Abstract
Objectives
The objectives were to (1) systematically review the literature on the implementation of eHealth interventions for informal caregivers of people with dementia, and (2) identify determinants of successful implementation.
Methods
Online databases were searched for articles about eHealth interventions for informal caregivers of people with dementia, providing information on their implementation. Articles were independently screened and inductively analyzed using qualitative analysis. The analysis was mapped onto the Consolidated Framework for Implementation Research (CFIR; Damschroder et al., 2009).
Findings
46 articles containing 204 statements on implementation were included. The statements on implementation were grouped into four categories: Determinants associated with the eHealth application, informal caregiver, implementing organization, or wider context. Mapping of the determinants on the CFIR revealed that studies have focused mostly on characteristics of the intervention and informal caregiver. Limited attention has been paid to organizational determinants and the wider context.
Conclusions
Despite prolific effectiveness and efficacy research on eHealth interventions for caregivers of people with dementia, there is a critical dearth of implementation research. Furthermore, there is a mismatch between eHealth intervention research and implementation frameworks, especially concerning organizational factors and wider context. This review underscores the importance of future implementation research in bridging the gap between research and practice.
Keywords: Dementia, Caregiver, Internet, eHealth, Implementation, Review
Highlights
-
•
There is a lack of implementation research for these interventions.
-
•
Research focuses on the caregiver and the characteristics of the intervention.
-
•
Research should focus more on the implementing organization and wider context.
-
•
There is a mismatch between research and implementation frameworks.
-
•
More research is needed to develop appropriate theories to frame these studies.
1. Introduction
Informal caregivers are essential to providing home-based care for people with dementia. Research has shown that the quality of care received by a person with dementia positively relates to a longer time spent being cared for at home, which is critical to the physical and mental health of the person with dementia (Alzheimer's Association, 2015; Spijker et al., 2008). However, informal caregivers of people with dementia often experience significant physical and psychological problems themselves as a result of this caregiving process, including increases in depression, stress, social isolation, financial burden, and disturbed sleep (Peacock and Forbes, 2003).
Given these adverse consequences, it is crucial to provide caregivers with tools to help them receive caregiving support, as well as to allow them a life outside of caregiving. With the dementia population (47 million people worldwide) expected to grow threefold by 2050 (Han et al., 2014), this increasing need for support has led to many innovative approaches, including those emerging from the promising field of eHealth research. The term ‘eHealth’ describes “the use of information and communication technologies (ICT) for health” (WHO, 2018). eHealth interventions are “treatments, typically behaviorally based, that are operationalized and transformed for delivery via the Internet” (Ritterband et al., 2006). For instance, eHealth interventions can take the form of an online course, administered via computer; they can also be smartphone or tablet applications designed to provide psychological support from peers and professionals alike. eHealth interventions have the advantage of a lower threshold of access for participation, as well as the ability to reach more isolated populations who struggle to access traditional services (Topo, 2009). Recent reviews have shown that eHealth interventions for informal caregivers of people with dementia are effective in improving a range of psychological outcomes in caregivers, such as the reduction of caregiver depression, anxiety, stress and burden, as well as increasing positive aspects of caregiving, caregiver self-efficacy, and confidence (Boots et al., 2014; Jackson et al., 2016; Lee, 2015; Parra-Vidales et al., 2017; Scott et al., 2016; Tyack and Camic, 2017).
However, despite this proven efficacy, little is known about how to ensure that these interventions are successfully implemented (i.e. put into practice). Previous research on eHealth interventions has shown that, despite their proven efficacy, as well as enthusiasm regarding eHealth from funding and policy institutions, the implementation of eHealth interventions in ageing populations has proven difficult. Reasons for this include older individuals' changes in their perceptual, cognitive, and motor abilities, in combination with the continuing rapid development of new technologies (Preschl et al., 2011). The objectives of this review are (1) to explore the evidence on the topic of implementing eHealth interventions for informal caregivers of people with dementia, and (2) to identify determinants that influenced whether the intervention was successfully implemented. The results of this study will help bridge the gap between our knowledge of the efficacy of eHealth interventions for informal caregivers of people with dementia, and the translation of this knowledge into practice.
2. Methods
2.1. Search strategy
A systematic literature search of bibliographic databases PubMed, CINAHL, PsycINFO, Cochrane Library and Web of Science was conducted in May 2017. The search was aimed at finding articles that contained information on which factors determined the implementation of eHealth interventions for caregivers of people with dementia. In order to accomplish this, the aforementioned databases were searched for articles that contained terms related to all three of the following main concepts: ‘dementia’, ‘eHealth’ and ‘caregivers’. Relevant MeSH and Thesaurus terms were used, as well as additional non-MeSH terms, so as to identify the full range of indexed and non-indexed articles. Appendix A details the employed search strategies: first the union (‘OR’) of terms to capture articles related to each single main concept, and second the intersection (‘AND’) of main concepts to focus on the purpose of this review.
The search strategy does not contain relevant terms related to ‘implementation’ (such as ‘facilitators and barriers’, ‘determinants’ or ‘implementation’), because the authors anticipated that such terms are often not mentioned in the title and/or abstract. Instead, implementation issues may only be discussed in the body of the text, potentially using different terms. This information could only be assessed by reading the full-texts in a later, post-abstract screening phase. Thus, we aimed to have a complete overview of all research on implementing eHealth interventions for caregivers of people with dementia, without missing important information due to terminology constraints.
2.2. Study selection
Titles and abstracts of the identified citations were imported into Endnote, deduplicated and independently evaluated by first reviewer (HLC) and second reviewer (SLB). Included references had to involve an (1) eHealth (2) intervention for (3) informal caregivers of people with dementia and (4) provide information on its implementation. In order to assess whether references met criterion 4 (provides information on implementation), the full-texts were scanned for the presence of determinants of implementation. These were statements about factors that either facilitated or impeded the process.
Non-intervention studies such as reviews, trial protocols, book reviews and consensus papers were excluded. Otherwise, any design was judged as suitable for inclusion. Studies on assistive technology that were not specifically designed to improve caregiver well-being, as well as telephone-only, video-only and CD-ROM-based interventions were also not included. Non-English-language publications and articles published before 2007 were excluded from this review. 2007 was chosen as the cut-off year for this review. It was believed that studies from more than 10 years ago would not provide much additional, relevant information due to the evaluated technologies having become outdated, as well as policies and organizations having changed greatly in the interim. After searching for eHealth [All Fields], the PubMed-generated histogram ‘Results by year’ showed a rise in eHealth research after 1994, followed by a plateau from 1998 to 2007. After 2007, the number of references recommenced its rise. The authors concluded that 2007, the year of the first iPhone, signified a turning point in mobile technology (Cuthbertson et al., 2015) and a relevant cut-off point. Any disagreements about inclusion were resolved through a consensus meeting consisting of three reviewers; HLC, SLB and MEdV.
2.3. Data extraction
Articles that met all four criteria were compiled into a standardized data extraction instrument as recommended by Cochrane Handbook for Systematic Reviews of Interventions (Higgins and Green, 2011) (see Appendix B) detailing primary study characteristics (author/year, design, setting, study population, intervention, measures, findings and country of study), as well as the extracted determinants. The PRISMA guidelines (Liberati et al., 2009) were used to guide the process of study selection and data analysis. However, not all elements of this guideline were followed as this systematic review focused on process characteristics and not on effectiveness.
2.4. Data analysis
A qualitative thematic analysis was performed in which statements related to eHealth implementation (“the process of putting the intervention into practice”) issues were coded and labeled ‘determinants’. The determinants were inductively grouped to form thematically similar categories, subcategories and groups. The authors opted for an inductive method in order to best scope the available literature and contrast the findings with existing implementation frameworks. Reviewers HLC and SLB independently coded and mapped these determinants by hand, identifying the article as 0 (contains no determinants) or 1 (contains determinants) and mapping these determinants into inductive categories using an online ‘mind mapping’ tool (Google Mindmup 2 software, October 2017 version, developed by Sauf Pompiers Ltd.; https://drive.mindmup.com). In the next step a consensus meeting was held between reviewers HLC and SLB, with the input of reviewer MEdV. Finally, to structure and contextualize the findings, the resulting analysis was compared and mapped onto the Consolidated Framework for Implementation Research (Damschroder et al., 2009). The Consolidated Framework for Implementation Research (CFIR) was chosen because it is a commonly used, practical set of constructs, which were readily applicable to eHealth intervention research for caregivers of people with dementia.
3. Results
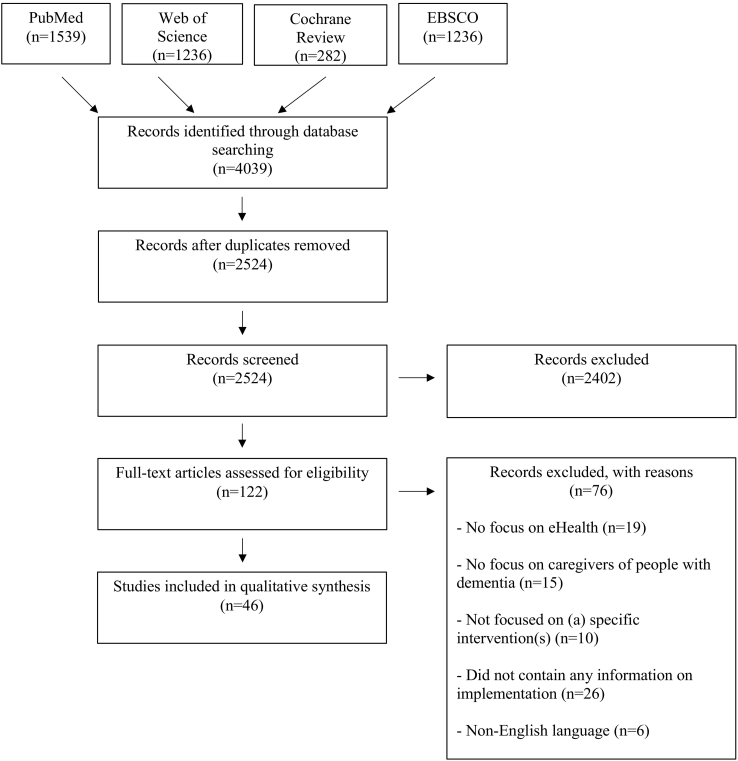
Fig. 1 depicts a flow chart illustrating the process of inclusion and exclusion. The search strategy described in Appendix A resulted in a total of 2524 records after deduplication. 2401 articles were excluded because they did not meet the criteria of involving an (1) eHealth (2) intervention for (3) informal caregivers of people with dementia. After screening these full texts for the fourth criterion (“provides information on implementation”), 46 records were included, which contained 204 determinants of implementation.
Fig. 1.
Flow chart of process of inclusion and exclusion.
The results of this search strategy show that only two of the included 46 references were implementation studies (Boots et al., 2017; Griffiths et al., 2016) The results of this search strategy show that only one of the included 46 references used the term ‘implementation’ in the title (Griffiths et al., 2016) and one study used the term ‘process evaluation’ in the title (Boots et al., 2017). Four more studies were designed as retrospective evaluations of barriers and facilitators to the development and implementation of eHealth interventions for caregivers of people with dementia (Chiu and Eysenbach, 2011; Davis et al., 2014; Malak et al., 2016; Werner et al., 2017). The included papers could be classified by type of study as RCTs (n = 16), pre-test and post-test mixed methods studies (n = 15), qualitative analyses of interviews and other text-based sources (n = 14), and quantitative studies, like questionnaires (n = 2). When classifying the references by type of intervention, the vast majority of the included interventions concerned web-based platforms for psycho-education and support (n = 38). The remaining interventions (n = 9) were adaptations of existing in-person psychosocial interventions to technological platforms including individual videophone, group and individual teleconference, and group virtual reality sessions. For a more detailed overview of the types of included interventions, see the Extraction Table included in Appendix B. The determinants have been grouped together inductively in four thematic categories, namely ‘Determinants associated with the eHealth application’, ‘Determinants associated with the informal caregiver’, ‘Determinants associated with the implementing organization’ and ‘Determinants associated with the wider context’. In the following sections the main findings are presented. Table 1 is an overview of the thematic categories and subcategories.
Table 1.
Overview of themes, categories and subcategories, with references.
3.1. Determinants associated with the characteristics of the eHealth application
The largest thematic category of determinants was ‘Characteristics of the eHealth application’: 116 of the 204 determinants fell into this category. A large group of the determinants in this category described ways of facilitating the implementation process by making the eHealth application itself more user-friendly. For instance, application developers must make hyperlinks to navigate through the application easily identifiable and consistent. In terms of the development process of the interventions, the importance of user-involvement throughout the whole process and allowing for enough time to improve the website were recurrently identified as important facilitating factors.
Additionally, the included articles listed many ‘lessons learned’ and a great number of determinants described ways in which the features of the applications could be optimized. First, several determinants specified additional features. A frequently mentioned request from participants was for the addition of a ‘search function’ to the platform. Next, many determinants stressed the importance of appropriate content: The determinants suggested that the content should take into account the phase of dementia and preferred themes of instruction, and that the developers must also invest in keeping the content up-to-date. Another important feature of an application is its link to social media: The included articles contained several determinants describing the positive effects of social media on the intervention's content and reach. Additionally, one study determined that ‘embodied experience’ was important for online engagement, and several studies stressed how applications must take appropriate measures to include the maximum amount of security. For instance, several determinants mentioned that continuous troubleshooting support was essential and that participants experienced concern about a lack of security as a significant barrier. Finally, many determinants proposed that a sense of adaptability and personal contact is what made the intervention effective.
Simplicity was a recurring subject of many implementation determinants. Application users stressed the importance of reducing the amount, spread and complexity of information, adding that complexity is associated with increased security risks. They also preferred the language used to be as simple as possible. Compatibility was another common theme, where determinants described the convenience of the at-home setting of eHealth interventions, the effect of time on both the emergence of effects, as well as on the changing needs of the users and the cost. A large number of determinants described the effect of the trial setting on the interventions and the implementation difficulties these restrictions caused. Finally, human interaction with application featured strongly in the literature, most noticeably in how the participants wanted their application to be adaptable and personalized to their needs.
3.2. Determinants associated with the informal caregiver
The second largest thematic category was ‘Determinants associated with the informal caregiver’. Sixty-nine of the 204 determinants fell in this category. Many implementation determinants described certain psychological characteristics of the informal caregiver that facilitated or impeded implementation. These characteristics included the caregiver's expectation of use, their psychological state (though studies reported both positive and negative effects of higher burden on engagement with the intervention), trust, autonomy, motivation, confidence, frustration, cyber rapport and privacy. Of note is that the largest group is ‘Privacy’, with statements emphasizing the anxiety often felt by participants about using technology to document personal issues, and the need to address this barrier.
Another factor that determined an intervention's success in being translated into practice was the informal caregiver's knowledge. For instance, (especially a lack of) digital literacy and mental health literacy, as well as the caregivers' learning styles, were mentioned as determinants by the included studies. Moreover, certain demographic variables such as gender and age were identified as implementation determinants. In particular, ethnicity and culture were frequently mentioned, with determinants suggesting that interventions could have minority specific effects. Interestingly, education was not described as having a large impact. The informal caregiver's relation to the person with dementia was seen as important. For example, increased severity of the dementia diagnosis was a barrier, though the presence of a formal diagnosis was seen as beneficial. Additionally, the type of relationship to the person with dementia (spouse, child, neighbor, etc.) also played a role. For instance, in one study (Cristancho-Lacroix et al., 2015) the relationship correlated with program opinion (husbands and sons were more positive about the program). Caregiving workload was also identified as an important factor, in that the busier caregivers were, the less usage took place. Finally, social support and regular usage were each reported (once) as facilitating factors.
3.3. Determinants associated with the implementing organization
This category contained 46 of the 204 determinants. Quite a few included studies mentioned determinants associated with the staff of the implementing organization. A lack of staff and a lack of interaction with staff were described as barriers to implementation. Staff training, replacement when staff leaves and the presence of staff practitioners were described as facilitators. Certain staff attitudes were cast as negative determinants of implementation. Reluctance about the technology, as well as insecurities (about both ethical and technological issues) was reported as impeding implementation within the organizational context.
Many determinants focused on the barriers posed by financial and time constraints. It was reiterated that including a face-to-face element to the intervention is beneficial, though it increases costs considerably. Some studies specified certain characteristics of the implementing organization itself. For instance, five determinants stressed that researchers need an intervention “provider” to collaborate with in implementing the intervention. Determinants also stressed the importance of teamwork and highlighted that smaller organizations struggle to provide the necessary support and up-to-date content previously described, due to lack of a PR department and other necessary facilities. The articles also included determinants detailing the barriers posed by this necessary integration of the intervention into existing (care) systems. Among them are privacy issues, competition between organizations, and gatekeeping by members of the organization. Finally, suggested implementation strategies included reconciling community and organizational characteristics, streamlining processes for monitoring intervention fidelity, and active facilitation of the service uptake.
3.4. Determinants associated with the wider context
This final category is the smallest and contains 20 determinants. Care policy was described in a few articles as an important determinant of implementation. In particular, the limited capability of health insurance authorities to support innovation, and their preference for classically delivered care was identified as a significant barrier. Moreover, many municipalities do not see the added value of a disease-specific tool. However, it was also stated that an important facilitator was that eHealth and its philosophy of self-management fits within recent policy developments. A country-specific facilitator was the Affordable Care Act in the U.S.A. Country-specific barriers included the slow availability of broadband in the Netherlands, and the difficulties associated with Spanish-language websites, such as barriers with international search engines. Finally, 11 determinants also discussed certain ethical issues encountered in their study that posed potential barriers in successfully implementing the intervention. In this regard, requirements concerning informed consent were described, as well as a number of issues pertaining to equal access. For instance, within a trial context, all users should be offered training, support, internet access, and all necessary equipment free of charge.
3.5. Mapping the determinants
The Consolidated Framework for Implementation Research (CFIR) (Damschroder et al., 2009) offers a framework to contextualize and structure the identified determinants. The CFIR is composed of five major domains: Intervention Characteristics, Outer Setting, Inner Setting, Characteristics of the Individuals Involved, and Process of the Implementation. These domains each contain a number of constructs, which are not discussed in detail here (Damschroder et al., 2009). The majority of the determinants (see the Extraction Table, Appendix B) identified by this review can be situated under the domain Characteristics of the Intervention and the domain Characteristics of the Individuals Involved (normally, the implementing organization; here, the informal caregivers) that used them. Very little work has been done on continuing the interventions past their trial phase (Vernooij-Dassen and Moniz-Cook, 2014) and evaluating factors associated with the Process, Inner Setting, and Outer Setting. Table 1 confirms that the majority of determinants provide information on how the application and user characteristics might influence successful implementation, while much less is being said about the determinants associated with the implementing organization and the wider context.
4. Discussion
4.1. Overview of the existing implementation research
The first objective of this study was to explore what research had been done concerning the implementation of eHealth interventions for caregivers of people with dementia given the abundance of effectiveness trials for these interventions (Boots et al., 2014; Jackson et al., 2016; Lee, 2015; Parra-Vidales et al., 2017; Scott et al., 2016; Tyack and Camic, 2017). The fact that only one study could be found referring to ‘implementation’ in its title suggests that implementation research on eHealth interventions for caregivers of people with dementia is still in its infancy (Griffiths et al., 2016). Indeed, the implementation literature is dwarfed by the efficacy literature, though this is by no means specific to eHealth interventions (Carroll and Rounsaville, 2007).
4.2. Summary of identified determinants of implementation
Despite the paucity of specific implementation research, there were many studies that described valuable experiences and ‘lessons learned’ in putting interventions into practice. In relation to this study's second objective, summarizing what the literature has described as determining factors for implementation, this review has identified four main groups of determinants. This has resulted in a useful overview of the current literature for future researchers to inform the development and implementation of their eHealth interventions for caregivers of people with dementia. For instance, when it comes to designing an eHealth intervention to facilitate implementation, a number of recommendations have been made to increase user-friendliness and design features relevant to caregivers. Furthermore, it is important for applications to be flexible, personalized, and adaptable to the individual needs of the participants. Previous eHealth studies have also underscored the importance of personalization (Camerini et al., 2013; Krebs et al., 2010; Lentferink et al., 2017; Strecher et al., 2006), citing the effect of the perceived increased personal relevance of the intervention. Moreover, this review provides evidence that there are a number of important factors associated with the person of the caregiver. Psychological factors, prior knowledge and learning styles, demographic variables, reasons to participate/withdraw, the relationship of the caregiver to the person with dementia, the availability of social support, and the caregivers' workload and regular usage of the intervention were all reported to influence engagement and subsequent implementation. This (in addition to the frequently mentioned prerequisite of ‘personalization’) suggests that there is no ‘one size fits all’ implementation approach to eHealth for caregivers of people with dementia. As is typical for psychological interventions, it is a matter of ‘what works for whom’ (Roth and Fonagy, 2013). The fairly limited amount of studies that discussed determinants associated with the implementing organization emphasized the importance of staff factors, financial resources, time, organizational factors, and integration into existing systems, in addition to recommending a number of specific strategies. When it came to the wider context, studies stressed the effect of local care policies, as well as ethical dilemmas that influenced implementation.
4.3. A mismatch between implementation research and eHealth research
The two largest themes of determinants were mapped onto the CFIR domains Characteristics of the Intervention and Characteristics of the Individual. There was a marked absence of studies going into depth on the CFIR domains Process, Inner Setting, and Outer Setting. This uneven distribution showcases an important finding of this review: There is a mismatch between the focus of research being conducted on eHealth interventions for caregivers of people with dementia, and the focus of implementation frameworks to guide and assess their implementation.
On the one hand, the focus of the research being conducted on eHealth interventions for caregivers of people with dementia does not match the existing implementation frameworks very well. Specifically, there are two implementation blind spots in the current literature on eHealth interventions for caregivers of people with dementia. First, there is a noticeable lack of research examining the effect of contextual factors, such as the organization and wider context. This is evidenced by the relatively few articles in the themes ‘Determinants associated with the implementing organization’ and ‘Determinants associated with the wider context’. The absence of knowledge on the contextual environment creates significant difficulties for health system planners and implementers who aim to translate these interventions into practice (Edwards and Barker, 2014; Vernooij-Dassen and Moniz-Cook, 2014). Indeed, Goldzweig et al. (2009) propose that, despite its many advantages, the paucity of information on contextual factors and process changes has contributed to the slow implementation of eHealth in general. Second, very few studies place emphasis on the process and time-related factors. For instance, there is a need for studies discussing the iterative process of adapting both the intervention and the organization (redefining and remodeling, respectively; Rogers (2010)), and formatively evaluating this adaptation process. Furthermore, the included studies mostly focused on putting the interventions into practice merely in the context of academic research, with very little work being done on continuing the interventions past their trial phase. The CFIR is not alone in emphasizing the importance of these contextual and time-related factors, as these are dimensions that recur frequently in many common implementation framework (DeLone and McLean, 2003; Greenhalgh et al., 2004; Meiland et al., 2004; Murray et al., 2010).
On the other hand, the focus of the implementation frameworks does not match the conducted eHealth research well. Implementation frameworks struggle to encompass the wealth of information from eHealth studies at the level of the end-user (in this case, the informal caregiver). Though the second largest group of identified determinants fell under the theme ‘Determinants associated with the informal caregiver’, the CFIR and other implementation frameworks have little room to place these end-user determinants. While there are more psychology-related models that emphasize the perspective of the end-user (Bandura and Walters, 1977; Davis, 1985; Venkatesh et al., 2012), there remains a lack of suitable implementation models to map the complexity of end-users' determinants and interactions with the application. Instead, as is the case with the majority of implementation frameworks (DeLone and McLean, 2003; Greenhalgh et al., 2004; Meiland et al., 2010), the CFIR describes implementation from the perspective of the implementing organization: The domain ‘Characteristics of the Individual’ again refers to the individuals within the organization, and not the end-users (informal caregivers).
In sum, both eHealth intervention research and organizational implementation research contain gaps of understanding, and future implementation research must take an integrative and multidisciplinary approach in order to be effective. Frameworks such as the Medical Research Council's (MRC) framework for complex interventions (Craig et al., 2008) can provide guidance for eHealth solutions by placing emphasis on investigating contextual determinants and other process characteristics through process evaluations.
4.4. Limitations
This study has some limitations. First, the employed search strategy did not include methods of searching grey literature or studies that have not been written up in English. By not including these sources, we may have missed valuable information. Second, because this review's focus was on implementation characteristics, articles were not selected based on the quality of their effectiveness study. However, the included articles were sourced from peer-reviewed journals, signifying that they are all of an academic quality and level. Finally, this review draws on secondary analyses. This highlights the lack of readily available primary data on eHealth intervention implementation, illustrating the need for the collection of such implementation data in future research.
5. Conclusions
This review aimed to explore what is known about the implementation of eHealth interventions of caregivers of people with dementia. Its findings illustrate that little attention has been paid to their implementation in the real world, outside of the academic intervention research context. When research does mention implementation, it is often limited to the characteristics of the application and of the end-users (in this case the informal caregivers). Practical implementation issues, systematically involving organizational factors, and taking into account contextual and societal factors, have largely been neglected. Conclusions drawn from the included non-implementation research nonetheless give insight into a range of ways in which characteristics of the eHealth application, informal caregiver, implementing organization, and wider context can facilitate their successful implementation.
eHealth interventions show promise for improving the lives of informal caregivers, and reducing future strain on health care services by enabling caregivers to care longer and more ably for their loved ones with dementia. Moreover, eHealth interventions are uniquely suited for widespread implementation due to their low cost, low threshold of access, and potential for personalization to achieve tailor-made solutions. However, it is imperative that future research prioritizes implementation research and evaluates barriers and facilitators to long-term use in the community. Finally, without evidence-based knowledge of effective implementations strategies, researchers developing eHealth interventions for caregivers of people with dementia will be hard-pressed to convince the necessary stakeholders and decision makers of their practical use, and thus allow these innovative and exciting interventions to make a difference in the lives of the caregivers who would (and should) benefit from them.
The following are the supplementary data related to this article.
Search strategy
Acknowledgements
The authors of this review would like to thank the authors of the included papers for providing additional information when requested, and access to the manuscripts when needed. The authors would also thank MindTech for their help and advice. The research presented in this paper was carried out as part of the Marie Curie Innovative Training Network (ITN) action, H2020-MSCA-ITN-2015, under grant agreement number 676265.
Contributor Information
Hannah L. Christie, Email: hannah.christie@maastrichtuniversity.nl.
Sara L. Bartels, Email: sara.bartels@maastrichtuniversity.nl.
Lizzy M.M. Boots, Email: l.boots@maastrichtuniversity.nl.
Huibert J. Tange, Email: h.tange@maastrichtuniversity.nl.
Frans R.J. Verhey, Email: f.verhey@maastrichtuniversity.nl.
Marjolein E. de Vugt, Email: m.devugt@maastrichtuniversity.nl.
References
- Alzheimer's Association 2015 Alzheimer's disease facts and figures. Alzheimers Dement. 2015;11:332. doi: 10.1016/j.jalz.2015.02.003. [DOI] [PubMed] [Google Scholar]
- Andersson S., Magnusson L., Hanson E. The use of information and communication technologies to support working carers of older people - a qualitative secondary analysis. Int. J. Older People Nursing. 2016;11:32–43. doi: 10.1111/opn.12087. [DOI] [PubMed] [Google Scholar]
- Bandura A., Walters R.H. 1977. Social Learning Theory. [Google Scholar]
- Blom M.M., Zarit S.H., Groot Zwaaftink R.B., Cuijpers P., Pot A.M. Effectiveness of an internet intervention for family caregivers of people with dementia: results of a randomized controlled trial. PLoS One. 2015;10 doi: 10.1371/journal.pone.0116622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boots L., Vugt M., Knippenberg R., Kempen G., Verhey F. A systematic review of Internet-based supportive interventions for caregivers of patients with dementia. Int. J. Geriatr. Psychiatry. 2014;29:331–344. doi: 10.1002/gps.4016. [DOI] [PubMed] [Google Scholar]
- Boots L.M., de Vugt M.E., Smeets C.M., Kempen G.I., Verhey F.R. Implementation of the blended care self-management program for caregivers of people with early-stage dementia (partner in balance): process evaluation of a randomized controlled trial. J. Med. Internet Res. 2017;19 doi: 10.2196/jmir.7666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boots L.M.M., de Vugt M.E., Withagen H.E.J., Kempen G., Verhey F.R.J. Development and initial evaluation of the web-based self-management program “partner in balance” for family caregivers of people with early stage dementia: an exploratory mixed-methods study. JMIR Res. Protoc. 2016;5 doi: 10.2196/resprot.5142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd K., Nugent C., Donnelly M., Bond R., Sterritt R., Hartin P. An Investigation into the Usability of the STAR Training and Re-Skilling Website for Carers of Persons With Dementia; Conference Proceedings: Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Annual Conference; 2014. pp. 4139–4142. [DOI] [PubMed] [Google Scholar]
- Camerini L., Camerini A.-L., Schulz P.J. Do participation and personalization matter? A model-driven evaluation of an Internet-based patient education intervention for fibromyalgia patients. Patient Educ. Couns. 2013;92:229–234. doi: 10.1016/j.pec.2013.04.007. [DOI] [PubMed] [Google Scholar]
- Carroll K.M., Rounsaville B.J. A vision of the next generation of behavioral therapies research in the addictions. Addiction. 2007;102:850–862. doi: 10.1111/j.1360-0443.2007.01798.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu T., Marziali E., Colantonio A., Carswell A., Gruneir M., Tang M., Eysenbach G. Internet-based caregiver support for Chinese Canadians taking care of a family member with Alzheimer disease and related dementia. Can. J. Aging. 2009;28:323–336. doi: 10.1017/S0714980809990158. [DOI] [PubMed] [Google Scholar]
- Chiu T.M.L. ProQuest Information & Learning; US: 2010. Usage and Non-usage Behaviour of Ehealth Services among Chinese Canadians Caring for a Family Member with Dementia; p. 2286. [Google Scholar]
- Chiu T.M.L., Eysenbach G. Theorizing the health service usage behavior of family caregivers: a qualitative study of an internet-based intervention. Int. J. Med. Inform. 2011;80:754–764. doi: 10.1016/j.ijmedinf.2011.08.010. [DOI] [PubMed] [Google Scholar]
- Chiu T.M.L., Marziali E., Tang M., Colantonio A., Carswell A. Client-centered concepts in a personalized e-mail support intervention designed for Chinese caregivers of family members with dementia: a qualitative study. Hong Kong J. Occup. Ther. 2010;20:87–93. [Google Scholar]
- Craig P., Dieppe P., Macintyre S., Michie S., Nazareth I., Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337 doi: 10.1136/bmj.a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cristancho-Lacroix V., Wrobel J., Cantegreil-Kallen I., Dub T., Rouquette A., Rigaud A.S. A web-based psychoeducational program for informal caregivers of patients with Alzheimer's disease: a pilot randomized controlled trial. J. Med. Internet Res. 2015 doi: 10.2196/jmir.3717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuthbertson R., Furseth P.I., Ezell S.J. Springer; 2015. Apple and Nokia: The Transformation from Products to Services, Innovating in a Service-Driven Economy; pp. 111–129. [Google Scholar]
- Czaja S.J., Loewenstein D., Schulz R., Nair S.N., Perdomo D. A videophone psychosocial intervention for dementia caregivers. Am. J. Geriatr. Psychiatry. 2013;21:1071–1081. doi: 10.1016/j.jagp.2013.02.019. [DOI] [PubMed] [Google Scholar]
- Damschroder L.J., Aron D.C., Keith R.E., Kirsh S.R., Alexander J.A., Lowery J.C. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement. Sci. 2009;4:50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dang S., Remon N., Harris J., Malphurs J., Sandals L., Cabrera A.L., Nedd N. Care coordination assisted by technology for multiethnic caregivers of persons with dementia: a pilot clinical demonstration project on caregiver burden and depression. J. Telemed. Telecare. 2008;14:443–447. doi: 10.1258/jtt.2008.080608. [DOI] [PubMed] [Google Scholar]
- Davis B.H., Nies M.A., Shehab M., Shenk D. Developing a pilot e-mobile app for dementia caregiver support: lessons learned. Online J. Nurs. Inform. 2014;18:21–28. [Google Scholar]
- Davis B.H., Shehab M., Shenk D., Nies M. E-mobile pilot for community-based dementia caregivers identifies desire for security. Gerontechnology. 2015;13:332–336. [Google Scholar]
- Davis F.D. Massachusetts Institute of Technology; 1985. A Technology Acceptance Model for Empirically Testing New End-User Information Systems: Theory and Results. [Google Scholar]
- Delone W.H., McLean E.R. The DeLone and McLean model of information systems success: a ten-year update. J. Manag. Inf. Syst. 2003;19(4):9–30. [Google Scholar]
- Edwards N., Barker P.M. The importance of context in implementation research. J. Acquir. Immune Defic. Syndr. 2014;67:S157–S162. doi: 10.1097/QAI.0000000000000322. [DOI] [PubMed] [Google Scholar]
- Finkel S., Czaja S.J., Schulz R., Martinovich Z., Harris C., Pezzuto D. E-care: a telecommunications technology intervention for family caregivers of dementia patients. Am. J. Geriatr. Psychiatry. 2007;15:443–448. doi: 10.1097/JGP.0b013e3180437d87. [DOI] [PubMed] [Google Scholar]
- Fowler C., Haney T., Rutledge C.M. An Interprofessional virtual healthcare neighborhood for caregivers of elderly with dementia. J. Nurse Pract. 2014;10:829–834. [Google Scholar]
- Gaugler J.E., Hobday J.V., Robbins J.C., Barclay M.P. CARES (R) dementia Care for Families (TM) effects of online, psychoeducational training on knowledge of person-centered care and satisfaction. J. Gerontol. Nurs. 2015;41:18–U81. doi: 10.3928/00989134-20150804-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaugler J.E., Reese M., Tanler R. Care to plan: an online tool that offers tailored support to dementia caregivers. Gerontologist. 2016;56:1161–1174. doi: 10.1093/geront/gnv150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldzweig C.L., Towfigh A., Maglione M., Shekelle P.G. Costs and benefits of health information technology: new trends from the literature. Health Aff. 2009;28:w282–w293. doi: 10.1377/hlthaff.28.2.w282. [DOI] [PubMed] [Google Scholar]
- Greenhalgh T., Robert G., Macfarlane F., Bate P., Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q. 2004;82(4):581–629. doi: 10.1111/j.0887-378X.2004.00325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths P.C., Whitney M.K., Kovaleva M., Hepburn K. Development and implementation of Tele-Savvy for dementia caregivers: a department of veterans affairs clinical demonstration project. The Gerontologist. 2016;56:145–154. doi: 10.1093/geront/gnv123. [DOI] [PubMed] [Google Scholar]
- Han J.W., Jeong H., Park J.Y., Kim T.H., Lee D.Y., Lee D.W., Ryu S.-H., Kim S.-K., Yoon J.C., Jhoo J. Effects of social supports on burden in caregivers of people with dementia. Int. Psychogeriatr. 2014;26:1639–1648. doi: 10.1017/S1041610214001331. [DOI] [PubMed] [Google Scholar]
- Hattink B., Droes R.M., Sikkes S., Oostra E., Lemstra A.W. Evaluation of the digital Alzheimer center: testing usability and usefulness of an online portal for patients with dementia and their carers. JMIR Res. Protoc. 2016;5:193–206. doi: 10.2196/resprot.5040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hattink B., Meiland F., van der Roest H., Kevern P., Abiuso F., Bengtsson J., Giuliano A., Duca A., Sanders J., Basnett F. Web-based STAR E-learning course increases empathy and understanding in dementia caregivers: results from a randomized controlled trial in the Netherlands and the United Kingdom. J. Med. Internet Res. 2015;17 doi: 10.2196/jmir.4025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayden L.J., Glynn S.M., Hahn T.J., Randall F., Randolph E. The use of Internet technology for psychoeducation and support with dementia caregivers. Psychol. Serv. 2012;9:215–218. doi: 10.1037/a0027056. [DOI] [PubMed] [Google Scholar]
- Hicken B.L., Daniel C., Luptak M., Grant M., Kilian S., Rupper R.W. Supporting caregivers of rural veterans electronically (SCORE) J. Rural. Health. 2016 doi: 10.1111/jrh.12195. [DOI] [PubMed] [Google Scholar]
- Higgins J.P., Green S. John Wiley & Sons; 2011. Cochrane Handbook for Systematic Reviews of Interventions. [Google Scholar]
- Jackson D., Roberts G., Wu M.L., Ford R., Doyle C. A systematic review of the effect of telephone, internet or combined support for carers of people living with Alzheimer's, vascular or mixed dementia in the community. Arch. Gerontol. Geriatr. 2016;66:218–236. doi: 10.1016/j.archger.2016.06.013. [DOI] [PubMed] [Google Scholar]
- Judge K.S., Bass D.M., Snow A.L., Wilson N.L., Morgan R., Looman W.J., McCarthy C., Kunik M.E. Partners in dementia care: a care coordination intervention for individuals with dementia and their family caregivers. Gerontologist. 2011;51:261–272. doi: 10.1093/geront/gnq097. [DOI] [PubMed] [Google Scholar]
- Kajiyama B., Thompson L.W., Eto-Iwase T., Yamashita M., Di Mario J., Marian Tzuang Y., Gallagher-Thompson D. Exploring the effectiveness of an Internet-based program for reducing caregiver distress using the iCare stress management e-training program. Aging Ment. Health. 2013;17:544–554. doi: 10.1080/13607863.2013.775641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kales H.C., Gitlin L.N., Lyketsos C. “We Care Advisor”: A Clinical Trial of a Caregiver Focused, ipad Administered Algorithm to Manage Behavioral Symptoms; Alzheimer's and Dementia. Conference: Alzheimer's Association international conference 2016. Canada. Conference start: 20160722. Conference end: 20160728; 2016. p. P217. [Google Scholar]
- Ko J.W. University of Iowa; 2011. Alzheimer's Disease and Related Disorders Caregiver's Acceptance of a Web-Based Structured Written Emotional Expression Intervention; p. 187. [Google Scholar]
- Krebs P., Prochaska J.O., Rossi J.S. A meta-analysis of computer-tailored interventions for health behavior change. Prev. Med. 2010;51:214–221. doi: 10.1016/j.ypmed.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwok T., Au A., Wong B., Ip I., Mak V., Ho F. Effectiveness of online cognitive behavioral therapy on family caregivers of people with dementia. Clin. Interv. Aging. 2014;9:631–636. doi: 10.2147/CIA.S56337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee E. Do Technology-based support groups reduce care burden among dementia caregivers? A review. J. Evid.-Inf. Soc. Work. 2015;12:474–487. doi: 10.1080/15433714.2014.930362. [DOI] [PubMed] [Google Scholar]
- Lentferink A.J., Oldenhuis H.K., de Groot M., Polstra L., Velthuijsen H., van Gemert-Pijnen J.E. Key components in eHealth interventions combining self-tracking and persuasive eCoaching to promote a healthier lifestyle: a scoping review. J. Med. Internet Res. 2017;19 doi: 10.2196/jmir.7288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6 doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorig K., Thompson-Gallagher D., Traylor L., Ritter P.L., Laurent D.D., Plant K., Thompson L.W., Hahn T.J. Building better caregivers: a pilot online support workshop for family caregivers of cognitively impaired adults. J. Appl. Gerontol. 2012;31:423–437. [Google Scholar]
- Lundberg S. The results from a two-year case study of an information and communication technology support system for family caregivers. Disabil. Rehabil. 2014;9:353–358. doi: 10.3109/17483107.2013.814170. [DOI] [PubMed] [Google Scholar]
- Malak R., Krawczyk-Wasielewska A., Mojs E., Grobelny B., Glodowska K.B., Millan-Calenti J.C., Nunez-Naveira L., Samborski W. The opinion of professional caregivers about the platform UnderstAID for patients with dementia. Med. Sci. Monit. 2016;22:3623–3627. doi: 10.12659/MSM.900444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marx K.A., Gitlin L.N., Lyketsos C., Kales H.C., Stanislawski B. Testing a web-based application to help informal caregivers manage behaviors in persons with dementia: we careadvisorTM, Alzheimer's and dementia; Conference: Alzheimer's Association International Conference 2016. Canada. Conference start: 20160722. Conference end: 20160728; 2016. p. 300. [Google Scholar]
- Marx K.A., Werner N.E., Kales H., Turnwald M., Stanislawski B., Gitlin L.N. Usability testing of a web-based application for caregivers of people with dementia: the WeCareAdvisor tool. Gerontologist. 2015;55:597. [Google Scholar]
- Meiland F.J., Dröes R.M., De J.L., Vernooij-Dassen M.J. Development of a theoretical model for tracing facilitators and barriers in adaptive implementation of innovative practices in dementia care. Arch. Gerontol. Geriatr. Suppl. 2004;(9):279–290. doi: 10.1016/j.archger.2004.04.038. Chicago. [DOI] [PubMed] [Google Scholar]
- Murray E., Treweek S., Pope C., MacFarlane A., Ballini L., Dowrick C.…Ong B.N. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Med. 2010;8(1):63. doi: 10.1186/1741-7015-8-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Núñez-Naveira L., Alonso-Búa B., Labra C., Gregersen R., Maibom K., Mojs E., Krawczyk-Wasielewska A., Millán-Calenti J.C. UnderstAID, an ICT platform to help informal caregivers of people with dementia: a pilot randomized controlled study. Biomed. Res. Int. 2016:5726465. doi: 10.1155/2016/5726465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connor M.-F., Arizmendi B.J., Kaszniak A.W. Virtually supportive: a feasibility pilot study of an online support group for dementia caregivers in a 3D virtual environment. J. Aging Stud. 2014;30:87–93. doi: 10.1016/j.jaging.2014.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagán-Ortiz M.E., Cortés D.E., Rudloff N., Weitzman P., Levkoff S. Use of an online community to provide support to caregivers of people with dementia. J. Gerontol. Soc. Work. 2014;57:694–709. doi: 10.1080/01634372.2014.901998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parra-Vidales E., Soto-Perez F., Perea-Bartolome M.V., Franco-Martin M.A., Munoz-Sanchez J.L. Online interventions for caregivers of people with dementia: a systematic review. Actas espanolas de psiquiatria. 2017;45:116–126. [PubMed] [Google Scholar]
- Peacock S.C., Forbes D.A. Interventions for Caregivers of Persons with Dementia: A Systematic Review Interventions auprès des aidantes naturelles dispensant des soins aux personnes atteintes de démence: une évaluation systématique. Can. J. Nurs. Res. 2003;35:88–107. [PubMed] [Google Scholar]
- Pino M., Boulay M., Jouen F., Rigaud A.-S. ‘Are we ready for robots that care for us?’ attitudes and opinions of older adults toward socially assistive robots. Front. Aging Neurosci. 2015;7 doi: 10.3389/fnagi.2015.00141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pot A.M., Blom M.M., Willemse B.M. Acceptability of a guided self-help internet intervention for family caregivers: mastery over dementia. Int. Psychogeriatr. 2015;27:1343–1354. doi: 10.1017/S1041610215000034. [DOI] [PubMed] [Google Scholar]
- Preschl B., Wagner B., Forstmeier S., Maercker A. E-health interventions for depression, anxiety disorder, dementia, and other disorders in old age: a review. J. CyberTher. Rehabil. 2011;4:371–386. [Google Scholar]
- Ritterband L.M., Andersson G., Christensen H.M., Carlbring P., Cuijpers P. Directions for the international society for research on internet interventions (ISRII) J. Med. Internet Res. 2006;8 doi: 10.2196/jmir.8.3.e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers E.M. Simon and Schuster; 2010. Diffusion of Innovations. [Google Scholar]
- Roth A., Fonagy P. Guilford Publications; 2013. What Works for Whom?: A Critical Review of Psychotherapy Research. [Google Scholar]
- Schaller S., Marinova-Schmidt V., Gobin J., Criegee-Rieck M., Griebel L., Engel S., Stein V., Graessel E., Kolominsky-Rabas P.L. Tailored e-Health services for the dementia care setting: a pilot study of ‘eHealthMonitor’. BMC Med. Informat. Decis. Making. 2015;15 doi: 10.1186/s12911-015-0182-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaller S., Marinova-Schmidt V., Setzer M., Kondylakis H., Griebel L., Sedlmayr M., Graessel E., Maler J.M., Kirn S., Kolominsky-Rabas P.L. Usefulness of a tailored eHealth service for informal caregivers and professionals in the dementia treatment and care setting: the eHealthMonitor dementia portal. JMIR Res. Protoc. 2016;5 doi: 10.2196/resprot.4354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott J.L., Dawkins S., Quinn M.G., Sanderson K., Elliott K.-E.J., Stirling C., Schüz B., Robinson A. Caring for the carer: a systematic review of pure technology-based cognitive behavioral therapy (TB-CBT) interventions for dementia carers. Aging Ment. Health. 2016;20:793–803. doi: 10.1080/13607863.2015.1040724. [DOI] [PubMed] [Google Scholar]
- Serafini J.D., Damianakis T., Marziali E. Clinical practice standards and ethical issues applied to a virtual group intervention for spousal caregivers of people with Alzheimer's. Soc. Work Health Care. 2007;44:225–243. doi: 10.1300/J010v44n03_07. [DOI] [PubMed] [Google Scholar]
- Spijker A., Vernooij-Dassen M., Vasse E., Adang E., Wollersheim H., Grol R., Verhey F. Effectiveness of nonpharmacological interventions in delaying the institutionalization of patients with dementia: a meta-analysis. J. Am. Geriatr. Soc. 2008;56:1116–1128. doi: 10.1111/j.1532-5415.2008.01705.x. [DOI] [PubMed] [Google Scholar]
- Strecher V.J., Shiffman S., West R. Moderators and mediators of a web-based computer-tailored smoking cessation program among nicotine patch users. Nicotine Tob. Res. 2006;8:S95–S101. doi: 10.1080/14622200601039444. [DOI] [PubMed] [Google Scholar]
- Topo P. Technology studies to meet the needs of people with dementia and their caregivers a literature review. J. Appl. Gerontol. 2009;28:5–37. [Google Scholar]
- Torp S., Bing-Jonsson P.C., Hanson E. Experiences with using information and communication technology to build a multi-municipal support network for informal carers. Inform. Health Soc. Care. 2013;38:265–279. doi: 10.3109/17538157.2012.735733. [DOI] [PubMed] [Google Scholar]
- Torp S., Hanson E., Hauge S., Ulstein I., Magnusson L. A pilot study of how information and communication technology may contribute to health promotion among elderly spousal carers in Norway. Health Soc. Care Commun. 2008;16:75–85. doi: 10.1111/j.1365-2524.2007.00725.x. [DOI] [PubMed] [Google Scholar]
- Tyack C., Camic P.M. Touchscreen interventions and the well-being of people with dementia and caregivers: a systematic review. Int. Psychogeriatr. 2017 doi: 10.1017/S1041610217000667. [DOI] [PubMed] [Google Scholar]
- van der Roest H.G., Meiland F.J.M., Jonker C., Droes R.M. User evaluation of the DEMentia-specific digital interactive social chart (DEM-DISC). A pilot study among informal carers on its impact, user friendliness and, usefulness. Aging Ment. Health. 2010;14:461–470. doi: 10.1080/13607860903311741. [DOI] [PubMed] [Google Scholar]
- Van Mierlo L.D., Meiland F.J., Van de Ven P.M., Van Hout H.P., Droes R.M. Evaluation of DEM-DISC, customized e-advice on health and social support services for informal carers and case managers of people with dementia; a cluster randomized trial. Int. Psychogeriatr. 2015;27:1365–1378. doi: 10.1017/S1041610215000423. [DOI] [PubMed] [Google Scholar]
- Venkatesh V., Thong J.Y., Xu X. Consumer acceptance and use of information technology: extending the unified theory of acceptance and use of technology. MIS Q. 2012:157–178. [Google Scholar]
- Vernooij-Dassen M., Moniz-Cook E. Taylor & Francis; 2014. Raising the Standard of Applied Dementia Care Research: Addressing the Implementation Error. [DOI] [PubMed] [Google Scholar]
- Verwey R., van Berlo M., Duymelinck S., Willard S., van Rossum E. Development of an online platform to support the network of caregivers of people with dementia. Studies in health technology and informatics. 2016;225:567–571. [PubMed] [Google Scholar]
- Wasilewski M.B., Webster F., Stinson J.N., Cameron J.I. Adult children caregivers' experiences with online and in-person peer support. Comput. Hum. Behav. 2016;65:14–22. [Google Scholar]
- Werner N.E., Stanislawski B., Marx K.A., Watkins D.C., Kobayashi M., Kales H., Gitlin L.N. Applied Clinical Informatics. Vol. 8. 2017. Getting what they need when they need it. Identifying barriers to information needs of family caregivers to manage dementia-related behavioral symptoms; pp. 191–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO eHealth at WHO. (2018, March 23) 2018. http://www.who.int/ehealth/about/en/ Retrieved from.
- Willems C.G., Vlaskamp F.J.M. Innovation of health care provision: observations made during the development of two care products in the Netherlands. Technol. Disabil. 2008;20:241–249. [Google Scholar]
- Williams K., Arthur A., Niedens M., Moushey L., Hutfles L. In-home monitoring support for dementia caregivers: a feasibility study. Clin. Nurs. Res. 2013;22:139–150. doi: 10.1177/1054773812460545. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search strategy