variability caused by slight differences in the volume of the loaded material, the damping factor (tanδ) was calculated. This is the ratio between the storage modulus (G’) and the loss modulus (G’’).
 |
The damping factor was calculated at different angular frequencies (rad/s) to determine the behavior of the gel in the so-called frequency sweep.
Statistical Analysis
For each experiment, the mean and SD were calculated. The Kolomochorov–Smirnov normality test was performed to test for normal distribution. Statistical significance was tested using unpaired t tests for a normal distribution and the Mann–Whitney U test for nonnormal distributions. P values < 0.05 were considered significant. Statistical tests were carried out using SPSS 20.0 (IBM Corp. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.)
RESULTS
Implant Characteristics
All irradiated and nonirradiated implants were volume and type matched.
Shell Tests
Tensile Test
Figure 2 shows the average outcomes of the tensile test for the 2 types of irradiated and nonirradiated implants. No significant differences were observed in the breaking force, elongation at break, strain, thickness, and the elastic modulus between the irradiated and nonirradiated implants for both manufacturers (Table 1).
Fig. 2.
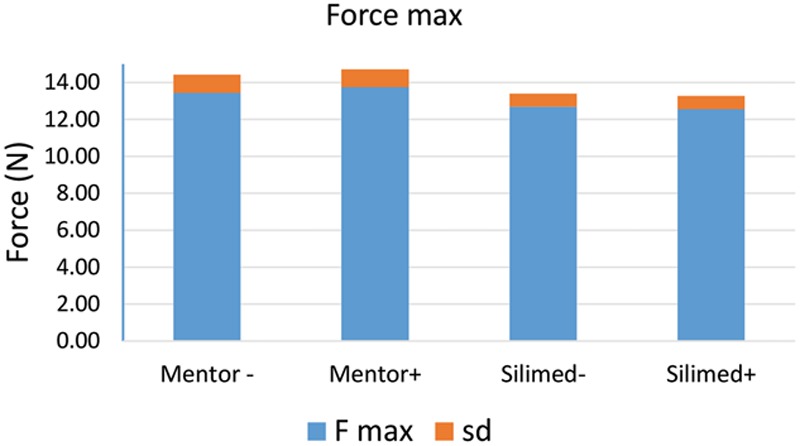
Measured effect of irradiation on the strength of the shell of Mentor (P = 0.34) and Silimed (P = 0.44) breast implants. N, force in Newton; −, nonirradiated implants; +, irradiated implants; dark gray, mean; light gray, SD.
Table 1.
Summarized Irradiation Effects on the Failure Force on Mentor and Silimed Breast Implants

Mechanical Hysteresis Test
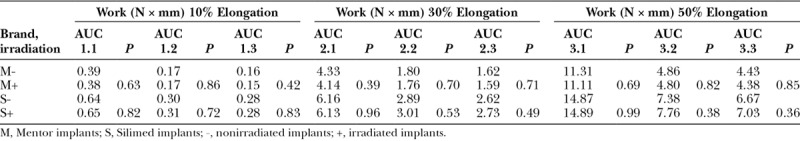
Figure 3 shows the maximum force (N) used for every cycle at 10%, 30%, and 50% elongation, whereas Figure 4 shows the work needed for every cycle. A summary of these results (average results per manufacturer) is shown in Tables 2, 3. No significant differences between the irradiated and nonirradiated implants of both manufacturers were observed in the maximum force used for elongation or the work.
Fig. 3.
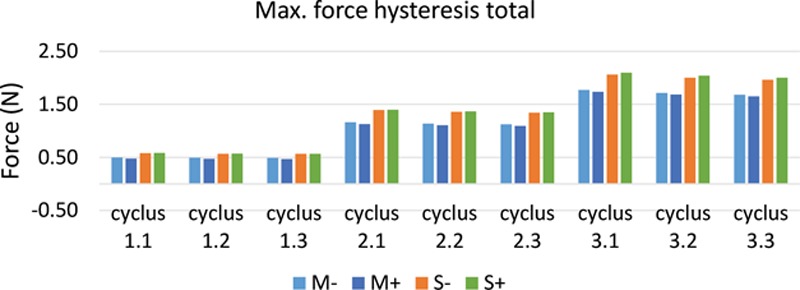
Measured effect of irradiation on the force needed to elongate the samples up to 10% (cyclus 1), 30% (cyclus 2), and 50% (cyclus 3) on Mentor and Silimed breast implants. Each level was tested 3 times. The P value for the Mentor implants varies between 0.37 and 0.70 for the 3 cycles and 0.75–0.96 for the Silimed implants. N, force in Newton; M, Mentor; S, Silimed; −, nonirradiated implants; +, irradiated implants.
Fig. 4.
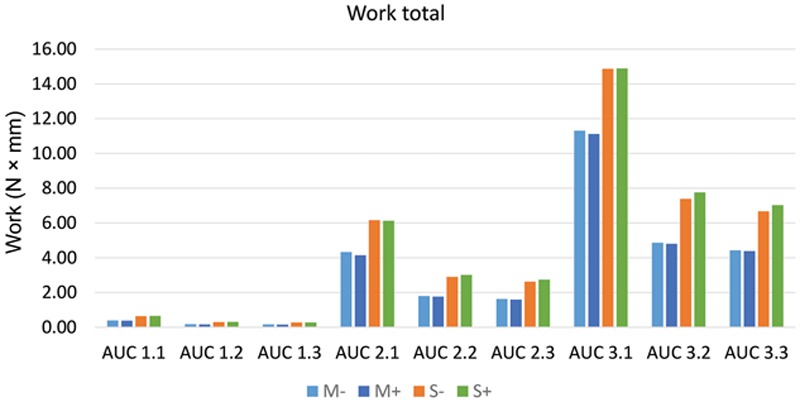
Measured effect of irradiation on the work (N·mm) needed to elongate the samples up to 10% (cyclus 1), 30% (cyclus 2), and 50% (cyclus 3) on Mentor and Silimed breast implants. Each level was tested 3 times. The P value for the Mentor implants varies between 0.39 and 0.86 for the 3 cycles and 0.38–0.96 for the Silimed implants. N, Force in Newton; mm, distance in millimeter; M, Mentor; S, Silimed; −, nonirradiated implants; +, irradiated implants.
Table 2.
Summarized Irradiation Effects of the Force Needed to Elongate the Specimens up to 10% (Cyclus 1), 30% (Cyclus 2), and 50% (Cyclus 3), Averaged Over 3 Separate Tests
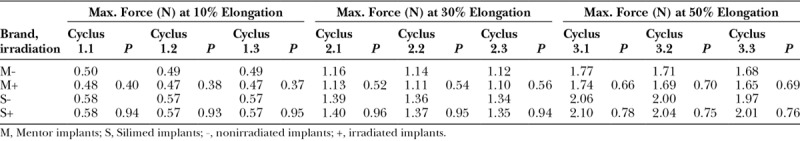
Table 3.
Summarized Irradiation Effects of the Force Needed to Elongate the Specimens up to 10% (Cyclus 1), 30% (Cyclus 2), and 50% (Cyclus 3), Averaged Over 3 Separate Tests
Gel Test
Rheology
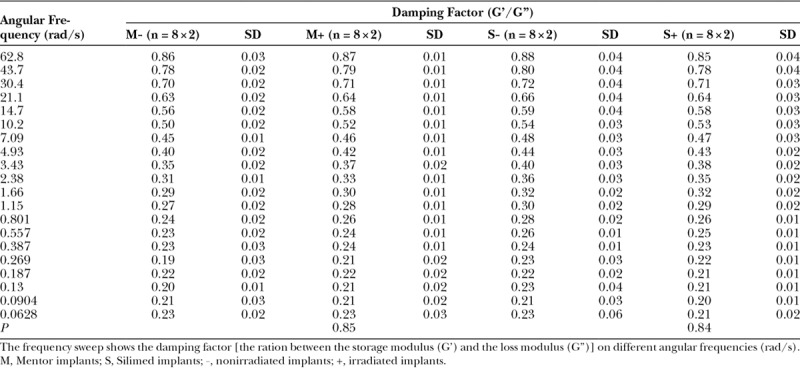
Figure 5 provides the results of the frequency sweep for the 2 brands. In the frequency sweep, we see a clear dependence of the damping factor—the ratio between storage and loss moduli—on the frequency of the oscillation. At low frequency (0.01 Hz), the storage modulus, representing elastic, solid-like behavior, is an order of magnitude higher than the loss modulus, representing viscous behavior, as indicated by a small value of tan (δ). At high frequency (10 Hz), the 2 moduli approach each other, indicating the vicinity of the cross-over from elastic behavior (low frequencies, G’ dominates) to viscous behavior (high frequencies, G’’ dominates). No significant differences over the entire frequency range in the viscoelastic properties of the irradiated and nonirradiated implants were found for both manufacturers (Table 4).
Fig. 5.

Measured effect of irradiation on the frequency sweep of Mentor (average P = 0.85) and Silimed (average P = 0.84) breast implants. The frequency sweep shows the damping factor tan(δ) [the ration between the storage modulus (G’) and the loss modulus (G’’)] on different angular frequencies (rad/s). Rad, radius; M, Mentor; S, Silimed; −, nonirradiated implants; +, irradiated implants.
Table 4.
Summarized Irradiation Effects on the Average Frequency Sweep of Mentor and Silimed Breast Implants, Averaged 2 Random Samples
DISCUSSION
In this study, the effect of a single dose of 60 Gy ionizing radiation on silicone breast implants in an ex vivo setting was investigated. Three mechanical tests on both irradiated and nonirradiated silicone breast implants were performed. Macroscopic mechanical properties of the outer shell and the gel were found not to differ significantly between irradiated and nonirradiated implants, and rheology tests also showed no significant change in the mechanical behavior of the gel after irradiation.
Traeger and Castonguay14 studied the effect of γ-radiation (up to 1 MGy) on the dynamic mechanical properties of silicone rubbers. They found an increase in the hardness (up to 170%) of silicone rubbers after irradiation. In our study, we did not observe significant changes in the tensile tests or mechanical hysteresis tests. It is possible that microscopic changes occur that are too small to be detected by these mechanical tests. We used the ISO 37 (for rubbers) and the ISO 14607 (for breast implants), but these standards are designed to provide a minimum threshold for implants to be approved for medical use. This threshold might be too crude to detect any possible (small) changes due to radiotherapy.
Gautriaud et al.12 also investigated the effect of γ-radiation for sterilization of silicone rubbers resulting in an increase of hardness, durometer and tensile modulus, and a reduction of tear strength of silicone rubber. However, both Gautriaud et al.12 and Treager and Castonguay14 used doses at least 1,000 times than 60 Gy. A local dose of 10 kGy irradiating breast cancer is necrotic, even when fractionated. Given at once, the patient will die immediately as the total body dose (1% of the dose locally delivered) far exceeds the tolerance level.
A recent review11 that included 12 studies showed that postmastectomy adjuvant radiation therapy leads to5: a significantly higher reconstruction failure rate (18.6% versus 3.1%),6 a higher rate of capsular contracture (1.3–15% versus 0–12%) and12 worse cosmetic outcomes. In addition, higher rates of complications such as hematoma,6,9 infection,5,6,9 seroma,5 necrosis,5,6,9 implant extrusion5,6,9 implant leakage,6 and implant luxation9 after irradiation have been reported. However, most of the available studies are retrospective cohort studies, and prospective data are lacking. Ideally, our experiment would have been carried out in vivo, but for obvious reasons, this is not possible and simulating exact physiological conditions was also not possible either because of complexity and lack of knowledge. Therefore, we were limited to studying the effects of ionizing irradiation on the silicone materials. To meet in vivo situation as good as possible, we used a water phantom although this was at room temperature, whereas 37°C would have been more consistent with in vivo conditions. However, temperature is not important for irradiation-induced damage. The implants were irradiated with 60 Gy in a single fraction, whereas typically, patients receive up to 60 Gy in multiple fractions. From an energetic point of view, a fractionated dose of 60 Gy equals that dose given at once. The reason we chose a single fraction is 2-fold. First, 1 reason for fractionation is that it is designed to take advantage of differences in the repair mechanism between healthy and cancerous tissue. There is, however, no repair mechanism in silicone breast implants because this is nonliving matter and so it is not necessary to fractionate. Second, the chance of irradiation induced destruction is higher when many chemically reactive structures are created per time period. In this analysis, the interval between irradiation and mechanical testing was only 2 months. In a patient, the longer term in vivo chemical environment around the implant, combined with radiotherapy might also influence the mechanical properties of the implant. Since we were unable to assess this in our experiment, a relatively short interval was considered acceptable.
Further research is needed to investigate the effects of irradiating breast implants in situ. We therefore suggest testing and comparing the mechanical properties of irradiated and nonirradiated breast implants that have had to be removed from the patient. Furthermore, it is important to (immuno)histologically investigate removed capsules that have been irradiated to understand the pathogenesis of implant-based reconstruction failure after irradiation. It is also important to perform a prospective study investigating the reason and numbers of explanation in nonirradiated and irradiated breast implants.
CONCLUSIONS
This ex vivo study demonstrated no difference in mechanical properties between irradiated and nonirradiated breast implants after a single fraction of radiation, with an absolute total dose comparable with what is clinically used in fractionated regimes. This suggests that it is safe to irradiate breast implants in terms of affecting the mechanical properties. Further research, however, is needed to investigate the effect of radiation on breast implants in situ.
Footnotes
Published online 13 July 2018.
Presented at the Barcelona Breast Meeting, March 2016, Barcelona, Spain.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Lyons JA, Sherertz T. Postmastectomy radiation therapy. Curr Oncol Rep. 2014;16:361. [DOI] [PubMed] [Google Scholar]
- 2.Overgaard M, Jensen MB, Overgaard J, et al. Postoperative radiotherapy in high-risk postmenopausal breast-cancer patients given adjuvant tamoxifen: Danish Breast Cancer Cooperative Group DBCG 82c randomised trial. Lancet. 1999;353:1641. [DOI] [PubMed] [Google Scholar]
- 3.Ragaz J, Jackson SM, Le N, et al. Adjuvant radiotherapy and chemotherapy in node-positive premenopausal women with breast cancer. N Engl J Med. 1997;337:956. [DOI] [PubMed] [Google Scholar]
- 4.Roje Z, Roje Z, Janković S, et al. Breast reconstruction after mastectomy. Coll Antropol. 2010;34:113. [PubMed] [Google Scholar]
- 5.Ascherman JA, Hanasono MM, Newman MI, et al. Implant reconstruction in breast cancer patients treated with radiation therapy. Plast Reconstr Surg. 2006;117:359. [DOI] [PubMed] [Google Scholar]
- 6.Cordeiro PG, Pusic AL, Disa JJ, et al. Irradiation after immediate tissue expander/implant breast reconstruction: outcomes, complications, aesthetic results, and satisfaction among 156 patients. Plast Reconstr Surg. 2004;113:877. [DOI] [PubMed] [Google Scholar]
- 7.Jhaveri JD, Rush SC, Kostroff K, et al. Clinical outcomes of postmastectomy radiation therapy after immediate breast reconstruction. Int J Radiat Oncol Biol Phys. 2008;72:859. [DOI] [PubMed] [Google Scholar]
- 8.Nava MB, Pennati AE, Lozza L, et al. Outcome of different timings of radiotherapy in implant-based breast reconstructions. Plast Reconstr Surg. 2011;128:353. [DOI] [PubMed] [Google Scholar]
- 9.Tallet AV, Salem N, Moutardier V, et al. Radiotherapy and immediate two-stage breast reconstruction with a tissue expander and implant: complications and esthetic results. Int J Radiat Oncol Biol Phys. 2003;57:136. [DOI] [PubMed] [Google Scholar]
- 10.Vandeweyer E, Deraemaecker R. Radiation therapy after immediate breast reconstruction with implants. Plast Reconstr Surg. 2000;106:56; discussion 59. [DOI] [PubMed] [Google Scholar]
- 11.Lam TC, Hsieh F, Boyages J. The effects of postmastectomy adjuvant radiotherapy on immediate two-stage prosthetic breast reconstruction: a systematic review. Plast Reconstr Surg. 2013;132:511. [DOI] [PubMed] [Google Scholar]
- 12.Gautriaud E, Stafford KT, Adamchuk J, et al. Effect of sterilization on the mechanical properties of silicone rubbers. 2017;1.
- 13.Palsule AS, Clarson SJ, Widenhouse CW. Gamma irradiation of silicones. J Inorg Organomet Polym. 2008;18:207. [Google Scholar]
- 14.Traeger RK, Castonguay TT. Effect of gamma-radiation on the dynamic mechanical properties of silicone rubbers. J Appl Polymer Sci. 1966;10:535. [Google Scholar]
- 15.International Standard ISO 37. Rubber, vulcanized or thermoplastic—determination of tensile stress-strain properties. 2011.
- 16.International Standard ISO 14607. Non-active surgical implants—mammary implants—particular requirements. 2007.


