Abstract
Background:
Using mechanical ventilation devices has unique advantages for the patient; however, it can also cause various problems. This study aimed to determine the effect of using communication boards on the ease of communication and anxiety in mechanically ventilated conscious patients admitted to intensive care units (ICUs).
Materials and Methods:
In this quasi-experimental study, 30 conscious patients undergoing mechanical ventilation were enrolled using consecutive sampling method and assigned to experimental (n = 15) and control (n = 15) groups. The control group included patients receiving primary communication methods, whereas the experimental group included patients who used the communication board for communication. The Hospital Anxiety and Depression Scale (HADS) and Ease of Communication Scale (ECS) were completed for both groups. Data were analyzed using descriptive-inferential statistics.
Results:
Communication scores of the patients indicated that there was no significant difference between the control and experimental groups before the intervention (z = −1.77; p = 0.070). However, after the intervention, there was a significant difference in communication scores between the two groups (z = −4.69; p = 0.001). The anxiety scale scores showed a significant difference between the control and experimental groups after the intervention, and patients' anxiety had significantly decreased in the experimental group (z = −2.98; p = 0.003).
Conclusions:
The results showed that the use of the communication board is possible in mechanically ventilated conscious patients and may contribute to ease of communication and decrease patients' anxiety during mechanical ventilation.
Keywords: Anxiety, communication, intensive care unit, Iran, ventilators
Introduction
Mechanical ventilation is widely used to treat patients who are in critical condition. This treatment method is commonly applied for breathing difficulties. However, the need for the use of this treatment method has increased due to the augmented rate of open-heart surgery and increased number of brain injuries due to road accidents.[1] The aim of using mechanical ventilation is not to treat lung disease, but to protect the patient's lungs by providing ventilation and oxygenation until the elimination of the underlying causes.[2] Although the use of assisted ventilation devices has unique benefits for patients, it also causes stress, sleep disturbance, isolation, and inability to speak.[3] Annually, about 2.7 million patients in the United States, who are hospitalized in intensive care units (ICUs), are not able to speak mostly because of the artificial airway and assisted ventilation.[4]
Some recent studies have revealed that providing mechanical ventilated conscious patients with light sedation has medical benefits, such as reduced duration of mechanical ventilation and length of stay in the ICU and even reduced risk of complications associated with immobility.[5],[6] Therefore, in the future practice, it is expected that patients be more conscious during mechanical ventilation.[7] Consciousness while undergoing mechanical ventilation results in various experiences associated with breathlessness, fear, anxiety, helplessness, lack of control, and pain.[8] Not being able to communicate either verbally or using assistive equipment is one of the worst experiences of these patients and leads to anger and hopelessness among them.[7] Happ et al. reported that although communication exchanges with patients in the ICU were generally (>70%) successful, more than one-third (37.7%) of communications about pain were unsuccessful.[9] Khalaila et al. found that fear and anger were expressed in response to difficulty in communication.[10] Patients in the ICU who are unable to communicate verbally may use nonverbal communication techniques to relate their needs, such as mouthing words, writing, or using gestures. However, these techniques, which can be subjectively interpreted by communication partners, may lead to misinterpretation of the patient's intent, thus further contributing to the patient's frustration and distress.[11] Therefore, to improve communication in mechanically ventilated patients, assisted communication approaches should be widely applied. One of these approaches is the communication board method which was first described by Appel-Hardin in 1984. The content of this board includes the basic needs of patients, such as pain, hunger, images of body parts, and names of people, such as spouse and family members.[12] The results of studies on using communication boards to communicate with conscious intubated patients showed that applying the communication board increases patients' satisfaction and reduces their anxiety and hopelessness.[12],[13] However, in Iran, only one research has been conducted on communication with patients who are mechanically ventilated[14] and no research has been performed on the use of communication boards among these patients. Therefore, this study aimed to evaluate the effect of using communication boards on ease of communication and anxiety in mechanically ventilated conscious patients admitted to ICUs.
Materials and Methods
This quasi-experimental study was carried out in the ICU of Imam Khomeini Hospital, Urmia, Iran. Participants were selected from among patients who were hospitalized in the ICU (general ICU (22 beds) and neurological ICU (6 beds)) during April 2014 to December 2014. The participants were divided into experimental and control groups. Based on 95% confidence interval (CI), power of 80%, effect size of 13.30, and the study results of Happ et al.,[15] the sample size was calculated as 15 individuals in each group. The conscious patients undergoing mechanical ventilation were chosen with the verification of an anesthesiologist using consecutive sampling method. The inclusion criteria included being in the age range of 18-65 years, oriented to person, place and date (Glasgow Coma Scale score >13), intubated for more than 24 h, literate at least at the primary school level, no previous history of hospitalization in an ICU, and lack of hearing/vision difficulties and mental illness.
To collect information, three questionnaires, including a demographic information questionnaire, the Hospital Anxiety and Depression Scale (HADS), and the Ease of Communication Scale (ECS), were used. The HADS consists of depression and anxiety subscales, each of which consists of seven questions. The anxiety subscale was used in this study. Items of the questionnaire were scored based on a 4-point Likert scale (0-3). The range of anxiety scores was from 0 to 21 and higher scores indicated greater anxiety. The validity and reliability of the Iranian version of the questionnaire have been evaluated by Montazeri et al.[16] They reported a Cronbach's alpha coefficient (to test reliability) of 0.78 for the anxiety subscale of the HADS.[16] The ECS consists of six questions that measure the difficulty of communication in patients who cannot speak. The hardness of communicating was scored based on a 5-point Likert scale (0 = not hard at all, 1 = a little hard, 2 = somewhat hard, 3 = very hard, 4 = too hard). The score of “ease of communication” for the patients who were not able to speak was obtained by summing up scores of the six questions. The score range was 0-24. In this questionnaire, higher scores indicated greater hardness of communication for the patients. The validity and reliability of the Iranian version of the ECS were determined by the researcher. The scale was translated into Persian and then translated back into English, and it was found that it was reversible. The validity and content quality of the questionnaire were evaluated and confirmed by 10 experts in the field of nursing and intensive care medicine. Content validity ratio (CVR) and content validity index (CVI) were used for the quantitative validation of the content. Thus, the questions that had a CVI of more than 0.75 and CVR of more than 0.42 were retained and used in this study. Validity analysis showed satisfactory results and all questions (six items) were retained. The reliability of the questionnaire, which was equal to 0.9, was assessed using Cronbach's alpha.
The communication board that was used in this study was partly derived from the Vidatak EZ Board that was designed in 1999 in the United States and its dimensions were 42 × 29.70 cm. The needs of the patient were illustrated on one side of the board using related images and written form. The other side of the board consisted of two parts: one part was the schematic picture of the body to determine the location of the pain and the other part was considered as a whiteboard. The study procedure was that patients who had the inclusion criteria were assigned to the control group using consecutive sampling method, and then, after completing the control group sampling, patients were consecutively assigned to the experimental group. The control group included patients receiving the routine nursing communication practices, whereas the experimental group consisted of patients who, in addition to routine communication, used the communication board (the researcher taught patients, nurses, and head nurses how to use the communication boards). Data collection methods were similar in both groups. The initial interview was conducted for both groups through completion of the questionnaires by the researcher 24 h after consciousness of the patients. The HADS and ECS questions were read to the patients who were asked to show the answers typed in bold. The questionnaires were completed again in both groups 48 h after the initial interview. The Statistical Package for the Social Sciences (version 20, IBM Corporation, Armonk, NY, USA) was used for data analysis. Data were presented as average and standard deviation (SD) and percentage. Because of the non-normal distribution of data, non-parametric tests (Mann–Whitney test) were used to compare communication and anxiety scores among control and experimental groups. p values of less than 0.05 were considered statistically significant.
Ethical consideration
This study was approved by the Ethics Committee of Urmia University of Medical Sciences, Iran (umsu.rec. 1392.80). The patients and their family members were informed of the study aim and process. Participation in this study was completely voluntary and free from any obligation to the physician, nursing staff, or researcher. Furthermore, the patients' companions were asked to sign the informed written consent form.
Results
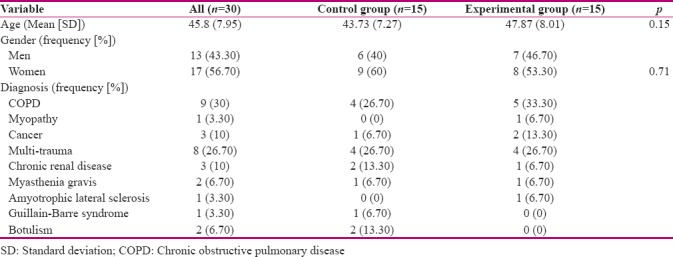
In this study, 30 patients met the inclusion criteria. Furthermore, the most common primary diagnosis among the participants was chronic obstructive pulmonary disease (COPD). Most of the patients were women (56.70%), and the mean (SD) age of the subjects was 45.8 (7.95) years. The results of this study showed that there was no significant difference between the experimental and control groups in terms of age and gender [Table 1].
Table 1.
Comparison of participants’ characteristics according to study groups
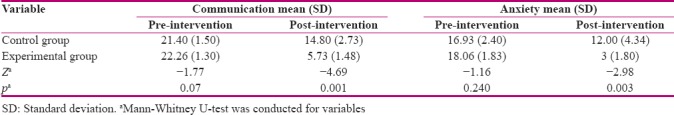
The mean communication and anxiety scores in both groups are presented in Table 2. Communication scores of the patients indicated that there was no significant difference between the two groups before the intervention (p < 0.070). After the intervention, mean (SD) communication score in the control group was 14.80 (2.73) and in experimental group was 5.73 (1.48), which showed a significant difference between the control and experimental groups (p < 0.001). The mean (SD) anxiety scores in the experimental and control groups before the intervention were 16.93 (2.49) and 18.06 (1.83), respectively (p < 0.24), which decreased significantly after the intervention among groups (p < 0.003).
Table 2.
Comparison of communication and anxiety scores before and after the intervention in control and experimental groups
Discussion
Communication is one of the most important factors affecting the outcome of treatment. Therefore, considering the communication problem in hospitalized patients who need mechanical ventilation is of particular importance.[17] Inability to speak and communication difficulty during mechanical ventilation have been reported as an unpleasant experience for many patients in the ICU.[18],[19]
The results of this study showed that using communication boards in mechanically ventilated conscious patients led to ease of communication. Radtke et al., in a case study examining three patients under mechanical ventilation, have reported that using Augmentative and Alternative Communication (AAC) with low and high technology led to increased effective communication in patients.[20] Moreover, Happ et al.[15] Das,[21] and El-Soussi et al.[22] found that communication board is one of the most important methods that facilitates communication in intubated patients and increases patients' satisfaction. In another study, nonspeaking postoperative patients who had undergone head and neck surgery [8 (72%)] reported that the commonly used communication strategy was writing with the use of loose paper, a tablet, or notepad.[19]
This study showed that communication boards reduced anxiety in mechanically ventilated patients. This finding is consistent with the findings of other studies which have shown that picture cards and communication boards can be effective approaches to reducing anxiety caused by the inability to speak.[14],[22] Another study, which aimed to determine the level of frustration in patients under mechanical ventilation at the time of using and not using communication boards, reported that using communication boards led to reduced frustration.[12] Moreover, Chan-ui et al. have reported that the care plans for the patients who used communication cards were more efficiently suited to their needs and reduced patients' frustration.[13] Lazarus and Cohen have stated in their study that when there is an appropriate response to a need, anxiety is reduced;[23] therefore, it can be concluded that resolving patients' needs, using the boards, results in a reduced level of anxiety.
The results of this study showed that communication was difficult for mechanically ventilated conscious patients after 24 h of intubation. However, this difficulty was reduced, after a while, in the control group without using communication aid supplies. In fact, the results of this study indicated that the conventional methods of communication, such as body language and eye contact, are effective factors in information exchange. This is in line with the findings of the study by El-Soussi et al. on the use of augmented alternative communication methods in intubated patients.[22] Their observation of the control group (primary communication methods) revealed that the critical care nurses were able to identify the patient's needs through gesture, mouthing, and facial expression, and half of the patients reported that communication was helpful.[22] Moreover, there are other studies that have demonstrated that conscious patients under mechanical ventilation can use public communication methods successfully and the use of other communication aids can also facilitate communication for them.[9],[24]
This study was limited to two ICUs in one hospital and may not reflect nurse–patient communication performance in other locales or settings. Differences in the ability of the patients to write on the communication board and the occurrence of stressful events in the research environment were factors that could affect the results and could not be controlled by the researchers.
Conclusion
Considering the findings of this study, it can be concluded that the use of communication aid supplies by mechanically ventilated conscious patients can facilitate communication, and subsequently, reduce the anxiety levels in these patients. However, further investigations are required to evaluate the efficiency of using communication boards and other facilitating communication methods with respect to increasing satisfaction, reducing anxiety, and achieving adequate and appropriate pain management. It may also be useful to study the experiences of families and nurses regarding the use of the communication board.
Financial support and sponsorship
Urmia University of Medical Sciences, Urmia, Iran.
Conflicts of interest
Nothing to declare.
Acknowledgements
The authors would like to express their deep appreciation of the participants for their cooperation, and also nurses and all those who collaborated in this study. They are also grateful to Urmia University of Medical Sciences, Urmia, Iran, for funding this research (code number 1296).
References
- 1.Aarabi A, Tavakol K. Patient's experiences of mechanical ventilation. IJNMR. 2009;14:83–8. [Google Scholar]
- 2.Nikravan-Mofrad M, Shiri H. Critical care nursing in ICU, CCU and dialysis. Tehran: Noore-Danesh; 2008. p. 115. [Google Scholar]
- 3.Coyer FM, Wheeler MK, Wetzig SM, Couchman BA. Nursing care of the mechanically ventilated patient: What does the evidence say? Part two. ICCN. 2007;23:71–80. doi: 10.1016/j.iccn.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 4.Angus D, Shorr A, White A, Dremsizov T, Schmitz R, Kelley M, et al. Critical care delivery in the United States: Distribution of services and compliance with Leapfrog recommendations. Crit Care Med. 2006;34:1016–24. doi: 10.1097/01.CCM.0000206105.05626.15. [DOI] [PubMed] [Google Scholar]
- 5.Strøm T, Martinussen T, Toft P. A protocol of no sedation for critically ill patients receiving mechanical ventilation: A randomised trial. Lancet. 2010;375:475–80. doi: 10.1016/S0140-6736(09)62072-9. [DOI] [PubMed] [Google Scholar]
- 6.Laerkner E, Stroem T, Toft P. No-sedation during mechanical ventilation: Impact on patient's consciousness, nursing workload and costs. Nurs Crit Care. 2016;21:28–35. doi: 10.1111/nicc.12161. [DOI] [PubMed] [Google Scholar]
- 7.Baumgarten M, Poulsen I. Patients' experiences of being mechanically ventilated in an ICU: A qualitative metasynthesis. Scand J Caring Sci. 2015;29:205–14. doi: 10.1111/scs.12177. [DOI] [PubMed] [Google Scholar]
- 8.Karlsson V, Bergbom I, Forsberg A. The lived experiences of adult intensive care patients who were conscious during mechanical ventilation: A phenomenological-hermeneutic study. ICCN. 2012;28:6–15. doi: 10.1016/j.iccn.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 9.Happ MB, Garrett K, Thomas DD, Tate J, George E, Houze M, et al. Nurse-patient communication interactions in the intensive care unit. AJCC. 2011;20:28–40. doi: 10.4037/ajcc2011433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khalaila R, Zbidat W, Anwar K, Bayya A, Linton DM, Sviri S. Communication difficulties and psychoemotional distress in patients receiving mechanical ventilation. AJCC. 2011;20:470–9. doi: 10.4037/ajcc2011989. [DOI] [PubMed] [Google Scholar]
- 11.Kleinpell RM, Patak L, Wilson-Stronks A, Costello J, Person C, Henneman EA, et al. Communication in the ICU 2008 [updated 2008; cited] [Last accessed on 2016 May 24]. Available from: http://nursing.advanceweb.com .
- 12.Patak L, Gawlinski A, Fung NI, Doering L, Berg J, Henneman EA. Communication boards in critical care: Patients' views. Appl Nurs Res. 2006;19:182–90. doi: 10.1016/j.apnr.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 13.Chan-ui P, Thaniwattananon P, Petpichetchian W. Effects of communication card on received care based on needs and perceived communication frustration in endotracheal intubated patients. Nurs Sci Health. 2010;33:1–11. [Google Scholar]
- 14.Parsa-Yekta Z, Sharifi-Neiestanak N, Mehran A, Imani-Pour M. Quasi experimental research on anxiety and satisfaction of patients undergoing open cardiac surgery having intubation. Hayat. 2002;8:5–12. [Google Scholar]
- 15.Happ MB, Roesch TK, Garrett K. Electronic voice-output communication aids for temporarily nonspeaking patients in a medical intensive care unit: A feasibility study. Heart Lung. 2004;33:92–101. doi: 10.1016/j.hrtlng.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 16.Montazeri A, Vahdaninia M, Ebrahimi M, Jarvandi S. The Hospital Anxiety and Depression Scale (HADS): Translation and validation study of the Iranian version. Health Qual Life Outcomes. 2003;1:1–5. doi: 10.1186/1477-7525-1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rajan R. Development of a communication board to identify needs of patient on mechanical ventilation post coronary artery bypass grafting. cognitive Discourse International Multidisicplinary. 2013;1:210–2. [Google Scholar]
- 18.Samuelson KAM. Unpleasant and pleasant memories of intensive care in adult mechanically ventilated patients–Findings from 250 interviews. ICCN. 2011;27:76–84. doi: 10.1016/j.iccn.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 19.Rodriguez CS, Blischak DM. Communication needs of nonspeaking hospitalized postoperative patients with head and neck cancer. Appl Nurs Res. 2010;23:110–5. doi: 10.1016/j.apnr.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 20.Radtke JV, Baumann BM, Garrett KL, Happ MB. Listening to the voiceless patient: Case reports in assisted communication in the intensive care unit. J Palliat Med. 2011;14:791–5. doi: 10.1089/jpm.2010.0313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Das D. A study to assess the effectiveness of communication pattern among patients on mechanical ventilator in Bombay hospital at Indore in the year 2014-2015. IJAR. 2016;4:1720–47. [Google Scholar]
- 22.El-Soussi AH, Elshafey MM, Othman SY, Abd-Elkader FA. Augmented alternative communication methods in intubated COPD patients: Does it make difference. Egyptian J Chest Dis Tuberc. 2015;64:21–8. [Google Scholar]
- 23.Lazarus R, Cohen JB. Environmental Stress. Human Behavior and Environment. New York: Springer US; 1977. pp. 89–127. [Google Scholar]
- 24.Happ MB, Garrett KL, Tate JA, DiVirgilio D, Houze MP, Demirci JR, et al. Effect of a multi-level intervention on nurse-patient communication in the intensive care unit: Results of the SPEACS trial. Heart Lung. 2014;43:89–98. doi: 10.1016/j.hrtlng.2013.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]


