Abstract
As of 2014, approximately 7.4% of U.S. adults had current asthma. The etiology of asthma is complex, involving genetics, behavior, and environmental factors. To explore the association between cumulative environmental quality and asthma prevalence in U.S. adults, we linked the U.S. Environmental Protection Agency’s Environmental Quality Index (EQI) to the MarketScan® Commercial Claims and Encounters Database. The EQI is a summary measure of five environmental domains (air, water, land, built, sociodemographic). We defined asthma as having at least 2 claims during the study period, 2003-2013. We used a Bayesian approach with non-informative priors, implementing mixed-effects regression modeling with a Poisson link function. Fixed effects variables were EQI, sex, race, and age. Random effects were counties. We modeled quintiles of the EQI comparing higher quintiles (worse quality) to lowest quintile best quality) to estimate prevalence ratios (PR) and credible intervals (CIs). We estimated associations using the cumulative EQI and domain-specific EQIs; we assessed U.S. overall (non-stratified) as well as stratified by rural-urban continuum codes (RUCC) to assess rural/urban heterogeneity. Among the 71,577,118 U.S. adults with medical claims who could be geocoded to county of residence, 1,147,564 (1.6%) met the asthma definition. Worse environmental quality was associated with increased asthma prevalence using the non-RUCC-stratified cumulative EQI, comparing the worst to best EQI quintile (PR:1.27; 95% CI: 1.21, 1.34). Patterns varied among different EQI domains, as well as by rural/urban status. Poor environmental quality may increase asthma prevalence, but domain-specific drivers may operate differently depending on rural/urban status.
Keywords: Asthma, environment, claims, MarketScan, Bayesian
1. Introduction
Asthma is a chronic respiratory condition characterized by wheezing, shortness of breath, tightness in the chest, and coughing that results from swollen and narrowed airways.1 From 2001 to 2009, asthma prevalence in the United States (U.S.) increased 12.3%,2 leading to 479,300 hospitalizations and 1.9 million emergency room visits in 2009.3 The overall cost of asthma, including medical costs and lost productivity due to both morbidity and mortality was $56 billion in 2007.4 As of 2014, the prevalence of asthma among U.S. adults was approximately 7.4%.5
Adults may have been diagnosed with asthma as children or may develop it in adulthood. Family history of asthma and atopy, a genetic predisposition to reaction to environmental allergens, increase the risk of asthma, but are more predictive of early-onset asthma in childhood.5,6 In adults, lower educational attainment and lower household income are associated with increased likelihood of having asthma.3,7 Behavior such as smoking and comorbidities such as obesity and depression are also risk factors for asthma in adults.5,8,9
Increasingly, environmental conditions have also been linked to asthma. Ambient air pollution has been associated with incident asthma in U.S. women,10 asthma-related emergency room visits11 and asthma risk in minorities,12 and a meta-analysis of six European cohorts indicated air pollution may be associated with adult-onset asthma.13 In the early 2000s, the built environment was targeted for policy and research to investigate its role in asthma prevalence.14,15 Subsequent studies yielded mixed results. For example, proximity of green areas or tree density near homes has been associated with reductions in atopic sensitization or lower asthma prevalence in some studies of children,16,17 but associated with increased current asthma in others.18,19 Exposure to land use contaminants such as living near an industrial park or concentrated animal feeding operation has been associated with increased risk of asthma in adults.20,21 Similarly, water quality provides another potential mechanism for exposure; for example, deposition of nitrates in water has been associated with respiratory tract infections.22
In short, asthma is a complex condition that is dependent on numerous individual and environmental factors.23 While exposures from multiple domains of the environment have been separately associated with asthma, no comprehensive measure capturing overall environmental quality, including air, water, land, built environment, and sociodemographics, has been examined in association with asthma. Examining asthma prevalence as a function of the many elements of environmental quality to which humans are simultaneously exposed can facilitate an understanding of how these complex exposures interact to affect asthma.
To explore the association between environmental quality and asthma prevalence, we linked the Environmental Quality Index (EQI),24-26 a metric from the U.S. Environmental Protection Agency (US EPA), to the Truven Health MarketScan® Commercial Claims and Encounters Database (hereafter, MarketScan). The EQI integrates information from numerous variables across five environmental domains, enabling a more complete assessment of environmental quality and a better understanding of the role of environmental quality in health outcomes. The EQI has been used in prior studies of health outcomes including cancer incidence, mortality, pediatric multiple sclerosis, and preterm birth, and may also be useful in better understanding asthma.27-30 The MarketScan database is a comprehensive source of individual-level, privately-insured medical claims; as such, MarketScan has data on millions more persons than would be covered in a survey, and is not subject to the same recall or non-response bias that occurs with self-reported surveys.31-33 We estimate the association between cumulative environmental quality and asthma among U.S. adults with health insurance plans captured in MarketScan; we further examine the association between individual environmental domains (air, water, land, built and sociodemographic environments) and asthma prevalence. Because health risk profiles differ in general between rural and urban areas in the U.S.,34 and because asthma studies in particular have indicated mixed results in assessing rural-urban variations,35-38 we additionally explore heterogeneity by county-level rural-urban status.
2. Materials and Methods
2.1. Exposure Data
The Environmental Quality Index (EQI) is a summary measure constructed by the US EPA which incorporates five environmental domains (air, water, land, built, sociodemographic) into a single index representing the years 2000 – 2005 for all counties in the U.S. Data sources; construction of the EQI has been described elsewhere,25,26 and the data, along with an accompanying technical report, are publicly available.24 The air, water, and land domains were identified using the EPA’s Report on the Environment;39 the built and sociodemographics domains were identified using the literature review and consultation with scientists.40 Then, 187 data sources across the five domains were evaluated to assess availability at the county level, availability for all 50 states, availability within the 2000 to 2005 time period, and data quality, which was assessed using reports by data source managers and project investigators, and through research papers that used and critiqued the data sources.25 Those which were retained for their data quality and availability at the county level for the entire U.S. enabled use of 219 unique variables across each of the five domains: air (87 variables), water (80), land (26), built (14), and sociodemographic (12).25 An initial principal components analysis (PCA) produced five domain-specific indices, and a final PCA of the domain-specific indices produced the cumulative EQI.
Because of heterogeneity in environmental quality across the rural-urban continuum, the two-stage PCA process (domain-specific EQIs followed by cumulative EQI) was replicated within each of four rural-urban strata identified using U.S. rural-urban continuum codes (RUCCs).26 RUCCs are a nine-part, county-level classification system defined by the United States Department of Agriculture, Economic Research Service.41,42 For the EQI, these nine categories were collapsed into four rural-urban strata: metropolitan-urbanized (original RUCC 1-3), non-metropolitan urbanized (original RUCC 4-5), less urbanized (original RUCC 6-7), and thinly populated (original RUCC 8-9). The use of these four categories is consistent with prior health studies.43-45
For our main exposure variable, we used quintiles of the EQI to compare higher quintiles (worse quality) to the lowest quintile (best quality). We conducted analyses using the cumulative EQI and the domain-specific indices across the entire U.S, and conducted stratified analyses within each RUCC to examine heterogeneity of effects by rural-urban status. For analyses using the domain-specific indices, all five indices were used in the same model so that associations could be examined in a multi-exposure context.
2.2. Outcome Data
The MarketScan health claims database is a compilation of nearly 110 million patient records with information from more than 100 private insurance carriers and large self-insuring companies. Public forms of insurance (i.e., Medicare and Medicaid) are not included, nor are small (<100 employees) or medium (<1,000 employees) self-insuring companies. For this cross-sectional study, approved claims for the years 2003 to 2013, which includes 17.5 to 45.2 million persons annually, are linked across years and geocoded at the county level. The dataset includes both inpatient and outpatient claims, medical procedures and prescription medications. In addition to diagnostic and pharmacy claims, records include patient’s age (in years), county of residence, and sex. This dataset defines the population in which we are estimating associations, specifically, U.S. adults aged 18 to 65 with private health insurance, primarily from large employers (those with >1,000 employees). We excluded the relatively few (n=6735) individuals over 65 years of age because Medicare is the primary insurance of U.S. adults over 65.
Our final dataset was a person-level dataset that summarized information from the one or more records available on each person to assess whether that person had asthma claims over the study period. Our binary outcome variable, asthma, was defined as adults 18 to 65 years old with at least two asthma claims over the 2003—2013 period, identified in MarketScan by International Statistical Classification of Diseases and Related Health Problems revision (ICD-9) code 493, including 493.22, 493.20, 493.90, 493.91, 493.12, 493.11, 493.10, 493.00, 493.01, 493.02, 493.92, 493.9, 493.8, 493.81, 493.82, 493.2, 493.1, 493.0, and 493.21.46 These claims cover inpatient and outpatient visits, procedures, and prescriptions. Given the possibility of misdiagnosis, we required two distinct asthma claims (in this case, not a prescription) be present to count as an asthma diagnosis. We used as many years of outcome data as possible (through 2013), even though the EQI exposure reflects data only through 2005, because we expect the county level EQI rankings to be stable over time. We also conducted parallel analyses requiring only one claim over the study period to assess the extent to which estimates may change based on the two-claim restriction.
2.3. Covariate Data
Individual-level demographic data such as sex and age are available in the MarketScan data. Adult asthma risk varies by race and ethnicity,47 but individual-level race/ethnicity is not available in MarketScan. However, factors that contribute to asthma may vary by county of residence, and minority composition of a county may partially represent the geographic racial distribution. We included county-level percent racial distributions using 2010 U.S. Census data48 to reflect the aspects of social-environmental exposure that are not included in the EQI. Even though the census-based racial distribution does not reflect the profile of the privately-insured study population, it does reflect the racial distribution of the county environment in which the study population lives.
Covariates included individual-level sex, individual-level age category (18-30 (referent), 31-40, 41-50, 51-65), and county-level race-ethnicity percentages for the following groups: American Indian, Asian, Black Hispanic, Black non-Hispanic, Pacific Islander, White Hispanic, and White non-Hispanic (referent).
2.4. Statistical Analyses
We used a Bayes approach with non-informative (weak) priors, implementing mixed-effects regression modeling with a Poisson link function.49 This approach uses the Poisson distribution to model the distribution of cell counts in a multiway contingency table, and is frequently used to model disease occurrence in insurance claims.50 This approach enabled us to examine whether environmental quality is associated with prevalence of asthma among individuals in our data.
The unit of our analysis (one row in the data matrix) was a specific sociodemographic group at a specific county, for example, females aged 18-30, in Cook County of Illinois. The Poisson regression response variable was the number of persons with asthma in the demographic group, where the total number of people in the group was the regression offset. The assumptions of the Poisson regression model were as follows. First, we assumed that the data, corresponding to the observed counts of people within each county diagnosed with asthma, were generated by a Poisson process, with rate (λij) varying over counties,
where: θ is a vector of all model parameters, (b, Σ). The observed counts of disease incidence (the response variable yij) was defined as the number of disease cases per county j in the given age and sex stratum i. Second, we assumed that the logarithm of Poisson rate (λijkl) was expressed as a linear combination of fixed (age and sex group (k)) and random effects (county (l)).
Here matrix X is the design matrix for the fixed effects; b is the corresponding vector of unknown regression weights; z is a design matrix for random effects; v is the vector of random effects. The fixed-effect design matrix is a matrix of county-specific zero-centered properties, such as the proportions of ethnic groups. The design matrix z has a very simple form: entries of 1 for random effects of a given county, and zeros in all other cells. Nij is a county-, and demographic-stratum-specific offset—the total number of people with a specified sex and age living within a given county. Lastly, we accommodated the fact that data were hierarchical;the random term was at the county level in which the county-level model intercepts could vary.
We estimated posterior distribution of parameter of the model using Monte Carlo Markov Chain (MCMC) algorithm, implemented in R package MCMCglmm.51 Fixed effects variables were EQI, sex, race, age and weather variables. Random effects were counties. We modeled quintiles of the EQI comparing higher quintiles (worse quality) to the lowest quintile (best quality) to estimate prevalence ratios (PR) and credible intervals (CIs). We estimated associations using the cumulative EQI and domain-specific EQIs, and did so for the U.S. overall (non-stratified) as well as stratified by RUCC.
Statistical analyses were conducted in R version 3.2.3 GUI 1.66 Mavericks build (7060).52
2.5. Ethical Considerations
This study involved de-identified claims data on human subjects. It was reviewed and approved by the Institutional Review Board at the University of Chicago.
3. Results
Among the 71,577,118 U.S. adults with medical claims in MarketScan from 2003-2013 who could be geocoded to county of residence, 1,147,564 (1.6%) met the asthma definition of having at least two asthma claims (Table 1). Approximately half (48%) the total population was male; approximately 31% of those with asthma were male. In the total population, the percentages in each age category were similar for individuals ages 18-65, approximately reflecting the age distribution of the general U.S. population.48 Among those with asthma, the greatest percentage (34%) was in the older age group (51-65).
Table 1.
Demographics of unique persons in the MarketScan study population, 2003-2013
| Characteristic (N=71,577,118) |
Total N | % | N unique persons with at least 1 asthma claim |
% | N unique persons with at least 2 asthma claims |
% | |
|---|---|---|---|---|---|---|---|
| Gender | |||||||
| Male | 34,380,820 | 48% | 1,486,408 | 36% | 354,533 | 31% | |
| Female | 37,196,298 | 52% | 2,680,079 | 64% | 793,031 | 69% | |
| Age | |||||||
| 18-30 | 20,487,389 | 29% | 918,545 | 22% | 217,570 | 19% | |
| 31-40 | 15,968,962 | 22% | 892,349 | 21% | 238,337 | 21% | |
| 41-50 | 16,628,351 | 23% | 1,046,318 | 25% | 299,838 | 26% | |
| 51-65 | 18,492,416 | 26% | 1,309,275 | 31% | 391,819 | 34% | |
| Rural-Urban Status | |||||||
| RUCC1: Metro-urbanized | 60,390,968 | 84% | 3,568,689 | 86% | 989,877 | 86% | |
| RUCC2: Non-metro-urbanized | 4,594,342 | 6% | 256,168 | 6% | 68,538 | 6% | |
| RUCC3: Less urbanized | 5,620,691 | 8% | 293,342 | 7% | 76,944 | 7% | |
| RUCC4: Thinly populated | 971,117 | 1% | 48,288 | 1% | 12,205 | 1% | |
Excludes records which could not be geocoded to county.
3.1. Cumulative EQI
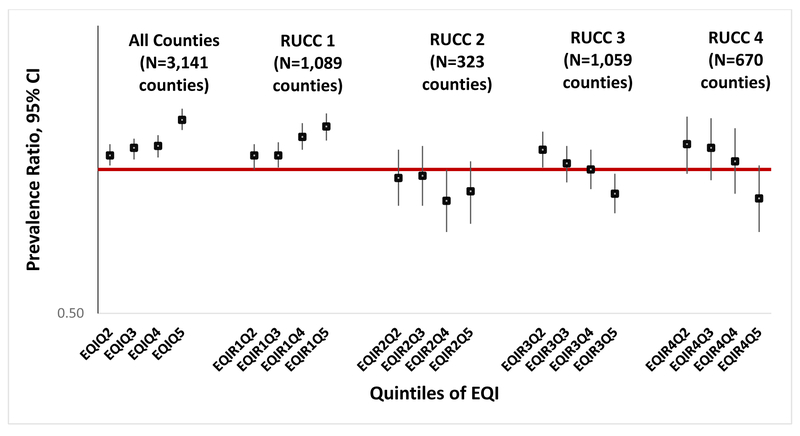
We observed an increased prevalence of asthma associated with worse environmental quality using the non-RUCC-stratified cumulative EQI (Table 2, Figure 1). The worst environmental quality EQI quintile (Q5) had the largest PR (1.27; 95% CI: 1.21, 1.34) relative to the best environmental quality quintile (Q1, referent).
Table 2.
Associations between cumulative EQI and asthma prevalence using 2 claims, all counties and stratified by RUCC
| EQI Quintile |
All Counties (N=3,141 counties) |
RUCC 1: Metropolitan- urbanized (N=1,089 counties) |
RUCC 2: Non- metropolitan urbanized (N=323 counties) |
RUCC 3: Less urbanized (N=1,059 counties) |
RUCC 4: Thinly Populated (N=670 counties) |
|---|---|---|---|---|---|
| PR (95% CI) | PR (95% CI) | PR (95% CI) | PR (95% CI) | PR (95% CI) | |
| Q1 (best) | (referent) | (referent) | (referent) | (referent) | (referent) |
| Q2 | 1.07 (1.02,1.13) | 1.07 (1.00,1.13) | 0.96 (0.84,1.10) | 1.10 (1.01,1.20) | 1.13 (0.98,1.29) |
| Q3 | 1.11 (1.05,1.16) | 1.07 (1.01,1.14) | 0.97 (0.84,1.12) | 1.03 (0.94,1.12) | 1.11 (0.95,1.28) |
| Q4 | 1.12 (1.06,1.18) | 1.17 (1.10,1.25) | 0.86 (0.74,1.00) | 1.00 (0.91,1.10) | 1.04 (0.89,1.22) |
| Q5 (worst) | 1.27 (1.21,1.34) | 1.23 (1.15,1.31) | 0.90 (0.77,1.04) | 0.89 (0.81,0.98) | 0.87 (0.74,1.02) |
EQI: Environmental Quality Index; RUCC: Rural-Urban Continuum Codes; PR: Prevalence Ratio; CI: Credible Interval
Figure 1.
Associations between Environmental Quality Index and having ≥ 2 asthma claims, all counties and stratified by Rural-Urban Continuum Codes
For RUCC-stratified analyses using the cumulative EQI, results varied by stratum (Table 2, Figure 1). For the metropolitan-urbanized stratum (RUCC 1), the association between environmental quality and asthma prevalence monotonically increased with increasingly worse environments. As with the non-stratified cumulative EQI, the worst EQI quintile in RUCC 1 had the largest PR (1.23; 95% CI: 1.15, 1.31) relative to the best quintile.
In RUCC 2 (non-metropolitan urbanized stratum), RUCC 3 (less urbanized) and RUCC 4 (thinly populated), estimates had a less clear pattern and were mostly null. The exceptions were the worst quality environments in RUCCs 3 and 4, which were inversely associated with asthma prevalence (RUCC 3 PR: 0.89 [95% CI: 0.81, 0.98]; RUCC 4 PR: 0.87 [95% CI: 0.74, 1.02]).
3.2. Domain-specific EQIs
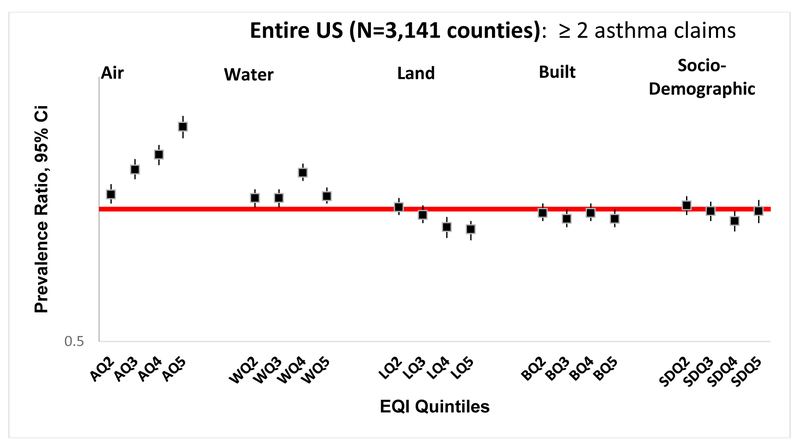
In analyses using each of the individual EQI domains, the most striking results were in the air domain. The non-stratified estimates indicated increased asthma prevalence with worsening air quality; the worst air quality environment had the largest association (PR: 1.54; 95% CI: 1.45, 1.63) (Table 3, Figure 2). Worse water quality was also positively associated with asthma in all quintiles. In the land, built, and sociodemographic domains, worse quality was somewhat negatively associated with increased asthma, with estimates close to null.
Table 3.
Associations between domain-specific EQIs and asthma prevalence using 2 claims, all counties and stratified by RUCC
| EQI Quintile | All Counties (N =3,141 counties) |
RUCC 1: Metropolitan- urbanized (N=1,089 counties) |
RUCC 2: Non- metropolitan urbanized (N=323 counties) |
RUCC 3: Less urbanized (N=1,059 counties) |
RUCC 4: Thinly populated (N=670 counties) |
|---|---|---|---|---|---|
| PR (95% CI) | PR (95% CI) | PR (95% CI) | PR (95% CI) | PR (95% CI) | |
| Air Q1 (best) | (referent) | (referent) | (referent) | (referent) | (referent) |
| Air Q2 | 1.08 (1.03,1.14) | 1.10 (1.03,1.17) | 0.91 (0.79,1.05) | 1.00(0.91,1.09) | 1.04 (0.89,1.21) |
| Air Q3 | 1.23 (1.17,1.30) | 1.18 (1.11,1.26) | 0.95 (0.82,1.10) | 1.01(0.92,1.10) | 0.92 (0.79,1.09) |
| Air Q4 | 1.33 (1.26,1.40) | 1.28 (1.19,1.37) | 0.96 (0.83,1.13) | 1.10(1.01,1.21) | 1.09 (0.93,1.28) |
| Air Q5 (worst) | 1.54 (1.45,1.63) | 1.25 (1.15,1.35) | 1.09 (0.94,1.28) | 1.22(1.11,1.34) | 1.26 (1.08,1.47) |
| Water Q1 (best) | (referent) | (referent) | (referent) | (referent) | (referent) |
| Water Q2 | 1.06 (1.01,1.11) | 1.04 (0.98,1.11) | 1.01 (0.88,1.15) | 1.11(1.02,1.21) | 1.08 (0.94,1.23) |
| Water Q3 | 1.06 (1.01,1.11) | 1.04 (0.98,1.11) | 1.1 (0.95,1.27) | 1.08(0.99,1.17) | 1.34 (1.16,1.54) |
| Water Q4 | 1.21 (1.16,1.27) | 1.11 (1.05,1.18) | 1.06 (0.93,1.22) | 1.30(1.20,1.41) | 1.25 (1.08,1.44) |
| Water Q5 (worst) | 1.07 (1.03,1.12) | 0.98 (0.92,1.04) | 0.98 (0.85,1.13) | 1.16(1.06,1.26) | 1.20 (1.04,1.38) |
| Land Q1 (best) | (referent) | (referent) | (referent) | (referent) | (referent) |
| Land Q2 | 1.01 (0.97,1.06) | 0.98 (0.01,81.35) | 1.03 (0.01,81.13) | 1.01(0.01,88.85) | 1.06 (0.01,84.73) |
| Land Q3 | 0.97 (0.93,1.02) | 0.97 (0.92,1.02) | 0.96 (0.86,1.08) | 1.03(0.96,1.11) | 1.04 (0.92,1.16) |
| Land Q4 | 0.91 (0.86,0.96) | 0.93 (0.89,0.98) | 0.88 (0.79,1.00) | 1.01(0.94,1.09) | 1.06 (0.92,1.21) |
| Land Q5 (worst) | 0.90 (0.85,0.94) | 0.99 (0.01,77.94) | 1.04 (0.01,87.01) | 1.04(0.01,87.18) | 1.06 (0.01,82.38) |
| Built Q1 (best) | (referent) | (referent) | (referent) | (referent) | (referent) |
| Built Q2 | 0.98 (0.94,1.03) | 0.97 (0.91,1.03) | 0.96 (0.84,1.10) | 0.94(0.86,1.01) | 0.93 (0.81,1.06) |
| Built Q3 | 0.95 (0.91,1.00) | 0.99 (0.92,1.06) | 1.05 (0.91,1.20) | 0.90(0.83,0.97) | 0.95 (0.83,1.09) |
| Built Q4 | 0.98 (0.94,1.03) | 0.93 (0.87,1.00) | 0.93 (0.82,1.07) | 0.90(0.83,0.98) | 0.98 (0.85,1.12) |
| Built Q5 (worst) | 0.95 (0.91,1.00) | 0.97 (0.90,1.04) | 0.91 (0.79,1.05) | 0.89(0.81,0.97) | 1.20 (1.04,1.39) |
| Socio Q1 (best) | (referent) | (referent) | (referent) | (referent) | (referent) |
| Socio Q2 | 1.02 (0.97,1.07) | 0.96 (0.91,1.02) | 0.91 (0.79,1.06) | 1.08(0.99,1.17) | 1.17 (1.03,1.33) |
| Socio Q3 | 0.99 (0.94,1.04) | 0.95 (0.90,1.01) | 0.91 (0.77,1.08) | 1.08(0.99,1.19) | 1.16 (1.00,1.34) |
| Socio Q4 | 0.94 (0.89,0.99) | 0.96 (0.90,1.02) | 0.85 (0.71,1.01) | 0.98(0.88,1.09) | 0.93 (0.80,1.10) |
| Socio Q5 (worst) | 0.99 (0.93,1.05) | 0.88 (0.82,0.95) | 0.90 (0.76,1.08) | 0.83(0.75,0.93) | 0.91 (0.78,1.06) |
EQI: Environmental Quality Index; RUCC: Rural-Urban Continuum Codes; PR: Prevalence Ratio; CI: Credible Interval
Figure 2.
Associations between domain-specific between Environmental Quality Indices and having ≥ 2 asthma claims, all counties.
In RUCC-stratified analyses of the domain-specific EQIs, patterns of domain-specific associations varied by RUCC stratum (Table 3). In RUCC 1 (metropolitan urbanized), worsening air quality was associated with increasing asthma, and poor water quality was somewhat associated with increased asthma. However, land quality was not statistically significantly associated with asthma and estimates had broad credible intervals including zero.. In the built and sociodemographic domains, worse quality was not associated or slightly negatively associated with asthma.
The patterns of domain-specific estimates in RUCC 3 (less urbanized) and RUCC 4 (thinly populated) were similar to those of RUCC 1 in the air domain but had more pronounced positive associations in the water domain and slightly positive (but imprecise) associations in the land domain. In RUCC2 (non-metropolitan urbanized) estimates in the air, water, and land domains were close to null. Built environmental quality varied across RUCCs but were mostly null. Sociodemographic environmental qualities also varied across RUCCs but associations were somewhat more pronounced (larger in magnitude), and worsening sociodemographic quality was associated with decreasing asthma prevalence in more rural RUCCs.
3.3. Sensitivity Analyses
As previously noted, we employed a conservative asthma definition of having at least two asthma claims during the study period. Defining asthma as requiring only one claim yielded similar effect estimates, which are presented in Supplemental Tables 1-2 and Supplemental Figures 1-2. We also examined including a third modeling level to cluster counties within states, using a state-specific random effect in addition to county-specific random effects. Estimates were similar to those reported (data not shown). Finally, we considered weather-related variables, but they did not contribute to the associations of interest and were excluded (data not shown).
4. Discussion
We found that worsening cumulative environmental quality is associated with increasing asthma prevalence in U.S. adults captured in MarketScan claims data. Estimates varied, however, across different rural-urban strata, with worsening environmental quality associated with increasing asthma prevalence in the most urban areas (RUCC 1); environmental quality was not associated or inversely associated with asthma in less urban and rural areas (RUCCs 2-4). In domain-specific analyses, decreasing air quality was consistently associated with higher asthma prevalence. Poor water quality was most strongly associated with elevated asthma prevalence in RUCCs 3 and 4, and was still positively associated in the non-RUCC-stratified analysis. Worsening land quality was associated with increasing asthma in stratified analyses for RUCC 3 and 4; however, these associations tended to be small and relatively imprecise with wide credible intervals. Worsening built quality showed inconsistent association with asthma, with some variation in the pattern of association across the stratified analyses, and worsening sociodemographic quality was associated with decreasing asthma in RUCCs 3 and 4.
Our results highlight the complex role of environmental quality in the prevalence of asthma. Prior studies have traditionally focused on single exposures when relating contaminants or environmental features to asthma.10-13,16,20 While studies of single exposures enable specificity, the challenging nature of high dimensional data often prevents accounting for the full context in which those exposures are operating. For example, nitrogen dioxide is thought to increase asthma symptoms.53 However, there are multiple pathways of exposure for pollutants such as nitrates, and nitrates in water have been associated with respiratory tract infections in children.22 By only focusing on the concentration of nitrates in the air, we would be missing the nitrates deposited in the water. The EQI captures both routes of exposure with air and water domain nitrate variables.
Our most meaningful results were in the air domain and in the most urban areas (RUCC 1), consistent with studies indicating that air quality is worse in urban areas. For example, a 2017 CDC surveillance study reported differences between rural and urban air quality; the authors found more unhealthy air-quality days in urban areas.54 This is consistent with the higher density production of pollution from traffic, factories, and human activity in urban areas.
Poor environmental quality was associated with increased asthma in RUCC 1, but patterns were less clear in RUCCs 2-4. Because 84% of the study sample lives in RUCC 1 counties, estimates for RUCC 1 are more precise. This distribution of individuals across RUCCs is consistent with the distribution of the US population across RUCCs.55 The variations across RUCCs may be due to differences in data availability of EQI variables. While all EQI variables were selected for their availability across the entire US, data were generally more profuse in urban areas, whereas data in suburban and rural areas were more likely to rely on estimation techniques. Variables were evaluated based on their overall contributions to a given domain, a process that occurred prior to stratification by RUCC, and may have resulted in different variable selection had the process occurred after stratification.
We observed some heterogeneity in the domain-specific analyses. Associations between poor air quality and asthma across RUCCs are consistent with prior studies of air pollution and asthma.10,11,13 Similar positive associations with water quality across RUCCs suggest potential opportunities for additional research; to our knowledge, no other study has quantified an association between ambient water quality and asthma. Associations in the land domain were difficult to interpret due to the imprecision in the Q2 and Q5 quintiles that likely stems from partitioning of data in those areas. Based on the distribution of the land domain index, the counties in Q2 and Q5 for the land domain may differ from those in other domains in the same RUCC.
Perhaps the most striking variation across RUCCs is in the sociodemographic domain. We would expect that worsening sociodemographic quality would be associated with increased asthma, particularly in urban environments, because the variables contributing to the sociodemographic domain are primarily based on knowledge of sociodemographic deprivation in urban settings; sociodemographic deprivation in suburban and rural settings is not as well understood or defined. Yet, poor sociodemographic quality was counter-intuitively associated with decreased asthma in RUCC 1, and in RUCCs 3 and 4 worsening sociodemographic quality was associated with decreasing asthma prevalence. It is possible that the population represented in this dataset helps explain the unexpected results. We note that the overall prevalence of asthma in this study (1.6%) is substantially lower than that estimated for the U.S (7.4%).5 The MarketScan claims represent a large portion of the U.S. adult population, and the distributions of the study population by RUCC (Table 1) match that of the U.S. population.55 However, this data source does not capture those who are uninsured, and the uninsured are known to be differentially affected by poor health outcomes in general56 and poor asthma management in particular.57 It also does not capture those on state-based insurance (i.e., Medicaid), which represented approximately 15% of US adults in 2011; Medicaid beneficiaries are lower-income and thus also burdened with worse health outcomes, including respiratory diseases.58 In other words, our study population is more affluent than the general population and is differentially advantaged relative to the sociodemographic environment of their county. For those in the worst sociodemographic quintiles in each RUCC, that individual-level advantage may be particularly stark. It is possible that stark contrast confers a health benefit to an individual of higher sociodemographic class in an area that is classified by the EQI as low sociodemographic quality; biologic benefits of social comparison have been previously demonstrated59 and may manifest in this context as well.
The inferences from this study are limited by the cross-sectional design and ecological nature of the exposure. However, we expect that the variables underlying the EQI are relatively stable over time, and that counties do not shift substantially in their relative ranking of environmental quality. Although the exposure is ecological, it provides a comprehensive representation of the environment, including multiple domains important to understanding asthma. Because the outcome is reliant on claims, persons with asthma who do not have an asthma-related claim during the study period will be misclassified as non-asthmatic. However, claims cover inpatient, outpatient, procedure, and prescription drug claims; routine appointments as well as maintenance and rescue medications are likely accessed even if there is not an acute asthma-related event. Furthermore, we assessed a less restrictive outcome definition that only required one claim, and both overall prevalence and estimates of association were similar. Still, the prevalence of individuals with asthma in this dataset, as measured by claims, is much lower than the prevalence in the U.S. The dataset used in this study is limited to privately insured persons in the U.S. aged 18 to 65 who work for large (>999 employees) companies or otherwise have private insurance plans captured by MarketScan. This is a more socioeconomically advantaged population than the U.S. as a whole, likely limiting generalizability.
This study also has several strengths. The EQI offers a novel metric for capturing information from numerous variables across five environmental domains, enabling a more comprehensive assessment of the multitude of simultaneous exposures that may affect asthma prevalence. We controlled for race, but do not expect additional threats from confounding since the EQI is “upstream” of other potentially relevant variables We did examine weather variables as a potential confounder, but did not observe a meaningful change in estimates and excluded the available variables from this analysis. We used MarketScan claims, a rich data source of individual-level data, to estimate the associations between environmental quality and asthma, and leveraged additional information on population demographics and weather by linking additional publicly available data. For parameter estimation, we used a Markov chain Monte Carlo approach. This approach does not rely on assumptions regarding the shape of a likelihood or a posterior distribution surface (as, for example, Laplace approximations do, assuming that the posterior distribution is Gaussian); as a result, the estimated credible intervals are broader than those obtained with a Laplace approximation, but are better estimated. Our study highlights how different aspects of the environment operate together to influence health outcomes. Single exposure studies are limited by the inability to adjust for and directly compare the multitude of environmental exposures to which humans are exposed.60-62 The EQI reduces the dimensionality of the vast quantity of data while retaining the information those data offer. It provides useful information on which domains may be particularly important, accounting for the other domains that would be ignored in most studies.
5. Conclusion
We found evidence that worsening environmental quality is associated with increased asthma prevalence, but that domain-specific drivers of this association may operate differently depending on rural-urban status. The EQI offers an upstream summary measure of the cumulative environment over multiple domains. Future U.S. asthma research may be enhanced through consideration of the EQI as a confounder or effect measure modifier.
Supplementary Material
Associations between Environmental Quality Index and having ≥ 1 asthma claims, all counties and stratified by Rural-Urban Continuum Codes.
Associations between domain-specific Environmental Quality Index and having ≥ 1 asthma claim, all counties.
Associations between cumulative EQI and asthma prevalence, all counties and stratified by RUCC using 1 asthma claim
Associations between domain-specific EQIs and asthma prevalence using 1 claim, all counties and RUCC-stratified
Highlights.
Asthma is a complex condition affecting 7.4% of U.S. adults
Asthma may be driven by multiple exposures operating in tandem
The Environmental Quality Index measures 5 environmental domains simultaneously
Worsening overall environmental quality is associated with increasing asthma
Patterns vary by domain (air, water, land, built, sociodemograhic) and rurality
Acknowledgements
This work was supported by the Office of Research and Development at the U.S. Environmental Protection Agency (contracts EP12D000264, EP09D000003 and EP17D000079 to LCM, contract EP17D000063 to JSJ, and appointment of CLG to the Research Participation Program, administered through the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and the U.S. Environmental Protection Agency); NIH grants 1P50MH094267 and R01HL122712, in addition to DARPA contract W911NF1410333, and a gift from Liz and Kent Dauten; and University of Chicago Clinical and Translational Science Award UL1 TR 002389. The views expressed in this manuscript are those of the authors and do not necessarily reflect the views or policies of the U.S. Environmental Protection Agency. Mention of trade names or commercial products does not constitute endorsement or recommendation for use.
Abbreviations
- CI
confidence interval
- EQI
environmental quality index
- IRB
institutional review board
- MCMC
monte carlo markov chain
- PCA
principal component analysis
- PR
prevalence ratio
- RUCC
rural urban continuum codes
- U.S.
United States
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest
The authors declare they have no conflicts of interest.
References
- 1.US Department of Health and Human Services. National Heart, Lung, and Blood Institute. What is asthma? https://www.nhlbi.nih.gov/health/health-topics/topics/asthma. Accessed September 20,2016.
- 2.CDC U Vital signs: asthma prevalence, disease characteristics, and self-management education: United States, 2001--2009. MMWR Morbidity and mortality weekly report. 2011;60(17):547–552. [PubMed] [Google Scholar]
- 3.U.S. Centers for Disease Control and Prevention. Asthma’s Impact on the Nation. https://www.cdc.gov/asthma/impacts_nation/asthmafactsheet.pdf. Accessed September 20, 2016.
- 4.Barnett SB, Nurmagambetov TA. Costs of asthma in the United States: 2002-2007. The Journal of allergy and clinical immunology. 2011;127(1):145–152. [DOI] [PubMed] [Google Scholar]
- 5.U.S. Centers for Disease Control and Prevention. 2014. National Center for Health Statistics. Fast Stats. http://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2014_SHS_Table_A-2.pdf Accessed Sept 20, 2016.
- 6.London SJ, James Gauderman W, Avol E, Rappaport EB, Peters JM. Family history and the risk of early-onset persistent, early-onset transient, and late-onset asthma. Epidemiology. 2001;12(5):577–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bacon SL, Bouchard A, Loucks EB, Lavoie KL. Individual-level socioeconomic status is associated with worse asthma morbidity in patients with asthma. Respir Res. 2009;10:125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brunner WM, Schreiner PJ, Sood A, Jacobs DR, Jr. Depression and risk of incident asthma in adults. The CARDIA study. American journal of respiratory and critical care medicine. 2014;189(9):1044–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kapadia SG, Wei C, Bartlett SJ, et al. Obesity and symptoms of depression contribute independently to the poor asthma control of obesity. Respiratory medicine. 2014;108(8):1100–1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Young MT, Sandler DP, DeRoo LA, Vedal S, Kaufman JD, London SJ. Ambient air pollution exposure and incident adult asthma in a nationwide cohort of U.S. women. American journal of respiratory and critical care medicine. 2014;190(8):914–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Newman NC, Ryan PH, Huang B, Beck AF, Sauers HS, Kahn RS. Traffic-related air pollution and asthma hospital readmission in children: a longitudinal cohort study. The Journal of pediatrics. 2014;164(6):1396–1402 e1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nishimura KK, Galanter JM, Roth LA, et al. Early-life air pollution and asthma risk in minority children. The GALA II and SAGE II studies. American journal of respiratory and critical care medicine. 2013;188(3):309–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jacquemin B, Siroux V, Sanchez M, et al. Ambient air pollution and adult asthma incidence in six European cohorts (ESCAPE). Environmental health perspectives. 2015;123(6):613–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brisbon N, Plumb J, Brawer R, Paxman D. The asthma and obesity epidemics: the role played by the built environment--a public health perspective. The Journal of allergy and clinical immunology. 2005;115(5):1024–1028. [DOI] [PubMed] [Google Scholar]
- 15.Cummins SK, Jackson RJ. The built environment and children's health. Pediatric clinics of North America. 2001;48(5):1241–1252, x. [DOI] [PubMed] [Google Scholar]
- 16.Ruokolainen L, von Hertzen L, Fyhrquist N, et al. Green areas around homes reduce atopic sensitization in children. Allergy. 2015;70(2):195–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lovasi GS, Quinn JW, Neckerman KM, Perzanowski MS, Rundle A. Children living in areas with more street trees have lower prevalence of asthma. Journal of epidemiology and community health. 2008;62(7):647–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dadvand P, Villanueva CM, Font-Ribera L, et al. Risks and benefits of green spaces for children: a cross-sectional study of associations with sedentary behavior, obesity, asthma, and allergy. Environmental health perspectives. 2014;122(12):1329–1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Andrusaityte S, Grazuleviciene R, Kudzyte J, Bernotiene A, Dedele A, Nieuwenhuijsen MJ. Associations between neighbourhood greenness and asthma in preschool children in Kaunas, Lithuania: a case-control study. BMJ open. 2016;6(4):e010341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Al-Wahaibi A, Zeka A. Health impacts from living near a major industrial park in Oman. BMC public health. 2015;15:524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Radon K, Schulze A, Ehrenstein V, van Strien RT, Praml G, Nowak D. Environmental exposure to confined animal feeding operations and respiratory health of neighboring residents. Epidemiology. 2007;18(3):300–308. [DOI] [PubMed] [Google Scholar]
- 22.Gupta SK, Gupta RC, Seth AK, JK B, A G. Recurrent acute respiratory tract infections in areas with high nitrate concentrations in drinking water. Environmental health perspectives. 2000;108(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Holgate ST. Asthma: a simple concept but in reality a complex disease. European journal of clinical investigation. 2011;41(12):1339–1352. [DOI] [PubMed] [Google Scholar]
- 24.Lobdell DT, Jagai JS, Messer LC, et al. Creating an Overall Environmental Quality Index - Technical Report EPA/600/R-14/304. https://edg.epa.gov/data/Public/ORD/NHEERL/EQI. Washington, DC: U.S. Environmental Protection Agency; 2014. [Google Scholar]
- 25.Lobdell DT, Jagai JS, Rappazzo K, Messer LC. Data sources for an environmental quality index: availability, quality, and utility. American journal of public health. 2011;101 Suppl 1: S277–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Messer LC, Jagai JS, Rappazzo KM, Lobdell DT. Construction of an environmental quality index for public health research. Environmental health : a global access science source. 2014;13(1):39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jian Y, Messer LC, Jagai JS, et al. The Associations between Environmental Quality and Mortality in the Contiguous United States, 2000-2005. Environmental health perspectives. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rappazzo KM, Messer LC, Jagai JS, Gray CL, Grabich SC, Lobdell DT. The associations between environmental quality and preterm birth in the United States, 2000–2005: a cross-sectional analysis. Environmental health : a global access science source. 2015;14:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jagai JS, Messer LC, Rappazzo KM, Gray CL, Grabich SC, Lobdell DT. County-level cumulative environmental quality associated with cancer incidence. Cancer. 2017;123(15):2901–2908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lavery AM, Waldman AT, Charles Casper T, et al. Examining the contributions of environmental quality to pediatric multiple sclerosis. Mult Scler Relat Disord. 2017;18:164–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fowles JB, Fowler E, Craft C, McCoy CE. Comparing claims data and self-reported data with the medical record for Pap smear rates. Eval Health Prof. 1997;20(3):324–342. [DOI] [PubMed] [Google Scholar]
- 32.Fowles JB, Fowler EJ, Craft C. Validation of claims diagnoses and self-reported conditions compared with medical records for selected chronic diseases. J Ambul Care Manage. 1998;21(1):24–34. [DOI] [PubMed] [Google Scholar]
- 33.Ferver K, Burton B, P J. The use of claims data in healthcare research. The open public health journal. 2009;2:11–24. [Google Scholar]
- 34.Moy E, Garcia MC, Bastian B, et al. Leading Causes of Death in Nonmetropolitan and Metropolitan Areas- United States, 1999-2014. MMWR Surveill Summ. 2017;66(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Malik HU, Kumar K, Frieri M. Minimal difference in the prevalence of asthma in the urban and rural environment. Clin Med Insights Pediatr. 2012;6:33–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Roy SR, McGinty EE, Hayes SC, Zhang L. Regional and racial disparities in asthma hospitalizations in Mississippi. The Journal of allergy and clinical immunology. 2010;125(3):636–642. [DOI] [PubMed] [Google Scholar]
- 37.Pesek RD, Vargas PA, Halterman JS, Jones SM, McCracken A, Perry TT. A comparison of asthma prevalence and morbidity between rural and urban schoolchildren in Arkansas. Annals of allergy, asthma & immunology : official publication of the American College of Allergy, Asthma, & Immunology. 2010;104(2):125–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Son JY, Kim H, Bell ML. Does urban land-use increase risk of asthma symptoms? Environmental research. 2015;142:309–318. [DOI] [PubMed] [Google Scholar]
- 39.United States Environmental Protection Agency (EPA): EPA’s 2008 Report on the Environment 2008, Washington, DC: National Center for Environmental Assessment. [Google Scholar]
- 40.DT L, JS J, LC M, et al. Creating an Overall Environmental Quality Index - Technical Report. U.S. Environmental Protection Agency, Washington, DC, EPA/600/R-14/304, 2014 2014. [Google Scholar]
- 41.USDA. United States Department of Agriculture. Rural Urban Continuum Codes, 2003. http://www.ers.usda.gov/data-products/rural-urban-continuum-codes/documentation.aspx#.VEfoLPnF8QE. Updated April 28, 2004. Accessed September 26, 2016 2003.
- 42.Hines F, Brown D, Zimmer J. Social and economic characteristics of the population in metro and nonmetro counties, 1970. Economic Research Service, USDA. Agricultural Economic Report 272. 1970. [Google Scholar]
- 43.Luben TJ, Messer LC, Mendola P, Carozza SE, Horel SA, Langlois PH. Urban-rural residence and the occurrence of neural tube defects in Texas, 1999-2003. Health & place. 2009;15(3):848–854. [DOI] [PubMed] [Google Scholar]
- 44.Messer LC, Luben TJ, Mendola P, Carozza SE, Horel SA, Langlois PH. Urban-rural residence and the occurrence of cleft lip and cleft palate in Texas, 1999-2003. Annals of epidemiology. 2010;20(1):32–39. [DOI] [PubMed] [Google Scholar]
- 45.Langlois PH, Jandle L, Scheuerle A, Horel SA, Carozza SE. Occurrence of conotruncal heart birth defects in Texas: a comparison of urban/rural classifications. The Journal of rural health : official journal of the American Rural Health Association and the National Rural Health Care Association. 2010;26(2):164–174. [DOI] [PubMed] [Google Scholar]
- 46.WHO. International statistical classification of diseases and related health problems. Tenth revision. 2010. [PubMed] [Google Scholar]
- 47.Gorman BK, Chu M. Racial and ethnic differences in adult asthma prevalence, problems, and medical care. Ethnicity & health. 2009;14(5):527–552. [DOI] [PubMed] [Google Scholar]
- 48.U.S. Census. Population Estimates 2000-2010. https://www.census.gov/data/datasets/time-series/demo/popest/intercensal-2000-2010-counties.html. Accessed August 2017.
- 49.Hedeker DR RDG Longitudinal Data Analysis. Univeristy of Chicago: John Wiley & Sons; 2006. [Google Scholar]
- 50.Atkin M Statistical modeling in GLM. Vol xi Oxford: Oxford University Press; 1989. [Google Scholar]
- 51.Hadfield JD. MCMC Methods for Multi-Response Generalized Linear Mixed Models: The MCMCglmm R Package. Journal of Statistical Software 2010;33:1–22. [PMC free article] [PubMed] [Google Scholar]
- 52.R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; 2013. [Google Scholar]
- 53.Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet. 2014;383(9928):1581–1592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Strosnider H, Kennedy C, Monti M, Yip F. Rural and Urban Differences in Air Quality, 2008-2012, and Community Drinking Water Quality, 2010-2015 - United States. MMWR Surveill Summ. 2017;66(13):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.United States Department of Agriculture. Rural Urban Continuum Codes, 2010. https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/ Updated April 28, 2004. Accessed September 1, 2017.
- 56.Hadley J Sicker and poorer--the consequences of being uninsured: a review of the research on the relationship between health insurance, medical care use, health, work, and income. Medical care research and review : MCRR. 2003;60(2 Suppl):3S–75S; discussion 76S-112S. [DOI] [PubMed] [Google Scholar]
- 57.Shields AE. Trends in private insurance, Medicaid/State Children's Health Insurance Program, and the health-care safety net: implications for asthma disparities. Chest. 2007;132(5 Suppl):818S–830S. [DOI] [PubMed] [Google Scholar]
- 58.Kaiser Family Foundation. 2010. Key Facts: Medicaid and the Uninsured. https://kaiserfamilyfoundation.files.wordpress.com/2013/01/8383_rd.pdf. Accessed September 10, 2017.
- 59.Fliessbach K, Weber B, Trautner P, et al. Social comparison affects reward-related brain activity in the human ventral striatum. Science. 2007;318(5854):1305–1308. [DOI] [PubMed] [Google Scholar]
- 60.Stingone JA, Buck Louis GM, Nakayama SF, et al. Toward Greater Implementation of the Exposome Research Paradigm within Environmental Epidemiology. Annu Rev Public Health. 2017;38:315–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Carlin DJ, Rider CV, Woychik R, Birnbaum LS. Unraveling the health effects of environmental mixtures: an NIEHS priority. Environmental health perspectives. 2013;121(1):A6–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Taylor KW, Joubert BR, Braun JM, et al. Statistical Approaches for Assessing Health Effects of Environmental Chemical Mixtures in Epidemiology: Lessons from an Innovative Workshop. Environmental health perspectives. 2016;124(12):A227–A229. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Associations between Environmental Quality Index and having ≥ 1 asthma claims, all counties and stratified by Rural-Urban Continuum Codes.
Associations between domain-specific Environmental Quality Index and having ≥ 1 asthma claim, all counties.
Associations between cumulative EQI and asthma prevalence, all counties and stratified by RUCC using 1 asthma claim
Associations between domain-specific EQIs and asthma prevalence using 1 claim, all counties and RUCC-stratified