Abstract
Background
It remains difficult to predict and prevent suicidal behaviour, despite growing understanding of the aetiology of suicidality. Clinical guidelines recommend that health care professionals develop a safety plan in collaboration with their high-risk patients, to lower the imminent risk of suicidal behaviour. Mobile health applications provide new opportunities for safety planning, and enable daily self-monitoring of suicide-related symptoms that may enhance safety planning. This paper presents the rationale and protocol of the Continuous Assessment for Suicide Prevention And Research (CASPAR) study. The aim of the study is two-fold: to evaluate the feasibility of mobile safety planning and daily mobile self-monitoring in routine care treatment for suicidal patients, and to conduct fundamental research on suicidal processes.
Methods
The study is an adaptive single cohort design among 80 adult outpatients or day-care patients, with the main diagnosis of major depressive disorder or dysthymia, who have an increased risk for suicidal behaviours. There are three measurement points, at baseline, at 1 and 3 months after baseline. Patients are instructed to use their mobile safety plan when necessary and monitor their suicidal symptoms daily. Both these apps will be used in treatment with their clinician.
Conclusion
The results from this study will provide insight into the feasibility of mobile safety planning and self-monitoring in treatment of suicidal patients. Furthermore, knowledge of the suicidal process will be enhanced, especially regarding the transition from suicidal ideation to behaviour.
The study protocol is currently under revision for medical ethics approval by the medical ethics board of the Vrije Universiteit Medical centre Amsterdam (METc number 2017.512/NL62795.029.17).
Keywords: Suicide prevention, Mobile health, Feasibility, Safety planning, Ecological momentary assessment
Highlights
-
•
Mobile applications provide opportunities to enhance suicide prevention methods.
-
•
Patients can augment personalised safety plans by monitoring their own mental state.
-
•
Real-time monitoring data of psychological processes can be analysed to improve our understanding of suicidality and develop new technology for suicide prevention.
1. Introduction
Suicide is a significant public health issue worldwide, with an estimated 800,000 suicides each year. Despite global efforts to reduce suicides (World Health Organization, 2014), suicide rates have either remained constant or risen in many countries in recent years (Nock et al., 2008). This highlights the need to better understand and prevent suicidal behaviour (Nock et al., 2008).
Several studies have targeted the aetiology of suicidality, and our understanding of factors associated with suicide has grown considerably over the last decade (Franklin et al., 2016). Many of the studies on risk factors associated with suicidality have focused on bivariate associations between epidemiological factors, such as the prevalence of psychopathology and suicidal behaviours (Nock et al., 2008). These distal risk factors are important from a general public health perspective, but are of limited clinical use in the identification and treatment of individuals who are at risk of acting on their thoughts of suicide (Nock et al., 2008; O'Connor and Nock, 2014; Ribeiro and Joiner, 2009).
In order to better understand and prevent suicidal behaviour in the clinical sector, the Continuous Assessment for Suicide Prevention And Research (CASPAR) study combines practice-based research with basic science. This paper describes the rationale and protocol of this study.
1.1. Theoretic framework
Most people who think about suicide (suicide ideators) do not attempt suicide, and not every transition from thoughts to suicidal behaviour results in a fatal suicide attempt (May and Klonsky, 2016). For each adult who dies by suicide, it is estimated that more than 20 others make a non-fatal suicide attempt (World Health Organization, 2014). To enhance suicide prevention methods in treatment, it is crucial to understand the factors that differentiate people who only think about suicide from those who act on their thoughts.
Suicidal behaviour is often defined as the whole of thoughts and behaviours related to an individual considering or taking their own life (O'Connor and Nock, 2014). In this study however, we make a distinction between suicidal ideation and suicidal behaviour per se, as the intention to engage in suicidal behaviour and acting on that intention are two different processes (O'Connor, 2011). Suicidal ideation will be defined as thinking about, considering, imagining or planning suicide, whereas suicidal behaviour is defined as engagement in potentially self-injurious behaviour with the intent to die (suicide attempts, both non-fatal and fatal) (Klonsky et al., 2016).
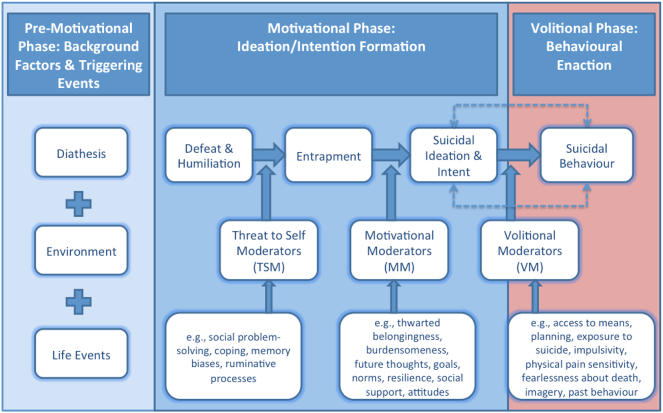
In order to reflect the difference between ideation and behaviour, the “ideation-to-action” framework of May and Klonsky (2016) suggests that there are distinct risk factors for suicidal ideation and suicidal behaviour. Consistent with the “ideation-to-action” framework, the integrated motivational-volitional (IMV) model of suicidal behaviour developed by O'Connor (2011) distinguishes between factors associated with ideation and behaviour. The IMV model integrates key factors from earlier theories to map the transition from suicidal thoughts to suicidal behaviour, among which: the Theory of Planned Behaviour (Ajzen, 1991), the diathesis-stress hypothesis (Schotte and Clum, 1987), the escape theory (Baumeister, 1990), the arrested flight model of suicidal behaviour (JMG, 2001) and the Interpersonal-Psychological model (Joiner Jr., 2005). In the IMV model, suicidal behaviour is conceptualised as behaviour that develops through pre-motivational, motivational and volitional phases and it has been recently refined (Fig. 1) (O'Connor, 2011; O'Connor & Kirtley, in press).
Fig. 1.
The integrated motivational-volitional (IMV) model of suicidal behaviour (from O'Connor & Kirtley (in press)).
The pre-motivational phase covers biosocial factors such as background factors (e.g. deprivation) and trigger events (e.g. negative life events). It describes the underlying cognitive vulnerability of a person as the result of the interaction between nature and nurture. The motivational phase defines the development of suicidal ideation and intent. It is predicted that feelings of entrapment are triggered by the experience of defeat. This transition is moderated by threat to self moderators such as coping and ruminative processes. Feelings of entrapment will trigger the development of suicidal ideation, moderated by motivational factors such as burdensomeness and dysfunctional thoughts about the future. The volitional phase is the last phase, and covers factors that govern the transition from suicidal thinking to suicidal behaviour. It is hypothesised that this transition is moderated by volitional moderators such as impulsivity, exposure to the suicidal behaviour of others, and the personal capacity for carrying out suicide (O'Connor and Nock, 2014; O'Connor, 2011; Mars et al., 2018). More information about the IMV model can be found in O'Connor (2011) and O'Connor & Kirtley (in press).
1.2. Safety planning
Safety planning is a clinical intervention component often included in the treatment of suicidal patients, and specifically aimed at the transition from having the thoughts/intention to engage in suicidal behaviours and acting upon the thoughts/intention. The research literature describes different methods of safety planning, including the safety planning intervention (Stanley and Brown, 2012; Stanley and Brown, 2008) and the crisis response plan (Rudd et al., 2006), but these methods are built on the same principles. A safety plan is a list of coping strategies and interventions (e.g., what patients can do when they are in an imminent suicidal crisis), written down on paper by the patient together with a clinician, in order to prevent suicidal behaviour (Stanley and Brown, 2012). This intervention is used in clinical practice, with the intention of enhancing the safety of high-risk suicidal patients by planning responses to impending suicidal crises (e.g. patients characterised by significant suicidal ideation, suicidal intent, suicidal plan, or/and a recent suicide attempt) (Pearson et al., 2001). The basic premise underpinning the safety plan approach is that patients can recognise and manage their suicidal thoughts and behaviours. Patients improve their self-management when faced with an imminent suicidal crisis, hereby addressing the problem before it fully emerges and preventing the impending suicidal behaviour (Stanley and Brown, 2012).
The use of safety planning strategies is primarily based on clinicians' beliefs about their effectiveness (Bryan et al., 2017). Even though safety planning has not yet been definitively tested (Hogan, 2016), it is recommended for patients at risk of suicide in suicide prevention guidelines (Van Hemert et al., 2012) and care quality standards (https://www.nice.org.uk/guidance/qs34/chapter/Quality-statement-6-Risk-management-plans) and safety plans are embedded in Cognitive Behavioural Therapy for suicide prevention (Stanley et al., 2009). Safety planning can also be considered a required safety net for research projects involving suicidal patients. As safety plans are already embedded in treatment protocols, it is difficult to test their effectiveness empirically. Fortunately, evidence for safety plans is building. In a recent RCT among US soldiers at high risk of suicide, Bryan et al. (2017) found crisis response safety planning, an intervention related to safety planning, to be effective in preventing suicide attempts compared to the use of contracts for safety (which entails a commitment from the suicidal patient to avoid engaging in suicidal behaviour).
A systematic and comprehensive method of safety planning commonly used in clinical practice is the safety planning intervention (SPI) developed by Stanley and Brown, 2012, Stanley and Brown, 2008. The SPI consists of six steps: 1) identifying early warning signs of an impending suicidal crisis (e.g. negative feelings and problematic behaviours); 2) employing internal coping strategies; 3) employing distraction activities and socialisation to distract from suicidal ideation; 4) making use of social support contacts who may offer help; 5) collating the contact details of mental health professionals and other crisis resources; and 6) making the environment safe (Stanley and Brown, 2012). These steps are personalised by the suicidal patients and their clinician in a collaborative process during treatment and written in the patient's own words. When a patient is able to identify personal negative feelings and problematic behaviours associated with their suicidality, these can be a cue for the patient to use their personal safety plan in order to obstruct the transition to suicidal behaviours (Stanley and Brown, 2012).
Safety plans are commonly written down on paper, implying they are either carried around or stored at the patients' home. Paper safety plans may therefore not always be at hand in times of crisis, which is crucial considering the fluid nature of suicidal processes (Kennard et al., 2015). There is a need for more flexible and adaptive resources for suicidal patients. The use of novel mobile technologies may improve the accessibility and usability of safety plans and can include interactive elements which make safety planning more dynamic.
1.3. Mobile mental health
Mobile technology provides new opportunities for mental health care and suicide prevention. Customised applications (apps) can be run on mobile devices to provide, for example, emotional support and behavioural coaching. Apps can be especially useful for suicide prevention interventions, because of their ability to deliver support and interventions in situ and at times of crisis, as suicide ideation and behaviour can change rapidly (Larsen et al., 2016). There are multiple apps designed to target suicidal behaviour. According to a systematic assessment of publicly available smartphone tools for suicide prevention (Larsen et al., 2016), most available apps focus on safety planning or/and obtaining support from the user's social networks. A report that studied available suicide prevention apps in the Apple Store (iOS) and Play Store (Android) concluded that it was not possible to indicate whether the provenance of the suicide apps was evidence-based, owing to the lack of information regarding how the app content was developed and tested (Aguirre et al., 2013).
Besides new opportunities for interventions, mobile technology also provides opportunities for psychological research. Self-monitoring techniques such as experience sampling or ecological momentary assessment (EMA) (Stone and Shiffman, 1994) have been used to monitor psychological processes by daily repeated self-report questions prompted by “beeps” at random times throughout the day (Shiffman et al., 2008). In recent years, the use of EMA in clinical research contexts has rapidly increased. In addition, some studies (Freedman et al., 2006; Schrimsher and Filtz, 2011; Aaron et al., 2004) have reported behavioural changes in participants over the EMA monitoring period, which may suggest that self-monitoring constitutes a therapeutic intervention in itself. Insights into the nature and dynamics of patients' own symptomatology may engender feelings of control and empowerment in relation to their symptoms (Groot, 2010).
By employing EMA in suicide research it may be possible to monitor the transition from suicidal thoughts to suicidal behaviour in real time (Myin-Germeys et al., 2009; de Beurs et al., 2015; Holmes et al., 2018). Multiple studies have demonstrated the feasibility of electronic monitoring of suicidal ideation, using hand-held computers (Nock et al., 2009; Husky et al., 2014). Results of these studies indicate that the repeated measures did not increase negative thoughts or suicidal ideation. This is consistent with retrospective reports indicating that the urge to self-harm does not increase after retrospective assessment of suicidal ideation (Eynan et al., 2014).
A recent study by Kleiman et al. (2017) examined fluctuations in suicidal ideation and its risk factors (e.g. hopelessness, burdensomeness and loneliness) using EMA on smartphones. They found that suicidal ideation and its risk factors fluctuate considerably over the course of hours. This study also attests to the feasibility of using smartphone-based EMA in research and in the treatment of suicidal patients. Since the rapid changes in suicidal ideation and its risk factors might be assessable via EMA, Kleiman et al. (2017) suggest that interventions can benefit from EMA by tracking and reacting to dynamic suicidal processes in real-time.
1.4. Study objectives
The CASPAR study has a two-fold design in which practice-based research is combined with basic science. The first part of this study will be an evaluation of the feasibility (i.e. usability, satisfaction and uptake) of mobile safety planning and daily mobile self-monitoring in routine care for patients with suicide risk. The second part will comprise fundamental research into suicidal processes, for which we have three aims: 1) validate the IMV model concerning psychological processes associated with suicidal behaviour; 2) identify individual pathways to suicidal behaviour; and 3) profile sub-types of suicidal individuals.
2. Method
2.1. Participants
The research population will consist of at least 80 adult outpatients or day-care patients in mental health care in the Netherlands who suffer from a major depressive disorder or dysthymia, and who are at elevated risk of suicidal behaviour because they engage in suicidal ideation. Participants will be recruited from 3 mental health organisations in the Netherlands. Written informed consent will be obtained from each participant.
The sample size is not based on a sample size calculation, because the primary outcomes of this study are not dependent on effect sizes. For feasibility studies, a sample size of around 60 has been recommended (Viechtbauer et al., 2015). Because of an expected 25% drop-out rate, we will recruit 80 participants. In respect of the secondary analyses, the high frequency measurement approach of EMA provides ample power for structural equation models to test the validity of theoretical models.
The CASPAR study protocol is currently under revision for medical ethics approval by the Vrije Universiteit Medical centre Amsterdam (METc number: 2017.512/NL62795.029.17).
2.2. Inclusion criteria
To be eligible to participate, patients must meet the following criteria:
-
•
Outpatient or day-care patient;
-
•
Main diagnosis of major depressive disorder or dysthymia;
-
•
Current suicidal ideation;
-
•
18 years or older;
-
•
In possession of a smartphone that runs either on Android or iOS.
2.3. Exclusion criteria
Patients are excluded from participation when they meet the following criteria:
-
•
Insufficient competence in the Dutch language;
-
•
Presence of psychotic symptoms;
-
•
Not willing or able to use smartphone apps.
2.4. Outcome measures of part 1: practice-based research
Primary outcome of part 1 is feasibility. We define feasibility by three related variables: usability, acceptability and uptake.
Usability of the mobile applications is measured with the System Usability Scale (SUS) (Brooke, 1996; Bangor et al., 2008). This scale consists of 10 questions, with a higher score representing higher usability. Based on several studies, Bangor et al. (2008) recommend that a SUS score above 70 can be considered adequate. Hence, we consider a SUS-score of 70 or more to be suitable. We translated the SUS into Dutch using forward- and blind backward-translation. The CASPAR study will be the first study to use this translated questionnaire.
Satisfaction with the mobile applications is measured with the Client Satisfaction Questionnaire-8 (CSQ-8) (Larsen et al., 1979). The CSQ is a standardised measure consisting of 8 questions to assess the patient's perspective on client satisfaction with the service. This questionnaire has good psychometric properties (Attkisson and Zwick, 1982; Nguyen et al., 1983). We will use the Dutch version of the Client Satisfaction Questionnaire-8 (CSQ-8), translated from English by de Brey (1983). The items can be answered on a scale from 1 to 4, with a total score on a range from 8 to 32. We consider a score of 20 or higher to be acceptable.
Uptake is operationalised as: 1) 75% of the patients complete the safety plan which is measured by retrospective questions; 2) 75% of the patients complete at least 50% of the self-monitoring questions during the second and third month of the study measured by analyses of the EMA data, and 3) 75% of the patients discuss the safety plan and self-monitoring at least once every two weeks with their clinician, measured by clinician feedback.
2.5. Outcome measures of part 2: fundamental research
The primary outcome measure of part 2 is the level of explorative power of the IMV model.(O'Connor, 2011) The secondary outcomes are to determine pathways to suicidal behaviour and to determine subtypes of suicidal individuals. To assess these three outcomes we have operationalised the phases and corresponding constructs described within the IMV model (Fig. 1), using both full scale questionnaires and single items selected from questionnaires (see Appendix 1 for the single items).
The pre-motivational phase of the IMV model, which consists of background factors and triggering events, is assessed by demographic questions. Anxiety is measured with the GAD-7, a self-report questionnaire with good psychometric properties.(Spitzer et al., 2006) The GAD-7 has 7 items (e.g. “Feeling nervous, anxious or on edge”) which are rated on a 4-point scale ranging from 0 (not at all) to 3 (nearly every day). Depression is measured with the Patient Health Questionnaire-9 (PHQ-9), a self-report questionnaire of 9 items (e.g. “Feeling down, depressed, or hopeless”) to measure depression severity on a 4-point scale ranging from 0 (not at all) to 3 (nearly every day). The PHQ-9 has adequate psychometric properties (Kroenke et al., 2001).
The motivational phase of the IMV model represents the formation of suicidal ideation and intent. Suicidal ideation and intent are measured with items from the Beck Scale for Suicide Ideation (BSS) (Beck et al., 1988). Feelings of defeat and entrapment are measured with the Short Defeat and Entrapment Scale (SDES). The SDES has 8 items (e.g. “I feel defeated by life”) which are rated on a 5-point scale ranging from 0 (not at all) to 4 (extremely like me). The psychometric properties of the SDES are adequate (Griffiths et al., 2015).The SDES was translated into Dutch by using forward-translation (translated and discussed by two independent health professionals) and blind backward-translation (by an independent translator whose primarily language is English).
The volitional phase of the IMV model covers behavioural enaction. Suicidal behaviour is assessed with questions from the Self-Injurious Thoughts and Behaviours Interview (SITBI). The SITBI assesses multiple suicide-related constructs, including recent and past suicidal ideation, plans, gestures and attempts. In its original form, the SITBI is a structured interview with good psychometric properties (Nock et al., 2007). For the CASPAR study, questions were selected and translated into Dutch using forward- and blind backward-translation. We adapted the interview questions into self-report questions.
The different phases of the IMV model contain multiple moderators, which are operationalised in the CASPAR study as well. Threat to self moderators are assessed via several questionnaires. Ruminative processes are assessed with single items originating from the GAD-7 (Spitzer et al., 2006) and the Ruminative Responses Scale (RRS) which is a self-report measure of rumination (Treynor et al., 2003). Coping, another threat to self moderator, is measured with items from the Utrechtse Coping Lijst (UCL). The UCL is a self-report questionnaire to assess people's coping strategies (Schreurs et al., 1984).
Motivational moderators within the IMV model are assessed with various questionnaires. Interpersonal needs are assessed with the self-report Interpersonal Needs Questionnaire-12 (INQ-12). The INQ-12 contains 12 items (e.g. “These days the people in my life would be better off if I were gone”) rated on a 7-point scale ranging from 1 (not at all true for me) to 7 (very true for me) and has good psychometric properties (Van Orden et al., 2008; Freedenthal et al., 2011). This questionnaire was translated into Dutch by 113 Suicide Prevention (the Dutch national suicide helpline) using forward- and backward-translation. One item from the Brief Resilience Scale (BRS) (Smith et al., 2008) is used to measure resilience and multiple items of the Reasons for Living Inventory (RFL-A) (Osman et al., 1998) are used to assess future thoughts. These items were translated into Dutch by using forward- and backward-translation.
Some of the volitional moderators are assessed with the Acquired Capability for Suicide Scale (ACSS), a self-report questionnaire. The ACSS is a 5-item measure (e.g. “I am not at all afraid to die”) with adequate psychometric properties to assess fearlessness about lethal self-injury (Ribeiro et al., 2014). Items are rated on a 5-point scale ranging from 0 (not at all like me) to 4 (very much like me). The ACSS was translated into Dutch by 113 Suicide Prevention using forward- and blind backward-translation. Impulsivity is another volitional moderator, measured with the Urgency, Premeditation, Perseverance, Sensation seeking, Positive Urgency Impulsive Behaviour Scale (UPPS-P) (Cyders et al., 2007). Suicide-related mental imagery is seen as a volitional moderator. The CASPAR study assessed imagery with items from the Social cognitions and Flash-forwards Interview (Imagery Interview) (Holmes et al., 2007). The Imagery Interview and the UPPS-P have been translated into Dutch using forward- and backward-translation.
The CASPAR study will be the first study to use the above mentioned translated questionnaires.
2.6. Interventions
The CASPAR study will investigate two mobile applications: safety planning and daily self-monitoring. For the safety planning app we will use BackUp. This app has been developed by the Vlaams Expertisecentrum Suïcidepreventie (VLESP) for use in Flanders, Belgium. A version for use in the Netherlands, with minor changes regarding the interface, has been developed in collaboration with 113 Suicide Prevention. The safety plan in BackUp is based on Stanley and Brown's Safety Planning Intervention (Stanley and Brown, 2012), and it contains the same 6 steps as the original safety plan (e.g. warning signs, internal coping strategies, distracting activities, social support, contacting mental health professionals, making the environment safe).
For the self-monitoring app we will use the mEMA app, which had been developed by Ilumivu (https://ilumivu.com/). The mEMA app will monitor suicidal processes by daily repeated self-report questions prompted by ‘beeps’ at random moments. The mEMA app computes a graph of all variables through time, which is visible to the patient. At the beginning of the study we will present 8 items to the patient at 3 random intervals a day. In addition to these assessments, the patients are prompted to complete an evening list consisting of 8 items. Based on feedback from patients we will adapt the self-monitoring questions, the number of questions at each beep and the number of beeps.
We chose the self-monitoring questions based on constructs mentioned within the IMV model. For each construct we selected established retrospective questionnaires that assess the constructs (see Section 2.5. Outcome measures of part 2: fundamental research) and we re-wrote the question in a more immediate (momentary) form. For example, the Generalized Anxiety Disorder-7 is a questionnaire which assesses anxiety symptoms in the last two weeks. The item ‘Being so restless that it's hard to sit still’ had been re-written for the CASPAR study as ‘I feel restless’ to make the item more assessable in real time.
mEMA will also gather unobtrusive measures that will accumulate automatically on the patient's mobile phone. Every self-monitoring assessment will include location data based on GPS, if has been activated by the patient. Accelerometer data is also collected continuously.
2.7. Design
The CASPAR study is a single cohort design among patients from three mental health centres. There will be three measurement points: T0 (baseline), T1 (one month after T0) and T2 (three months after T0). We consider this study to be an adaptive design, which means that the two apps that we investigate will be improved based on patient feedback. As a result, the apps may change slightly during the study.
2.8. Procedure
Clinicians from the participating mental health organisations will be invited to participate in the CASPAR study. Participating clinicians will receive training from the researchers on using both the safety planning app and self-monitoring app add-ons in regular treatment with their patients. Participating clinicians will select patients from their caseload based on the inclusion criteria and the clinician's experience with the patient. The clinician will then invite the patient to participate in the CASPAR study and provide them with further information. CASPAR is additional to regular treatment and it will be made clear that non-participation will have no negative consequences for patients.
If the patient is willing to participate, the researchers will invite the patient for the first measurement session (baseline; T0) in a face-to-face meeting. The patient will sign the informed consent form and answer 5 questionnaires (i.e. ACSS, GAD-7, INQ-12, PHQ-9 and SDES) and multiple single items from questionnaires (i.e. BRS, BSS, Imagery Interview, RFL-A, RRS, SITBI, UCL and UPPS-P). Furthermore, the researcher will install both the BackUp app and the mEMA app on the patient's smartphone and explain both apps in detail. The patient starts using the apps after T0. The mEMA app will prompt the patient to answer multiple self-monitoring questions throughout the day. The patient and clinician will complete the BackUp safety plan in the first (clinical) session after T0, from that moment on the patient can use the BackUp app if necessary. Both these apps will be used during the patient's regular treatment. For example, the mEMA graph of the self-monitoring questions the patient has filled in can be used to discuss the patient's symptoms and subsequently be added to the safety plan on the BackUp app.
One month after T0 a researcher will contact the patient by phone for general feedback on the apps. The researcher will send the second measurement questions (T1) to the patient via an online survey tool. The patient is invited to answer the same questionnaires as at T0, and two additional questionnaires related to the feasibility endpoints (i.e. CSQ and SUS). After completing T1, the patient will continue to use both apps and they will be used in treatment.
Three months after baseline (T2) the researcher will contact the patient again by phone for general feedback on the apps. The patient will be invited to answer the same questions as at T1, which the researcher will send via the online survey tool. After completing T2, the patient and clinician will decide whether to keep using the apps (either or both). If the patient wants to stop using the apps, or when the patient is discharged from treatment, the clinician will assist in uninstalling the apps from the patient's smartphone.
2.9. Incentives
Patients will receive Bol.com discount codes worth 5 Euro after every completed measurement point (i.e. T0, T1, T2), as well as when they have completed over 60% of the self-report questions between T0 and T1. Patients can receive a maximum of 20 Euro for participation.
2.10. Analyses (statistical methods)
The primary outcomes are feasibility measures, i.e. uptake, patient satisfaction and usability, and will be presented using descriptive statistics. For the secondary outcome measures we will analyse the self-monitoring data. Our approach to validating psychological processes and stages of suicide pathways as outlined by the IMV model of O'Connor (2011) is a structural equation model. The IMV model postulates phases, variables per phase, temporal relations and moderated relations between variables. We will test these hypothesised relations until we find the optimal model. Because the self-monitoring data consist of time-series data with irregular intervals between measurement points, we will apply continuous time modelling (e.g. Ryan et al. (submitted)), in which time is viewed as a continuous variable. This modelling technique is robust for different intervals between measurement points, as well as for missing data.
For identifying individual pathways to suicidal behaviour, we will focus on both the individual and subgroup level. We will conduct a longitudinal network analysis applying vector-autoregression (VAR; e.g. Basu et al. (2012)). Temporal networks of subgroups will be analysed using multilevel VAR. Finally, latent class growth analyses (van de Schoot, 2015) will be conducted to identify subgroups based on variable trajectories over time. Analyses will be carried out in R, using various packages such as lavaan, ctsem, mlVAR and bootnet.
3. Discussion
The CASPAR study combines practice-based research with fundamental research in order to enhance suicide prevention methods and theories targeting the transition phase from suicidal thinking to suicidal behaviour. With this two-fold study we aim to contribute to the field of suicide prevention and mobile health in the following ways. First, we will assess the feasibility of integrating mobile health interventions (i.e. safety planning and self-monitoring) into the routine care and treatment of suicidal patients. Second, central constructs of suicidality will be assessed at a symptom level and in real-time, hereby providing insight into the mental health of suicidal patients. While patients can use these data for self-monitoring and self-management, clinicians can use this information directly in treatment. We assume that the combination of a mobile safety plan and daily self-monitoring will lead to a decrease in suicidal symptoms, and ultimately to fewer suicide attempts (although this is beyond the scope of the present study). Third, analyses of the EMA data will be used to enhance current knowledge of the suicidal process, especially regarding the transition from suicidal ideation to behaviour. This will help in the identification and treatment of individuals who are at risk of acting on their thoughts of suicide.
If the use of applications is feasible for patients, the next step would be to combine mobile safety-planning and self-monitoring apps. It could be possible to trigger the safety plan app based on self-monitoring answers. Such an intervention is called an ecological momentary intervention (EMI) (Schueller et al., 2017). EMIs are able to make use of information about the user and their related environment, by gathering self-monitoring data (EMA), in order to optimise the intervention delivery. In this way it becomes possible for EMIs to provide support to patients when they need it the most. With the rapidly changing nature of suicidality, patients are likely to benefit from this kind of intervention.
4. Conclusion
This paper describes the study protocol of the CASPAR study. The CASPAR study is designed to evaluate the feasibility of safety planning and self-monitoring in the treatment of suicidal patients. Furthermore, the CASPAR study will apply basic science methods to advance understanding of dynamic suicidal processes thereby increasing knowledge of the proximal risk factors of suicidality.
Trial status
At the time of the revised manuscript submission, the study is in a preparatory phase. The protocol is under revision for approval by the medical ethics board of the Vrije Universiteit Medical center (METc number: 2017.512/NL62795.029.17). The first patients are expected to be included in August 2018.
Conflict of interests
The authors declare that they have no competing interests.
Funding
The CASPAR study is funded by the Netherlands organisation for health research and development (ZonMw project number 537001008). The funding body has no influence on the study whatsoever.
Acknowledgements
The study will be part of the doctoral thesis of CN.
Appendix A. Single item questions
| Nr. | Item | |
|---|---|---|
| RFL-A | 4 | I have a desire to live. |
| 13 | I have future plans I am looking forward to carrying out | |
| 40 | I have hope that things will improve and the future will be happier | |
| BRS | 5 | Tend to bounce back after illness or hardship |
| UCL | 10 | I can discuss my concerns with someone |
| 46 | I do not feel able to do anything | |
| UPPS | 2 | I have trouble controlling my impulses. |
| 48 | I usually think carefully before doing anything. | |
| RRS | 12 | I think about a recent event of which I wish it had gone better |
| 24 | I think ‘What am I doing to deserve this?’ | |
| BSS | 4 | I have the desire to make kill myself |
| 12 | I have a specific plan how I can to kill myself | |
| SITBI-SF | 2 | How old were you the first time you had thoughts of killing yourself? |
| 4 | During how many separate times in your life have you had thoughts of killing yourself? | |
| 5 | How many separate times in the past year? | |
| 6 | How many separate times in the past month? | |
| 7 | How many separate times in the past week? | |
| 8 | When was the last time? | |
| 9 | On this scale of 0 to 4, at the worst point how intense were your thoughts of killing yourself? | |
| 10 | On average, how intense were these thoughts? | |
| 14 | Have you ever actually made a plan to kill yourself? | |
| 22 | On average, how seriously have you considered acting on them? | |
| 23 | When you've had a plan, what method did you think of using? | |
| 36 | Have you ever made an actual attempt to kill yourself in which you had at least some intent to die? | |
| 37 | How old were you the first time you made a suicide attempt? | |
| 38 | When was the most recent attempt? | |
| 40 | How many suicide attempts have you made in your lifetime? | |
| 41 | How many have you made in the past year? | |
| 42 | How many have you made in the past month? | |
| 43 | How many have you made in the past week? | |
| 44 | What method did you use for your most recent attempt? | |
| 50 | On the scale of 0 to 4, what do you think the likelihood is that you will make a suicide attempt in the future? |
References
- Aaron L.A., Mancl L., Turner J.A., Sawchuk C.N., Klein K.M. Reasons for missing interviews in the daily electronic assessment of pain, mood, and stress. Pain. 2004;109(3):389–398. doi: 10.1016/j.pain.2004.02.014. [DOI] [PubMed] [Google Scholar]
- Aguirre R.T.P., McCoy M.K., Roan M. Development guidelines from a study of suicide prevention mobile applications (apps) J. Technol. Hum. Serv. 2013;31(3):269–293. [Google Scholar]
- Ajzen I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991;50(2):179–211. [Google Scholar]
- Attkisson C.C., Zwick R. The client satisfaction questionnaire. Psychometric properties and correlations with service utilization and psychotherapy outcome. Eval. Program Plann. 1982;5(3):233–237. doi: 10.1016/0149-7189(82)90074-x. [DOI] [PubMed] [Google Scholar]
- Bangor A., Kortum P.T., Miller J.T. An empirical evaluation of the system usability scale. Int. J. Hum. Comput. Interact. 2008;24(6):574–594. [Google Scholar]
- Basu S., Shojaie A., Michailidis G. Vol. 16. 2012. Network Granger Causality With Inherent Grouping Structure; pp. 417–453.http://arxiv.org/abs/1210.3711 [PMC free article] [PubMed] [Google Scholar]
- Baumeister R.F. Suicide as escape from self. Psychol. Rev. 1990;97(1):90–113. doi: 10.1037/0033-295x.97.1.90. http://www.ncbi.nlm.nih.gov/pubmed/2408091 [DOI] [PubMed] [Google Scholar]
- Beck A.T., Steer R.A., Ranieri W.F. Scale for suicide ideation: psychometric properties of a self-report version. J. Clin. Psychol. 1988;44(4):499–505. doi: 10.1002/1097-4679(198807)44:4<499::aid-jclp2270440404>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- de Beurs D., Kirtley O., Kerkhof A., Portzky G., O'Connor R.C. The role of mobile phone Technology in understanding and preventing suicidal behavior. Crisis. 2015;36(2):79–82. doi: 10.1027/0227-5910/a000316. [DOI] [PubMed] [Google Scholar]
- de Brey H. A cross-national validation of the client satisfaction questionnaire: the Dutch experience. Eval. Program Plann. 1983;6(3–4):395–400. doi: 10.1016/0149-7189(83)90018-6. [DOI] [PubMed] [Google Scholar]
- Brooke J. SUS: a quick and dirty usability scale. Usebility Eval Ind. 1996;189(194):4–7. [Google Scholar]
- Bryan C.J., Mintz J., Clemans T.A. Effect of crisis response planning vs. contracts for safety on suicide risk in U.S. army soldiers: a randomized clinical trial. J. Affect. Disord. 2017;212(October 2016):64–72. doi: 10.1016/j.jad.2017.01.028. [DOI] [PubMed] [Google Scholar]
- Cyders M.A., Smith G.T., Spillane N.S., Fischer S., Annus A.M., Peterson C. Integration of impulsivity and positive mood to predict risky behavior: development and validation of a measure of positive urgency. Psychol. Assess. 2007;19(1):107–118. doi: 10.1037/1040-3590.19.1.107. [DOI] [PubMed] [Google Scholar]
- van de Schoot R. Latent trajectory studies: the basics, how to interpret the results, and what to report. Eur. J. Psychotraumatol. 2015;6(1) doi: 10.3402/ejpt.v6.27514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eynan R., Bergmans Y., Antony J. The effects of suicide ideation assessments on urges to self-harm and suicide. Crisis. 2014;35(2):123–131. doi: 10.1027/0227-5910/a000233. [DOI] [PubMed] [Google Scholar]
- Franklin J.C., Ribeiro J.D., Fox K.R. Risk factors for suicidal thoughts and behaviors: a meta-analysis of 50 years of research. Psychol. Bull. 2016;143(2):187–232. doi: 10.1037/bul0000084. [DOI] [PubMed] [Google Scholar]
- Freedenthal S., Lamis D.A., Osman A., Kahlo D., Gutierrez P.M. Evaluation of the psychometric properties of the interpersonal needs Questionnaire-12 in samples of men and women. J. Clin. Psychol. 2011;67(6):609–623. doi: 10.1002/jclp.20782. [DOI] [PubMed] [Google Scholar]
- Freedman M.J., Lester K.M., McNamara C., Milby J.B., Schumacher J.E. Cell phones for ecological momentary assessment with cocaine-addicted homeless patients in treatment. J. Subst. Abus. Treat. 2006;30(2):105–111. doi: 10.1016/j.jsat.2005.10.005. [DOI] [PubMed] [Google Scholar]
- Griffiths A.W., Wood A.M., Maltby J., Taylor P.J., Panagioti M., Tai S. The development of the short defeat and entrapment scale (SDES) Psychol. Assess. 2015;27(4):1182–1194. doi: 10.1037/pas0000110. [DOI] [PubMed] [Google Scholar]
- Groot P.C. Patients can diagnose too: how continuous self-assessment aids diagnosis of, and recovery from, depression. J. Ment. Health. 2010;19(4):352–362. doi: 10.3109/09638237.2010.494188. [DOI] [PubMed] [Google Scholar]
- Hogan M.F. Better suicide screening and prevention are possible. JAMA Psychiat. 2016;73(11):1111–1112. doi: 10.1001/jamapsychiatry.2016.2411. [DOI] [PubMed] [Google Scholar]
- Holmes E.A., Crane C., Fennell M.J.V., Williams J.M.G. Imagery about suicide in depression—“flash-forwards”? J. Behav. Ther. Exp. Psychiatry. 2007;38(4):423–434. doi: 10.1016/j.jbtep.2007.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., Ghaderi A., Harmer C.J. The Lancet Psychiatry Commission on psychological treatments research in tomorrow's science. Lancet Psychiatry. 2018;5(3):237–286. doi: 10.1016/S2215-0366(17)30513-8. [DOI] [PubMed] [Google Scholar]
- Husky M., Olié E., Guillaume S., Genty C., Swendsen J., Courtet P. Feasibility and validity of ecological momentary assessment in the investigation of suicide risk. Psychiatry Res. 2014;220(1–2):564–570. doi: 10.1016/j.psychres.2014.08.019. [DOI] [PubMed] [Google Scholar]
- JMG Williams. Penguin; London: 2001. Suicide and Attempted Suicide: Understanding the Cry of Pain. [Google Scholar]
- Joiner T.E., Jr. Harvard University Press; Cambridge, MA: 2005. Why People Die by Suicide. [Google Scholar]
- Kennard B.D., Biernesser C., Wolfe K.L. Developing a brief suicide prevention intervention and mobile phone application: a qualitative report. J. Technol. Hum. Serv. 2015;33(4):345–357. doi: 10.1080/15228835.2015.1106384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleiman E.M., Turner B.J., Fedor S., Beale E.E., Huffman J.C., Nock M.K. Examination of real-time fluctuations in suicidal ideation and its risk factors: results from two ecological momentary assessment studies. J. Abnorm. Psychol. 2017;126(6):726–738. doi: 10.1037/abn0000273. (May) [DOI] [PubMed] [Google Scholar]
- Klonsky E.D., May A.M., Saffer B.Y. Suicide, suicide attempts, and suicidal ideation. Annu. Rev. Clin. Psychol. 2016;12(1):307–330. doi: 10.1146/annurev-clinpsy-021815-093204. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen D.L., Attkisson C.C., Hargreaves W.A., Nguyen T.D. Assessment of client/patient satisfaction: development of a general scale. Eval. Program Plann. 1979;2(3):197–207. doi: 10.1016/0149-7189(79)90094-6. [DOI] [PubMed] [Google Scholar]
- Larsen M.E., Nicholas J., Christensen H.A. Systematic assessment of smartphone tools for suicide prevention. Seedat S, ed. PLoS One. 2016;11(4) doi: 10.1371/journal.pone.0152285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mars B., Heron J., Klonsky E.D. What distinguishes adolescents with suicidal thoughts from those who have attempted suicide? A population-based birth cohort study. J. Child Psychol. Psychiatry. 2018 doi: 10.1111/jcpp.12878. (March) (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- May A.M., Klonsky E.D. What distinguishes suicide attempters from suicide ideators? A meta-analysis of potential factors. Clin. Psychol. Sci. Pract. 2016;23(1):5–20. [Google Scholar]
- Myin-Germeys I., Oorschot M., Collip D., Lataster J., Delespaul P., van Os J. Experience sampling research in psychopathology: opening the black box of daily life. Psychol. Med. 2009;39(9):1533. doi: 10.1017/S0033291708004947. [DOI] [PubMed] [Google Scholar]
- Nguyen T.D., Attkisson C.C., Stegner B.L. Assessment of patient satisfaction: development and refinement of a service evaluation questionnaire. Eval. Program Plann. 1983;6(3–4):299–313. doi: 10.1016/0149-7189(83)90010-1. [DOI] [PubMed] [Google Scholar]
- Nock M.K., Holmberg E.B., Photos V.I., Michel B.D. Self-injurious thoughts and behaviors interview: development, reliability, and validity in an adolescent sample. Psychol. Assess. 2007;19(3):309–317. doi: 10.1037/1040-3590.19.3.309. [DOI] [PubMed] [Google Scholar]
- Nock M.K., Borges G., Bromet E.J., Cha C.B., Kessler R.C., Lee S. Suicide and suicidal behavior. Epidemiol. Rev. 2008;30(1):133–154. doi: 10.1093/epirev/mxn002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock M.K., Prinstein M.J., Sterba S.K. Revealing the form and function of self-injurious thoughts and behaviors: a real-time ecological assessment study among adolescents and young adults. J. Abnorm. Psychol. 2009;118(4):816–827. doi: 10.1037/a0016948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connor R.C. Towards an integrated motivational-volitional model of suicidal behaviour. In: O'Connor R.C., Platt S., Gordon J., editors. International Handbook of Suicide Prevention: Research, Policy and Practice. Wiley-Blackwell; Chichester, UK: 2011. pp. 181–198. [Google Scholar]
- O'Connor R.C., Kirtley O.J. The integrated motivational-volitional model of suicidal behaviour. Philos. Trans. R. Soc. B. 2018 doi: 10.1098/rstb.2017.0268. (In press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connor R.C., Nock M.K. The psychology of suicidal behaviour. Lancet Psychiatry. 2014;1(1):73–85. doi: 10.1016/S2215-0366(14)70222-6. [DOI] [PubMed] [Google Scholar]
- Osman A., Downs W.R., Kopper B.A. The reasons for living inventory for adolescents (RFL-A): development and psychometric properties. J. Clin. Psychol. 1998;54(8):1063–1078. doi: 10.1002/(sici)1097-4679(199812)54:8<1063::aid-jclp6>3.0.co;2-z. http://www.ncbi.nlm.nih.gov/pubmed/9840778 [DOI] [PubMed] [Google Scholar]
- Pearson J.L., Stanley B., King C.A., Fisher C.B. Intervention research with persons at high risk for suicidality: safety and ethical considerations. J. Clin. Psychiatry. 2001;62(25):17–26. http://www.ncbi.nlm.nih.gov/pubmed/11765091 [PubMed] [Google Scholar]
- Ribeiro J.D., Joiner T.E. The interpersonal-psychological theory of suicidal behavior: current status and future directions. J. Clin. Psychol. 2009;65(12):1291–1299. doi: 10.1002/jclp.20621. [DOI] [PubMed] [Google Scholar]
- Ribeiro J.D., Witte T.K., Van Orden K.A. Fearlessness about death: the psychometric properties and construct validity of the revision to the acquired capability for suicide scale. Psychol. Assess. 2014;26(1):115–126. doi: 10.1037/a0034858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd M.D., Mandrusiak M., Joiner T.E., Jr. The case against no-suicide contracts: the commitment to treatment statement as a practice alternative. J. Clin. Psychol. 2006;62(2):243–251. doi: 10.1002/jclp.20227. [DOI] [PubMed] [Google Scholar]
- Ryan O., Kuiper R.M., Hamaker E.L. 2018. A continuous time approach to intensive longitudinal data: What, Why and How? Submitted. (Pre-print available on request) [Google Scholar]
- Schotte D.E., Clum G.A. Problem-solving skills in suicidal psychiatric patients. J. Consult. Clin. Psychol. 1987;55(1):49–54. doi: 10.1037//0022-006x.55.1.49. [DOI] [PubMed] [Google Scholar]
- Schreurs P.J.G., Tellegen B., van de Willige G. Gezondheid, stress en coping: de ontwikkeling van de Utrechtse Coping Lijst. Gedrag Tijdschr voor Psychol. 1984;12:101–117. [Google Scholar]
- Schrimsher G., Filtz K. Assessment reactivity: can assessment of alcohol use during research be an active treatment? Alcohol. Treat. Q. 2011;29(2):108–115. [Google Scholar]
- Schueller S.M., Aguilera A., Mohr D.C. Ecological momentary interventions for depression and anxiety. Depress. Anxiety. 2017;(April):1–6. doi: 10.1002/da.22649. [DOI] [PubMed] [Google Scholar]
- Shiffman S., Stone A.A., Hufford M.R. Ecological momentary assessment. Annu. Rev. Clin. Psychol. 2008;4(November 2007):1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- Smith B.W., Dalen J., Wiggins K., Tooley E., Christopher P., Bernard J. The brief resilience scale: assessing the ability to bounce back. Int. J. Behav. Med. 2008;15(3):194–200. doi: 10.1080/10705500802222972. [DOI] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A brief measure for assessing generalized anxiety disorder. Arch. Intern. Med. 2006;166(10):1092. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Stanley B., Brown G.K. Washington; DC United States Dep Veteran Aff: 2008. Safety Plan Treatment Manual to Reduce Suicide Risk: Veteran Version. [Google Scholar]
- Stanley B., Brown G.K. Safety planning intervention: a brief intervention to mitigate suicide risk. Cogn. Behav. Pract. 2012;19(2):256–264. [Google Scholar]
- Stanley B., Brown G., Brent D.A. Cognitive-behavioral therapy for suicide prevention (CBT-SP): treatment model, feasibility, and acceptability. J. Am. Acad. Child Adolesc. Psychiatry. 2009;48(10):1005–1013. doi: 10.1097/CHI.0b013e3181b5dbfe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone A.A., Shiffman S. Ecological momentary assessment (EMA) in behavioral medicine. Ann. Behav. Med. 1994;16(3):199–202. [Google Scholar]
- Treynor W., Gonzalez R., Nolen-Hoeksema S. Rumination reconsidered: a psychometric analysis. Cogn. Ther. Res. 2003;27(3):247–259. [Google Scholar]
- Van Hemert A.M., Kerkhof A.J.F.M., De Keijser J. 2012. Multidisciplinaire Richtlijn Diagnostiek En Behandeling van Suïcidaal Gedrag. [Google Scholar]
- Van Orden K.A., Witte T.K., Gordon K.H., Bender T.W., Joiner T.E. Suicidal desire and the capability for suicide: tests of the interpersonal-psychological theory of suicidal behavior among adults. J. Consult. Clin. Psychol. 2008;76(1):72–83. doi: 10.1037/0022-006X.76.1.72. [DOI] [PubMed] [Google Scholar]
- Viechtbauer W., Smits L., Kotz D. A simple formula for the calculation of sample size in pilot studies. J. Clin. Epidemiol. 2015;68(11):1375–1379. doi: 10.1016/j.jclinepi.2015.04.014. [DOI] [PubMed] [Google Scholar]
- World Health Organization . 2014. Preventing Suicide: A Global Imperative. [Google Scholar]