Abstract
Background
Work and work environment have a critical influence on adolescent workers' health. They are subjected to more risks than adults. The aim of this study is to examine psychological health outcomes in adolescent workers in the areas of depression, somatization, anxiety, hostility, and negative self-concept, and to investigate any related factors.
Methods
This is a descriptive and cross-sectional study. Research samples were collected from adolescent workers between 15 and 18 years old attending a 1-day mandatory education course at vocational training centers, working 5 days per week in small enterprises. Data were collected using the following instruments: Brief Symptom Inventory, Multidimensional Scale of Perceived Social Support, and Descriptive Characteristics of Children's Assessment Form.
Results
The investigation covers 837 young workers, of whom 675 were males and 162 were females. The majority of the families had low incomes (68.1%). Overall, 33.5% of the adolescents had been hospitalized because of health problems. Their average weekly working hours were 78.1 ± 10.7. Almost 50% of adolescent workers scored above the mean average in the Brief Symptom Inventory, indicating serious pschological health symptoms.Those who scored high for hostility, depression, negative self-concept, anxiety, and somatization were between 45.4% and 48.9% of the sample. Logistic regression analysis was conducted to determine the underlying factors: a perception of “feeling very bad” health conditions was 2.07-fold whereas the rate of “no annual leave” was 0.73-fold, and both were found to be effective on psychological problems.
Conclusion
In this study, it seems likely that psychological health problems are the result of multiple adverse factors including working conditions, annual leave, and health considerations.
Keywords: adolescent workers, child Workers, occupational health, psychological problems, social support
1. Introduction
The increasing worldwide concern over the well-being of adolescent workers has raised awareness over adolescents' working conditions, mainly centering on physical health, but recently also on psychological health. Adolescence is a crucial part of the child development process because of the ongoing physical and psychosocial developments that occur during this stage. Adolescents are subjected to more risks than adults when they are exposed to negative work-related factors [1]. Adolescence refers to ages 10–19 years. Anyone younger than 18 years is defined as a child [2]. According to a report in 2008 by the International Labour Organization, 308 million children between the ages of 5 years and 17 years worldwide were involved in child labor. Comparison of findings in a previous report published by the International Labour Organization in 2004, shows that the number of child workers has decreased by only 17 million. It is also important to note that the total number of child workers in the age group 15–17 years has increased from 127 million to 129 million across the same period [3]. These statistical trends parallel those in Turkey. According to the last Child Labour Survey by the Turkish Statistical Institute, 2012, that covers only registered workers. There were 17 million children in the age group 6–17 years, of which 893,000 were working and almost 67.3% of them were 15–17 years old (boys comprising 68.8%). Almost 45% of them were engaged in agriculture, and half of the rest were engaged in household chores (shopping, cooking, and ironing, looking after younger brother/sisters or older family members, washing dishes, working on the family farm, etc.). However, the majority of them (46.2%) were unpaid family workers [4]. Compared with the Child Labour Survey in 2006, the incidence of adolescent workers has decreased. According to an informal comprehensive report, 75.2% of 15- to 19-year-old adolescent workers living in cities were unregistered in 2006 [5].
There are many side effects of harsh working conditions on adolescent workers' health. They will likely be exposed to violence, accidents, or injury incidents more than nonworking at-school adolescents. In particular, work-related accidents and physical health symptoms on skin, eyes, the respiratory system, and musculoskeletal system were common among adolescent workers [6]. Rates of fatal work accidents have increased in recent years. More than 1,700 workers lost their lives owing to work-related accidents in Turkey in 2015, and of these, almost 4% (n = 63) were younger than 18 years. [7]. The work of Servili and Yartey [8] found that 20% of adolescents who were not working experienced psychological problems, most commonly depression or anxiety. According to limited research on such adolescents, working conditions and environment have a strong influence on their health. For example, in a comparative research project in India and the Philippines on adolescent workers by Hesketh et al. [9], long working hours as well as lack of support from peers and adults were correlated with low psychosocial scores in both countries. Also, working at a young age, not having a day off, and being subjected to nonverbal punishments such as beatings and witholding food were found to be significantly correlated with low psychosocial development in India. Moreover, It was found that adolescent workers smoke more and also report more frequent abuses compared to school adolescents of the same age. They had more physopathological health problems [10]. In a similar research in Nigeria and Turkey, the workers had poor physical development compared to their nonworking counterparts [11], [12]. Moreover, psychological factors also have an important influence on the prevalence of physical symptoms [13].
However, the assessment and prevention of work-related health problems at an early stage in life decreases negative risk factors, and consequently averts psychological issues in later life [8]. In this context, occupational health services have a crucial function to protect the health and safety of youth exposed to work. As key members of the health team, nurses can observe and identify psychological changes in adolescents and initiate an action plan to resolve their problems or refer them to an expert if needed. They can implement health protection and promotion at an early stage prior to the development of problems in adulthood. Based on these considerations, the aim of the study was to examine psychological health outcomes in adolescent workers for symptoms of depression, somatization, negative self-concept, hostility, and anxiety, and to investigate social and work-related factors.
The following research questions were addressed by this study.
Research question 1: What is the prevalence of psychological health symptoms (depression, somatization, negative self-concept, hostility, anxiety) among adolescent workers?
Research question 2: Which factors are related to psychological health in a sample of adolescent workers?
2. Materials and nethods
2.1. Sample and settings
This study is descriptive and cross-sectional. The study population comprised adolescent workers in the 15–18 years age range. The sample was selected using a purposive sampling method from five vocational training centers (VTCs), which had 500 enrolled adolescent workers on the European side of Istanbul. The data were collected in March, April, and May 2012.
The centers are a kind of formal and mandatory school for those who prefer having a specific occupational certificate (hairdressing, electric technician, cooking, etc.) and support their family financially, rather than enrolling in high school after leaving mandatory elementary school at age 14. The adolescents are permitted to attend the VTC 1 day per week, working 7 hours per day for a total 35 hours per week according to the labor law [14] (they work longer in practice). Istanbul is the most developed and crowded city in Turkey with almost 15 million residents. It is the main target of internal migration from inside Turkey and also from abroad [15]. The European side of Istanbul is an attractive place for such migrants owing to the variety of work positions available.
The study consisted of 1,085 adolescent workers, of whom 70 did not fully complete the questionnaire, 126 were absent during the data collection in the VTCs, and 54 refused to participate in the study. The study was conducted during their study days at these VTCs. The researcher informed all participants about the study and then let them complete the questionnaire. It took participants 25–30 minutes to complete all the questionnaires. The final total of children participating in the research was 837 (77.1%).
2.2. Measures
The survey comprised three measurements:
-
•
Descriptive Characteristics of Adolescents Assessment Form—this was modified by the researcher according to similar academic studies, research, and literature. It consisted of the following:
-
1.
Sociodemographic characteristics—including sex, age, education, birthplace, the length of time living in Istanbul, the adults he or she lives with
-
2.
Family characteristics—including the parents' level of education, amount of family income, number of siblings, and their education and working environment
-
3.
Health characteristics—including perceptions about their health, body mass index, any chronic disease under medical control or treatment, any disease or symptoms requiring a medical visit in the past 6 months
-
4.
Working characteristics—including working hours, the amount of time spent at work and off work, number of work breaks, and duration of annual leave
The initial version of the survey form was piloted using 40 students in one of the VTCs. It was found that most of the adolescent workers did not account for all the time they spent at work such as having lunch, break times, and spare time. The survey form was consequently amended to identify the time spent at the job center and time spent on and off work in detail.
-
•
Multidimensional Scale of Perceived Social Support (MSPSS) is a self-reporting inventory that consists of 12 items. It measures perceived social support from family, friends, and significant others [16]. The MSPSS has been translated and adapted for use among Turkish respondents [17]. In this study, the Cronbach alpha was found compatible with previous studies in this research (α = 0.85).
-
•
Brief Symptom Inventory (BSI), developed by Derogatis (1992) [18], is a 53-item inventory adapted from symptom checklist-90 (SCL 90). The validity and reliability of the scale were investigated by Şahin et al in 2002 [19]. It was standardized for use with Turkish adults and adolescents, and has been found to have high reliability and validity values in previous studies. The BSI has five subscales: depression, anxiety, negative self-concept, somatization, and hostility. The scale does not have a cutoff point; high scores indicate the presence of more symptoms [19]. The Turkish version of the BSI has a high validity value and significant psychometric measurements, and the Cronbach alpha was found similar to that reported in previous studies. In this study, the Cronbach alpha of the BSI was 0.95, and the subscales' Cronbach alpha values were as follows: anxiety, α = 0.86; depression, α = 0.88; somatization, α = 0.77; negative self-concept, α = 0.84; and hostility, α = 0.72.
2.3. Statistical analysis
Statistical analyses were conducted using the SPSS version 17 for Windows (SPSS Inc., Chicago, IL, USA). Descriptive statistics of demographic characteristics, family, health, and work characteristics of the study population are presented as numbers, percentages, and mean ± standard deviation (SD). Logistic regression and chi-square tests were used for statistical analyses of the data. The chi-square test was carried out for assessing univariate associations between independent variables and reported psychological symptoms. Logistic regression analysis was applied to identify the independent risk factors for psychological problems. In this process, if BSI and its subscales scores were above the median value, they were coded as 1. If it is not, their scores were coded as 0. All independent variables were taken into consideration.
2.4. Ethical approval
This study was approved by the Ethics Committee of the Cardiology Institute of Istanbul University (no. B.30.2.IST.0510000/36), and permission was obtained from the Directorate of National Education, Istanbul (no. 18796). Then, informed consent forms were given to the managers and teachers, and later to the workers and their families in both verbal and written versions. Then, informed consent was obtained from parents and children prior to the administration of measurements.
3. Results
3.1. Descriptive characteristics of adolescents
3.1.1. Demographic characteristics
More than 80% (n = 675) of the adolescent workers were male. The age range was between 15 years and 18 years. The majority of them (75%) were 17 years and 18 years old (mean age, 17 ± 0.8 years). Almost 72% of the adolescents finished primary school, and more than 45% of them were at their 1st year at the VTC. More than 86% of the workers moved from different parts of Turkey to Istanbul with their families (Table 1).
Table 1.
Sociodemographic and family's characteristics and their relationship to Brief Symptom Inventory (n = 837)
| Independent variables (n) | % | Brief Symptom Inventory |
Statistics | Significance (p) | |
|---|---|---|---|---|---|
| Median ≤ 51 (n = 423), % | Median > 51 (n = 414), % | ||||
| Age (y) | |||||
| 15 (45) | 5.4 | 48.9 | 51.1 | χ2 = 0.601, df = 3 | >0.05 |
| 16 (169) | 20.2 | 52.7 | 47.3 | ||
| 17 (312) | 37.3 | 51 | 49 | ||
| 18 (311) | 37.2 | 49.2 | 50.8 | ||
| Sex | |||||
| Female (162) | 19.4 | 46.9 | 53.1 | χ2 = 1.055, df = 1 | >0.05 |
| Male (675) | 80.6 | 51.4 | 48.6 | ||
| Grade at VTE (in years) | |||||
| First (379) | 45.3 | 48.5 | 51.5 | χ2 = 5.098, df = 2 | >0.05 |
| Second (316) | 37.8 | 49.1 | 50.9 | ||
| Third (142) | 17.0 | 59.2 | 40.8 | ||
| Length of time living in Istanbul | |||||
| 7 y or less (112) | 13.4 | 51.8 | 48.2 | χ2 = 0.08, df = 1 | >0.05 |
| 8 y or more (725) | 86.6 | 50.3 | 49.7 | ||
| Mother's educational level | |||||
| Never attended school(122) | 14.6 | 48.4 | 51.6 | χ2 = 0.867, df = 2 | >0.05 |
| Graduated from primary school (652) | 77.9 | 56.5 | 49.5 | ||
| Graduated from high school or university (63) | 7.5 | 55.6 | 44.4 | ||
| Father's educational level | |||||
| Never attend to school (60) | 7.2 | 60 | 48.3 | χ2 = 1.845, df = 2 | >0.05 |
| Graduated from primary school (642) | 76.7 | 642 | 48.4 | ||
| Graduated from high school or university (135) | 16.1 | 135 | 54.8 | ||
| Father's work situation | |||||
| Works (688) | 82.2 | 51.7 | 48.3 | χ2 = 2.251, df = 1 | >0.05 |
| Does not work (149) | 17.8 | 45.0 | 55.0 | ||
| Mothers work situation | |||||
| Works (188) | 22.5 | 52.7 | 47.3 | χ2 = 0.437, df = 1 | >0.05 |
| Does not work (649) | 77.5 | 49.9 | 50.1 | ||
| Family income | |||||
| Low (570) | 68.1 | 50.9 | 49.1 | χ2 = 0.590, df = 3 | >0.05 |
| Lower middle (116) | 13.9 | 47.4 | 52.6 | ||
| Upper middle (119) | 14.2 | 51.3 | 48.7 | ||
| High (32) | 3.8 | 53.1 | 46.9 | ||
| Ranking among siblings in family | |||||
| First (269) | 32.1 | 49.8 | 50.2 | χ2 = 1.273, df = 2 | >0.05 |
| Second (202) | 24.1 | 54.0 | 46.6 | ||
| Third (366) | 43.1 | 49.2 | 50.8 | ||
| Perceived social support from family | |||||
| Median < 5 (422) | 50.4 | 47.2 | 52.8 | χ2 = 3.893, df = 1 | >0.05 |
| Median > 5 (415) | 49.6 | 54.0 | 46.0 | ||
| Perceived social support from significant others | |||||
| Median < 5 (414) | 49.4 | 49.5 | 50.5 | χ2 = 0.341, df = 1 | >0.05 |
| Median > 5 (423) | 50.6 | 51.5 | 48.5 | ||
| Perceived social support from friends | |||||
| Median < 5 (432) | 51.6 | 48.8 | 51.2 | χ2 = 1.026, df = 1 | >0.05 |
| Median > 5 (405) | 48.4 | 52.3 | 47.7 | ||
| Total MSPSS score | |||||
| Median < 5 (421) | 50.2 | 48.5 | 51.5 | χ2 = 1.468, df = 1 | >0.05 |
| Median> 5 (416) | 49.8 | 52.6 | 47.4 | ||
MSPSS, Multidimensional Scale of Perceived Social Support.
3.1.2. Family characteristics
The vast number of parents had only primary school education, and 77.5% of the mothers did not have any job at this time. The level of illiteracy was higher in their parents, i.e., 122 (14.6%) mothers and 60 (7.2%) fathers. Nonetheless, many of the participants (43.7%) were the youngest members of their families. The family incomes of more than 68% of the participants were low. The MSPSS score was 4.9 ± 1.3 (median = 5), and perceived social support scores from its subscales were as follows: from friends, 4.7 ± 1.7 (median = 5); from family, 5.3 ± 1.6 (median = 5.5); and from significant others, 4.8 ± 1.8 (median = 5.2) (Table 1).
3.1.3. Health characteristics
More than 45% of the participants stated that their health situation was “good”; 33.5% had been admitted to hospitals with symptoms such as headache, sore throat, tingling, arm legs pain, weakness and fatigue; and 10.2% of participants suffered from a chronic disease. Almost 16% of them were underweight (˂19 kg) and 14.2% were overweight (between 25 kg and 29.9 kg) (Table 2).
Table 2.
Health and work characteristics and its relationship to Brief Symptom Inventory (n = 837)
| Independent variables | Brief Symptom Inventory |
Statistics | Significance (p) | ||
|---|---|---|---|---|---|
| Median ≤51 (n = 414), % | Median > 51 (n = 423), % | ||||
| Referred to hospital due to health problems | |||||
| Yes (280) | 33.5 | 44.6 | 55.4 | χ2 = 5.849, df = 1 | <0.05 |
| No (557) | 66.5 | 53.5 | 46.5 | ||
| To having chronic diseases | |||||
| Yes (85) | 10.2 | 44.7 | 55.3 | χ2 = 1.287, df = 1 | >0.05 |
| No (752) | 89.8 | 51.2 | 48.8 | ||
| Body mass index | |||||
| Underweight (130) | 15.5 | 49.2 | 50.8 | χ2 = 0.112, df = 2 | >0.05 |
| Normal (588) | 70.3 | 50.9 | 49.1 | ||
| Overweight (119) | 14.2 | 50.4 | 49.6 | ||
| Health conditions | |||||
| Very bad(34) | 4.1 | 41.2 | 58.8 | χ2 = 21.649, df = 3 | <0.01 |
| Bad (82) | 9.8 | 41.5 | 58.5 | ||
| Good (384) | 45.9 | 44.8 | 55.2 | ||
| Very good (337) | 40.3 | 66.2 | 39.8 | ||
| Occupation | |||||
| Motor mechanic technician (184) | 22 | 53.8 | 46.2 | χ2 = 1.224, df = 2 | >0.05 |
| Electrical technician (142) | 17 | 47.9 | 52.1 | ||
| Hairdressing and barbering (511) | 61.1 | 50.1 | 49.9 | ||
| Time work begins | |||||
| At 7 am (57) | 6.8 | 47.4 | 52.6 | χ2 = 0.473, df = 2 | >0.05 |
| At 8 am (485) | 57.9 | 50.1 | 49.9 | ||
| At 9 am (295) | 35.2 | 51.9 | 48.1 | ||
| Time of leaving from work | |||||
| At 18–20 pm (359) | 42.9 | 52.6 | 47.4 | χ2 = 1.211, df = 2 | >0.05 |
| At 21–23 pm (443) | 52.9 | 48.8 | 51.2 | ||
| At 12 midnight or later (35) | 4.2 | 51.4 | 48.6 | ||
| Working hours (per week) | |||||
| 60–78 h (436) | 52.1 | 51.6 | 48.4 | χ2 = 0.415, df = 1 | >0.05 |
| 79–96 h (401) | 47.9 | 49.4 | 50.6 | ||
| Working hours (per day) | |||||
| 8–12 h | 51.9 | 52.8 | 47.2 | χ2 = 1.789, df = 1 | >0.05 |
| 13–16 h | 48.1 | 48.1 | 51.9 | ||
| Break times | |||||
| Yes (323) | 38.6 | 54.8 | 45.2 | χ2 = 3.821, df = 1 | 0.05 |
| No (514) | 61.4 | 47.9 | 52.1 | ||
| Break time duration | |||||
| N/A (514) | 61.4 | 47.9 | 52.1 | χ2 = 6.671, df = 2 | <0.05 |
| 30 min (147) | 17.6 | 49.2 | 50.3 | ||
| 60 min (176) | 21.0 | 59.1 | 40.9 | ||
| Annual leave | |||||
| Yes (428) | 51.1 | 54.7 | 45.3 | χ2 = 5.992, df = 1 | ≤0.01 |
| No (409) | 48.9 | 46.2 | 53.8 | ||
| Annual leave duration (d) | |||||
| N/A (409) | 48.9 | 46.2 | 53.8 | χ2 = 6.283, df = 3 | >0.05 |
| 7 (164) | 19.6 | 53.7 | 46.3 | ||
| 15 (198) | 23.7 | 56.1 | 43.9 | ||
| 21 (66) | 7.8 | 53.0 | 47.0 | ||
N/A, not available.
3.1.4. Working characteristics
More than 61% of the participants were working in the specialty area of hairdressing and barbering, with 58% of them beginning to work early in the morning (at 8 am), and more than half of them leave work between 9 pm and 11 pm. Thus, the mean average of working hours per day was 13 (SD, 1.7) hours and 78.1 (SD, 10.7) hours per week. The adolescent monthly income ranged between US$116 and US$266. Furthermore, 61.4% had no daily breaks, and 48.9% had no annual leave (Table 2).
3.2. Psychological symptoms of adolescent workers and related factors
3.2.1. Psychological symptoms
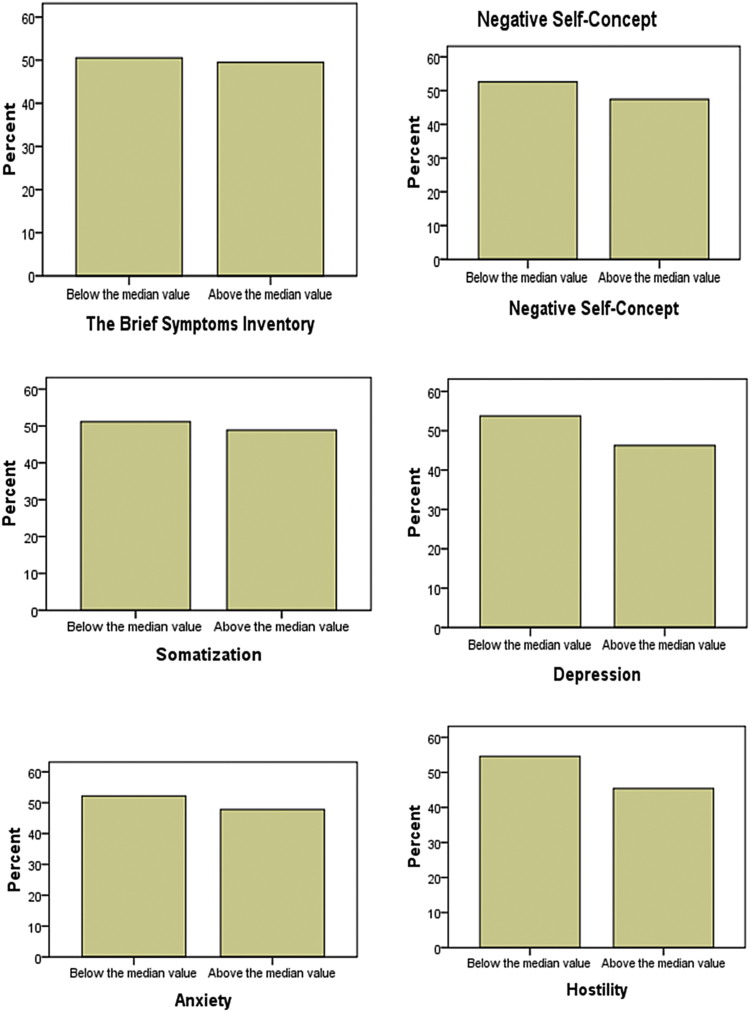
The total BSI score was 57.6 (SD, 36; median = 51). The total score of anxiety was 12.8 (SD, 9.4; median =11); depression, 14.6 (SD, 10.5; median = 13); negative self-concept, 11.9 (SD, 9; median = 10); somatization, 7.7 (SD, 6.1; median = 6); and hostility, 10.4 (SD, 5.6; median = 10) (Table 3). Almost half of the workers (414 workers, 49.5%) had a score exceeding the BSI scale's median point, indicating potentially more psychological health problems (Fig. 1).
Table 3.
Brief Symptom Inventory (BSI) scores (range) of adolescent workers (n = 837)
| Subscales | BSI min–max scores | Min–max scores of BSI in this study | X ± SD | Median |
|---|---|---|---|---|
| Anxiety | 0–52 | 0–52 | 12.8 ± 9.4 | 11 |
| Depression | 0–48 | 0–48 | 14.6 ± 10.5 | 13 |
| Negative self-concept | 0–48 | 0–45 | 11.9 ± 9.0 | 10 |
| Somatization | 0–36 | 0–31 | 7.7 ± 6,1 | 6 |
| Hostility | 0–28 | 0–28 | 10.4 ± 5,6 | 10 |
| Total BSI score | 0–212 | 0–199 | 57.6 ± 36,0 | 51 |
SD, standard deviation.
Fig. 1.
Percentage of psychological health symptoms among adolescent workers.
3.2.2. Factors affecting the prevalence of psychological symptoms
The BSI score of half of the participants were above the median value, indicating high psychological symptoms. Hospital admissions for health problems (p ˂ 0.05), health conditions (p ˂ 0.01), break times (p ˂ 0.05), and lack of annual leave (p ≤ 0.01) were significant factors for psychological symptoms (Table 2). No significance was found, indicating an association between psychological problems and the MSPSS and the subscales (Table 1).
3.2.3. Relationship between risk factors and psychological symptoms
Table 4 (logistic regression) summarises the main statistically significant predictors on BSI and its subscales. “Feeling very bad” [odds ratio (OR) = 2.07; 95% confidence interval (CI), 1.01–4.27) and “no annual leave” (OR = 0.73; 95% CI, 0.55–0.97) had an increased risk of psychological symptoms. The significant predictors on the subscale are as follows:
-
•
Anxiety: The main statistically significant risk factors were “referred to hospital for health problems” (OR = 0.63; 95% CI, 0.47–0.85).
-
•
Depression: The main statistically significant risk factor was “feeling very bad” about their health, which had a 2.44 times higher risk than “feeling very good” (OR = 2.44; 95% CI, 1.08–4.64).
-
•
Somatization: “Being in the 1st year at VTC” had a 1.91 times higher risk than being at 3rd year in the VTC (OR = 1.91; 95% CI, 1.26–2.91), and “feeling very bad” about their health had a 2.57 times higher risk than “feeling very good” (OR = 2.57; 95% CI, 1.54–4.28).
-
•
Negative self-concept: The main statistically significant predictor was “referred to hospital for health problems” (OR = 0.73; 95% CI, 0.57–1.01).
-
•
Hostility: “Daily working hours” (13–16 hours) had 1.35 times higher risk (OR = 1.35; 95% CI, 1.02–1.79), and adolescent workers who had “no annual leave” were 0.74 times more at risk than those with annual leave.
Table 4.
Predictor factors in Brief Symptom Inventory (BSI) and its subscales scores: logistic regression
| BSI and its subscales | Variables | Odds ratio | 95% CI∗ |
|---|---|---|---|
| BSI, Health Conditions (with symptom %) | |||
| (n = 414) | Very bad (58.8) | 2.07 | 1.01–4.27 |
| Bad (58.5) | |||
| Good (55.2) | |||
| Very good (39.8) (ref.) | |||
| BSI, Annual leave (with symptom %) | |||
| (n = 414) | Yes (45.3) (ref.) | 0.73 | 0.55–0.97 |
| No (53.8) | |||
| Anxiety, Grade at VTE (with symptom %) | |||
| (n = 400) | First (48.3) | 1.58 | 1.05–2.38 |
| Second (50.9) | |||
| Third (39.4) (ref.) | |||
| Anxiety, Refer to hospital due to health problems (with symptom %) | |||
| (n = 400) | Yes (55.0) | 0.63 | 0.47–0.85 |
| No (44.2) (ref.) | |||
| Depression, Health conditions (with symptom %) | |||
| (n = 387) | Very bad (58.8) | 2.44 | 1.08–4.64 |
| Bad (58.5) | |||
| Good (51.0) | |||
| Very good (36.5) (ref.) | |||
| Somatization, Health conditions (with symptom %) | |||
| (n = 409) | Very bad (55.9) | 2.57 | 1.54–4.28 |
| Bad (54.9) | |||
| Good (47.7) | |||
| Very good (39.5) (ref.) | |||
| Somatization, Grade at VTE (with symptom %) | |||
| (n = 409) | First (51.7) | 1.91 | 1.26–2.91 |
| Second (51.6) | |||
| Third (35.2) (ref.) | |||
| Negative self-concept, Grade at VTE (with symptom %) | |||
| (n = 397) | Yes (54.3) | 0.73 | 0.53–1.00 |
| No (44.0) (ref.) | |||
| Hostility, Working hours a day (with symptom %) | |||
| (n = 380) | 13–16 h (49.4) | 1.35 | 1.02–1.79 |
| 10–12 h (41.7) (ref.) | |||
| Hostility, Annual leave (with symptom %) | |||
| (n = 380) | No (49.9) | 0.74 | 0.56–0.98 |
| Yes (41.1) (ref.) | |||
95% confidence interval.
4. Discussion
Work and the working environment have a strong influence on health. Adolescent workers' health is affected more compared to adults by work-related risk factors. The present research investigated the psychological symptoms of depression, anxiety, negative self-concept, hostility, and somatization and related factors among a statistically important number of adolescent workers in Istanbul, Turkey.
4.1. Psychological health symptoms of adolescent workers
The prevalence of psychological symptoms among adolescent workers was found to be higher compared to similar research in the literature [20], [21]. The total BSI score significantly exceeded the median point, which gives rise to psychological health problems in this study. Also, the subscales scores were higher than the median value. Examined in detail, more than 49% of workers had serious psychological health problem symptoms. Compared to adolescent boys, the girls had more psychological symptoms in the study, and this was congruent with results of research elsewhere [20]. Adolescent workers aged 14–19 years working as electricians, engineers, hairdressers, barbers, and also studying at VTCs in the west of Turkey, showed a lower rate of psychological symptoms [21]. However, a similar research was conducted on 13- to 17-year-old students who were studying at elementary and high schools in the capital of Turkey, Ankara [19]. The anxiety scores there were 14.25 (SD, 9.89); depression, 14.58 (SD, 10.27); somatisation, 3.37 (SD, 3.73); negative self-concept, 5.40 (SD, 4.99); and hostility scores, 4.94 (SD, 3.91). When the scores were compared to the research, anxiety and depression scores were higher, but negative self-concept, hostility, and somatization scores were lower. Istanbul is the most developed, crowded city in Turkey. So, it is much more expensive and difficult to live in the area compared with other cities in Turkey, which also affects their psychology. It depends on several factors, but the younger you are, the more likely you are to have health problems under similar working conditions. Fekadu et al. [22] studied 528 child workers aged 5–15 years employed in domestic service, street, and private enterprise, and compared them with 472 noneconomically active controls. They found that the “childhood emotional and behavioral disorders” rate was higher in street child workers at 20.1%. It is not easy to compare this result with this study because of the different measurements used, but the child workers probably will have much complicated and serious health problems when they reach post-adolescence.
It was found that individuals suffering from depression often demonstrate somatic symptoms rather than mood disorder symptoms. These included pain, weakness, dizziness, tremors, fatigue, gastrointestinal symptoms, pain in epigastrium, feeling pressure on chest, headaches, and “tingling” in different parts of the body [23]. The results of this study were congruent with these findings. Almost 34% of these adolescent workers had applied for medical help because of physical symptoms (headache, sore throat, flame, arm–shoulder–legs pain, weakness, and fatigue). Some research also showed that depression and somatization psychological problems increased the prevalence and intensity of pain in different parts of the body [24], [25]. Those who were admitted to hospitals because of physical symptoms also had high levels of anxiety and negative self-concept. However, cultural differences and approaches have a significant influence on psychological problems and their prevalence. In less-developed societies, people tend to be more open about physical health problems, which are accepted and receive attention, support, and value from the community, rather than psychological health problems, which are likely to make them feel humiliated. People with psychological problems are mostly stigmatized as “mad and weak,” which discouraged them from expressing their emotional feelings [26].
4.2. Associated and predictor factors with psychological symptoms of adolescent workers
There was no statistically significant correlation between family characteristics and psychological symptoms in this study. Also, perceived social support from family, friends, and significant others was measured using the MSPSS, and there was no significant statistical correlation with psychological symptoms. However, it was documented elsewhere that if individuals receive social support at the adolescent stage, they readily develop self-esteem, become successful in academic life, and are able to cope with stressful situations in their life. They also have more positive expectations about the future [27]. Support from peer groups also has a strong influence on their psychological development. A significant correlation was found between psychological health and poor support from peers or significant other in their lives in India and Philippines [9]. In addition, family economic conditions have a strong influence on adolescent health [28]. According to many studies on adolescent workers, the most common reason for working was poverty [9], [20], [22]. As a result, approximately 2.5 million children were prevented from attending school mainly because of the inability to pay school expenses and the necessity of working to help support their families in Turkey [5].
In this research, their health conditions were found to be strongly predictive of psychological well-being. The most common predictors were the lack of annual leave and having bad health. However, the main factors for psychological health symptoms were related to working conditions, such as having break times, lack of annual leave, daily working hours (8–16 hours per day), and beginning work at a very early time (8 am). The results were found to be similar to those in some studies; however, a systematic review of 17 studies did not find a similar relationship in 10 studies [29]. Moreover, beginning work at 8 am, especially in Istanbul, is really challenging. When we count the average time spent for transport, at work, and for other daily activities, there would not be enough time left for resting or for getting sufficient sleep. For all that, in their study, Lee et al. [30] found that anxiety was associated with sleep quality but not with working conditions. However, there was a strong correlation between hostility and negative self-concept for those with no annual leave and long daily working hours in this study. In addition, long working hours also cause adolescents to feel incapable and angry and to experience loss of self-confidence, disappointment, and low self-esteem [31]. In studies conducted on adolescent workers, in correlation to Turkey, there was a similar significant association between working conditions and health of adolescents [6], [20]. Even though daily working time (11 hours) was less than this study, there was still a significant correlation between psychopathology and physical development. It can be seen that the working hours of this group have increased rather than being limited by the law. Legally, they are just allowed to work 7 hours per day and 35 hours per week as mandated by legislation. In particular, beginning work at 8 am is very challenging considering the developmental stage that adolescents go through and also because of the traffic jams that normally clog metropolitan cities such as Istanbul.
In conclusion, the study has provided evidence that work and working conditions have a strong influence on psychological health. These factors have an increased negative impact on children's health compared to adults because of their developmental stage. It is important to determine psychological symptoms at an early age to prevent future complications. Ultimately, these findings can be used as guidelines for the prevention of psychological health problems in adolescent workers by health professionals. In addition, the results could justify establishing official investigators to review the work conditions, and collaborations between the national adolescent labor, education, and health organizations about taking steps for amending legal requirements.
4.3. Strengths and limitations of the study
The strength of this study is the application of a reliable large sample and valid measurements to the data. The results of the study are limited to the sample, and the data were based on self-reporting and the probability of conferred report bias. Furthermore, the study consisted of just five VTCs in Istanbul. As such, the results cannot be generalized to all adolescent workers in Turkey.
Conflicts of interests
Neither author has conflicts of interest to disclose.
Acknowledgments
The abstract of this study was an oral presentation under the title “Psychological problems and related factors among working children in urban Istanbul, Turkey” at the 5th FOHNEU Congress in Tarragona, Spain, on 19–21 September 2012. We give special thanks to all children for participating in the study and also to Julie Staun RN, CRNA; OHN, doctoral candidate, University of Cumbria, United Kingdom, former President of the Federation of Occupational Health Nurses within EU, International Representative, the Danish Society of Occupational Health Nurses for editing of the English text. This study was supported by the Research Fund of Istanbul University (Project No. 15949).
References
- 1.Thabet A.A., Matar S., Carpintero A., Bankart J., Vostanis P. Mental health problems among labour children in the Gaza Strip. Child Care Health Dev. 2011;37:89–95. doi: 10.1111/j.1365-2214.2010.01122.x. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization [Internet]. Adolescent health. World Health Organization. 2016 [cited 2016 June 16]. Available from: http://www.who.int/topics/adolescent_health/en/.
- 3.Gonzalez ER, Cockburn W, Irastorza X [Internet]. European Survey of Enterprises on New and Emerging Risks. Managing safety and health at work. European Agency for Safety and Health at Work. 2010 [cited 2016 June 16]. Available from: https://osha.europa.eu/en/node/6745/file_view.
- 4.Turkish Statistical Institute (TurkStat) [Internet]. Turkish Statistical Institute Child Labour Force Survey 2012. Turkish Statistical Institue, Ankara, Turkey. 2013 [cited 2016 July 16]. Available from: http://www.turkstat.gov.tr/PreHaberBultenleri.do?id=13659.
- 5.Candaş A, Buğra A, Yilmaz V, Günseli S, Yakut Çakar B. [Internet]. Türkiye’de eşitsizlikler: kalici eşitsizliklere genel bir bakiş (Inequalities in Turkey: an overview of permanent inequalities). Boğaziçi Üniversitesi, Istanbul. 2010 [cited 2016 July 16]. Available from: http://www.aciktoplumvakfi.org.tr/pdf/turkiyede_esitsizlikler.pdf.
- 6.Esin M.N., Bulduk S., Ince H. Work-related risks and health problems of working children in urban Istanbul, Turkey. J Occup Health. 2005;47:431–436. doi: 10.1539/joh.47.431. [DOI] [PubMed] [Google Scholar]
- 7.Isci Sagligi ve Is Guvenligi Meclisi (Workers Health and Occupational Safety) [Internet]. 2015 yilinda en az 1730 işçi yaşamini yitirdi (At least 1730 workers lost their life in 2015). Istanbul, Turkey. 2016 [cited 2016 July 16]. Available from: http://www.guvenlicalisma.org/index.php?option=com_content&view=article&id=168512015-yilinda-en-az-1730-isci-yasamini-yitirdi&catid=149:is-cinayetleri raporlari&Itemid=236.
- 8.Servili C, Yartey J [Internet]. Adolescent Mental Health; Mapping actions of nongovermental organizations and other international developmental organization. Switzerland: World Health Organization, United Nations Children’s Fund. 2012. [cited 2016 July 16]. Available from: http://apps.who.int/iris/bitstream/10665/44875/1/9789241503648_eng.pdf.
- 9.Hesketh T.M., Gamlin J., Ong M., Camacho A.Z.V. The psychosocial impact of child domestic work: a study from India and the Philippines. Arch Dis Child. 2012;97:931. doi: 10.1136/archdischild-2012-301816. [DOI] [PubMed] [Google Scholar]
- 10.Nuwayhid I.A., Usta J., Makarem M., Khudr A., El-Zein A. Health of children working in small urban industrial shops. Occup Environ Med. 2005;62:86–94. doi: 10.1136/oem.2004.015503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Duyar I., Özener B. Growth and nutritional status of male adolescent laborers in Ankara, Turkey. Am J Phys Anthropol. 2005;128:693–698. doi: 10.1002/ajpa.20064. [DOI] [PubMed] [Google Scholar]
- 12.Omokhodion F.O., Omokhodion S.I. Health status of working and non-working school children in Ibadan, Nigeria. Ann Trop Paediatr. 2004;24:175–178. doi: 10.1179/027249304225013457. [DOI] [PubMed] [Google Scholar]
- 13.Pinheiro M.B., Ferreira M.L., Refshauge K., Maher C.G., Ordoñana J.R., Andrade T.B., Tsathas A., Ferreira P.H. Symptoms of depression as a prognostic factor for low back pain: a systematic review. Spine J. 2016;16:105–116. doi: 10.1016/j.spinee.2015.10.037. [DOI] [PubMed] [Google Scholar]
- 14.Regulations: 25425 [Internet]. Labour Act Hours of Work Regulations,Mevzuat Geliştirme ve Yayin Genel Müdürlüğü, Ankara, Turkey, 2004. [cited July 16].Available from: file:///C:/Users/pc/Downloads/TUR87408%20Turk.pdf.
- 15.Turkish Statistical Institute (TurkStat) [Internet]. Main Statics: Population and Demography. Turkish Statistical Institue, Ankara, Turkey. 2015 [cited 2016 July 16]. Available from: http://www.turkstat.gov.tr/UstMenu.do?metod=temelist.
- 16.Zimet G.D., Dahlem N.W., Zimet S.G., Farley G.K. The multidimensional scale of perceived social support. J Pers Assess. 1988;52:30–41. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
- 17.Eker D., Arkar H. Perceived social support: psychometric properties of the MSPSS in normal and pathological groups in a developing country. Soc Psychiatry Psychiatr Epidemiol. 1995;30:121–126. doi: 10.1007/BF00802040. [DOI] [PubMed] [Google Scholar]
- 18.Derogatis L.R. Clinical Psychometric Research Inc; USA: 1992. The Brief Symptom Inventory-BSI administration, scoring and procedures manual-II. [Google Scholar]
- 19.Şahin N.H., Batigün A.D., Uğurtaş S. Kisa Semptom Envanteri (KSE): Ergenler için kullaniminin geçerlik, güvenilirlik ve faktör yapisi [The validity, reliability and factor structure of the Brief Symptom Inventory (BSI)] Turk Psikiyatri Derg. 2002;13:125–135. [PubMed] [Google Scholar]
- 20.Caglayan C., Hamzaoglu O., Yavuz C.I., Yüksel S. Working conditions and health status of child workers: cross-sectional study of the students at an apprenticeship school in Kocaeli. Pediatr Int. 2010;52:6–12. doi: 10.1111/j.1442-200X.2009.02881.x. [DOI] [PubMed] [Google Scholar]
- 21.Bozkurt S., Çam O. Calisan ergenlerde ofke bilesenleri ile ruhsal belirtiler arasindaki iliskinin incelenmesi [Investigation of the relationship between anger components and mental symptoms in working adolescents] Arch Neuropsychiatry. 2010;47:105–111. [Google Scholar]
- 22.Fekadu A., Kebede D., Alem A., Fekadu D., Mogga S., Negash A., Medhin G., Beyero T., Shibre T. Clinical outcome in bipolar disorder in a community-based follow-up study in Butajira, Ethiopia. Acta Psychiatr Scand. 2006;114:426–434. doi: 10.1111/j.1600-0447.2006.00825.x. [DOI] [PubMed] [Google Scholar]
- 23.Sayar K., Kirmayer L.J., Taillefer S.S. Predictors of somatic symptoms in depressive disorder. Gen Hosp Psychiatry. 2003;25:108–114. doi: 10.1016/s0163-8343(02)00277-3. [DOI] [PubMed] [Google Scholar]
- 24.Ailliet L., Rubinstein S.M., Knol D., Van Tulder M.W., de Vet H.C.W. Somatization is associated with worse outcome in a chiropractic patient population with neck pain and low back pain. Man Ther. 2016;21:170–176. doi: 10.1016/j.math.2015.07.007. [DOI] [PubMed] [Google Scholar]
- 25.Fernández-Muñoz J.J., Palacios-Ceña M., Cigarán-Méndez M., Ortega-Santiago R., de-la-Llave-Rincón A.I., Salom-Moreno J., Fernández-de-las-Peñas C. Pain is associated to clinical, psychological, physical, and neurophysiological variables in women with carpal tunnel syndrome. Clin J Pain. 2016;32:122–129. doi: 10.1097/AJP.0000000000000241. [DOI] [PubMed] [Google Scholar]
- 26.Baskak B., Çevik A. Somatizasyonun kültürel boyutlari [Cultural aspects of somatization] Türkiye’de Psikiyatri. 2007;9:50–57. [Google Scholar]
- 27.Kaltiala-Heino R., Rimpelä M., Rantanen P., Laippala P. Adolescent depression: the role of discontinuities in life course and social support. J Affect Disord. 2001;64:155–166. doi: 10.1016/s0165-0327(00)00233-0. [DOI] [PubMed] [Google Scholar]
- 28.Miller M.E. Child labor and protecting young workers around the world: an introduction to this issue. Int J Occup Environ Health. 2010;16:103–112. doi: 10.1179/107735210799160435. [DOI] [PubMed] [Google Scholar]
- 29.Fujino Y., Horie S., Hoshuyama T., Tsutsui T., Tanaka Y. A systematic review of working hours and mental health burden. Sangyo Eiseigaku Zasshi. 2006;48:87–97. doi: 10.1539/sangyoeisei.48.87. [DOI] [PubMed] [Google Scholar]
- 30.Lee K.H., Chae C.H., Kim Y.O., Son J.S., Kim J.H., Woo Kim C., Ouk Park H., Ho Lee J., Saeng Jung Y. Anxiety symptoms and occupational stress among young Korean female manufacturing workers. Ann Occup Environ Med. 2015;27:1. doi: 10.1186/s40557-015-0075-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bandeali S., Jawad A., Azmatullah A., Liaquat H.B., Aqeel I., Afzal A., Umal A., Abidi K., Israr S.M. Prevalence of behavioural and psychological problems in working children. J Pak Med Assoc. 2008;58:345. [PubMed] [Google Scholar]