Abstract
Introduction
Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) is an inflammatory central nervous system (CNS) disorder with particular involvement of the pons. Diagnostic criteria include a range of clinical symptoms related to the underlying brainstem pathology, visible with magnetic resonance imaging (MRI). MRI findings include the appearance of punctuate and curvilinear gadolinium enhancement ‘peppering’ the pons. We discuss a patient presenting with clinical and radiographic characteristics of CLIPPERS who was diagnosed with Erdheim–Chester disease (ECD).
Case report
A 52-year-old male presented with 2 years of progressive spasticity, dysarthria, and gait instability. Initially, he was diagnosed with Parkinson’s disease at an outside hospital, based on tremor, rigidity, and gait instability; however, he failed to improve with a trial of levodopa. Brain MRI showed small enhancing parenchymal nodules coalescing in the central pons, but also affecting the cerebellum and cerebellar peduncles, with more punctate enhancing lesions in the cerebral lobar subcortical white matter. When the patient’s response to steroids was inadequate, further imaging was done, revealing perinephric processes. Subsequent biopsy revealed ECD.
Conclusions
A review of the literature for cases of CLIPPERS demonstrated a subset of patients later found to have various malignancies involving the CNS. This case report uses the patient’s unique radiographic and clinical presentation to demonstrate the importance of the exclusion criteria within the CLIPPERS diagnostic requirements and stresses red flags suggestive of alternative diagnoses. This distinction is of high importance when differentiating a relatively benign process such as CLIPPERS from more malignant diseases.
Keywords: Erdheim–Chester disease, CLIPPERS, central nervous system imaging
Introduction
Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) is an inflammatory central nervous system (CNS) disorder with particular involvement of the pons. This disorder was first described in 2010 by Pittock and colleagues as a distinct pontine-predominant encephalomyelitis with striking imaging features. At the time, all patients in their series had clinical symptoms relating to brainstem involvement, including gait ataxia and diplopia. Diagnosis is made by the presence of a range of clinical symptoms related to brainstem pathology along with magnetic resonance imaging (MRI) appearance of punctate and curvilinear gadolinium enhancement ‘peppering’ the pons. Brain biopsy may confirm the diagnosis when pathology is consistent with T-lymphocytic infiltration with perivascular predominance.1,2
In the initial description of CLIPPERS, all patients had subacute gait ataxia and diplopia. A total of seven of eight developed dysarthria, and most described an altered sensation or tingling of the face. Other symptoms included pseudobulbar affect, dizziness, nausea, tremor, nystagmus, sensory loss and spasticity.1 The clinical course without treatment is suggested to be relapsing–remitting with progressive worsening seen during relapses and residual neurologic sequelae.3
As the name implies, this disorder is responsive to glucocorticosteroid-based immunosuppression that must be administered long-term for sustained improvement.4 The pathogenesis of CLIPPERS is unknown but the presence of lymphocytic infiltration and responsiveness to immunosuppressive therapies suggests an inflammatory or autoimmune mediated pathogenesis.
Case report
The patient is a 52-year-old man who presented with 2 years of progressive spasticity, dysarthria, and gait instability. In the first year of symptoms, he was diagnosed with Parkinson’s disease based on tremor, rigidity, and gait instability; however, he failed to improve with a trial of levodopa. In his second year of symptoms, he experienced night sweats, 60-pound weight loss, and progressive worsening of gait and coordination.
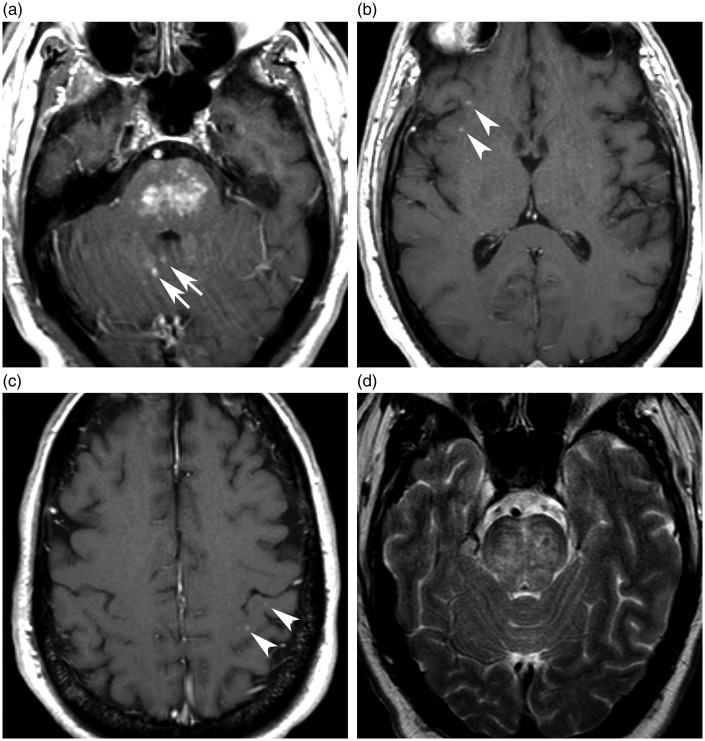
Neurologic examination was remarkable for ataxia (optic, truncal, appendicular and speech), and diffuse spasticity and hyperreflexia. A brain MRI showed small enhancing parenchymal nodules coalescing in the central pons, but also affecting the cerebellum and cerebellar peduncles, with more punctate enhancing lesions in the cerebral lobar subcortical white matter, in a pattern suggestive of CLIPPERS.1,2 Although corresponding edema has been variably reported with CLIPPERS, the pons edema in our patient was in a pattern suggesting a perivascular process, with transverse bands in a pattern nearly identical to one previously reported (Figure 1).1,3,5,6 A presumptive diagnosis of CLIPPERS was made while tests were arranged to narrow the broad differential diagnosis for his presentation. The patient received a 5-day course of high-dose steroids, which significantly improved his ataxia. His spasticity and hyperreflexia remained unchanged. A computer tomography (CT) scan of the abdomen revealed perirenal soft tissue infiltration suggestive of lymphoma, leukemia, or Erdheim–Chester disease (ECD). Biopsy of the perirenal soft tissue mass revealed foamy non-Langerhans histiocytes compatible with a diagnosis of ECD.
Figure 1.
Selected images from MRI brain exam obtained at presentation, ECD of the CNS mimicking imaging findings of CLIPPERS. (a) Axial T1-weighted post-contrast image through the pons shows small, discrete enhancing lesions coalescing in the central pons. Additional cerebellar lesions (arrows). (b–c) Axial T1-weighted post-contrast images through the cerebral hemispheres show additional punctate lobar subcortical lesions (arrowheads). (d) Axial T2-weighted image through the pons shows transverse bands of edema, and mild swelling, a pattern of CLIPPERS reported by Taieb and colleagues.3
CLIPPERS: chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids; CNS: central nervous system; ECD: Erdheim–Chester disease MRI: magnetic resonance imaging.
Discussion
This case illustrates the brain imaging similarities between ECD and CLIPPERS. Our patient was initially managed with a working diagnosis of CLIPPERS but was found on further investigation to have ECD, confirmed with biopsy.
Though the patient presented in this case was eventually diagnosed with ECD, the differential diagnosis for CLIPPERS is large and includes infectious etiologies, paraneoplastic, neoplastic, and dominant inflammatory processes.2 Patients have been identified whose clinico-radiological presentations initially resembled the diagnosis of CLIPPERS but later were discovered to have malignancy, including cases of lymphomatoid granulomatosis that evolved into fatal B-cell lymphoma, primary CNS lymphoma, low grade glioma, and potential primary angiitis of the CNS.2 Furthermore, the linkage to lymphoma is confounded by cases of CLIPPERS in coexistence with indolent lymphoma, such as have been reported with Mycosis fungoides.7 In addition to cases of malignancy, other immunologic processes have been shown to be connected to cases of CLIPPERS. Overall, two cases of CLIPPERS in patients with pre-existing multiple sclerosis, which is a demyelinating disease of the central nervous system, have been described.2
There are important aspects of a clinical case that should cause physicians to question the presumptive diagnosis of CLIPPERS (i.e. poor response to glucocorticoids). The patient presented in this case did respond to glucocorticoids, much like other patients thought to have CLIPPERS subsequent changes in the diagnosis. De Graaff ande colleagues reported a patient with CLIPPERS who repeatedly responded well to high-dose corticosteroids, but had a biopsy-confirmed diagnosis of lymphomatoid granulomatosis that evolved to fatal B-cell lymphoma of the CNS.6 The clinical and radiologic findings in our patient were consistent with CLIPPERS and only after significantly worsening of the Glasgow Coma Scale score did the team search for an alternative diagnose. The differential diagnosis of CLIPPERS includes lymphoid malignancy and other inflammatory processes largely mediated by lymphocytes. Thus, it is not surprising that the response to steroids cannot be relied upon as a means of ruling out differential diagnoses given that lymphocyte reduction in the presence of glucocorticoids is not unique to one process.8
While brainstem biopsy allows for accurate histologic diagnosis of CLIPPERS, the potential danger of brainstem biopsy limits its utility in diagnosis. In one report, parenchymal brainstem biopsy had an 11% complication rate and a greater than one percent fatality rate.9 A CT scan of the chest, abdomen, and pelvis was performed in the presented case to evaluate for systemic disease, leading to perirenal soft tissue biopsy and the histologic diagnosis of ECD.
In summary, this case highlights the importance of recognizing the differential diagnosis of patchy pontine enhancement. In our case, CLIPPERS was used as a working diagnosis, with continued pursuit of the final diagnosis of ECD. Diagnosis of certain pathologic brain regions continues to be a difficult process. Due to high morbidity of biopsy, imaging and clinical history and physical exam play important roles in outlining the differential diagnosis. Due to high concern for more malignant processes, the exclusion criteria of the CLIPPERS diagnosis must be stringently implemented in order to avoid an incorrect diagnosis. This is particular relevant when attempting to differentiate a relatively benign process such as CLIPPERS from the comparatively more malignant diseases such as B-cell lymphoma and histiocytosis.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Pittock S, Debruyne J, Krecke K, et al. Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS). Brain 2010; 133: 2626–2634. [DOI] [PubMed] [Google Scholar]
- 2.Dudesek A, Rimmele F, Tesar S, et al. CLIPPERS: chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids. Review of an increasingly recognized entity within the spectrum of inflammatory central nervous system disorders. J Clin Exp Immunol 2014; 175: 385–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taieb G, Duflos C, Renard D, et al. Long-term outcomes of CLIPPERS (chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids) in a consecutive series of 12 patients. Arch Neurol 2012; 69: 847–855. [DOI] [PubMed] [Google Scholar]
- 4.Sedrak P, Ketonen L, Hou P, et al. Erdheim–Chester disease of the central nervous system: new manifestations of a rare disease. Am J Neuroradiol 2011; 32: 2126–2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pesaresi I, Sabato M, Desideri I, et al. 3.0 T MR investigation of CLIPPERS: Role of susceptibility weighted and perfusion weighted imaging. Magn Reson Imaging 2013; 31: 1640–1642. [DOI] [PubMed] [Google Scholar]
- 6.De Graaff HJ, Wattjes MP, Rozemuller-Kwakkel AJ, et al. Fatal B-cell lymphoma following chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids. JAMA Neurol 2013; 70: 915–918. [DOI] [PubMed] [Google Scholar]
- 7.Reddy, Soma Madhan, et al. Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS): A case report and review of literature. Ann Indian Acad Neurol 2015; 18: 345–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coutinho AE, Chapman KE. The anti-inflammatory and immunosuppressive effects of glucocorticoids, recent developments and mechanistic insights. Mol Cell Endocrinol 2011; 335: 2–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mokhtari K, Houillier C, Hoang-Xuan K. Brain biopsy in a patient suffering from primary CNS lymphoma treated with steroids. EANO 2012; 2: 95–96. [Google Scholar]