Abstract
Background
Cardiovascular diseases are among the most common causes of death in industrialized countries. The goal of the DECADE study (“decision aid, action planning, and follow-up support for patients to reduce the 10-year risk of cardiovascular diseases”) is to improve patient activation and health-related behavior by means of structured cardiovascular risk counseling and DECADE brochures. In this pilot study, the applicability of DECADE and the potential effects of the intervention on patients with cardiovascular risk factors were investigated.
Methods
87 patients were included in the two-arm, randomized, controlled pilot study. All of them participated in four structured counseling sessions. The A+D group received DECADE brochures (intervention group), while the A group did not (control group). The change in patient activation four months later (PAM13-D) was the primary endpoint. Secondary endpoints included, among others, changes in health status and health-related behavior, goal achievement, and patient satisfaction. These changes were studied in an intention-to-treat analysis.
Results
Endpoint data were available for 78 patients (38 in the A+D group and 40 in the A group) at four months. The use of DECADE brochures had a significant beneficial effect on PAM13-D scores (an increase of 3.30 points, p = 0.023), corresponding to a moderate effect size of 0.54. Positive trends were seen in most of the other endpoints. The improved patient activation was associated with an overall reduction of risk factors.
Conclusion
This pilot study shows that DECADE can support patient activation. The effects can be expected to be stronger in a larger study and in comparison to usual care. If this can be confirmed, DECADE should be embedded in routine patient care.
Cardiovascular diseases are among the most common causes of death in industrialized countries (1) and the most common cause for seeking treatment from a primary care physician (2). Cardiovascular risk (CVR) consultations are therefore among the most important tasks of primary care physicians (3). Most patients, however, have difficulty in putting into practice health promoting behavior changes to lower their cardiovascular risk (CVR) (4, 5). Studies have found that patient activation in the sense of knowledge, skills and confidence in managing one’s own health (6) is associated with the willingness to adopt health-relevant behaviors (7, 8). Primary care physicians often experience physician–patient communication in this setting as demotivating (9, 10). At the same time, a lack of time on the physician’s part will prevent regular and patient-oriented risk consultations embedded in routine care (11, 12). Rehabilitation research and evaluations of different disease management programs, by contrast, have shown that structured treatments can have positive effects on patient-relevant endpoints and clinical parameters (13, 14).
In order to improve cardiovascular risk consultations, we developed in an iterative process the intervention DECADE—“decision aid, action planning, and follow-up support for patients to reduce the 10-year risk of cardiovascular diseases”. The study protocol includes details on the development process (15).
DECADE is based on the principles of evidence-based medicine, shared decision making (16) while using decision aids (17), and the health action process approach (HAPA) (18) and links these to structured follow-up consultations. The aim of DECADE is to support patients’ health literacy and self-management in a participatory process so that patients’ health is promoted in the long run.
DECADE links the use of the cardiovascular risk calculator Arriba (www.arriba-hausarzt.de/arriba) (3, 19)—which is recommended in the general practice guideline of the German Society of General Practice/Family Medicine—with structured follow-up consultations (table 1). In these consultations, treatment objectives are agreed in a participatory process, and plans to change behaviors are discussed, as are successes or a lack thereof. In order to support patient activation and targeted communication between doctors and patients, the patients receive DECADE brochures, which are structured as modules. These brochures contain evidence-based decision aids and action plans and are matched to the follow-up consultations. In the sense of shared decision making, the brochures are intended as a support offering for the patients and may be used according to their own needs.
Table 1. DECADE: structured follow-up consultations.
| Start | + 1 week | + 4 weeks | + 4 weeks (if needed) | + 7 weeks |
| Arriba consultation: CVR score, treatment options |
Goal agreements and plans for changing behaviors | Follow-up consultation: Successes/lack of success/ changing goals and plans if needed |
Follow-up consultation: Successes/lack of success/ changing goals and plans if needed |
Arriba consultation: CVR score, treatment options + follow-up consultation |
| DECADE brochures |
CVR score, cardiovascular risk score; DECADE, decision aid, action planning, and follow-up support for patients to reduce the 10-year risk of cardiovascular diseases
Readers who have an interest in viewing the DECADE brochures are advised to direct their request to the first author.
We are not aware of any other intervention that includes a similarly complex, but still easy-access, approach to cardiovascular risk consultations.
The research questions of this pilot study were:
Can the DECADE intervention be successfully implemented in the primary care setting?
Does using the DECADE brochures have a greater effect in terms of patient activation and health behaviors than structured follow-up consultations alone?
Patient activation as the primary endpoint was assessed by using the Patient Activation Measure (PAM13-D) (20). The changes in health behaviors were elicited by direct questioning (21) and documented using questions on risk factors, such as smoking and lack of exercise (22). Additionally, we asked about health status (EQ-VAS, European quality of life—visual analogue scale) (23), whether health goals had been achieved (24), and about satisfaction, and we analyzed changes in clinical parameters.
Methods
Details of the methods are described in the eMethods section.
Study design
Adult patients with at least one risk factor for cardiovascular diseases were included in the two-arm, randomized controlled pilot study. All patients received an Arriba printout for patients, and four structured follow-up consultations. The patients in the A+D group also had DECADE brochures at their disposal, whereas no further interventions were made available to patients in group A (control group).
Data collection and endpoints
At the time of inclusion in the study (T0) and after four months (T1), patients completed a questionnaire. At the end of the study, primary care physicians were interviewed.
The primary endpoint was the change in patient activation (PAM13-D) (20). Secondary endpoints were:
Improvement in health status (EQ-VAS) (23).
Change in risk factors (22)
Change in general health behaviors (21)
Achieving self-determined goals (24)
Satisfaction with achieved goals and structured consultations
Usefulness of patient information materials (usefulness scale for patient information material, USE) (25).
Changes in clinical parameters were studied as additional endpoints.
Statistical analyses
The analyses were conducted in the intention-to-treat (ITT) population, which included all patients with available data according to the randomized intervention. We used linear regression models to analyze the effects of the DECADE brochures on the endpoints. Goal attainment, satisfaction, and associations of the PAM13-D score with patient characteristics were analyzed descriptively. We qualitatively evaluated subjects’ free-text responses (to open questions) and interviews with the primary care physicians.
Results
The use of the DECADE brochures was found to have a positive effect on patient activation (difference 3.30 points on a scale of 1–100, 95% confidence interval CI: [0.47; 6.14], p = 0.023 with a moderate effect size of 0.54). Health status in the A+D group compared with the A group improved by 5.79 points on a scale of 0–100 (95% CI: [–0.69; 12.21], p = 0.076 with a small effect size of 0.44). We did not see any relevant effects on the clinical parameters (table 2a). Altogether, the descriptive analyses in the A+D group showed tendentially improved health behaviors compared with the A group, in general (55.9% versus 43.2%) as well as in terms of exercise (40.5% versus 25.6%) and stress (40.5% versus 12.5%) (table 2b).
Table 2a. Mean changes*1 in endpoints between T0 and T1 and estimated effects (mean differences) between the two study arms.
| Endpoints | A group | A+D group |
Estimated effect |
95% CI |
p-value (two-sided) |
Effect size *5 | ||||
| n | T1–T0 | 95% CI | n | T1–T0 | 95% CI | |||||
| PAM13-D*2 | 39 | −1.81 | [−3.78 to 0.17] | 38 | 1.50 | [−0.53 to 3.52] | 3.30 | [0.47 to 6.14] | 0.023 | 0.54 |
| EQ-VAS*3 | 37 | 1.05 | [−3.42 to 5.51] | 36 | 6.84 | [2.33 to 11.35] | 5.79 | [−0.63 to 12.21] | 0.076 | 0.44 |
| CVR score*4 (%) | 40 | 1.36 | [−0.42 to 3.13] | 38 | 0.83 | [−1.01 to 2.68] | –0.53 | [−3.10 to 2.05] | 0.685 | −0.09 |
| Systolic blood pressure *4 (mm Hg) |
40 | 2.80 | [−0.81 to 6.41] | 38 | 4.21 | [0.48 to 7.95] | 1.41 | [−3.78 to 6.60] | 0.589 | 0.12 |
| Total cholesterol*4 (mg/dL) | 40 | −1.13 | [−9.60 to 7.34] | 38 | –2.25 | [−11.04 to 6.54] | –1.13 | [−13.34 to 11.09] | 0.855 | −0.04 |
| HDL cholesterol*4 (mg/dL) | 40 | −0.80 | [−2.87 to 1.27] | 38 | 0.60 | [−1.55 to 2.75] | 1.40 | [−1.57 to 4.38] | 0.350 | 0.21 |
| BMI*4 | 37 | 0.185 | [−0.23 to 0.60] | 35 | –0.15 | [−0.59 to 0.28] | –0.33 | [−0.94 to 0.27] | 0.272 | −0.27 |
BMI, body mass index; CVR score, cardiovascular risk score; EQ-VAS, European quality of life—visual analogue scale (subjective health status);
HDL cholesterol, high density lipoprotein cholesterol; CI, confidence interval; n, number; PAM13-D, German version of Patient Activation Measure questionnaire;
T0, time point of study inclusion (baseline); T1, time point after four months (follow-up)
*1 Adjusted means
*2 Primary endpoint patient activation (PAM13-D), adjusted for PAM13-D at T0, CVR score at T0, and treating primary care physician;
PAM13-D scores from 0 (lowest level of patient activation) to 100 (highest level of patient activation)
*3 Secondary endpoint EQ-VAS, adjusted for EQ-VAS at T0, CVR score at T0, and treating primary care physician;
EQ-VAS scores from 0 (worst health) to 100 (best health)
*4 Additional endpoints, adjusted for the respective endpoint at T0 and treating primary care physician
*5 Effect size calculated as the difference of the adjusted means divided by the square root of the residual variance; absolute values of 0.5–0.8 can be interpreted as moderate effects
Table 2b. Changes in health behaviors*1.
|
Reduction in risk factors between T0 and T1*2 |
A group | A+D group | ||
| Valid n | % (n) | Valid n | % (n) | |
| Smoking | 40 | 10.0 (4) | 37 | 10.8 (4) |
| Overweight | 39 | 20.5 (8) | 36 | 16.7 (6) |
| Poor diet | 40 | 32.5 (13) | 38 | 36.8 (14) |
| Lack of exercise | 39 | 25.6 (9) | 37 | 40.5 (15) |
| Stress and hecticness | 40 | 12.5 (5) | 37 | 40.5 (15) |
| Alcohol consumption | 40 | 22.5 (9) | 38 | 13.1 (5) |
| General comment (T1) | N | % | N | % |
| “Overall I now live …“ | ||||
| “…more healthily.“ | 16 | 43.2 | 19 | 55.9 |
| “…just like before [no change].“ | 21 | 56.8 | 14 | 41.2 |
| “…less healthily.“ | 0 | 0 | 1 | 2.9 |
n, number; T0, time point of inclusion in the study (baseline); T1, time point after four months (follow-up)
*1 descriptive analyses according to study protocol (15)
*2 Number of patients in whose estimation their risk factors at T1 were lower than at T0 (for details, see Figure 2)
We tested these results in per protocol analyses and observed only small deviations compared with the ITT analyses (eMethods).
Patient population
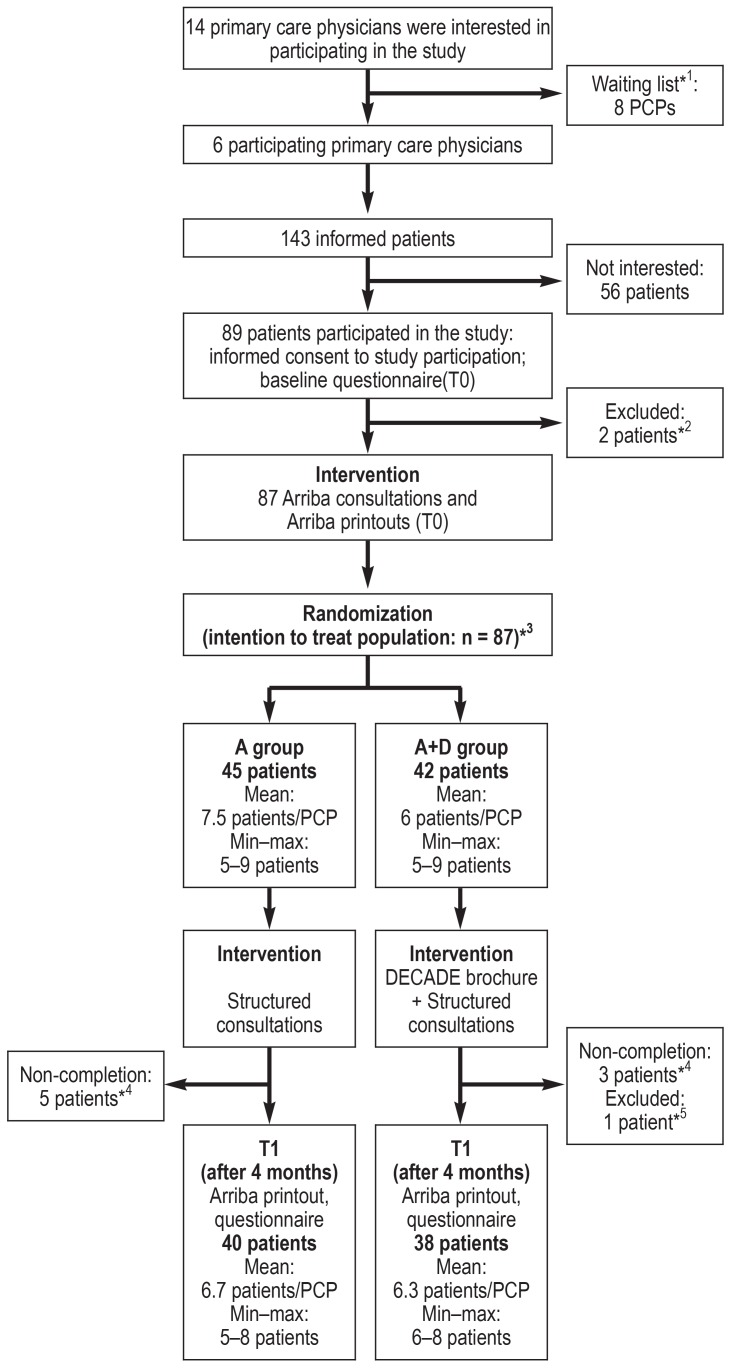
In six primary care practices, 143 adult patients were informed about the study. 87 patients consented to participation, received the Arriba consultation, and were randomized (A group: n = 45; A+D group: n = 42). Eight subjects did not complete the study (dropout rate 9.2%). Deviations from the study protocol (n = 16) were documented and per protocol analyses were conducted for 71 patients. Details on dropouts and per protocol analyses are in the annotations of the flow diagram (Figure 1) and in the eMethods section. One questionnaire was returned to the data management team after the data evaluation had been completed.
Figure 1.
Flow diagram: Inclusion and course of the study
PCP, primary care physician; min, minimum; max, maximum; T0, time point of inclusion into the study (baseline); T1, time point after four months (follow-up)
*1 None of the participating primary care physicians had withdrawn from participation, primary care physicians on the waiting list were therefore not included in the study.
*2 Patients did not participate in the Arriba consultation.
*3 Per protocol population (N = 71; A group = 36; A+D group = 35); 16 patients were excluded because of protocol breaches: In one practice, patients in the A group were given the second part of the DECADE brochures (rather than no brochure), 12 patients were excluded. In two practices each, one married couple was included, 4 patients were excluded.
*4 The reasons for not completing the study, where known (primarily communicated by patients): very low cardiovascular risk (n = 1), no gain from participation (n = 1); shift work and therefore too little time to attend follow-up consultations (n = 1); familial reasons (n = 1); severe illness owing to non-cardiovascular cause (n = 1).
*5 Receipt of the T1 questionnaire after data analysis had been completed.
The patients in the A+D group were a mean of 6 years older than those in the A group. All other characteristics did not differ materially between the study arms (table 3). The mean PAM13-D score of 88 points, measured on a scale of 0 (lowest level of activation) to 100 (highest level of activation), exceeded in both study arms the expected baseline score by about 20 points.
Table 3. Study population.
| Patient characteristics at T0 | A group | A+D group | Total | ||||||
| n = 45 | % | Mean (SD) | n = 42 | % | Mean (SD) | n = 87 | % | Mean (SD) | |
| Age | 45 | 59.3 (10.8) | 42 | 65.1 (13.0) | 87 | 62.1 (12.2) | |||
| Women | 27 | 60.0 | 22 | 52.4 | 46 | 56.3 | |||
| School leaving certificate from secondary school (9 years of education)*1 |
20 | 44.4 | 20 | 47.6 | 44 | 46.0 | |||
| Economically active | 23 | 51.1 | 18 | 42.9 | 41 | 47.1 | |||
| PAM13-D score 0–100*2 | 44 | 88.1 (8.4) | 42 | 88.4 (8.4) | 86 | 88.2 (8.1) | |||
| EQ-VAS score 0–100*3 | 42 | 68.0 (19.6) | 42 | 67.3 (16.6) | 84 | 67.6 (18.1) | |||
| CVR score 0–51 %*4 | 45 | 14.6 (14.8) | 42 | 20.6 (17.1) | 87 | 17.5 (16.1) | |||
| Smoker | 11 | 24.1 | 9 | 21.4 | 20 | 23.0 | |||
| Arteriosclerosis | 5 | 11.1 | 6 | 14.3 | 11 | 12.6 | |||
| Positive family history | 21 | 46.7 | 17 | 40.5 | 38 | 43.7 | |||
| Antihypertensive medication | 26 | 57.8 | 31 | 73.8 | 57 | 65.5 | |||
| Systolic blood pressure (mm Hg) | 45 | 130.9 (16.6) | 42 | 134.7 (17.2) | 87 | 132.7 (16.9) | |||
| Total cholesterol (mg/dL) | 45 | 221.7 (48.6) | 42 | 213.5 (50.3) | 87 | 217.8 (49.3) | |||
| HDL cholesterol (mg/dL) | 45 | 56.4 (16.9) | 42 | 55.5 (16.8) | 87 | 55.9 (16.8) | |||
| Diabetes mellitus | 16 | 35.6 | 14 | 33.3 | 30 | 34.5 | |||
| HbA1c % | 16 | 6.44 (1.26) | 14 | 6.49 (0.65) | 30 | 6.46 (0.97) | |||
CVR score, cardiovascular risk score; EQ-VAS, European quality of life—visual analogue scale (subjective health status); HbA1c. hemoglobin A;
HDL cholesterol, high density lipoprotein cholesterol; n, number; PAM13-D, German version of Patient Activation Measure questionnaire;
SD, standard deviation; T0, time point of inclusion in study (baseline)
*1 Highest school leaving certificate: secondary school (9 years of education); secondary school (10 years of education); higher education entrance qualification (12–13 years of education); university/technical college degree
*2 PAM13-D scores from 0 (lowest level of patient activation) to 100 (highest level of patient activation)
*3 EQ-VAS scores from 0 (worst health) to 100 (best health)
*4 CVR scores from 0% (lowest risk) to 51% (highest calculated risk; manifest arteriosclerosis)
The effect of the DECADE brochures on the primary endpoint patient activation
The patients in the A+D group increased their mean patient activation score (PAM13-D), which had been high at the start of the study, by 1.50 points after four months, whereas the mean PAM13-D score in the A group fell by 1.81 points. The use of the DECADE brochures showed a significant effect of 3.30 points (95%-CI [0.47; 6.14], p = 0.023; effect size 0.54) on patient activation (table 2a).
Secondary endpoints
Health status (EQ-VAS) scored better during the course of the study than at the start of the study: by a mean of 6.84 points in the A+D group and by 1.05 points in the A group. The estimated effect of the DECADE brochures was 5.79 points (95% CI: [-0.63; 12.21], p = 0.076; effect size 0.44) (table 2a).
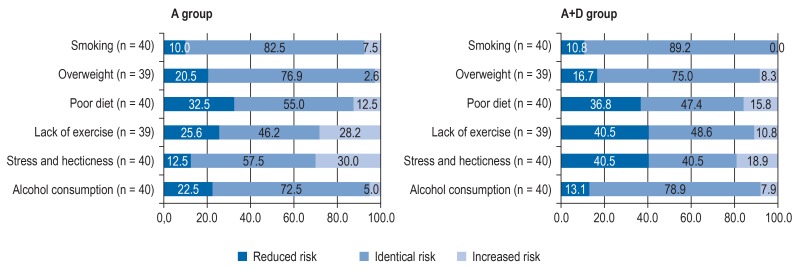
Patients rated their own health behaviors regarding smoking, weight, diet, exercise, stress, and alcohol as low risk or moderate risk. At the start of the study, the mean risk factor scores in the A group were 1.5 (standard deviation SD = 0.8) points, and in the A+D group, 1.1 (SD = 0.6) points. The changes in risk factor scores were altogether small, but in the A+D group 40.5% of patients each improved their risk behaviors relating to lack of exercise and stress/hecticness. In the A group, this was the case for 25.6% and 12.5%, respectively (figure 2).
Figure 2.
Categorical changes of risk factors (RF) after four months in both study arms in percent
Change of risk evaluation T1 (time point after four months, follow-up) versus T0 (time point of study inclusion, baseline)
– Reduced risk: risk evaluation at T1 is lower than at T0
– Identical risk: risk evaluation at T1 is the same as at T0
– Increased risk: risk evaluation at T1 is greater than at T0
The question relating to general modifications in health behaviors since the start of the study was answered by 34 patients in the A+D group and 37 patients in the A group. 55.9% (n = 19) in the A+D group and 43.2% (n = 16) in the A group agreed with the statement that they now “lived altogether more healthily”. One patient (A+D group) communicated that at the end of the study, he “lived altogether less healthily”. The mean sums of goals attained were 20.8 points in the A+D group (SD = 10.1) and 19.3 points (SD = 11.1) in the A group. Subjects in the A+D group were on average slightly more satisfied with attaining their goals (14.2, SD = 5.9) than in the A group (13.1, SD = 7.2). The patients in the A+D group scored the usefulness of the information materials (USE) as 65.0 points (SD = 17.3) on a scale of 0–90; this was slightly higher than among participants in the A group (62.4, SD = 18.9). The mean values for the subscales on cognition, emotions, and behaviors in both study arms were between 19.2 points and 22.8 points.
The patients in the A+D group scored the consultations with their primary care physicians on a scale of 1 (very satisfied) to 4 (very dissatisfied) similar to the patients in the A group, with mean scores of 1.36 (SD = 0.4) and 1.47 (SD = 0.8), respectively.
Additional endpoints
Table 2a shows changes in clinical parameters and body mass index (BMI) at T1 versus T0. The estimated effects of the DECADE brochures on these parameters were small. In altogether 30 patients with diabetes mellitus, the number of hemoglobin measurements (HbA1C) collected was too small to be analyzed. We conducted exploratory analyses independently of the study arm and detected inverse correlations between the PAM13-D score at T0 and health behaviors relating to an unhealthy diet, lack of exercise, stress and hecticness, as well as alcohol consumption. Relevant correlations between PAM13-D scores and patients’ sociodemographic characteristics, clinical parameters, or health status (EQ-VAS) did not exist (eMethods, eTable 1). An increase in PAM13-D scores between T0 and T1 was correlated with a reduction in risk factors and total cholesterol concentrations (eMethods, eTable 2).
eTable 1. Associations between PAM13-D and patient characteristics at T0.
| Patient characteristics at T0 | PAM13-D T0 | |
| Correlation coefficient*1 | n | |
| Age | 0.165 | 86 |
| EQ-VAS*2 | 0.110 | 83 |
| CVR score*3 | 0.104 | 86 |
| Risk factors (RF)*4 | ||
| RF total mean value | −0.272 | 86 |
| Smoking | 0.010 | 86 |
| Overweight | −0.014 | 83 |
| Poor diet | −0.278 | 84 |
| Lack of exercise | −0.303 | 83 |
| Stress and hecticness | −0.256 | 85 |
| Alcohol consumption | −0.316 | 85 |
CVR score, cardiovascular risk score; EQ-VAS, European quality of life—visual analogue scale (subjective health);
n, number; PAM13-D, German version of Patient Activation Measure questionnaire with scores from 0 (lowest level of patient activation) to 100 (highest level of patient activation);
T0, time point of study inclusion (baseline);
T1, time point after four months (follow-up)
*1 Correlation coefficient Spearman‘s rho
*2 EQ-VAS scores from 0 (worst health) to 100 (best health)
*3 CVR scores from 0 % (lowest risk) to 51 % (highest calculated risk; manifest arteriosclerosis)
*4 Risk factors (RF) with scores from 0 (not at all) to 4 (strong)
eTable 2. Associations between changes in patient activation (PAM13-D) and patient characteristics, changes in health behaviors and clinical parameters.
| Patient characteristics T1 vs. T0 | PAM13-D T1 vs. T0 | |
| Correlation coefficient*1 | n | |
| Risk factors (RF) T1 vs. T0*2 | ||
| RF total mean value T1 vs. T0 | −0.329 | 77 |
| Smoking T1 vs. T0 | 0.079 | 76 |
| Overweight T1 vs. T0 | 0.056 | 74 |
| Poor diet T1 vs. T0 | −0,418 | 77 |
| Lack of exercise T1 vs. T0 | −0.254 | 75 |
| Stress and hecticness T1 vs. T0 | −0.198 | 76 |
| Alcohol consumption T1 vs. T0 | −0.102 | 77 |
| Changes in health behaviors T1*3 | 0.171 | 70 |
| EQ-VAS T1 vs. T0*4 | 0.087 | 72 |
| Body mass index T1 vs. T0 | −0.110 | 71 |
| Clinical parameters T1 vs. T0 | ||
| Systolic blood pressure T1 vs. T0 | −0.086 | 76 |
| Total cholesterol T1 vs. T0 | −0.298 | 76 |
| HDL cholesterol T1 vs. T0 | −0.075 | 76 |
| CVR score T1 vs. T0*5 | −0.090 | 76 |
CVR score, cardiovascular risk score, EQ-VAS, European quality of life—visual analogue scale (subjective health); HDL cholesterol, high density lipoprotein cholesterol;
n, number; PAM13-D, German version of Patient Activation Measure questionnaire with scores from 0 (lowest level of patient activation) to 100 (highest level of patient activation);
T0, time point of study inclusion (baseline); T1, time point after four months (follow-up)
*1 Correlation coefficient Spearman‘s rho
*2 Risk factors with scores from 0 (not at all) to 4 (strong)
*3 Change in health behaviors: score of 1 (less healthy), 2 (unchanged), 3 (healthier)
*4 EQ-VAS scores from 0 (worst health) to 100 (best health)
*5 CVR scores from 0 % (lowest risk) to 51 % (highest calculated risk; manifest ?arteriosclerosis)
Qualitative responses from patients and primary care physicians
We report our qualitative results only briefly here as they will be published in greater detail elsewhere. 34 patients in the A+D group answered most of the free-text questions on the evaluation of the DECADE brochures.
The overwhelming majority of these rated the clear presentation, the content of the information and its comprehensibility, as well as the design of the DECADE brochures as positive and reported that the brochures motivated them to keep an eye on their own health behaviors in the long term. 25 patients were altogether (very) satisfied with the DECADE brochures and four patients partly satisfied. One patient was dissatisfied.
Doctors’ opinions on the brochures were more divergent and were, among others, shaped by their own expectations of their patients’ willingness to modify their behaviors and adherent processing of the materials. They were under the impression that the uptake and processing of information, as well as the willingness to engage in self-management, depended more on the individual patient and less on the materials made available. Overall, primary care physicians rated the structured follow-up consultations as positive.
Discussion
The positive course of the study and patients’ positive ratings of the consultations and the DECADE brochures showed that the intervention DECADE is feasible in general practice. The use of the DECADE brochures, in addition to structured follow-up consultations, had an amplifying effect on patient activation (PAM13-D + 3.3 points, 95% CI: [0.47; 6.14], p = 0.023).
Several studies showed that high PAM13-D scores were associated with positive health behaviors and willingness to modify behaviors (7, 8, 26, 27). A study including 4865 patients with chronic disorders showed a gain in patient activation of 2.8 points on the PAM13-D scale. This was regarded as a remarkable score since improved health behaviors can be expected (7). The exploratory analyses of the DECADE pilot study partly support this finding. In the entire sample (independently of the study arm), an association was observed between increased PAM13-D scores and a reduction in risk factors and cholesterol concentrations.
Results from individual studies give rise to the assumption that changes in patient activation are associated with the duration and intensity of individually tailored patient care. Merely making available information materials did not increase patient activation in a study reported by Boyle et al. (28). By contrast, Hibbard et al. showed in a study of 357 patients with chronic disorders that tailoring their care increased PAM13-D scores after two to three months by +2.5 points versus 1.8 points compared with usual care. After a further three months, the scores rose by +4.6 points versus +2.6 points (29). Further studies have shown similar results (26, 30).
A higher proportion of patients in the A+D group said that at the end of the study they were “living generally more healthily” (55.9% versus 43.2%) and rated their health status (EQ-VAS) after four months tendentially as better than those in the A group (+6.84 points versus +1.05 points). Further secondary endpoints such as goal attainment (adapted goal attainment scale) and satisfaction with this, the usefulness of patient information materials (USE), and satisfaction with the consultations scored slightly better in the A+D group than in the A group. The clinical parameters of the two groups differed to a negligible degree.
Limitations
Because of the pilot character of this study, the sample size was small (n = 87). Six primary care practices participated, which meant that we were able to realize a two-arm study only, so that the intervention was not compared with routine care. It was not possible to blind the study nor the scientists involved (eMethods). Some questionnaire instruments were newly developed for this study, or existing ones were adapted. Their validity is therefore limited.
Our findings on patient activation (primary endpoint) were based on patients’ self-reported information, and scores were higher at the start of the study (mean value 88.2) than in other studies (means between 61.2 and 67.2 points) (31). Since patients were consecutively included (study protocol [15]), it is fair to assume that our subjects differed from the patients of other doctors. One reason for this might be that only primary care physicians from teaching practices with a great interest in the topic of cardiovascular diseases participated in the study. It is possible that patients in such practices are better informed about the relevance of adequate health behaviors than is usually the case. If this is indeed so, the additional rise in the PAM13-D scores in the A+D group should be interpreted even more positively.
As in all surveys, it can be assumed in this study that social desirability has an influence on the self-reported information, as do expectations associated with the study. Even though we cannot report the qualitative results of the study in detail here, we can say in sum that patients in the A+D group rated the DECADE brochures as mostly very positive in their free-text responses. By comparison, the primary care physicians responded in a clearly more differentiated fashion in the interviews. The structure follow-up consultations were rated positively by both primary care physicians and patients.
Conclusion
The DECADE pilot study was conducted successfully. It showed that structured consultations in the primary and secondary prevention of cardiovascular diseases were rated positively by primary care physicians and patients, and that the DECADE brochures increased patient activation. Relevant effects on clinical parameters were not seen, however. These results should now be tested in a study with a longer intervention period in different regions of Germany and in comparison with usual care. If successful it would make sense to implement DECADE in routine healthcare service provision. Until that is the case, primary care physicians should determine cardiovascular risk in at-risk patients, discuss evidence-based treatment options, and show a sustained interest in their patients’ health behaviors.
Supplementary Material
eMethods
Study design
The study objectives were tested by using qualitative and quantitative methods. In this article, we report primarily the quantitative results of the two-arm, randomized controlled pilot study. The qualitative results were mentioned only in passing. Details on the qualitative methods are described in the study protocol (15).
The study was conducted in Germany’s South Baden region between July 2016 and March 2017. We included adult male and female patients with at least one of the following risk factors for cardiovascular disease:
Exclusion criteria included pregnancy, alcohol or drug addiction, severe eating disorders, relevant cognitive impairments or mental disorders, severe illness or short life expectancy, current or planned rehabilitation measure, as well as insufficient knowledge of written and spoken German. If patients were living in the same household, only one of the interested parties was allowed to participate, so as to avoid contamination of the study arms.
The practices were instructed to include patients in a structured and consecutive manner. Details are described in the study protocol (15).
In both study arms, four structured consultations were mandatory (table 1). At the start of the study, all patients received cardiovascular risk advice/counseling by using the software program Arriba. This calculates a 10 year risk for a cardiovascular event (0 to >50%) as well as the possible absolute risk reduction associated with different treatment options. The patients received an individually tailored Arriba printout generated by the program.
In order to avoid selection bias, the randomization was done after the patients’ CVR calculation. Physicians opened pre-prepared sealed randomization envelopes that allocated each patient to one of the two study arms. The randomization envelopes were prepared by the study center at the Medical Center—University of Freiburg. The 1:1 randomization was stratified by treating primary care physician (block randomization). The patients in the A+D group received the DECADE brochures in addition to the Arriba printouts; the patients in the A group received the Arriba printouts, but no additional materials.
It was not possible to blind the study and participating scientists, for the following reasons:
Data collection and endpoints
Quantitative data were collected at the time of inclusion into the study (baseline T0) and after four months (follow-up T1). The measurement instruments are described in detail in the study protocol (15).
The primary endpoint was the change in patient activation (Patient Activation Measure, PAM13-D) between T0 and T1. PAM13-D measures patients’ activity with regard to self-management. 13 items on a scale ranging from 1 (does not apply/not true) to 4 (applies exactly/completely true) were used to assess knowledge, skills and confidence to manage one’s own health (20). We calculated the transformed sum value with values of 0 (low level of activation) to 100 (high level of activation).
Secondary endpoints
Additional endpoints
Additional endpoints were changes in the CVR score, systolic blood pressure, total and high density lipoprotein (HDL) cholesterol, hemoglobin A (HbA1c), and body mass index (BMI) between T0 and T1.
The primary care practices used Arriba to calculate the CVR score. For the study we used Arriba printouts and the following data: age, sex, the dichotomous data smoking, family history, prescribed antihypertensive medications, manifest arteriosclerosis, and diabetes mellitus; the metric data systolic blood pressure, total and HDL cholesterol, HbA1c in diabetes mellitus, and CVR score.
BMI was calculated on the basis of patient-reported height and weight.
Attendance at the follow-up appointments and ratings of the DECADE brochures and the intensity of their use were documented in interviews with primary care physicians and in open patient questions, and qualitatively evaluated.
Data analyses
The statistical quantitative analyses were done according to the intention-to-treat principle, as predefined in the study protocol. The population to be analyzed consisted of all randomized patients. Missing data were not imputed. The only exception to this rule was the instrument used to score the usefulness of patient information materials (USE), whose manual stipulates data imputation in certain circumstances (25). The patients were analyzed according to the randomized intervention (intention-to-treat population). Sensitivity analyses were performed in the per-protocol-population. The analysis of the potential effect of the intervention on the primary endpoint difference in patient activation (PAM13-D) T1 versus T0 was undertaken by using a linear regression model. In addition to the intervention, the model included the treating primary care physician, the CVR score (T0), and the PAM13-D score (T0) as covariates for adjustment. The potential effects of the DECADE brochures on the secondary endpoint variables were investigated in analog regression models; the covariates treating primary care physician, CVR score (T0) and EQ-VAS (T0) were adjusted for in the analysis of the current health status (EQ-VAS). For the additional endpoints CVR score, systolic blood pressure, total and HDL cholesterol, and BMI T1 versus T0, the covariates treating primary care physician and the respective value of the endpoint at T0 were included in the model. Adjusted means were calculated from the models. All other endpoints were analyzed descriptively. Details are described in the study protocol (15).
Exploratory, non–pre-specified analyses were used to investigate bivariate associations of the PAM13-D scores and changes in PAM13-D scores over the course of the study, with sociodemographic data and health behaviors.
We used SAS version 9.3 and SPSS version 24 for our quantitative data analyses.
We used MAXQDA version 11 to analyze qualitative data from the interviews with the primary care physicians and the free-text patients’ comments were evaluated by qualitative content analysis. The study protocol includes details on the qualitative method (15).
Results of the per protocol analyses
From the primary care physicians’ interviews it transpired that in one practice, patients in the A group (control group) wrongly received the second part of the DECADE brochures at the start of the study. This practice with n = 12 patients was therefore excluded from the per protocol (PP) analyses. Two practices erroneously included a married couple each. The relevant patients (n = 4) were excluded. The PP analysis population included 71 patients (A+D group: n = 35; A group = 36).
The results of the PP population are in the main consistent with those of the ITT population. The following slight differences were: the tendentially positive effect of the DECADE brochures on health status (EQ-VAS) seen in the ITT analysis increased in the PP analysis (8.90, 95% confidence interval: [1.47; 16.33], p = 0.02). The difference between the two study arms in terms of the question about a general modification in health behaviors was more clearly expressed in the PP analysis than in the ITT analysis: at the end of the study, 60% of patients in the A+D group (n = 18) reported that they lived “more healthily now than before”, whereas the proportion in the A group was 37.9% (n = 11).
Arterial hypertension
Hypercholesterolemia
Diabetes mellitus
Arteriosclerosis
Smoking
Overweight
High levels of stress
Prescribed medication for hypertension
High cholesterol level.
The doctors used the DECADE brochures together with their patients.
The questionnaires at T1 differed between the A group and the A+D group. The participating scientists knew the datasets.
The patients in the control group were informed in the study materials that they would be given the DECADE brochures after the conclusion of the study.
Change in health status on a visual analogue scale (EQ-VAS, European quality of life—visual analogue scale) between T0 and T1. The patients scored their current health status on a scale ranging from 0 (worst health) to 100 (best health) (23).
Changes in risk factors between T0 and T1: the patients evaluated the risk factors smoking, lack of exercise, overweight, poor diet, hecticness and stress on a five-point scale ranging from 0 (not at all) to 4 (strong) (22).
Change in health behaviors: the patients were able to select from three statements: “I now live generally more healthily”, “I live no differently to before”, or “I live generally less healthily” (21).
Attainment of own behavioral goals: to this end, the goal attainment scale (GAS) (24) was adapted to the setting of the DECADE pilot study. The adapted GAS included 13 possible behavioral goals that patients scored on a scale ranging from 0 (not at all achieved) to 5 (more than achieved). The sum value was calculated (0–65).
Satisfaction with having reached one’s individual goal (development). This was scored by using a scale ranging from 0 (very dissatisfied) to 3 (very satisfied). The sum value was calculated (0–39).
The usefulness of the patient information materials was scored using 9 items on the usefulness scale for patient information material (USE), ranging from 0 (don’t agree at all) to 10 (fully agree). The sum value was calculated (0–90), as were the subscales for cognition, emotions, and behaviors (0–30, each) (25).
The satisfaction with cardiovascular risk consultations (own questionnaire development) was scored using 6 items in a scale ranging from 1 (very satisfied) to 4 (very dissatisfied).
Key Messages.
It was possible to implement cardiovascular risk counseling with structured follow-up consultations in primary care.
Primary care physicians and patients expressed satisfaction.
Additionally, making the DECADE brochures available increased, even if they were used to differing degrees of intensity, patient activation and generally had a beneficial effect on health behaviors.
Clinical parameters had not changed to a relevant degree after four months.
The results of this pilot study should be tested in a larger study with a longer follow-up period and in comparison with current routine care.
Primary care physicians should support their patients in the sense of shared decision making to put evidence-based treatment options for lowering their cardiovascular risk into practice and should use appropriate patient information materials in support.
Acknowledgments
Translated from the original German by Birte Twisselmann, PhD.
Acknowledgments
We thank all patients and practice teams that participated in the DECADE pilot study. We thank Britta Seifer and Inna Shara for their administrative support and data entry.
Registration
The study received ethics approval from the ethics committee at the Albert Ludwig University Freiburg and was registered with the German Clinical Trials Register (DRKS) on 7 July 2016: DRKS00010584.
Footnotes
Conflict of interest statement
Dr. Maun is a board member of the Arriba cooperative and holds shares in the cooperative, which supports the maintenance and further development of the software used in the study.
The other authors declare that they have not received any support from commercial organizations relating to this study or intervention. They also declare that no other conflict of interest exists.
References
- 1.World Health Organisation (WHO) Cardiovascular diseases. www.euro.who.int/en/health-topics/noncommunicable-diseases/cardiovascular-diseases (last accessed on 16 May 2018) [Google Scholar]
- 2.Federal health reporting. Most frequent diagnoses in percent of all cases of treatment in medical practices in the region North Rhine (2015) www.gbe-bund.de/oowa921-install/servlet/oowa/aw92/dboowasys921xwdevkit/xwd_init?gbe.isgbetol/xs_start_neu/&p_aid=i&p_aid=15988 906&nummer=638&p_sprache= D&p_indsp=-&p_aid=19947716 (last accessed on 8 May 2017) [Google Scholar]
- 3.Ludt S, Angelow A, Baum E, et al. Hausärztliche Risikoberatung zur kardiovaskulären Prävention S3-Leitlinie. Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin (DEGAM) 2017. www.degam.de/degam-leitlinien-379.html (last accessed on 21 December 2017) [Google Scholar]
- 4.Kelly MP, Barker M. Why is changing health-related behaviour so difficult? Public Health. 2016;136:109–116. doi: 10.1016/j.puhe.2016.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schmitz R, Jordan S, Muters S, Neuhauser H. Population-wide use of behavioural prevention and counselling programmes for lifestyle-related cardiovascular risk factors in Germany. Eur J Prev Cardiol. 2012;19:849–856. doi: 10.1177/1741826711410949. [DOI] [PubMed] [Google Scholar]
- 6.Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res. 2005;40:1918–1930. doi: 10.1111/j.1475-6773.2005.00438.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hibbard JH, Greene J, Shi Y, Mittler J, Scanlon D. Taking the long view: how well do patient activation scores predict outcomes four years later? Med Care Res Rev. 2015;72:324–337. doi: 10.1177/1077558715573871. [DOI] [PubMed] [Google Scholar]
- 8.Sacks RM, Greene J, Hibbard J, Overton V, Parrotta CD. Does patient activation predict the course of type 2 diabetes? A longitudinal study. Patient Educ Couns. 2017 100:1268–1275. doi: 10.1016/j.pec.2017.01.014. [DOI] [PubMed] [Google Scholar]
- 9.Neuner-Jehle S, Schmid M, Gruninger U. [Short time counseling in medical practice for improving health behaviour: problems and solutions] Praxis. 2014;103:271–277. doi: 10.1024/1661-8157/a001572. [DOI] [PubMed] [Google Scholar]
- 10.Geense WW, van de Glind IM, Visscher TL, van Achterberg T. Barriers, facilitators and attitudes influencing health promotion activities in general practice: an explorative pilot study. BMC Fam Pract. 2013:14–20. doi: 10.1186/1471-2296-14-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.von Poellnitz PB. [Implementation of shared decision making in general practice: experiences of doctors during in a study with hypertensive patients]. Freiburg in Breisgau. Medical dissertation. Medical Center - University of Freiburg, Faculty of Medicine 2014. freidok.uni-freiburg.de/data/9695 (last accessed on 21 December 2017) [Google Scholar]
- 12.Lager KE, Mistri AK, Khunti K, Haunton VJ, Sett AK, Wilson AD. Interventions for improving modifiable risk factor control in the secondary prevention of stroke. Cochrane Database Syst Rev. 2014 doi: 10.1002/14651858.CD009103.pub2. CD009103. [DOI] [PubMed] [Google Scholar]
- 13.Fleig L, Pomp S, Schwarzer R, Lippke S. Promoting exercise maintenance: how interventions with booster sessions improve long-term rehabilitation outcomes. Rehabil Psychol. 2013;58:323–333. doi: 10.1037/a0033885. [DOI] [PubMed] [Google Scholar]
- 14.Pimouguet C, Le Goff M, Thiebaut R, Dartigues JF, Helmer C. Effectiveness of disease-management programs for improving diabetes care: a meta-analysis. CMAJ. 2011;183:E115–E127. doi: 10.1503/cmaj.091786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tinsel I, Siegel A, Schmoor C, Buchholz A, Niebling W. DECADE-pilot: decision aid, action planning, and follow-up support for patients to reduce the 10-year risk of cardiovascular diseases-a protocol of a randomized controlled pilot trial. Pilot Feasibility Stud. 2017;3 doi: 10.1186/s40814-017-0172-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Elwyn G, Frosch D, Thomson R, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27:1361–1367. doi: 10.1007/s11606-012-2077-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stacey D, Légaré F, Lewis K, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017 doi: 10.1002/14651858.CD001431.pub5. CD001431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schwarzer R. Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Applied Psychology. 2008;57:1–29. [Google Scholar]
- 19.Krones T, Keller H, Sonnichsen A, et al. Absolute cardiovascular disease risk and shared decision making in primary care: a randomized controlled trial. Ann Fam Med. 2008;6:218–227. doi: 10.1370/afm.854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brenk-Franz K, Hibbard JH, Herrmann WJ, et al. Validation of the German version of the patient activation measure 13 (PAM13-D) in an international multicentre study of primary care patients. PLoS One. 2013;8 doi: 10.1371/journal.pone.0074786. e74786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Siegel A, Stößel U, Zerpies E. GEKIM- Gesundes Kinzigtal Mitgliederbefragung 2012/2013. Medizinische Psychologie und Medizinische Soziologie, Albert-Ludwigs-Universität Freiburg. 2013;94 [Google Scholar]
- 22.Frey C, Bührlen B, Gerdes N, Jäckel W. Handbuch zum IRES-3 Indikatoren des Reha-Status, Version 3 mit IRES-24 (Kurzversion) Regensburg: Roderer. 2007 [Google Scholar]
- 23.Oemar M, Oppe M. EQ-5D-3L User guide Basic information on how to use the EQ-5D-3L instrument. www.euroqol.org/wp-content/uploads/2016/09/EQ-5D-5L_UserGuide_2015.pdf(last accessed on 21 December 2017) [Google Scholar]
- 24.Schaefer I, Kolip P. Leitfaden Goal Attainment Scaling (Zielerreichungsskalen) Universität Bilefeld 2015. www.uni-bielefeld.de/gesundhw/ag4/GAS_Leitfaden.pdf (last accessed on 21 March 2018) [Google Scholar]
- 25.Hölzel LP, Ries Z, Dirmaier J, et al. Usefulness scale for patient information material (USE)—development and psychometric properties. BMC Med Inform Decis Mak. 2015;15 doi: 10.1186/s12911-015-0153-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fowles JB, Terry P, Xi M, Hibbard J, Bloom CT, Harvey L. Measuring self-management of patients‘ and employees‘ health: further validation of the patient activation measure (PAM) based on its relation to employee characteristics. Patient Educ Couns. 2009;77:116–122. doi: 10.1016/j.pec.2009.02.018. [DOI] [PubMed] [Google Scholar]
- 27.Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Aff. 2013;32:207–214. doi: 10.1377/hlthaff.2012.1061. [DOI] [PubMed] [Google Scholar]
- 28.Boyle F, Mutch A, Dean J, Dick M, Del Mar C. The contribution of consumer health organisations to chronic disease self management in the context of primary care. Canberra: Australian Primary Health Care Research Institute. www.researchgate.net/publication/46422100_The_Contribution_of_Consumer_Health_Organisations_to_Chronic_Disease_Self_Management_in_the_Context_of_Primary_Care (last accessed on 21 December 2017) 2009 [Google Scholar]
- 29.Hibbard JH, Greene J, Tusler M. Improving the outcomes of disease management by tailoring care to the patient‘s level of activation. Am J Manag Care. 2009;15:353–360. [PubMed] [Google Scholar]
- 30.Hibbard JH, Mahoney ER, Stock R, Tusler M. Do increases in patient activation result in improved self-management behaviors? Health Serv Res. 2007;42:1443–1463. doi: 10.1111/j.1475-6773.2006.00669.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rademakers J, Maindal HT, Steinsbekk A, Gensichen J, Brenk-Franz K, Hendriks M. Patient activation in Europe: an international comparison of psychometric properties and patients‘ scores on the short form Patient Activation Measure (PAM-13) BMC Health Serv Res. 2016;16 doi: 10.1186/s12913-016-1828-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods
Study design
The study objectives were tested by using qualitative and quantitative methods. In this article, we report primarily the quantitative results of the two-arm, randomized controlled pilot study. The qualitative results were mentioned only in passing. Details on the qualitative methods are described in the study protocol (15).
The study was conducted in Germany’s South Baden region between July 2016 and March 2017. We included adult male and female patients with at least one of the following risk factors for cardiovascular disease:
Exclusion criteria included pregnancy, alcohol or drug addiction, severe eating disorders, relevant cognitive impairments or mental disorders, severe illness or short life expectancy, current or planned rehabilitation measure, as well as insufficient knowledge of written and spoken German. If patients were living in the same household, only one of the interested parties was allowed to participate, so as to avoid contamination of the study arms.
The practices were instructed to include patients in a structured and consecutive manner. Details are described in the study protocol (15).
In both study arms, four structured consultations were mandatory (table 1). At the start of the study, all patients received cardiovascular risk advice/counseling by using the software program Arriba. This calculates a 10 year risk for a cardiovascular event (0 to >50%) as well as the possible absolute risk reduction associated with different treatment options. The patients received an individually tailored Arriba printout generated by the program.
In order to avoid selection bias, the randomization was done after the patients’ CVR calculation. Physicians opened pre-prepared sealed randomization envelopes that allocated each patient to one of the two study arms. The randomization envelopes were prepared by the study center at the Medical Center—University of Freiburg. The 1:1 randomization was stratified by treating primary care physician (block randomization). The patients in the A+D group received the DECADE brochures in addition to the Arriba printouts; the patients in the A group received the Arriba printouts, but no additional materials.
It was not possible to blind the study and participating scientists, for the following reasons:
Data collection and endpoints
Quantitative data were collected at the time of inclusion into the study (baseline T0) and after four months (follow-up T1). The measurement instruments are described in detail in the study protocol (15).
The primary endpoint was the change in patient activation (Patient Activation Measure, PAM13-D) between T0 and T1. PAM13-D measures patients’ activity with regard to self-management. 13 items on a scale ranging from 1 (does not apply/not true) to 4 (applies exactly/completely true) were used to assess knowledge, skills and confidence to manage one’s own health (20). We calculated the transformed sum value with values of 0 (low level of activation) to 100 (high level of activation).
Secondary endpoints
Additional endpoints
Additional endpoints were changes in the CVR score, systolic blood pressure, total and high density lipoprotein (HDL) cholesterol, hemoglobin A (HbA1c), and body mass index (BMI) between T0 and T1.
The primary care practices used Arriba to calculate the CVR score. For the study we used Arriba printouts and the following data: age, sex, the dichotomous data smoking, family history, prescribed antihypertensive medications, manifest arteriosclerosis, and diabetes mellitus; the metric data systolic blood pressure, total and HDL cholesterol, HbA1c in diabetes mellitus, and CVR score.
BMI was calculated on the basis of patient-reported height and weight.
Attendance at the follow-up appointments and ratings of the DECADE brochures and the intensity of their use were documented in interviews with primary care physicians and in open patient questions, and qualitatively evaluated.
Data analyses
The statistical quantitative analyses were done according to the intention-to-treat principle, as predefined in the study protocol. The population to be analyzed consisted of all randomized patients. Missing data were not imputed. The only exception to this rule was the instrument used to score the usefulness of patient information materials (USE), whose manual stipulates data imputation in certain circumstances (25). The patients were analyzed according to the randomized intervention (intention-to-treat population). Sensitivity analyses were performed in the per-protocol-population. The analysis of the potential effect of the intervention on the primary endpoint difference in patient activation (PAM13-D) T1 versus T0 was undertaken by using a linear regression model. In addition to the intervention, the model included the treating primary care physician, the CVR score (T0), and the PAM13-D score (T0) as covariates for adjustment. The potential effects of the DECADE brochures on the secondary endpoint variables were investigated in analog regression models; the covariates treating primary care physician, CVR score (T0) and EQ-VAS (T0) were adjusted for in the analysis of the current health status (EQ-VAS). For the additional endpoints CVR score, systolic blood pressure, total and HDL cholesterol, and BMI T1 versus T0, the covariates treating primary care physician and the respective value of the endpoint at T0 were included in the model. Adjusted means were calculated from the models. All other endpoints were analyzed descriptively. Details are described in the study protocol (15).
Exploratory, non–pre-specified analyses were used to investigate bivariate associations of the PAM13-D scores and changes in PAM13-D scores over the course of the study, with sociodemographic data and health behaviors.
We used SAS version 9.3 and SPSS version 24 for our quantitative data analyses.
We used MAXQDA version 11 to analyze qualitative data from the interviews with the primary care physicians and the free-text patients’ comments were evaluated by qualitative content analysis. The study protocol includes details on the qualitative method (15).
Results of the per protocol analyses
From the primary care physicians’ interviews it transpired that in one practice, patients in the A group (control group) wrongly received the second part of the DECADE brochures at the start of the study. This practice with n = 12 patients was therefore excluded from the per protocol (PP) analyses. Two practices erroneously included a married couple each. The relevant patients (n = 4) were excluded. The PP analysis population included 71 patients (A+D group: n = 35; A group = 36).
The results of the PP population are in the main consistent with those of the ITT population. The following slight differences were: the tendentially positive effect of the DECADE brochures on health status (EQ-VAS) seen in the ITT analysis increased in the PP analysis (8.90, 95% confidence interval: [1.47; 16.33], p = 0.02). The difference between the two study arms in terms of the question about a general modification in health behaviors was more clearly expressed in the PP analysis than in the ITT analysis: at the end of the study, 60% of patients in the A+D group (n = 18) reported that they lived “more healthily now than before”, whereas the proportion in the A group was 37.9% (n = 11).
Arterial hypertension
Hypercholesterolemia
Diabetes mellitus
Arteriosclerosis
Smoking
Overweight
High levels of stress
Prescribed medication for hypertension
High cholesterol level.
The doctors used the DECADE brochures together with their patients.
The questionnaires at T1 differed between the A group and the A+D group. The participating scientists knew the datasets.
The patients in the control group were informed in the study materials that they would be given the DECADE brochures after the conclusion of the study.
Change in health status on a visual analogue scale (EQ-VAS, European quality of life—visual analogue scale) between T0 and T1. The patients scored their current health status on a scale ranging from 0 (worst health) to 100 (best health) (23).
Changes in risk factors between T0 and T1: the patients evaluated the risk factors smoking, lack of exercise, overweight, poor diet, hecticness and stress on a five-point scale ranging from 0 (not at all) to 4 (strong) (22).
Change in health behaviors: the patients were able to select from three statements: “I now live generally more healthily”, “I live no differently to before”, or “I live generally less healthily” (21).
Attainment of own behavioral goals: to this end, the goal attainment scale (GAS) (24) was adapted to the setting of the DECADE pilot study. The adapted GAS included 13 possible behavioral goals that patients scored on a scale ranging from 0 (not at all achieved) to 5 (more than achieved). The sum value was calculated (0–65).
Satisfaction with having reached one’s individual goal (development). This was scored by using a scale ranging from 0 (very dissatisfied) to 3 (very satisfied). The sum value was calculated (0–39).
The usefulness of the patient information materials was scored using 9 items on the usefulness scale for patient information material (USE), ranging from 0 (don’t agree at all) to 10 (fully agree). The sum value was calculated (0–90), as were the subscales for cognition, emotions, and behaviors (0–30, each) (25).
The satisfaction with cardiovascular risk consultations (own questionnaire development) was scored using 6 items in a scale ranging from 1 (very satisfied) to 4 (very dissatisfied).