Supplemental Digital Content is available in the text.
Summary:
Vasospastic disorders in the hand have been treated with surgical sympathectomy and recently with botulinum toxin A (BTX) injections in the palm. The purpose of this study was to evaluate if it is possible to obtain precise administration of BTX around the radial artery using a single ultrasound-guided injection. We present a novel technique using 1 single ultrasound-guided BTX injection around the radial artery to treat vasospastic symptoms. Ten patients were included in a pilot study. All patients were referred by a rheumatologist after been diagnosed with primary or secondary Raynaud. Under ultrasound guidance, BTX was injected around the radial artery and its comitant veins 3–5 cm proximal to the wrist. Ultrasound-guided injection of BTX allowed for a precise distribution of BTX into the perivascular space of the radial artery and its comitant veins. Intravascular injection could easily be excluded. One patient reported temporary reduced grip strength, most likely due to leakage of BTX to the flexor pollicis longus muscle. No other complications were registered. All patients reported reduced number of vasospastic episodes, warmer hands, and reduced pain. Ultrasound-guided injection enables precise administration of BTX in the space surrounding the radial artery and its comitant veins. This novel approach could be a promising treatment for vasospastic disorders of the hands in patients with primary and secondary Raynaud.
INTRODUCTION
Patients with primary and secondary Raynaud suffer from episodes of vasospasm, often caused by exposure to low temperatures or emotional distress. The vasospasm causes impaired blood circulation to the hands and is associated with pain, paresthesia, and cold hands. In some patients, it may even result in nonhealing ulcers at the fingertips.1 Cold sensitivity is another frequently reported complaint.2
Recently vasospastic disorders related with Raynaud have been successfully treated with botulinum toxin (BTX) using multiple injection points in the palm of the hand. BTX is a potent vasodilator and studies indicate that the number of vasospastic episodes are reduced and that amputation can be avoided when using this technique.3 However, the multiple injections in the palm can be rather painful and can result in temporary weakness of the intrinsic muscles even when performed under ultrasound guidance.4 The purpose of this study was to evaluate if it is possible to obtain precise administration of BTX around the radial artery using a single ultrasound-guided injection at wrist level.
We present a novel method using 1 single ultrasound-guided injection of BTX in the perivascular space of the radial artery to treat vasospasms in the hands. Both the radial and ulnar artery provide arterial perfusion of the superficial and deep palmar arcs of the hand, and therefore also the digital arteries. According to Gray’s Anatomy, the radial artery leaves the superficial radial nerve 7 cm proximal to the wrist.5 Distally to this point, the radial artery has a superficial course isolated from the nerve. Theoretically, BTX injection 3–5 cm proximal to the wrist would not affect the superficial radial nerve.
METHODS
Ten adult female patients, all referred from the Department of Rheumatology with a diagnosis of primary or secondary Raynaud, were included in this prospective pilot study. All had received prior medical treatment for their vasospastic disorder of the hands. Exclusion criteria were open wounds on the fingers, former allergic reactions to BTX, pregnancy, and neurological diseases involving muscle weakness. Smokers were also excluded due to the vasoconstrictive effect of nicotine. The usefulness of our technique was evaluated by the possibility to avoid vascular penetration and to obtain a precise administration of the fluid in the perivascular space around the artery. Before injection, aspiration was performed to exclude intravascular position of the needle. After each procedure, ultrasound was used to evaluate the distribution of fluid around the artery. All patients were followed up by the authors and interviewed about the severity and number of vasospastic episodes per week at the first consultation and after 3 weeks.
With a high-frequency linear ultrasound transducer (preferably of the hockey stick type), the radial artery and comitant veins were visualized in a transverse plane 5 cm proximal to the wrist (see video, Supplemental Digital Content 1, which shows ultrasound-guided sympathetic block of the radial artery with BTX. This video is available in the “Related Video” section of the Full-Text article on PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A792).
Video Graphic 1.

See video, Supplemental Digital Content 1, which shows ultrasound-guided sympathetic block of the radial artery with BTX. This video is available in the “Related Video” section of the Full-Text article on PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A792.
To visualize both the artery and veins, one should avoid compressing the veins with the transducer. Under ultrasound-guidance, a 27G needle was advanced through the skin at the short end of the transducer. The needle tip was advanced within the visualized plane through the subcutaneous tissue, antebrachial fascia and the perivascular fascia into the perivascular space. The needle was carefully manipulated between the artery and 1 of the comitant veins (Fig. 1). The perivascular fascia is very elastic and has a tendency to follow the tip of the needle in between the vessels; therefore, the needle should be advanced deeply between the artery and vein to be sure that the fascia has been penetrated. Before injection, aspiration was performed to exclude intravascular position of the needle. When no blood was aspirated, a small test injection was performed to see that the fluid was spreading inside the perivascular space (Fig. 2). If fluid was spreading outside the perivascular space, the needle tip was repositioned. A new aspiration and test injection were performed to secure that the needle tip was correctly positioned. BTX (Allergan Botox 40 IU/mL) was injected under ultrasound guidance visualizing the fluid distributing around the artery; a total of 0.5 mL iswas injected. A high BTX concentration was used to limit leakage and diffusion to surrounding structures. The procedure was repeated at the contralateral side resulting in a total BTX dose of 40 IU per patient.
Fig. 1.
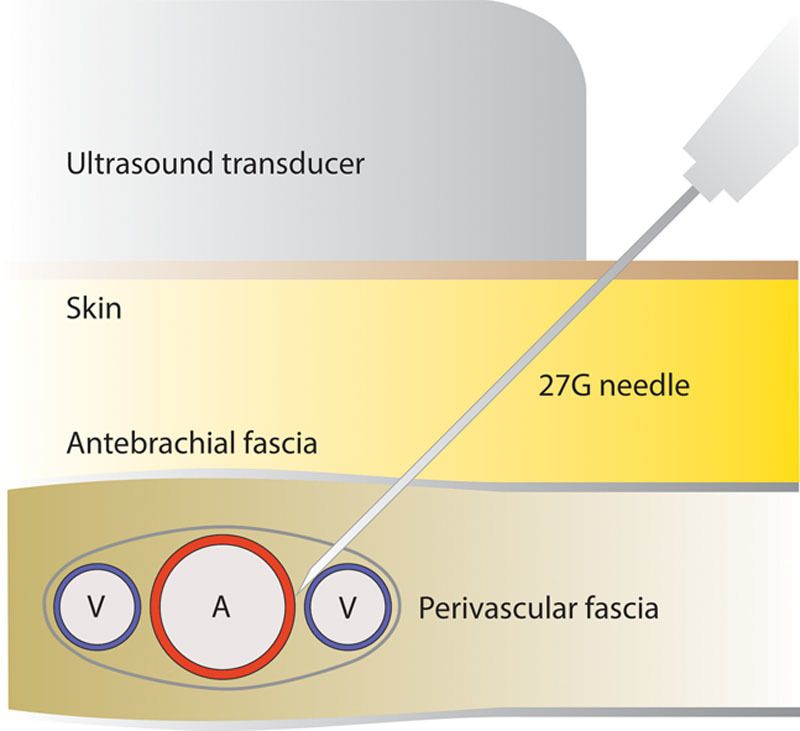
Ultrasound-guided injection in the perivascular space.
Fig. 2.
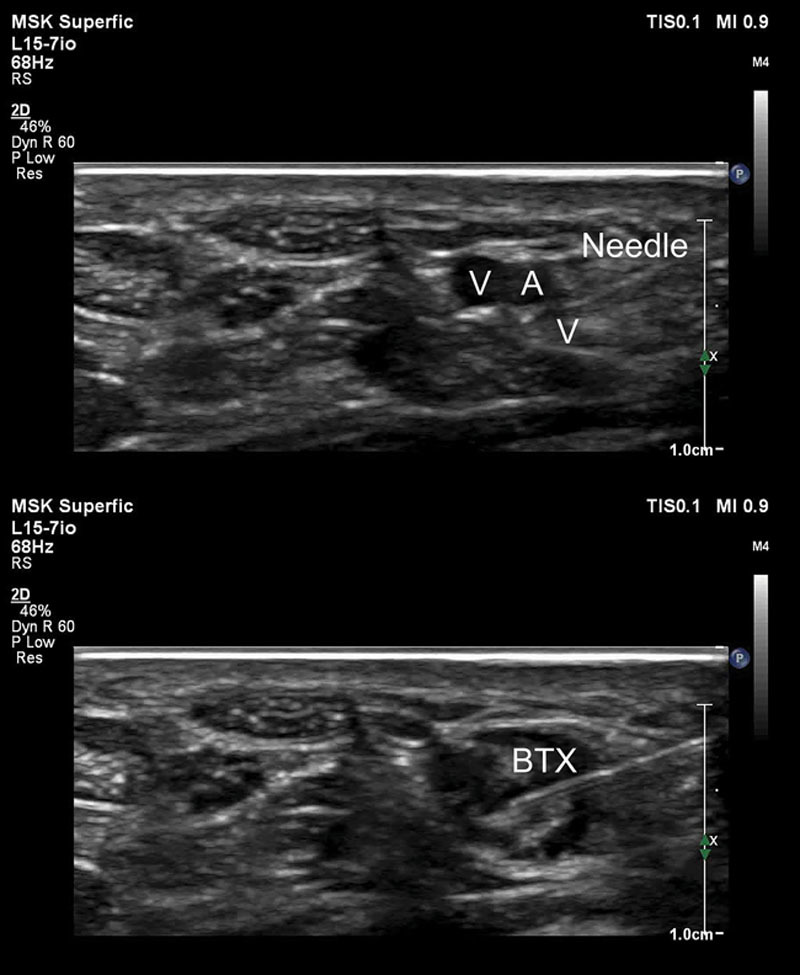
Transverse ultrasound of the radial artery (A) and veins (V) before and after perivascular injection of botulinum toxin (BTX).
RESULTS
In all cases, ultrasound confirmed that BTX was precisely administered and distributed within the perivascular space of the radial artery and comitant veins. In 1 patient, intravascular needle position occurred. In this case, a new syringe was used and the procedure was repeated uneventfully. Only 1 patient reported temporary reduced grip strength, most probably due to BTX diffusion to the flexor pollicis longus muscle.
The therapeutic effect of BTX is beyond the scope of this study. However, after 3 weeks all patients reported reduced number of vasospastic episodes, warmer hands, and reduced pain.
DISCUSSION
The treatment of the vasospastic disorders associated with primary and secondary Raynaud can be very challenging. Although surgical sympathectomy can be used successfully, it requires microsurgical skills and may cause paresthesia and intolerance to cold.6 Medical treatment with the synthetic prostaglandin analogue iloprost is also well-established. However, it requires several days of hospital stay on a regular basis.
Earlier we used multiple injections of BTX in the palm of the hand in the treatment of vasospasm in Raynaud patients as described by Neumeister.3 However, patients reported considerable discomfort and pain related to the injections at the level of the metacarpophalangeal joints. In addition, a number of patients reported temporary intrinsic muscle weakness even when multiple injections were given with ultrasound guidance.4 As the radial artery provides the dominant arterial blood supply to the hand, we postulated that a single BTX injection around the radial artery could be a valuable alternative. Our study showed that ultrasound-guided injection provided precise administration and distribution of BTX in the perivascular space with minimal risk for vascular penetration. The single injection technique around the radial artery is much less painful compared with the multiple injections in the palm of the hand. The risk of temporary intrinsic muscle weakness is minimal as BTX is not diffused to these muscles when injected proximal to the wrist. Theoretically, the vasodilator effect of BTX on the radial artery will increase blood flow to the hand in the same way as obtained with surgical sympathectomy. The radial artery and comitant veins are easily identified with ultrasound. Our experience with ultrasound-guided BTX treatment of anterior cutaneous nerve entrapment syndrome has shown that precise administration of BTX can be obtained using ultrasound guidance.7 With ultrasound-guided injection 3–5 cm proximal to the wrist the risk of BTX leakage to the superficial radial nerve is minimized. Theoretically, such leakage could result in reduced sensibility on the radiodorsal side of the hand. Nevertheless, 1 patient reported a temporary weakness of grip function, most likely due to diffusion of BTX to the flexor pollicis longus muscle.
As in surgical sympathectomy, both the ulnar and radial artery could be treated with BTX. However, the ulnar nerve accompanies the ulnar artery. Therefore, BTX injection around the ulnar artery might lead to leakage of BTX to the ulnar nerve and could theoretically cause intrinsic muscle weakness. Although one could treat both the radial and ulnar artery, our results showed a positive effect by treating only the radial artery with a single injection.
The most important limitation of this study is the small number of patients. Although all patients reported a positive effect, more research with objective evaluation of hand perfusion before and after treatment is necessary.
CONCLUSIONS
Ultrasound-guided injection of BTX in the perivascular space of the radial artery is a promising technique that provides precise administration of BTX with minimal risk of complications in patients with vasospastic disorders as primary or secondary Raynaud.
Supplementary Material
Footnotes
Published online 12 July 2018.
The publication charges for this article have been funded by a grant from the publication fund of UiT The Arctic University of Norway.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The publication charges for this article have been funded by a grant from the publication fund of UiT The Arctic University of Norway.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.Fardoun MM, Nassif J, Issa K, et al. Raynaud’s phenomenon: a brief review of the underlying mechanisms. Front Pharmacol. 2016;7:438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shapiro SC, Wigley FM. Treating Raynaud phenomenon: beyond staying warm. Cleve Clin J Med. 2017;84:797. [DOI] [PubMed] [Google Scholar]
- 3.Neumeister MW. Botulinum toxin type A in the treatment of Raynaud’s phenomenon. J Hand Surg Am. 2010;35:2085. [DOI] [PubMed] [Google Scholar]
- 4.Rajendram R, Hayward A. Ultrasound-guided digital sympathectomy using botulinum toxin. Anaesthesia. 2013;68:1077. [DOI] [PubMed] [Google Scholar]
- 5.Johnson D, Forearm EH. Standring S. In: Gray’s Anatomy The Anatomical Basis of Clinical Medicine. 2005:39 ed Edinburgh, Scotland: Elsevier Churchill Livingstone; 886. [Google Scholar]
- 6.Letamendia A, López-Román J, Bustamante-Munguira J, et al. Digital periarterial sympathectomy in the management of post-traumatic Raynaud syndrome. J Vasc Surg. 2016;63:459. [DOI] [PubMed] [Google Scholar]
- 7.Weum S, de Weerd L. Perforator-guided drug injection in the treatment of abdominal wall pain. Pain Med. 2016;17:1229. [DOI] [PubMed] [Google Scholar]


