Abstract
The current study examined developmentally informed pathways from peer victimization and exclusion to adolescent alcohol use. Using multiple informants (target and peer report of negative peer experiences) and a longitudinal sample of 387 adolescents, we examined two developmental pathways from these negative peer experiences to alcohol use, one through externalizing symptoms and the other through internalizing symptoms. When analyzed in separate models, results suggested that self-reported chronic peer victimization and exclusion were positively related to alcohol use through internalizing symptoms and coping motivated drinking. The risk pathway replicated for exclusion when using peer report of negative peer experiences. When victimization and exclusion were tested simultaneously in the same model, the risk pathway through internalizing symptoms and coping drinking motives was only supported for chronic exclusion and this finding replicated across reporters. No support was found for negative peer experiences operating through externalizing symptoms. Findings from the present study help clarify developmental pathways linking negative peer experiences to alcohol use and suggest that experiencing chronic exclusion may have a particularly deleterious impact on alcohol use during adolescence.
Keywords: Victimization, Exclusion, Externalizing and Internalizing Symptoms, Alcohol Use
Introduction
Peer victimization and exclusion are two common negative peer experiences that place adolescents at risk for the development of adjustment problems, including alcohol use (Rubin, Bukowski, & Bowker, 2015; Sullivan, Farrell, & Kliewer, 2006;). Alcohol use is typically initiated and escalates during adolescence, and it is a major health concern because it is associated with a number of maladaptive outcomes such as illicit drugs use (Hill, White, Chung, Hawkins, & Catalano, 2000) and the development of Alcohol Use Disorder (Grant et al., 2006). Despite evidence for the association between these negative peer experiences and alcohol use, only one study to date has longitudinally assessed mediational pathways linking peer victimization to alcohol use (Earnshaw et al., 2017) and no studies, to our knowledge, have assessed mediational pathways linking peer exclusion to alcohol use or examined unique effects of peer victimization and exclusion.
The current study sought to clarify the associations between negative peer experiences and alcohol use by assessing developmentally informed longitudinal pathways linking both peer victimization and exclusion to adolescent alcohol use. We focus on victimization and exclusion in early adolescence because these negative peer experiences are particularly harmful during this developmental period (LaFontana & Cillessen, 2010). Moreover, we examine alcohol use in late adolescence when drinking is common and youth are at peak risk for heavy problem drinking (Grant et al., 2006). In line with the developmental psychopathology concept of equifinality that the same problem may emerge through multiple pathways (Cicchetti & Rogosch, 1996), the current study assessed multiple mediational pathways from peer victimization and peer exclusion to adolescent alcohol use. In consideration of speculation that negative developmental sequela of peer victimization and exclusion may be similar (Buhs, Ladd, & Herald, 2006; Rubin et al., 2015), peer victimization and exclusion were included in the same models to assess unique associations with alcohol.
Negative Peer Experiences
Peer victimization and peer exclusion are two of the most common negative peer group experiences adolescents encounter (Coie, 1990). Peer victimization has been defined as being the target of any form of an aggressive attack by a similar-aged peer (e.g., being physically assaulted, being the subject of negative rumors and gossip; receiving dirty looks; Card & Hodges, 2008). Peer exclusion is the behavioral manifestation of peer rejection and refers to rejecting behaviors that isolate or keep an individual from engaging with a peer group (Buhs et al., 2006). Theoretical models suggest peer exclusion can be passive (e.g., peers do not include an adolescent in social interactions, an adolescent’s attempts to interact with peers are ignored) or active (e.g., an adolescent’s access to social activities are opposed or obstructed) (Williams, 2009). In line with these conceptualizations, studies that distinguish peer victimization and exclusion typically consider being the recipient of a physically, verbally, or relationally aggressive act as an instance of peer victimization, but not peer exclusion (e.g., Bowker, Markovic, Cogswell, & Raja, 2012; Shell, Gazelle, & Faldowski, 2014).
Although many victimized youth are also excluded, many are not, likely due to some differences in the individual child characteristics that appear to elicit peer victimization and exclusion (e.g., physical weakness has been linked to peer victimization but not exclusion; Rubin et al., 2015). Considering these subtle but important differences between peer victimization and exclusion, peer relations researchers have advocated for future research to distinguish between victimization and exclusion as they not only represent different forms of negative peer experiences but may also be differentially implicated and targeted in prevention and intervention efforts (Rubin et al., 2015).
Chronic Negative Peer Experiences
Although many adolescents experience occasional victimization and exclusion, a subset of youth suffer chronic maladaptive peer group experiences, and these youth are at high risk for negative outcomes (Pouwels, Souren, Lansu, & Cillessen, 2016). Indeed, relative to occasional victimization and exclusion, chronically victimized and excluded youth experience higher levels of internalizing and externalizing problems (Burk et al., 2011). The current study focused on potential developmental pathways from chronic victimization and exclusion in early adolescence to alcohol use in late adolescence.
Informed by developmental theories of alcohol use (Catalano & Hawkins, 1986; Hussong, Jones, Stein, Baucom, & Boeding, 2011), we considered two potential mediational pathways that might account for the link between chronic negative peer experiences and adolescent alcohol use. The first is an internalizing pathway whereby chronic negative peer experiences increase adolescents’ risk for developing internalizing symptoms, which in turn, increase motivation to drink as a means of coping with negative affect, and subsequent increased levels of alcohol use. The second is an externalizing pathway whereby chronic victimization and exclusion leads to increases in externalizing symptoms, which in turn, leads to higher levels of alcohol use.
An Internalizing Pathway to Alcohol Use
Adolescents who experience victimization or exclusion are at increased risk for the development of internalizing symptoms (Reijntjes, Kamphuis, Prinzie, & Telch, 2010). For example, Bowker and colleagues (2014) found peer victimization and peer exclusion were both associated uniquely with depressive symptoms. Further, neuroimaging studies and experimental studies that manipulated social exclusion also show increased susceptibility for internalizing symptoms for victimized and excluded youth (Reijntjes, Dekovic, Vermande, & Telche, 2007; Will, van Lier, Crone, &, Güroğlu, 2016). For example, Will et al. (2016) found that chronically excluded children had greater activation in brain regions implicated in emotional processing when being excluded in a game of Cyberball. Taken together, a strong body of empirical work points to the increased susceptibility of adolescents to develop internalizing symptoms in response to peer victimization and exclusion.
We propose that negative peer experiences can lead to increased alcohol involvement through an internalizing pathway. In a synthesis of the alcohol literature, Hussong and colleagues’ (2011) proposed several potential internalizing pathways that might increase risk for alcohol use. One of these pathways is relevant to the current study as it posits that victimized or excluded adolescents are at increased risk for developing internalizing symptoms, which in turn, lead some youth to develop motives to drink for coping reasons (coping motives). Coping motives refer to a motivation to use alcohol as a means of reducing emotional distress (Cooper, Frone, Russell, & Mudar, 1995) and figure prominently in some cognitive-behavioral models of alcohol use such as self-medication theory (Khantzian, 1985). Acute reductions in negative affect through the physiological effects of alcohol are thought to negatively reinforce drinking (Baker et al., 2004). Indeed, drinking coping motives have been associated with alcohol use (Armeli, Conner, Cullum, & Tennen, 2010).
In support of this risk pathway, recent cross-sectional (Lambe & Craig, 2017; Luk, Wang, & Simons-Morton, 2010) and longitudinal studies (Earnshaw et al., 2010) have found support for a risk pathway from victimization to alcohol use through negative affect and depressive symptoms. For example, Earnshaw and colleagues (2010) found evidence for a risk pathway from 5th grade victimization to 10th grade alcohol use through 7th grade depressive symptoms. These findings support part of the risk pathway described by Hussong and colleagues (2011), but without including coping motives, a critical mediator involved in this pathway.
Despite a common assumption that internalizing symptoms are a risk factor for alcohol use in adolescence, the evidence linking internalizing symptoms to alcohol use has been notably mixed (Hussong, Ennet, Cox, & Haroon, 2017). There are several possible reasons for this mixed literature, and one possibility is that internalizing symptoms operates through multiple pathways that can either increase or decrease risk for alcohol use (Hussong et al., 2011). In the absence of strong coping motivations for drinking, it is likely that internalizing symptoms decrease risk for alcohol use because characteristic features of internalizing symptoms, such as fearfulness, social withdrawal, and avoidance, may protect them from engaging with peer contexts that promote alcohol use (Fite, Colder, & O’Connor, 2006). In a recent review, Hussong et al. (2017) noted that such an effect is likely to be most evident after partialing out co-occurring externalizing symptoms. This is an important point because internalizing and externalizing symptoms are often moderately to strongly associated (Achenbach & Rescorla, 2001) and past research has not consistently statistically controlled for externalizing symptoms when examining associations between internalizing symptoms and alcohol use. Not doing so can lead to misattributing an observed risk effect to internalizing symptoms that is due to co-occurring externalizing symptoms (Colder et al., 2017a; Hussong et al., 2017).
The current study addresses several gaps in the literature on an internalizing pathway from negative peer experiences to alcohol use in several important ways. First, consistent with self-medication conceptualizations, we include coping motives as a mediator in our test of the internalizing pathway. Second, we statistically control for externalizing symptoms. This is critical as internalizing and externalizing symptoms often co-occur, and examining such unique effects has not been consistently done in studies examining mediational pathways from victimization to alcohol use (Earnshaw et al., 2017; Luk et al., 2010). Lastly, no studies have assessed whether peer exclusion is prospectively associated with alcohol use through an internalizing risk pathway.
An Externalizing Pathway to Alcohol Use
Chronic negative peer experiences may also place adolescents at increased risk for developing externalizing symptoms (Coie, 2004). Longitudinal studies have demonstrated that peer victimization and exclusion are associated with higher levels of externalizing behaviors such as aggression and rule breaking even after taking into account prior levels of externalizing behaviors (Reijntjes et al., 2011), suggesting that these negative peer experiences can escalate externalizing behaviors. The poor social skills often seen in adolescents who experience negative peer experiences has been suggested to account for the increased likelihood of victimized and excluded adolescents to engage in externalizing behaviors (Coie, 2004). These social deficits have been shown to lead victimized or excluded adolescents to use less effective strategies to manage social conflicts such as reactive aggression towards those who victimized or excluded them (Dodge & Coie, 1987; Murray-Close & Ostrov, 2009).
The Social Development Model (Catalano & Hawkins, 1986) posits a pathway from negative peer experiences to alcohol use through externalizing symptoms. The theory is based on the premise that strong bonds to conventional institutions and individuals provide informal control over behavior and can prevent youth from engaging in nonconventional behaviors such as alcohol use and delinquency. Negative peer experiences are thought to interfere with forming bonds with conventional institutions (e.g., school) and individuals (e.g., peers, family), and hence, high levels of alcohol use and delinquency. Indeed, findings suggest that chronic victimization and exclusion damage bonds to school, parents, and prosocial peers, decrease motivation to follow prosocial norms, and increase engagement in aggressive and rule breaking behaviors (Buhs et al., 2006; Hong & Espelage, 2012; Scholte et al., 2009). In turn, aggressive and rule breaking behaviors prospectively predict adolescent alcohol use (e.g., D’Amico, Edelen, Miles, & Morral, 2008; Fite, Colder, Lochman, & Wells, 2007), perhaps because externalizing behavior evokes negative parenting practices (Dishion, Nelson, & Kavanagh, 2003) and promotes affiliations with delinquent peers that support alcohol use (Laird, Jordan, Dodge, Pettit, & Bates, 2001). To date, no work, to our knowledge, has longitudinally assessed whether chronic victimization and exclusion lead to alcohol use through externalizing symptoms as forwarded by the Social Development Model.
The Current Study
Although negative peer experiences have been implicated in adolescent alcohol use (Topper & Conrod, 2011), few longitudinal studies have examined mechanisms for this association. The current study tested two pathways from chronic victimization and exclusion in early adolescence to alcohol use in late adolescence. We address several gaps in the literature. First, we include both peer victimization and peer exclusion, which allowed us to examine whether these negative peer experiences operated in a similar fashion. However, we see no strong rationale for hypothesizing differences regarding pathways to alcohol use, and hence we expected victimization and exclusion to operate similarly in our proposed mediational pathways. Second, coping motives for drinking are a critical feature of mechanisms proposed to account for links between negative peer experiences and alcohol use, yet prior work has not included this variable. We include coping motives in the proposed internalizing risk pathway. Third, internalizing and externalizing symptoms often co-occur, and we examine their unique effects.
For the internalizing pathway, we hypothesized that chronic victimization and exclusion will be positively associated with internalizing symptoms, and that internalizing symptoms will be positively associated with coping drinking motives, which in turn, will be positively associated with alcohol use. Consistent with prior work (Niemelä et al., 2006; Scalco et al., 2014), we hypothesize that the direct effect from internalizing symptoms to alcohol use, controlling for externalizing symptoms, will be negative. For the externalizing pathway, we hypothesized that chronic victimization and exclusion would both be positively associated with externalizing symptoms, which in turn, would be positively associated with alcohol use.
Methods
Participants
Participants were taken from a longitudinal study examining risk and protective factors associated with the initiation and escalation of early adolescent substance use. Random-digit dialing (RDD) procedures were utilized to recruit the 387 families (1 child, 1 caregiver) from 2007 to 2009. Listed and unlisted telephone numbers were used, and 98.5% of households had a landline at the time of recruitment in our sampling area (in Erie County NY). The sample was evenly split on gender (N = 205 female, 55%) and included non-Hispanic Caucasian (83.1%), African American (9.1%), Hispanic (2.1%), and Asian (1.0%), as well as youth of mixed ethnicity (4.7%). Median family income was $70,000 and ranged from $1,500 to $500,000, and 6.2% of the families received public income assistance. At Waves one through three (W1–W3), target adolescents provided the names of four close friends and one was recruited into the study (peer) to provide a collateral report of the target adolescent’s peer environment. Peers were required to be within two years of age of the target adolescent and could not be a sibling. Moreover, targets were allowed to nominate different peers at each wave to allow for the fluid nature of adolescent peer relationships (Knecht, Snijders, Baerveldt, Steglich, & Raub 2010). Demographic characteristics of our sample are similar to those of Erie County from whence the sample came (for more complete details, see Authors et al., 2014).
The current study used data from W1 to W3, and Waves seven and eight (W7 and W8) of the longitudinal project when internalizing and externalizing symptoms as well as peer victimization and exclusion were assessed. Waves four through six were not included because only drug and alcohol use was assessed at these waves. Average ages (in years) of target participants were 12.1 at W1 and 18.9 at W8 and the average age of peers at W1 were 11.8. Overall retention across the eight waves was excellent (91%). Chi-square and analysis of variance tests comparing those with and without missing data on W1 variables suggested no significant differences (ps > 0.05) for age, gender, ethnicity, parental income, externalizing and internalizing symptoms, victimization, exclusion, and alcohol use. The low attrition rate and lack of differences suggest that missing data did not have a substantial impact on the findings of the current study.
Procedures
At W1–W3, both target (target and caregiver) and peer (peer and caregiver) families were interviewed annually in university research offices. After informed consent and assent procedures, caregiver and adolescents were escorted to separate rooms for the assessments, which consisted of both laboratory tasks as well as questionnaires assessing a wide range of family, peer, and individual level risk and protective factors for adolescent drug use. Assessments took approximately 2.5 to 3 hours. Target and peer families were compensated for their participation.
Procedures at W7 and W8 closely aligned with those at W1–W3 except that peer data were not collected in these later waves. Participants (target adolescent) and their caregivers completed annual interviews in university research offices. Considering the age of our participants at W7 and W8, a number of participants had relocated out of the area. To retain these individuals, participants were provided with an opportunity to complete the questionnaires remotely (N=18 or 5% of the W7 sample and N=33 or 9% of the W8 sample completed the questionnaires remotely). All procedures were approved by the University at Buffalo’s Institutional Review Board (Study title: Internalizing problems, motivation, peers, & development of adolescent drug use; MODCR00000706).
Measures
Target and peer report of victimization (W1–W3)
Our measure of peer victimization included four items taken from the Perceptions of Peer Support Scale (Kochenderfer & Ladd, 1996; e.g., “Other kids pick on you at school” and “Other kids say mean things to you”) and one item taken from the Multidimensional-Peer Victimization Scale (Mynard & Joseph, 2000), “other kids make fun of you because of your appearance.” Target adolescents chose the response that best described how often they had these experiences when with other kids (1=never to 3=a lot). Peers chose the response that best described how often the target adolescent had these experiences when with other kids (1=never to 3=a lot). The internal consistency of this measure ranged from α=.80 to α=.82 for target reports and from α=.74 to α=.77 for peer reports.
Target and peer report of exclusion (W1–W3)
Peer exclusion was assessed using the revised version of the Child Social Preference Scale (CSPS; Bowker & Raja, 2011). This self-report measure includes four items (“I’d like to hang out with other kids, but I’m often excluded,” “I want to play with others but often they don’t want to play with me,” “sometimes kids don’t want me to hang out with them,” and “I wish I could spend more time with other kids, but they don’t let me.”) and adolescents rated how much they are like each statement using a 5-point response scale (1= not at all, 5=a lot). Peers reported how much the target adolescent is like each statement using the same response scale. The internal consistency for the revised CSPS was good for target (α range=.82–83) and peer reports (α range=.86–.88).
Externalizing and internalizing symptoms (W3, W7)
Externalizing and internalizing symptoms were measured using the Youth Self-Report (YSR) at W3 and the Adult Self-Report at W7 (Achenbach & Rescorla, 2001, 2003). The Rule Breaking Behavior and Aggressive Behavior subscales were averaged to form the externalizing symptoms variable at W3 and W7, and the Anxious-Depressed, Withdrawn-Depressed, and Somatic Complaints subscales were averaged to form the internalizing symptoms variable at W3 and W7. Substance use items excluded from the externalizing subscales to eliminate item overlap with our outcomes. The YSR and ASR have demonstrated strong reliability and validity (Achenbach & Rescorla, 2001, 2003). Internal consistency for externalizing symptoms was α=.84 (W3) and α=.84 (W7) and α=.73 (W3) and α=.80 (W7) for internalizing symptoms.
Alcohol use (W3, W7, W8)
Items from the National Youth Survey (NYS; Elliot & Huizinga, 1983) were used to assess past year alcohol use at W3. Adolescents reported the number of times in the past year they used alcohol without their parents’ permission as well as the typical quantity of alcohol they consumed on drinking days. These items were combined to create a quantity x frequency score representing past year alcohol use. At W7 and W8, participants reported past year alcohol frequency using an 8-point response scale (1=not at all to 8=everyday), and responses were converted to represent the number of drinking days in the past year to be consistent with our W3 measurement of alcohol use. Typical quantity of alcohol use at W7 and W8 was assessed using a calendar to report on the typical number of drinks consumed each day in a typical week in the past 90-days (Collins, Parks, & Marlatt, 1985) and computed by taking the average number of drinks consumed across drinking days. A quantity x frequency index was created to represent the total number of drinks in the past year for W7 and W8. To reduce the influence of outliers, extreme values were recoded to three standard deviations above the mean at each wave (Tabachnick & Fidell, 2007).
Coping motives (W7)
The coping motives subscale of the Drinking Motives Questionnaire (DMQ) was used to assess coping drinking motives (Cooper, 1994). Participants used a 5-point response scale (1=almost never/never to 5=almost always/always) to report how often they drank to cope (e.g., “Because it helps you when you feel depressed or nervous?”). Items were averaged to form a scale score (α=.87).
Data Analytic Strategy
Structural Equation Modeling with Robust Maximum Likelihood estimation (MLR) was used to test the proposed pathways from chronic peer victimization and exclusion to alcohol use in Mplus 8.0 (Muthen and Muthen, 1998–2014). MLR was used to accommodate the non-normality of some of our observed endogenous variables (see Table 1). Second-order factor models for both target and peer report of peer victimization and peer exclusion were first estimated using W1–W3 data to test the feasibility of specifying peer victimization and exclusion as chronic latent variables in early adolescence. These models were estimated by first specifying first-order factor models for victimization (using the five item indicators) and exclusion (using the four item indicators) at W1, W2, and W3. Next, first-order factors of victimization and exclusion served as indicators of second-order factors of victimization and exclusion, respectively (see Figure 1). Second-order factors of victimization and exclusion represent the shared variances in victimization and exclusion at W1 to W3, thus higher scores on the victimization and exclusion second-order factors represent higher levels of victimization and exclusion across W1–W3. All other variables included in our models were observed to reduce the number of estimated parameters.
Table 1.
Bivariate Spearman Correlations
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Alc W3 | --- | ||||||||||||||||||||||
| 2. Alc W7 | 0.25 | --- | |||||||||||||||||||||
| 3. Alc W8 | 0.20 | 0.62 | --- | ||||||||||||||||||||
| 4. Vic W1 (T) | 0.00 | −0.01 | −0.09 | --- | |||||||||||||||||||
| 5. Vic W2 (T) | 0.09 | 0.01 | −0.02 | 0.58 | --- | ||||||||||||||||||
| 6. Vic W3 (T) | 0.12 | 0.08 | 0.01 | 0.50 | 0.57 | --- | |||||||||||||||||
| 7. Vic W1 (P) | 0.06 | −0.04 | −0.03 | 0.10 | 0.07 | 0.08 | --- | ||||||||||||||||
| 8. Vic W2 (P) | 0.06 | −0.04 | −0.08 | 0.14 | 0.13 | 0.15 | 0.25 | --- | |||||||||||||||
| 9. Vic W3 (P) | 0.00 | 0.10 | 0.02 | 0.12 | 0.14 | 0.17 | 0.14 | 0.33 | --- | ||||||||||||||
| 10. Exc W1 (T) | −0.04 | −0.06 | −0.11 | 0.52 | 0.37 | 0.32 | 0.04 | 0.08 | 0.07 | --- | |||||||||||||
| 11. Exc W2 (T) | −0.04 | −0.15 | −0.16 | 0.46 | 0.51 | 0.34 | −0.03 | 0.14 | 0.06 | 0.54 | --- | ||||||||||||
| 12. Exc W3 (T) | 0.04 | −0.11 | −0.10 | 0.34 | 0.37 | 0.45 | 0.05 | 0.15 | 0.05 | 0.47 | 0.52 | --- | |||||||||||
| 13. Exc W1 (P) | −0.09 | −0.15 | −0.11 | 0.21 | 0.11 | 0.13 | 0.26 | 0.12 | 0.09 | 0.17 | 0.11 | 0.11 | --- | ||||||||||
| 14. Exc W2 (P) | −0.03 | −0.08 | −0.15 | 0.19 | 0.13 | 0.22 | 0.16 | 0.34 | 0.15 | 0.22 | 0.31 | 0.30 | 0.34 | --- | |||||||||
| 15. Exc W3 (P) | 0.00 | 0.05 | −0.03 | 0.17 | 0.12 | 0.19 | 0.09 | 0.19 | 0.30 | 0.14 | 0.22 | 0.20 | 0.21 | 0.41 | --- | ||||||||
| 16. Ext W3 | 0.44 | 0.15 | 0.12 | 0.28 | 0.37 | 0.38 | 0.06 | 0.14 | 0.08 | 0.14 | 0.22 | 0.32 | −0.01 | 0.15 | 0.08 | --- | |||||||
| 17. Ext W7 | 0.22 | 0.29 | 0.23 | 0.14 | 0.27 | 0.23 | −0.02 | 0.00 | 0.04 | 0.12 | 0.12 | 0.16 | −0.01 | 0.04 | 0.02 | 0.45 | --- | ||||||
| 18. Int W3 | 0.26 | −0.04 | −0.07 | 0.23 | 0.30 | 0.34 | 0.05 | 0.13 | 0.05 | 0.20 | 0.28 | 0.35 | −0.03 | 0.16 | 0.02 | 0.62 | 0.27 | --- | |||||
| 19. Int W7 | 0.16 | 0.03 | −0.04 | 0.22 | 0.21 | 0.24 | 0.05 | 0.03 | 0.00 | 0.26 | 0.29 | 0.32 | 0.04 | 0.15 | 0.02 | 0.32 | 0.56 | 0.44 | --- | ||||
| 20. Cope W7 | 0.22 | 0.58 | 0.49 | 0.03 | 0.05 | 0.11 | −0.03 | 0.02 | 0.06 | 0.01 | −0.03 | 0.01 | −0.13 | 0.00 | 0.07 | 0.21 | 0.40 | 0.05 | 0.30 | --- | |||
| 21. Income | 0.00 | 0.19 | 0.26 | −0.10 | −0.14 | −0.09 | −0.15 | −0.19 | −0.14 | −0.06 | −0.10 | −0.06 | −0.12 | −0.18 | −0.10 | −0.17 | −0.02 | −0.13 | −0.08 | 0.16 | --- | ||
| 21. Age | 0.24 | 0.19 | 0.09 | −0.07 | −0.07 | −0.06 | 0.04 | −0.10 | −0.06 | −0.07 | −0.06 | 0.06 | −0.05 | 0.01 | −0.01 | 0.15 | −0.02 | 0.12 | 0.11 | 0.14 | −0.02 | --- | |
| 22. Gender | 0.04 | −0.04 | −0.11 | −0.10 | −0.09 | −0.07 | −0.01 | 0.00 | 0.09 | −0.14 | −0.12 | −0.16 | −0.10 | −0.17 | −0.07 | −0.10 | −0.06 | 0.04 | 0.18 | 0.08 | −0.03 | 0.04 | --- |
| Mean | 1.63 | 147.87 | 194.03 | 6.91 | 1.36 | 6.61 | 1.38 | 1.38 | 1.35 | 1.73 | 1.59 | 1.50 | 1.79 | 1.74 | 1.61 | 0.26 | 0.32 | 0.25 | 0.38 | 1.51 | 81321.16 | 12.09 | 0.55 |
| SD | 10.36 | 318.99 | 353.13 | 1.98 | 0.38 | 1.89 | 0.37 | 0.39 | 0.36 | 0.77 | 0.71 | 0.64 | 0.84 | 0.83 | 0.68 | 0.22 | 0.26 | 0.28 | 0.29 | 0.72 | 58349.70 | 0.59 | 0.50 |
| Skew | 8.82 | 3.17 | 2.44 | 1.08 | 0.96 | 1.45 | 0.87 | 1.24 | 1.21 | 1.14 | 1.45 | 1.87 | 1.35 | 1.34 | 1.12 | 1.26 | 1.33 | 1.47 | 1.36 | 1.89 | 2.73 | −0.16 | −0.20 |
| Kurtosis | 81.03 | 10.52 | 5.35 | 1.34 | 0.64 | 3.01 | 0.28 | 2.14 | 1.81 | 0.86 | 2.28 | 4.93 | 1.88 | 1.71 | 0.60 | 2.01 | 2.06 | 2.01 | 2.52 | 3.96 | 12.90 | −1.12 | −1.97 |
Note. Correlations in bold are significant at p<.05. T= target report of negative peer experience, P= peer report of negative peer experience, W= wave, Alc= alcohol use, Vic= victimization, Exc= exclusion, Ext=externalizing symptoms, Int=Internalizing symptoms, Cope=coping motives, Income=family income.
Figure 1.
Second-Order Factor Model Specification for Chronic Victimization and Exclusion
Note. Panel A depicts the second-order factor model for chronic victimization and Panel B depicts the second-order factor model for chronic exclusion. V1 = victimization item 1. E1= exclusion item 1. W=wave.
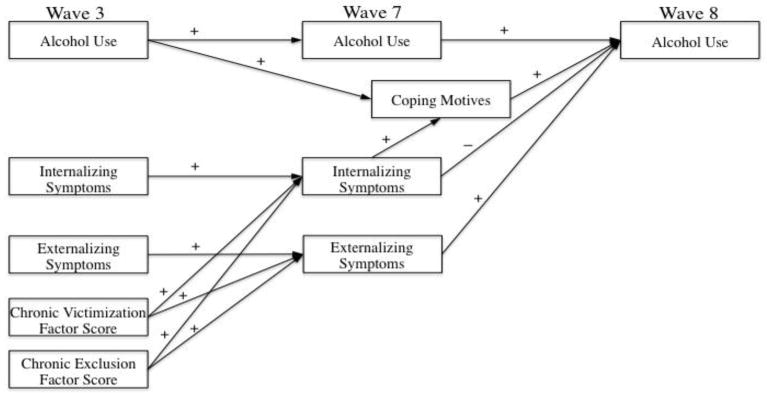
After obtaining a good fitting measurement model, structural models with causal paths were estimated separately for peer victimization and exclusion. First, we estimated models that included our hypothesized mediational pathways for chronic peer victimization (target and peer report) to alcohol use, and the second set of models included our hypothesized mediational pathways from chronic peer exclusion (target and peer report) to alcohol use. The final models (target and peer report) included both peer victimization and exclusion simultaneously, and this allowed us to test the unique contribution of each above and beyond the other (see Figure 2). For these models, we used factor scores from the measurement models for chronic victimization and chronic exclusion, rather than specifying these variables as latent variables, to reduce the complexity of the models.
Figure 2.
Hypothesized Pathways Linking Chronic Victimization and Exclusion to Alcohol Use
Note. Positive and negative signs denote the hypothesized direction of regression coefficients. Chronic victimization and exclusion factor scores represent the second-order factor models for victimization and exclusion. Second-order factor scores are a function of victimization and exclusion at W1, W2, and W3.
Gender1, age and family income were included as statistical control variables, and initially the models included paths from these variables to all W7 and W8 variables and then non-significant paths were removed to reduce model complexity. All models also controlled for prior waves of alcohol use, externalizing symptoms, and internalizing symptoms. Coping motives at W7 were also regressed on W3 alcohol use because prior drinking levels have been associated with higher levels of coping motives (Settles, Cyders, & Smith, 2010). Covariances were freely estimated within time. Bias-corrected confidence intervals using 5000 randomly generated samples were used to formally test our mediational pathways (Hayes & Scharkow, 2013).
Model fit was assessed using the Comparative Fit Index (CFI), Tucker-Lewis Index (TLI), Root Mean Square Error Approximation (RMSEA), and Standardized Root-Mean-Square Residual (SRMR). Specific cut-offs for assessing “good” fit cannot be generalized across all models (Hu & Bentler, 1999; Marsh, Hau, & Wen, 2004), therefore, ranges were used to determine the acceptability of model fit (for CFI and TLI, <.90 is poor, .90 to .94 is acceptable, and >.95 is excellent; for RMSEA, .08 is poor, .05 to .07 is acceptable, and <.05 is excellent; and for SRMR, .09 is poor, .06 to .09 is acceptable, and <.06 is excellent). Power analysis indicated that we had between 83% to 99% power for identifying a good-fitting model across our measurement and hybrid models with our sample size of 387 (Preacher & Coffman, 2006).
Results
Descriptive Statistics
Spearman correlations among study variables are provided in Table 1 because of the non-normality of many study variables. Target report of peer victimization and exclusion were correlated both within and across time points, although the associations were only moderate in magnitude. Peer report of victimization and exclusion were also significantly correlated within time. Target report of peer victimization and exclusion were also both correlated with internalizing and externalizing symptoms within and across waves. W2 peer report of victimization and exclusion were significantly associated with both internalizing and externalizing symptoms at W3. W2 peer report of exclusion was also positively associated with W7 internalizing symptoms. Alcohol use and target report of victimization were only correlated at W3 and peer report of victimization was unrelated to alcohol use. Target and peer report of peer exclusion at W1 and W2 was negatively correlated with alcohol use at W8, and target report of exclusion at W2 and W3 was negatively correlated with W7 alcohol use. Alcohol use variables were highly skewed and kurtotic at W1–W3 (see Table 1), thus a log transformation was used to reduce the influence of the non-normality of alcohol use.
Measurement Models for Peer Victimization and Peer Exclusion
For both target and peer report of peer victimization and peer exclusion, nested tests supported equality of factor loadings, but only partial scalar and residual invariance. The final models for target report of chronic peer victimization (X2=135.37(105), p=.02, CFI=.98, TLI=.98, RMSEA=.02, SRMR=.05) and peer report of chronic victimization (X2=111.75(109), p=.40, CFI=1.0, TLI=1.0, RMSEA=.01, SRMR=.04) as well as target report of chronic peer exclusion (X2=74.31(61), p=.11, CFI=.99, TLI=.99, RMSEA=.02, SRMR=.05) and peer report of chronic exclusion (X2=79.07(70), p=.21, CFI=.99, TLI=.99, RMSEA=.01, SRMR=.05) fit the data well2.
Independent Effects of Victimization on Alcohol Use
Target Report Model
The model assessing our hypothesized mediational pathways from chronic victimization to alcohol use provided an excellent fit to the data (X2=378.28(276), p<.0001, CFI=.96, TLI=.96, RMSEA=.03, SRMR=.05). All autoregressive paths were statistically significant. Females had significantly higher levels of internalizing symptoms at W7 relative to males. Age was significantly positively associated W3 and W7 alcohol use, W7 internalizing symptoms, and negatively associated with chronic victimization. Family income was positively associated with alcohol use at W7 and W8 as well as coping motives. Chronic victimization was significantly associated with both internalizing symptoms (β=.27, p=.003) and externalizing symptoms (β=.16, p=.03) at W7, even after controlling for internalizing and externalizing symptoms at W3. W7 internalizing symptoms had a significant negative association with W8 alcohol use (β=−.14, p=.01) and W7 externalizing symptoms were not significantly associated with alcohol use at W8 (β=.06, p=.28). W7 internalizing symptoms were significantly associated with W7 coping motives, (β=.41, p<.001) and coping motives at W7 were significantly associated with W8 alcohol use (β=.14, p=.003). Overall, the model accounted for 41% of the variance of W8 alcohol use.
As seen in Table 2, results of the mediational analyses using bias corrected confidence intervals indicated a significant indirect effect of chronic victimization to alcohol use through W7 internalizing symptoms. There was a significant indirect effect from chronic victimization to alcohol use, such that chronic victimization was positively associated with internalizing symptoms, which in turn positively predicted coping motives, and coping motives were significantly associated with W8 alcohol use. Lastly, there was no support for an indirect effect from chronic victimization to alcohol use through externalizing symptoms, which was not surprising considering externalizing symptoms at W7 was not associated with W8 alcohol use.
Table 2.
Indirect Effects from Chronic Victimization and Exclusion to Alcohol Use
| Indirect Effects | Target Report | Peer Report | ||
|---|---|---|---|---|
|
| ||||
| Victimization | Exclusion | Victimization | Exclusion | |
|
|
||||
| Independent Effects of Victimization and Exclusion on Alcohol Use | ||||
| Total Indirect Effect from NPE to Alcohol Use | (−.48, .11) | (−.37, .08) | (−.55, .17) | (−.25, .04) |
| NPE to Internalizing Symptoms to Alcohol use | (−.92, −.07) | (−.68, −.05) | (−.92, .31) | (−.42, −.002) |
| NPE to Internalizing Symptoms to Coping Motives to Alcohol Use | (.06, .35) | (.05, .26) | (−.14, .32) | (.01, .16) |
| NPE to Externalizing Symptoms to Alcohol Use | (−.05, .37) | (−.03, .20) | (−.30, .19) | (−.02, .17) |
| Unique Effects of Victimization and Exclusion on Alcohol Use | ||||
| Total Indirect Effect from NPE to Alcohol Use | (−.12, .14) | (−.25, .07) | (−.24, .22) | (−.18, .05) |
| NPE to Internalizing Symptoms to Alcohol use | (−.34, .05) | (−.43, −.04) | (−.26, .51) | (−.35, −.01) |
| NPE to Internalizing Symptoms to Coping Motives to Alcohol Use | (−.03, .16) | (.04, .21) | (−.24, .13) | (.01, .16) |
| NPE to Externalizing Symptoms to Alcohol Use | (−.03, .24) | (−.01, .14) | (−.37, 06) | (−.02, .16) |
Note. NPE=negative peer experience. Significant indirect effects are bolded.
Peer Report Model
The peer report model also provided an excellent fit to the data (X2=352.98(286), p=.004, CFI=.97, TLI=.97, RMSEA=.02, SRMR=.04). Unlike the target report model, peer victimization was not prospectively associated with internalizing (β=.04, p=.62) or externalizing symptoms (β=−.01, p=.92). No significant indirect effects were found from peer victimization to alcohol use. The model accounted for 41% of the variance in W8 alcohol use.
Independent Effects of Chronic Exclusion on Alcohol Use
Target Report Model
The model examining longitudinal associations between chronic peer exclusion and alcohol use provided an excellent good fit to the data (X2=249.43(204), p=.01, CFI=.98, TLI=.98, RMSEA=.02, SRMR=.05), and results mirrored the results for peer victimization. Females had significantly lower levels of chronic exclusion. Chronic exclusion was significantly associated with both W7 internalizing (β=.41, p=.001) and externalizing symptoms (β=.18, p=.02). Results for all other paths were identical to those from the target report model for chronic victimization. Overall, the model accounted for 41% of the variance in W8 alcohol use.
As seen in Table 2, there was again a significant negative indirect effect from chronic exclusion to alcohol use through W7 internalizing symptoms. Again, there was evidence of a risk pathway from chronic exclusion to alcohol use through internalizing symptoms such that chronic exclusion was positively associated with internalizing symptoms, and internalizing symptoms were associated with coping motives, which in turn, were associated with alcohol use. There was no evidence of an indirect relationship from chronic exclusion to alcohol use through externalizing.
Peer Report Model
The peer report model provided an excellent fit to the data (X2=269.67(219), p=.02, CFI=.98, TLI=.98, RMSEA=.02, SRMR=.05). The only difference observed in the peer report model was that chronic exclusion was not a significant predictor of W7 internalizing (β=.14, p=.07) and externalizing symptoms (β=.07, p=.28). The indirect effects through internalizing symptoms and internalizing symptoms and coping motives were both statistically significant. The model accounted for 41% of the variance in W8 alcohol use.
Unique Effects of Victimization and Exclusion on Alcohol Use
Target Report Model
The model examining the unique effects of chronic victimization and exclusion on internalizing and externalizing symptoms and their subsequent relationships with alcohol use provided a good fit to the data (X2=46.45(25), p=.01, CFI=.97, TLI=.94, RMSEA=.04, SRMR=.03). Females had higher levels of W7 internalizing symptoms and lower levels of chronic exclusion and victimization. Age was positively associated with W3 alcohol use and W7 internalizing symptoms. Family income was positively associated with W7 and W8 alcohol use as well as coping motives. Chronic exclusion was statistically significantly associated with W7 internalizing symptoms (β=.29, p<.001) and was not significantly associated with W7 externalizing symptoms (β=.10, p=.07). Chronic victimization was not associated with either W7 externalizing (β=.07, p=.23) or internalizing symptoms (β=.05, p=.38). W7 externalizing symptoms were not associated with W8 alcohol use (β=.06, p=.28). Similar to previous models, W7 internalizing symptoms were negatively associated with W8 alcohol use (β=−.14, p=.01), and W7 internalizing symptoms were positively associated with W7 coping motives (β=.54, p<.001), that in turn, positively predicted W8 alcohol use (β=.16, p=.003). Overall, the model accounted for 41% of the variance in W8 alcohol use.
As seen in Table 2, mediational effects demonstrated a statistically significant negative indirect effect from chronic exclusion to W8 alcohol use through W7 internalizing symptoms such that chronic exclusion was positively associated with W7 internalizing symptoms, which in turn, was negatively associated with W8 alcohol use. There was also support for a positive indirect effect from chronic exclusion to W8 alcohol use through W7 internalizing symptoms and coping motives. There was no support for indirect effects from chronic victimization to W8 alcohol, and none that operated through externalizing symptoms.
Peer Report Model
The peer report model provided an excellent fit to the data (X2=38.09(25), p=.04, CFI=.98, TLI=.96, RMSEA=.03, SRMR=.03). Results from the peer report model largely replicated those from the target report model. The only difference observed across reporters was that chronic exclusion was not a significant predictor of externalizing symptoms at W7 (β=.07, p=.22). The indirect effects through internalizing symptoms and internalizing symptoms and coping motives were both statistically significant. The model accounted for 40% of the variance in W8 alcohol use.
Discussion
Chronic negative peer experiences have repeatedly been implicated in maladaptive health outcomes, including underage alcohol use (Sullivan et al., 2006). We focused on alcohol use, a behavior that is a significant public health concern and one that emerges and escalates during the adolescent period, and tested externalizing and internalizing risk pathways from negative peer experiences that spanned early to late adolescence. We extend prior research by including both peer victimization and exclusion, enabling us to examine potential unique effects of each, and by including externalizing symptoms, a potential confound of an internalizing pathway. Furthermore, we included coping motives as part of the internalizing risk pathway, a key mediator in this pathway. When analyzed separately, results supported a risk pathway from chronic victimization and exclusion to alcohol use through internalizing symptoms and coping motives as well as a negative indirect effect from chronic victimization and exclusion to alcohol use through internalizing symptoms. When both domains of chronic peer negative experiences were included in the same model, the risk and negative indirect pathways were only observed for chronic exclusion. No support was found for an externalizing pathway from negative peer experiences to alcohol use.
Independent Effects of Victimization and Exclusion on Alcohol Use
Our findings suggest that when chronic victimization and exclusion were examined in separate models, results supported a complex set of both positive and negative indirect effects involving internalizing symptoms. In the risk pathway, chronic peer victimization and peer exclusion were both prospectively associated with increased internalizing symptoms. Internalizing symptoms predicted coping motives, which in turn, were associated with higher levels of alcohol use. These findings are consistent with the idea that negative peer experiences lead to emotional distress, which can evoke strong motivations to drink as a way of coping with emotional distress (Hussong et al., 2011). Some prior work has similarly found evidence for a risk pathway from victimization to alcohol use through depressive symptoms and negative affect (Earnshaw et al., 2017; Lambe & Craig, 2017; Luk et al., 2010). Our findings provide a crucial extension of this prior research by showing that this pathway operates through coping motivated drinking, and hence garners stronger evidence for a self-medication pathway.
The negative indirect effect did not operate through coping motives. Instead, both peer victimization and exclusion were associated with high levels of internalizing symptoms, which in turn, were directly associated with low levels of alcohol use. This pathway replicated across target and peer reports for exclusion but was only supported in the target self-report model for victimization. Characteristic features of internalizing symptoms, such as fearfulness, worry, and social withdrawal, may protect adolescents from engaging with peer contexts that may promote alcohol use (Fite, Colder, & O’Connor, 2006; Hussong et al., 2017).
Support for both a positive and negative indirect pathway involving internalizing symptoms is notable. The broader literature examining links between internalizing symptoms and adolescent alcohol use provides evidence for positive and negative associations, and also no association (Hussong et al., 2017). There are likely a variety of reasons for this mixed literature, but our findings provide compelling evidence that including relevant mediators can help distinguish positive and negative pathways involving internalizing symptoms. If internalizing symptoms lead to strong coping motivations, then a risk pathway is evident. However, if internalizing symptoms do not lead to strong coping motives, then a negative pathway emerges. These multiple pathways are consistent with the idea of multifinality that argues that risk factors, such as internalizing symptoms, may be differentially related to outcomes (e.g., alcohol use) depending on an adolescent’s experiences and contexts (Cicchetti & Rogosch, 1996).
We found no support for the externalizing pathway from chronic victimization or exclusion to alcohol use. Although victimization and exclusion were consistently associated with W7 externalizing symptoms when analyzed separately, W7 externalizing symptoms were not significantly associated with W8 alcohol use. One explanation for the non-significant associations between externalizing symptoms and alcohol use likely stems from moderate associations between W7 externalizing symptoms and W7 alcohol use (r=.29). This within time correlation was much stronger than the correlation between W7 internalizing symptoms and W7 alcohol use (r=.03). Indeed, when removing W7 alcohol use from our models, externalizing symptoms at W7 significantly predicted W8 alcohol use. In sum, these analyses in conjunction with the zero-order correlations suggest that the lack of support for the externalizing pathway was a function of strong contemporaneous associations between externalizing symptoms and alcohol outcomes. A second possibility is that we did not include potential mediators of the relationship between externalizing symptoms and alcohol forwarded by the Social Development Model such as affiliations with delinquent peers, parenting, and school connectedness use (Catalano & Hawkins, 1986; Chassin et al., 2016).
Indirect effects from negative peer experiences to alcohol use replicated using peer reports of exclusion but not victimization. Observable forms of victimization decrease during adolescence whereas subtler, indirect, forms increase (Yeager, Fong, Lee, & Espelgae, 2015), which may lead peer reports to become less accurate or may lead peers to identify youth who are victimized in the most noticeable ways. Consistent with these findings, self-reports are argued to be more relevant than peer-reports of victimization because victims are likely most aware of, and impacted by, their victimization experiences (Card & Hodges, 2008). Relative to peer victimization, peer exclusion may be used to maintain social status hierarchies during adolescence (e.g., Shell et al., 2014). As such, many adolescents, who are highly sensitive to their own social status and that of their peers, are likely well aware of the extent to which their peers are excluded, especially when exclusion occurs in easily observed ways (LaFontana & Cillessen, 2010). As a result, peer and self-reports of peer exclusion likely overlap. Considering that few studies have included multiple reporters of adolescent peer exclusion, these findings highlight the need for future work assessing the strength of self-versus peer-reports of exclusion in the prediction of adjustment outcomes.
Unique Effects of Victimization and Exclusion on Alcohol Use
Limited work has examined peer victimization and peer exclusion simultaneously in adolescence and peer relations researchers have argued for the importance of assessing whether these negative peer experiences operate through similar mechanisms to influence maladaptive outcomes (Rubin et al., 2015). When analyzed in separate models, results from our study were largely consistent for peer victimization and exclusion despite only a moderate correlation between the two (rs = .50 at each wave). These findings suggest that with respect to their influence on drinking behaviors in adolescence, self-reported peer victimization and peer exclusion operate through similar mechanisms.
In line with suggestions of the importance of understanding the unique effects of negative peer experiences on adjustment (Bowker et al., 2014), we also examined our mediational pathways to alcohol use with victimization and exclusion included in the same model. When victimization and exclusion were included in the same model, the risk and protective pathways through internalizing symptoms to alcohol use were only observed for peer exclusion in both target and peer report models. These results may reflect the heightened impact of peer exclusion on maladaptive outcomes during adolescence. Peer exclusion appears to be particularly detrimental during adolescence, perhaps because being excluded makes it difficult to meet the critical developmental milestones of achieving peer acceptance and forming close and meaningful peer relationships (LaFontana & Cillessen, 2010). In contrast, victimized adolescents (who are not also excluded) are often still members of peer groups, perhaps making it possible for them to form meaningful interpersonal bonds (Rubin et al., 2015). These findings are compatible with research that has emphasized the unique impact of related but different types of peer experiences on adolescent adjustment outcomes (see Rubin et al., 2015). Our results are the first though to indicate that peer exclusion may be uniquely important for understanding alcohol use during adolescence.
Clinical Implications and Limitations
Support for an internalizing pathway to alcohol use involving internalizing symptoms and coping motives may have implications for prevention and intervention. Although prior work has suggested that preventative interventions for adolescent alcohol use targeting internalizing symptoms may have limited utility (e.g., Colder et al., 2017a), findings from the present study highlight a potential caveat to this claim. Specifically, interventions targeting internalizing symptoms to reduce alcohol use may be warranted for adolescents with strong motivations to drink for coping reasons and a history of chronic maladaptive peer experiences. Targeting coping motives through treatment components common in interventions for adolescent internalizing symptoms, such as cognitive restructuring and adaptive coping strategies (Kendall, 2011), may further reduce the risk of victimized and excluded adolescents from engaging in alcohol use.
The risk pathway to alcohol use through internalizing symptoms and coping motives reinforces the importance of early intervention to combat victimization and exclusion (Coie, 2004). Early intervention targeting victimization and exclusion may reduce internalizing symptoms and prevent adolescents from engaging in drinking to cope. Moreover, while considerable recent attention has been paid to understanding and targeting peer victimization during adolescence (Troop-Gordon, 2017), our findings suggest that increased clinical and basic research is needed to enhance understanding of the unique risks associated with peer exclusion.
The current study should be understood within the context of certain limitations. Our measure of peer victimization was more heavily representative of verbal than physical victimization. Considering increasing attention has been given to the different forms of victimization and their impact on developmental outcomes (Card, Stucky, Sawalani, & Little, 2008), future work should assess whether the mediational pathways in the present study operate differently for physical and verbal victimization. Another limitation was that we were unable to control for prior levels of coping motives because motives were not assessed prior to W7. Thus, we could not establish full temporal precedence for the internalizing pathway to alcohol use.
Conclusion
Overall, the present study supported an internalizing risk pathway to alcohol use from peer victimization and peer exclusion. Examining the role of internalizing symptoms above and beyond externalizing symptoms, and our inclusion of coping motives more clearly establishes that this risk pathway represents efforts to use alcohol to cope with the sequelae of negative peer experiences. Our results further suggested the mediating mechanisms of peer victimization and exclusion to alcohol use largely overlap. However, when analyzed in the same model, only peer exclusion was associated with alcohol use through internalizing symptoms suggesting that being excluded during adolescence may be particularly detrimental to adolescent adjustment.
Acknowledgments
This research was funded by a grant from the National Institute on Drug Abuse (R01DA019631) awarded to C.R.C.
Footnotes
Although we did not have a-priori hypotheses regarding gender differences in our proposed model, we tested potential gender differences were assessed in causal paths based on some prior work suggesting potential differences in the internalizing pathway (Lambe & Craig, 2017; Luk et al., 2010). Multiple group models supported constraining all estimated paths to be equal across gender. This suggests no gender differences in the proposed mediational pathways.
Measurement invariance was assessed across waves for internalizing and externalizing symptom variables. For externalizing symptoms, the rule breaking and aggressive behavior subscales were used as indicators of the latent externalizing variables at W3 and W7. Nested model tests supported configural, and metric invariance. Partial scalar invariance was supported after allowing the intercepts for rule breaking to vary across W3 and W7. For internalizing symptoms, the anxious-depressed, withdrawn-depressed, and somatic complaints subscales were used as indicators of latent internalizing symptoms at W3 and W7. Nested tests supported configural variance and partial metric, after freeing the loadings for anxious-depressed at W3 and W7, and scalar invariance, after freeing the intercepts for anxious-depressed and withdrawn-depressed across waves.
References
- Achenbach TM, Rescorla LA. Manual for the ASEBA school-age forms and profiles. Burlington: University of Vermont, Department of Psychiatry; 2001. [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASEBA adult forms & profiles. University of Vermont, Research Center for Children, Youth, and Families; Burlington: 2003. [Google Scholar]
- Armeli S, Conner TS, Cullum J, Tennen H. A longitudinal analysis of drinking motives moderating the negative affect-drinking association among college students. Psychology of Addictive Behaviors. 2010;24(1):38–47. doi: 10.1037/a0017530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Authors et al. 2014 [Google Scholar]
- Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review. 1977;84:191–215. doi: 10.1037/0033-295X.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bowker JC, Adams RE, Fredstrom BK, Gilman R. Experiences of being ignored by peers during late adolescence: Linkages to psychological maladjustment. Merrill-Palmer Quarterly. 2014;60(3):328–354. [Google Scholar]
- Bowker JC, Markovic A, Cogswell A, Raja R. Moderating effects of aggression on the associations between social withdrawal subtypes and peer difficulties during early adolescence. Journal of Youth and Adolescence. 2012;41(8):995–1007. doi: 10.1007/s10964-011-9712-0. [DOI] [PubMed] [Google Scholar]
- Bowker JC, Raja R. Social withdrawal subtypes during early adolescence in India. Journal of Abnormal Child Psychology. 2011;39(2):201–212. doi: 10.1007/s10802-010-9461-7. [DOI] [PubMed] [Google Scholar]
- Buhs ES, Ladd GW, Herald SL. Peer exclusion and victimization: Processes that mediate the relation between peer group rejection and children’s classroom engagement and achievement? Journal of Educational Psychology. 2006;98(1):1–13. doi: 10.1037/0022-0663.98.1.1. [DOI] [Google Scholar]
- Burk LR, Armstrong JM, Park JH, Zahn-Waxler C, Klein MH, Essex MJ. Stability of early identified aggressive victim status in elementary school and associations with later mental health problems and functional impairments. Journal of Abnormal Child Psychology. 2011;39(2):225–238. doi: 10.1007/s10802-010-9454-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Card NA, Hodges EV. Peer victimization among schoolchildren: Correlations, causes, consequences, and considerations in assessment and intervention. School Psychology Quarterly. 2008;23(4):451. doi: 10.1037/a0012769. [DOI] [Google Scholar]
- Card NA, Stucky BD, Sawalani GM, Little TD. Direct and indirect aggression during childhood and adolescence: A meta-analytic review of gender differences, intercorrelations, and relations to maladjustment. Child Development. 2008;79(5):1185–1229. doi: 10.1111/j.1467-8624.2008.01184.x. [DOI] [PubMed] [Google Scholar]
- Catalano RF, Hawkins JD. The social development model: A theory of antisocial behavior. Paper presented at the Safeco Lectureship on Crime and Delinquency; Seattle: University of Washington; 1986. [Google Scholar]
- Chassin L, Colder CR, Hussong A, Sher KJ. Developmental psychopathology, volume 3: Risk, disorder, and adaptation. Wiley; 2016. Substance use and substance use disorders; pp. 833–897. [DOI] [Google Scholar]
- Cicchetti D, Rogosch FA. Equifinality and multifinality in developmental psychopathology. Development and Psychopathology. 1996;8:597–600. [Google Scholar]
- Coie JD. Towards a theory of peer rejection. In: Asher SR, Coie JD, editors. Peer rejection in childhood. New York: Cambridge University Press; 1990. pp. 365–398. [Google Scholar]
- Coie JD. The impact of negative social experiences on the development of antisocial behavior. In: Kupersmidt JB, Dodge KA, editors. Children’s peer relations: From development to intervention. Washington, DC: American Psychological Association; 2004. pp. 243–267. [DOI] [Google Scholar]
- Colder CR, Frndak S, Lengua LJ, Read JP, Hawk LW, Wieczorek WF. Internalizing and externalizing problem behavior: a test of a latent variable interaction predicting a two-part growth model of adolescent substance use. Journal of Abnormal Child Psychology. 2017a:1–12. doi: 10.1007/s10802-017-0277-6. [DOI] [PMC free article] [PubMed]
- Colder CR, Shyhalla K, Frndak S, Read JP, Lengua LJ, Hawk LW, Wieczorek WF. The prospective association between internalizing symptoms and adolescent alcohol involvement and the moderating role of age and externalizing symptoms. Alcoholism: clinical and experimental research. 2017b doi: 10.1111/acer.13512. [DOI] [PMC free article] [PubMed]
- Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: the effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology. 1985;53(2):189–200. doi: 10.1037//0022-006x.53.2.189. [DOI] [PubMed] [Google Scholar]
- Cooper ML. Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychological Assessment. 1994;6(2):117–128. doi: 10.1037/1040-3590.6.2.117. [DOI] [Google Scholar]
- Cooper ML, Frone MR, Russell M, Mudar P. Drinking to regulate positive and negative emotions: a motivational model of alcohol use. Journal of Personality and Social Psychology. 1995;69(5):990–1005. doi: 10.1037/0022-3514.69.5.990. [DOI] [PubMed] [Google Scholar]
- D’Amico EJ, Edelen MO, Miles JN, Morral AR. The longitudinal association between substance use and delinquency among high-risk youth. Drug and Alcohol Dependence. 2008;93(1):85–92. doi: 10.1016/j.drugalcdep.2007.09.006. [DOI] [PubMed] [Google Scholar]
- Dodge KA, Coie JD. Social-information-processing factors in reactive and proactive aggression in children’s peer groups. Journal of Personality and Social Psychology. 1987;53(6):1146. doi: 10.1037/0022-3514.53.6.1146. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Nelson SE, Kavanagh K. The family check-up with high-risk young adolescents: Prevention early-onset substance use by parent monitoring. Behavior Therapy. 2003;34(4):553–571. doi: 10.1016/S00057894(03)80035-7. [DOI] [Google Scholar]
- Earnshaw VA, Elliott MN, Reisner SL, Mrug S, Windle M, Emery ST, Peskin MF, Schuster MA. Peer victimization, depressive symptoms, and substance use: a longitudinal analysis. Pediatrics. 2017:e20163426. doi: 10.1542/peds.2016-3426. [DOI] [PMC free article] [PubMed]
- Elliott DS, Huizinga D. Social class and delinquent behavior in a national youth panel: 1976–1980. Criminology. 1983;21(2):149–177. doi: 10.1111/j.1745-9125.1983.tb00256.x. [DOI] [Google Scholar]
- Fite PJ, Colder CR, Lochman JE, Wells KC. The relation between childhood proactive and reactive aggression and substance use initiation. Journal of Abnormal Child Psychology. 2008;36(2):261–271. doi: 10.1007/s10802-007-9175-7. [DOI] [PubMed] [Google Scholar]
- Fite PJ, Colder CR, O’Connor RM. Childhood behavior problems and peer selection and socialization: Risk for adolescent alcohol use. Addictive Behaviors. 2006;31(8):1454–1459. doi: 10.1016/j.addbeh.2005.09.015. [DOI] [PubMed] [Google Scholar]
- Grant JD, Scherrer JF, Lynskey MT, Lyons MJ, Eisen SA, Tsuang MT, … Bucholz KK. Adolescent alcohol use is a risk factor for adult alcohol and drug dependence: evidence from a twin design. Psychological Medicine. 2006;36(1):109–118. doi: 10.1017/S0033291705006045. [DOI] [PubMed] [Google Scholar]
- Hayes AF, Scharkow M. The relative trustworthiness of inferential tests of the indirect effect in statistical mediation analysis does method really matter? Psychological Science. 2013;24(10):1918–1927. doi: 10.1177/0956797613480187. [DOI] [PubMed] [Google Scholar]
- Hill KG, White HR, Chung IJ, Hawkins JD, Catalano RF. Early adult outcomes of adolescent binge drinking: person-and variable-centered analyses of binge drinking trajectories. Alcoholism: Clinical and Experimental Research. 2000;24(6):892–901. doi: 10.1111/j.1530-0277.2000.tb02071.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirschi T. Causes of delinquency. Berkeley, CA: University of California Press; 1969. [Google Scholar]
- Hong JS, Espelage DL. A review of research on bullying and peer victimization in school: An ecological system analysis. Aggression and violent behavior. 2012;17(4):311–322. doi: 10.1016/j.avb.2012.03.003. [DOI] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Hussong AM, Ennett ST, Cox MJ, Haroon M. A systematic review of the unique prospective association of negative affect symptoms and adolescent substance use controlling for externalizing symptoms. Psychology of Addictive Behaviors. 2017;31(2):137–147. doi: 10.1037/adb0000247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM, Jones DJ, Stein GL, Baucom DH, Boeding S. An internalizing pathway to alcohol use and disorder. Psychology of Addictive Behaviors. 2011;25(3):390–404. doi: 10.1037/a0024519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khantzian EJ. The self-medication hypothesis of addictive disorders: focus on heroin and cocaine dependence. American Journal of Psychiatry. 1985;142:1259–1264. doi: 10.1176/ajp.142.11.1259. https://doi.org 10.1002/ab.21517. [DOI] [PubMed] [Google Scholar]
- Kendall PC, editor. Child and adolescent therapy: Cognitive-behavioral procedures. Guilford Press; 2011. [Google Scholar]
- Knecht A, Snijders TA, Baerveldt C, Steglich CE, Raub W. Friendship and delinquency: Selection and influence processes in early adolescence. Social Development. 2010;19(3):494–514. doi: 10.1111/j.1467-9507.2009.00564.x. [DOI] [Google Scholar]
- Kochenderfer BJ, Ladd GW. Peer victimization: Cause or consequence of school maladjustment? Child Development. 1996;67(4):1305–1317. doi: 10.1111/j.1467-8624.1996.tb01797.x. [DOI] [PubMed] [Google Scholar]
- LaFontana KM, Cillessen AH. Developmental changes in the priority of perceived status in childhood and adolescence. Social Development. 2010;19(1):130–147. doi: 10.1111/j.1467-9507.2008.00522.x. [DOI] [Google Scholar]
- Laird RD, Jordan KY, Dodge KA, Pettit GS, Bates JE. Peer rejection in childhood, involvement with antisocial peers in early adolescence, and the development of externalizing behavior problems. Development and Psychopathology. 2001;13:337–354. doi: 10.1016/j.appdev.2008.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambe LJ, Craig WM. Bullying involvement and adolescent substance use: A multilevel investigation of individual and neighbourhood risk factors. Drug and Alcohol Dependence. 2017;178:461–468. doi: 10.1016/j.drugalcdep.2017.05.037. [DOI] [PubMed] [Google Scholar]
- Luk JW, Wang J, Simons-Morton BG. Bullying victimization and substance use among US adolescents: Mediation by depression. Prevention Science. 2010;11(4):355–359. doi: 10.1007/s11121-010-0179-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsh HW, Hau KT, Wen Z. In search of golden rules: Comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing 2004 [Google Scholar]
- Hu and Bentler’s. findings. Structural equation modeling. 1999;11(3):320–341. doi: 10.1207/s15328007sem1103_2. [DOI] [Google Scholar]
- Murray-Close D, Ostrov JM. A longitudinal study of forms and functions of aggressive behavior in early childhood. Child Development. 2009;80(3):828–842. doi: 10.1111/j.1467-8624.2009.01300.x. [DOI] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus User’s Guide. 7. Muthen & Muthen; Los Angeles, CA: 1998–2014. [Google Scholar]
- Mynard H, Joseph S. Development of the multidimensional peer-victimization scale. Aggressive Behavior. 2000;26(2):169–178. [Google Scholar]
- Niemelä S, Sourander A, Poikolainen K, Helenius H, Sillanmäki L, Parkkola K, Piha J, Kumpulainen K, Almqvist F, Moilanen I. Childhood predictors of drunkenness in late adolescence among males: A 10-year population-based follow-up study. Addiction. 2006;101:512–521. doi: 10.1111/j.1360-0443.2006.01381.x. [DOI] [PubMed] [Google Scholar]
- Pouwels JL, Souren PM, Lansu TA, Cillessen AH. Stability of peer victimization: A meta-analysis of longitudinal research. Developmental Review. 2016;40:1–24. doi: 10.1016/j.dr.2016.01.001. [DOI] [Google Scholar]
- Preacher KJ, Coffman DL. Computing power and minimum sample size for RMSEA [Computer software] 2006 May; Retrieved from http://quantpsy.org/
- Reijntjes A, Dekovic M, Vermande M, Telch MJ. Children’s feedback preferences in response to an experimentally manipulated peer evaluation outcome: The role of depressive symptoms. Journal of Abnormal Child Psychology. 2007;35(3):497–507. doi: 10.1007/s10802-007-9105-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reijntjes A, Kamphuis JH, Prinzie P, Boelen PA, Van der Schoot M, Telch MJ. Prospective linkages between peer victimization and externalizing problems in children: A meta-analysis. Aggressive Behavior. 2011;37(3):215–222. doi: 10.1002/ab.20374. [DOI] [PubMed] [Google Scholar]
- Reijntjes A, Kamphuis JH, Prinzie P, Telch MJ. Peer victimization and internalizing problems in children: A meta-analysis of longitudinal studies. Child Abuse & Neglect. 2010;34(4):244–252. doi: 10.1016/j.chiabu.2009.07.009. [DOI] [PubMed] [Google Scholar]
- Rose AJ, Rudolph KD. A review of sex differences in peer relationship processes: potential trade-offs for the emotional and behavioral development of girls and boys. Psychological bulletin. 2006;132(1):98. doi: 10.1037/0033-2909.132.1.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin KH, Bukowski W, Bowker J. Children in peer groups. In: Bornstein M, Leventhal T, Lerner RM, editors. Handbook of Child Psychology and Developmental Science (formerly The Handbook of Child Psychology), (Vol. 4: Ecological settings and processes) 7. New York, NY: Wiley; 2015. pp. 175–222. [DOI] [Google Scholar]
- Scalco MD, Colder CR, Hawk LW, Jr, Read JP, Wieczorek WF, Lengua LJ. Internalizing and externalizing problem behavior and early adolescent substance use: A test of a latent variable interaction and conditional indirect effects. Psychology of Addictive Behaviors. 2014;28(3):828–840. doi: 10.1037/a0035805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scholte RH, Overbeek G, Ten Brink G, Rommes E, De Kemp RA, Goossens L, Engels RC. The significance of reciprocal and unilateral friendships for peer victimization in adolescence. Journal of Youth and Adolescence. 2009;38(1):89–100. doi: 10.1007/s10964-008-9287-6. [DOI] [PubMed] [Google Scholar]
- Settles RF, Cyders M, Smith GT. Longitudinal validation of the acquired preparedness model of drinking risk. Psychology of Addictive Behaviors. 2010;24(2):198–208. doi: 10.1037/a0017631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shell MD, Gazelle H, Faldowski RA. Anxious solitude and the middle school transition: A diathesis× stress model of peer exclusion and victimization trajectories. Developmental Psychology. 2014;50(5):1569. doi: 10.1037/a0035528. [DOI] [PubMed] [Google Scholar]
- Sullivan TN, Farrell AD, Kliewer W. Peer victimization in early adolescence: Association between physical and relational victimization and drug use, aggression, and delinquent behaviors among urban middle school students. Development and Psychopathology. 2006;18(01):119–137. doi: 10.1017/S095457940606007X. [DOI] [PubMed] [Google Scholar]
- Sutherland EH. Development of the theory [Private paper published posthumously] In: Schuessler KF, editor. Edwin Sutherland on analyzing crime. Chicago, IL: University of Chicago Press; 1973. pp. 13–29. [Google Scholar]
- Tabachnick BG, Fidell LS. Using Multivariate Statistics. 5. New York: Allyn and Bacon; 2007. [Google Scholar]
- Topper L, Conrod PJ. A review of the association between alcohol misuse and bullying victimization in adolescence. Mind Brain. 2011 000-1. [Google Scholar]
- Troop-Gordon W. Peer victimization in adolescence: the nature, progression, and consequences of being bullied within a developmental context. Journal of adolescence. 2017;55:116–128. doi: 10.1016/j.adolescence.2016.12.012. [DOI] [PubMed] [Google Scholar]
- Will GJ, van Lier PA, Crone EA, Gü;roğlu B. Chronic childhood peer rejection is associated with heightened neural responses to social exclusion during adolescence. Journal of Abnormal Child Psychology. 2016;44(1):43–55. doi: 10.1007/s10802-015-9983-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams KD. Ostracism: A temporal need-threat model. In: Zanna MP, editor. Advances in experimental social psychology. Vol. 41. San Diego, CA: Elsevier Academic Press; 2009. pp. 275–314. [Google Scholar]
- Yeager DS, Fong CJ, Lee HY, Espelage DL. Declines in efficacy of anti-bullying programs among older adolescents: Theory and a three-level meta-analysis. Journal of Applied Developmental Psychology. 2015;37:36–51. doi: 10.1016/j.appdev.2014.11.005. [DOI] [Google Scholar]