Abstract
To further improve treatments, we need to better understand potential common treatment mechanisms, such as decentering, or the ability to observe thoughts and feelings as objective events in the mind rather than personally identifying with them (Safran & Segal, 1990). Therefore, this study examined whether 12-sessions of Cognitive Behavioral Group Therapy for 81 clients (57.6% female, 50.8% White) diagnosed with social anxiety disorder led to increases in decentering and whether increased decentering was associated with improved outcome. Furthermore, this study examined whether decentering was associated with outcome over and above a competing mechanism - cognitive reappraisal. Overall, results indicated that CBGT in this study led to similar outcomes compared to previous studies and decentering increased over CBGT (d’s from 0.81 to 2.23). Change in decentering predicted improvement on most, but not all measures of outcome and those who no longer met criteria for social anxiety disorder at post-treatment had significantly greater change in decentering across therapy and significantly higher decentering scores at post-treatment compared to those who retained a social anxiety disorder diagnosis at post-treatment. Finally, changes in decentering predicted outcome over and above change reappraisal on all outcome measures. These results largely support the role of decentering in CBGT for social anxiety; however, the implications of the inconsistencies in results based on which outcome measure was used are discussed.
Keywords: decentering, mechanisms of action, cognitive behavioral group therapy, social anxiety
Approximately 12.1% of the United States population suffers from clinically significant social anxiety during their lifetime (Kessler, Chiu, Demler, & Waters, 2005). Studies indicate that social anxiety disorder (SAD), characterized by a persistent fear or anxiety in social or performance situations (DSM-5; American Psychiatric Association, 2013), is associated with vocational and social difficulties, higher rates of outpatient medical treatment, suicidality, financial dependency, psychiatric comorbidity, and lower wages than those without social anxiety (Katzelnick et al., 2001; Schneier et al., 1992; Schneier et al., 1994).
While SAD has a high prevalence rate, psychotherapies, particularly cognitive and behavioral therapies (CBT), have been shown to be efficacious in reducing symptoms of SAD. For example, five meta-analyses examining the relative efficacy of cognitive-behavioral techniques for SAD have shown that CBT significantly improved symptoms compared to a wait-list, with mean effect sizes for CBT ranging from 0.74 to 1.06 and from −0.13 to 0.03 for wait-list (Acarturk, Cuijpers, van Straten, & de Graaf, 2009; Fedoroff & Taylor, 2001; Feske & Chambless, 1995; Gould et al., 1997; Taylor, 1996). Additionally, one of the classic and most frequently studied treatments for SAD, Heimberg’s Cognitive Behavioral Group Treatment (CBGT; Heimberg, 1991; Heimberg & Becker, 2002), which combines Beckian style cognitive restructuring with in-session and between-session exposures, has been shown to be more effective than wait-list control (Hope, Heimberg, & Bruch, 1995), and equally as effective as the monoamine oxidase inhibitor phenelzine (Heimberg et al., 1998). At a five-year follow-up, clients who went through CBGT were more likely to have maintained or improved than were clients from the control group (Heimberg, Salzman, Holt, & Blendell, 1993). Within-group effect sizes for CBGT range from 0.84 to 1.13 (Heimberg, 2002).
However, CBGT is not the only efficacious treatment for SAD1. For example, CBGT has been shown to have comparable efficacy to a mindfulness and acceptance-based group therapy (MAGT: Kocovski, Fleming, Hawley, & Antony, 2013), with effect sizes of 1.02 for CBGT and 1.00 for MAGT. Findings from a systematic review indicate that mindfulness and acceptance-based treatments may be efficacious treatments for SAD with pre- to post-treatment changes in social anxiety ranging from ds of 0.32 to 1.24 and η2ps from 0.41 to 1.54 (Norton, Abbott, Norberg, & Hunt, 2015). The comparable effect sizes for MAGT and CBGT may indicate a common mechanism between the two therapies is at least partially contributing to change. There is a particular need to better understand the mechanism that cut across behavioral treatments to further improve upon our current treatments (Arch & Craske, 2008; Castonguay, 2011; Mennin et al., 2013; Orsillo, Roemer, Block Lerner, & Tull, 2004; Kazdin, 2007).
Decentering as a Potential Mechanism
Decentering, or the ability to observe thoughts and feelings as objective events in the mind, rather than personally identifying with them (Safran & Segal, 1990), has been hypothesized as a mechanism of action in both CBT (Beck et al., 1979; Teasdale, 1999) and acceptance and mindfulness based therapies (AMBT) (Bishop et al., 2004). According to the metacognitive processes model of decentering (Bernstein et al., 2015), decentering involves meta-awareness, disidentification from internal experiences, and reduced reactivity to thought content. In other words, decentering involves a meta-awareness where the focus is on observing thoughts or the thinking process rather than a focus on the content of the thought. This allows for a disidentification from internal experiences where the thought or other internal state is separate from one’s self as the act of observing one’s internal process naturally leads to disidentification from it. Similarly, meta-awareness also directs attention to the present moment which shifts attention away from the content of the thought. This shift away from the content of the thought reduces emotional reactivity. The metacognitive processes model of decentering also applies to other closely related to distancing processes such as meta-cognitive awareness (Teasdale et al., 2002). Of note, decentering also shares some conceptual overlap (i.e., reduced emotional reactivity) with the related construct of defusion (see Bernstein et al., 2015); however, they also appear to differ in that decentering, but not defusion may also involve the disidentification from internal experiences. These conceptual differences appear to be supported in a factor analysis of measures of decentering and defusion (Naragon-Gainey & DeMarree, 2017).
Decentering in social anxiety
Theories on the development of social anxiety disorder indicate that social anxiety may be maintained through biased and fused attention processes. Building on prominent models of social anxiety (see Clark & Wells, 1995; Herbert & Cardaciotto, 2005; Rapee & Heimberg, 1997). Individuals with social anxiety may experience an external threat attention bias, which may lead to cognitive fusion. When fused, the negatively biased thoughts are believed to be true and therefore the individual is not decentered. This lack of decentering may then result in increased behavioral avoidance and reduced opportunities for new learning that social situations may not be dangerous. In support of this theory, studies have shown that individuals with social anxiety are more likely to attend to external threat cues in the environment (Bar-Haim et al., 2007; Heinrichs & Hofmann, 2001; Mogg & Bradley, 2002), while also diverting attention away from positive cues (Taylor, Bomyea, & Amir, 2010), fostering a belief that a social situation is dangerous and should be avoided. There is also evidence that those with social anxiety have a difficulty disengaging from threat information (Amir, Elias, Klumpp, & Przeworski, 2003; Fox, Russo, Bowles, & Dutton, 2001). Combined, initial vigilance to threat and difficulty disengaging fosters a fused attention, where attention is rigidly focused only on threat cues, as opposed to the individual taking a more decentered perspective.
At the same time, there is support for the connection between self-focused attention and social anxiety (see Spurr & Stopa, 2002). For example, when engaged in self-focused attention, individuals with social anxiety experience excessively negative self-images, which they believe are accurate (Hackmann, Suraway, & Clark, 1998; Hofmann & Heinrichs, 2003). Further, intentionally manipulating increases in self-focused attention results in increased negative thoughts and subjective anxiety (Spurr & Stopa, 2003; Wells & Papageorgiou, 2001). In other words, individuals with social anxiety are experiencing fusion, the belief in and over-identification with the literal meaning of a thought or image, with their thoughts and images (Hayes, 2004; Herzberg et al., 2012). This fusion is consistent with Clark and Wells’ (1995) view that self-focused attention prevents the individual from noticing and incorporating objective feedback. Additionally, self-focused attention leads individuals to miss positive cues from their environment (Hirsch & Matthews, 2000). This is likely because attention resources are directed towards the fusion with the negative representations of self and are vigilantly examining the environment for threat, thus limiting the opportunities for new learning to disconfirm the negative representations of self. Given the strong connection between these biased and fused attention processes and social anxiety, reducing these biased attention processes through decentering should lead to a reduction of anxiety symptoms.
As further support for decentering in social anxiety disorder, theory highlights that decentering may address the cognitive and attention processes that maintain distress in general (e.g., Mennin et al., 2013). Experimental results have shown that taking a distanced perspective decreases distress (e.g., Davis, Gross, & Ochsner, 2011) and the believability of negative thoughts (e.g., Masuda et al., 2010). Decentering has also been shown to be related to decreased social anxiety symptoms (Hayes-Skelton & Graham, 2012) in a cross-sectional study. Decentering may provide this cognitive distancing by shifting the negative, self-focused attention biases characteristic of social anxiety. Thus, allowing individuals to disengage their attention from negative cues in the environment and in themselves. This then allows individuals to take a broader perspective, increasing opportunities for new learning (see Treanor, 2011), a key outcome of behavior therapies for social anxiety (Craske et al., 2008).
Decentering in Treatment
While acceptance and mindfulness-based therapies often target decentering directly, cognitive behavioral therapies have also been theorized as targeting decentering (see Segal, Williams, & Teasdale, 2013). For example, self-monitoring exercises, often used as part of CBTs, may lead to a cognitive distancing and disidentification from internal experiences of anxiety. Similarly, the process of cognitive restructuring where anxious thoughts are systematically identified and examined likely leads to decentering by providing a disidentification from the anxious thoughts (see Beck, 1979). For example, Bernstein et al. (2015) hypothesize that decentering may facilitate reappraisal by reducing the reactivity of the initial thought or by allowing for a different appraisal of one’s experience. Additionally, the distancing that decentering allows may enable new learning and new meaning making to take place in this context of expanded awareness, possible through cognitive reappraisal. Experimental evidence suggests that individuals who adopt a self-distancing perspective experience focus more on reconstructing the experience and experience less distress than those who adopt a self-immersed perspective (i.e., Kross & Ayduk, 2008, for a review see Kross & Ayduk, 2011). In this way, decentering through self-monitoring and cognitive restructuring exercises may allow clients to reconstruct their experiences from a broader perspective which may enhance insight and new learning.
Teatment studies have shown that decentering increases across both CBT (Fresco, Segal, Buis, & Kennedy, 2007) and Mindfulness-Based Cognitive Therapy (MBCT; Teasdale et al., 2002) for depression relapse prevention and changes in decentering predicted changes in symptoms of depression (Bieling et al., 2012). While one study found defusion to be a mediator of depression outcome in Acceptance and Commitment Therapy (ACT), but not CBT (Zettle, Rains, & Hayes, 2011), another showed that decentering mediated outcome in mindfulness-based stress reduction for generalized anxiety disorder (Hoge et al., 2015). Others have found evidence supporting the common mechanism hypothesis in that defusion mediated post-treatment worry and quality of life in CBT and ACT (Arch, Wolitzky-Taylor, Eifert, & Craske, 2012). To examine the time course of change in decentering, decentering was a leading indicator of symptom change for individuals receiving either applied relaxation or an acceptance-based behavior therapy for GAD, with no evidence for the reverse pattern (symptoms leading to decentering) being significant (Hayes-Skelton, Calloway, Roemer, & Orsillo, 2015). The literature has shown that decentering (or defusion) has been a mechanism of change across CBTs and acceptance-based treatments for depression, generalized anxiety, and mixed anxiety samples, the role of decentering has not been examined in relation to treatment for social anxiety.
The goal of the current study was to examine whether CBGT for social anxiety disorder, a cognitive and exposure-based treatment, leads to increases in decentering and whether increased decentering is associated with improved outcome. Furthermore, if decentering is a more universal mechanism of change, than we would expect changes in decentering to be associated with outcome, but also to lead to change over and above cognitive reappraisal, another hypothesized mechanism of change in this cognitive therapy.
Specifically, we hypothesized that: 1) CBGT in this study would lead to similar outcomes and response rates as previous studies, 2) decentering would increase over the course of CBGT, 3) increases in decentering would be associated with decreased symptoms, increased quality of life, and that treatment responders would have experienced more of an increase in decentering than nonresponders, and 4) that change in decentering would predict outcome over and above change in a competing mechanism (reappraisal).
Methods
Participants
We recruited 81 participants from an urban university and its surrounding community for this treatment study between 2012 and 2014, using emails, bus advertisements, and flyers advertising a study on treatment for social anxiety sent to the campus and surrounding community. Potential participants were referred to this study if they received a principal diagnosis of SAD on a semi-structured intake diagnostic interview (Anxiety Disorders Interview Scheduled for DSM-IV, ADIS-IV, Brown, DiNardo & Barlow, 1994). Inclusion criteria were: a principal diagnosis of SAD on the ADIS-IV with at least moderate severity (score of 4) on the Clinician’s Severity Rating; b) being stable on medications for three months, or one month for benzodiazepines; c) being willing to maintain current psychotropic medication levels and to refrain from other psychosocial treatments for anxiety or mood problems during the course of therapy; d) fluent in English; and e) 18 years or older. Participants were included even if they had comorbid diagnoses. Participants were excluded if they exhibited symptoms that require more immediate attention such as psychotic symptoms, active suicidal intent, bipolar disorder, or substance dependence. Independent assessors conducting the diagnostic assessment assessed eligibility, and a study therapist confirmed inclusion and exclusion criteria.
The participant flowchart (Figure 1) shows the number of participants at each stage. We contacted 81 participants for a phone screen following their initial assessment to further determine eligibility and interest in the study. Of the 81 participants, 3 were excluded by the therapist because they did not meet criteria, 10 chose not to pursue the therapy, 2 had schedule conflicts with group therapy times, and 3 did not specify a reason for not pursuing the therapy. Thus, 63 participants met the inclusion/exclusion, consented to the study, and were offered treatment. Of the 63 participants, 4 did not complete at least 1 session. Treatment was provided to a total of 59 participants, 50 of which were assessed at post-treatment. The demographic characteristics of participants can been seen in Table 1.
Figure 1.
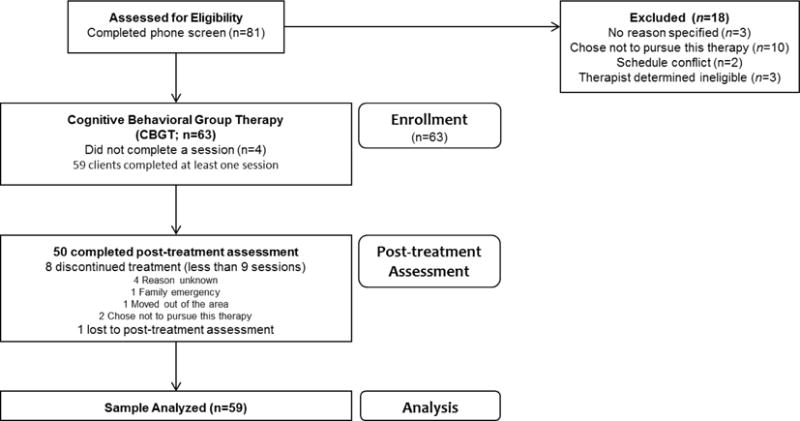
Participant Flow
Table 1.
Demographic Characteristics
| Characteristic | |
|---|---|
|
| |
| Gender n(%) | |
| Female | 34 (57.60%) |
| Male | 25 (42.40%) |
| Other | 0 (0.00%) |
| Mean Age (SD) | 27.90 (10.06) |
| Min/Max | 18.00/60.00 |
| Sexual Orientation n(%) | |
| Heterosexual | 49 (83.10%) |
| Gay/Lesbian | 4 (6.80%) |
| Bisexual | 2 (3.40%) |
| Other | 1 (1.70%) |
| Racial/Ethnic Identity n(%) a | |
| White | 30 (50.80%) |
| Asian | 14 (23.70%) |
| Black | 8 (13.60%) |
| Latino/Hispanic | 6 (10.17%) |
| Pacific Islander | 1 (1.70%) |
| Alaskan/Native | 1 (1.70%) |
| Other/Multiracial b | 7 (11.86%) |
| Previous Psychotherapyc | |
| Yes | 32 (54.23%) |
| No | 24 (48.98%) |
| Taking Medication for Anxiety or Depressiond | |
| No | 51 (87.93%) |
| Yes | 7 (12.07%) |
| SSRIs | 5 (8.62%) |
| SNRIs | 1 (1.72%) |
| Aminoketone (Burpopion) | 1 (1.72%) |
| Mean Pre-Treatment Clinician’s Severity Ratings (SD) SAD subtype | 5.54 (0.80) |
| Generalized n (%) | 46 (78.00%) |
| Non-generalized n (%) | 13 (22.00%) |
| Additional Diagnoses | |
| Yese | 36 (61.02%) |
| No | 23 (38.98%) |
Participants checked as many racial identities as applied
Other identities endorsed: White and Korean, African, Don’t identify, East Indian, Latino skin tone, Serbian, Vietnamese and Italian
Missing data from three participants
Missing data from one participant
Additional Diagnoses n(%): 11 (18.64%) GAD; 10 (16.95%) each for Dysthymia and Specific Phobias; 5 (8.47%) Depressive Disorder NOS; 4 (6.78%) each for MDD, OCD, and Alcohol Abuse 4 (6.78%); 2 (3.39%) each for Panic Disorder with Ag, Substance Abuse, Adjustment Disorder, and PTSD; 1 (1.69%) each for Ag without Panic Disorder, Alcohol use, and Anxiety NOS
Outcome Measures
Anxiety Disorders Interview Schedule
Anxiety Disorders Interview Schedule (ADIS-IV; Brown, DiNardo, & Barlow, 1994) is a semi-structured diagnostic interview used to diagnose DSM-IV anxiety disorders, using a clinician’s severity rating (CSR; ranging from 0 to 8, with ratings 4 or greater indicating clinical significance) for each diagnosis. For SAD, the ADIS-IV has demonstrated adequate reliability (Brown, DiNardo, Lehmann, & Campbell, 2001). Independent assessors gave the ADIS-IV at pre-treatment and post-treatment assessments. Independent assessors were graduate students, unaware of pre- or post-treatment status, trained in the administration and scoring of the ADIS. Training consisted of reading the manual, observing interviewers, and administering interviews with a certified interviewer. To be certified, assessors were required to match a senior interviewer’s diagnoses on three consecutive interviews. Diagnostic matches were defined as agreement on diagnoses within one point on the CSR. Diagnoses were also confirmed in a consensus meeting with a doctoral-level psychologist (Dr. Sarah Hayes-Skelton) and by therapists. Additionally, 20% of interviews were scored by a second rater, with an interclass correlation (ICC) between raters on CSR for SAD of .964.
Social Phobia Anxiety Inventory
Social Phobia Anxiety Inventory (SPAI: Turner, Beidel, & Dancu, 1996) is a widely used, reliable, and valid 45-item self-report measure of social anxiety, accounting for agoraphobia. Items examine the frequency of anxious feelings, somatic symptoms, and thoughts on a 7-point Likert scale, with higher ratings indicating greater frequency. The measure also contains two subscales, social phobia and agoraphobia. Total SPAI score is derived from the difference between the two subscales. The SPAI demonstrated excellent internal consistency in our sample (Pre: α = .98, Post: α = .99).
Brief Fear of Negative Evaluation
Brief Fear of Negative Evaluation (BFNE: Leary, 1983) is a 12-item self-report measure examining participants’ fears of being negatively evaluated using a 1 (not at all characteristic) to 5 (extremely characteristic) Likert scale. The BFNE has been shown to have excellent internal consistency (α= .96) and excellent reliability and validity (Leary, 1983). Studies have also demonstrated that the BFNE has good test re-test reliability (r= .75) and good convergent and divergent validity (Leary, 1983). The BFNE-S was used as a measure of social anxiety and was given to participants at pre- and post-treatment assessment, as well as at the beginning of each session. The BFNE demonstrated acceptable to excellent internal consistency in our sample (α’s from .69 at session 1 to .90 at session 11).
Liebowitz Social Anxiety Scale – Self Report
Liebowitz Social Anxiety Scale – Self Report (LSAS-SR: Liebowitz, 1987) is a self-report measure consisting of 24 social situations that are likely to elicit social anxiety. Participants rate their fear on a scale from 0 (never) to 3 (severe) and their avoidance on a scale from 0 (never) to 3 (usually – 67–100% of the time) for each situation. While the LSAS was originally developed as a clinician-administered interview, a self-report version of the LSAS has been developed (Baker, Heinrichs, Kim & Hofmann, 2002; Fresco et al., 2001). Both studies demonstrated that the self-report version is highly correlated with the clinician version, and that the self-report version has high internal consistency and good test-retest reliability of the self-report version. The LSAS demonstrated excellent internal consistency in our sample (Pre: α= .96, Post: α= .97).
Quality of Life Inventory
Quality of Life Inventory (QOLI: Frisch, 1992) is a 32-item self-report measure examining quality of life. Participants rate the importance of 16 life domains on a 3-point Likert scale, as well as their current satisfaction with each domain on a 6-point Likert scale. Importance scores and satisfaction scores are multiplied for each domain, and then summed to yield an overall quality of life score. Frisch et al. (1992) report good internal consistency (α’s = .77 – .89) and excellent reliability (r’s= .80–.91). The QOLI demonstrated good internal consistency in our sample at all time points (Pre: α = .81, Post: α = .88).
Mean Subjective Units of Distress
Mean Subjective Units of Distress (SUDS) is a rating scale from 0 to 100, with 0 indicating “no anxiety, calm, relaxed” and 100 indicating “severe anxiety, the worst ever encountered” (Hope et al., 2000). The present study measured anxious arousal using participants’ ratings of SUDS during a Behavioral Assessment Test (BAT), administered at pre- and post-treatment assessment. The BAT consisted of a five-minute impromptu speech in front of a confederate and a video camera, as well as five-minute conversation with a confederate. Participants were familiarized with the rating scale prior to the BAT, and then verbalized their SUDS ratings when prompted throughout the BAT at one minute intervals, yielding a total of five SUDS scores. Mean SUDS is the result of averaging the ten scores for each participant.
Mechanism Measures
Experience Questionnaire – decentering subscale
Experience Questionnaire – decentering subscale (EQ – decentering: Fresco et al., 2007) is an 11-item self-report measure assessing trait-like decentering using a 5-point Likert scale. Higher scores indicate greater levels of decentering. The decentering factor of the EQ has been shown to have adequate to good internal consistency as well as convergent and divergent validity (Fresco et al., 2007). Participants completed the EQ at pre- and post-assessment, as well as before every session. The EQ-decentering demonstrated acceptable to excellent internal consistency in our sample (α’s from .78 at pre-treatment to .96 at sessions 11 and 12).
Thought Control Questionnaire – reappraisal subscale
Thought Control Questionnaire – reappraisal subscale (TCQ – reappraisal: Wells & Davies, 1994) is a 6-item self-report scale intended to examine the extent to which cognitive reappraisal is utilized to control thoughts. The TCQ has demonstrated acceptable internal consistency (α= .67) and good test-retest reliability (Wells & Davies, 1994). The TCQ – reappraisal demonstrated good internal consistency in our sample (Pre: α= .81, Post: α= .88).
Procedures
All study procedures were approved by the University of Massachusetts Boston Internal Review Board. All participants provided informed consent for the study. Participants were enrolled in this study following completion of the ADIS and a phone screen to determine eligibility. Participants received therapy free of charge and were paid $75 for completing the post-treatment assessment. All self-report measures and BATs were completed pre- and post-treatment; additionally, the BFNE and the EQ was administered before each session.
Cognitive Behavioral Group Therapy
Clients received a course of cognitive behavioral group therapy, which is a 12-session group therapy (CBGT: Heimberg & Becker, 2002). Each group consisted of two therapists and four to six clients meeting weekly for two and a half hour sessions. Additionally, clients received an initial engagement session prior to the first session, in which they were oriented to the treatment. The first three sessions of CBGT focused on psychoeducation and training in Beckian-style cognitive restructuring. Clients identified automatic thoughts and associated thinking errors, followed by a process of asking and answering disputing questions. By the third session, sessions involved therapist-led cognitive restructuring followed by in-session exposures. Therapists and clients also worked together to design homework exposures that built on the in-session exposures to do between sessions. On average, clients completed 9.22 of the 12 sessions.
Therapists
Therapists for this study were the first author, a licensed clinical psychologist, or advanced doctoral students (n = 9) trained and supervised on a weekly basis by the first author. Additionally, Dr. Heimberg provided an initial training to therapists.
Adherence
A total of 30 sessions (20% of all sessions) were rated for adherence by doctoral students in clinical psychology. For each group, one session was randomly chosen from sessions 1–6, and one from sessions 7–12. The adherence checklist listed 32 allowed (adapted from Hope, VanDyke, Heimberg, Turk, & Fresco, unpublished) and 6 forbidden strategies (e.g., limiting experiential control, mindfulness, explicit mention of decentering, problem solving, psychodynamic themes, and relaxation strategies; adapted from those used in Hayes-Skelton, Roemer, & Orsillo, 2013). Each of the allowed elements were rated on a Likert scale for the frequency/depth with which it was addressed in session from 1 (not at all/not effective) to 5 (highly/extremely effective). The allowed components were typically rated as being addressed effectively [means from 4.40 (SD= 0.89) to 5.00 (SD= 0.00)]. Only one session had a forbidden strategy (limiting experiential control and using psychodynamic themes). Additionally, of the thirty sessions rated for adherence, 25% of these sessions were rated by a second rater with adequate reliability (α= .58).
Statistical Analysis
Data were examined for skewness, kurtosis, and outliers. At pre-treatment, the BFNE score had substantial skew and kurtosis. This was driven by one outlier from a participant with a BFNE score approximately four standard deviations below the mean. Therefore, analyses were run with and without this participant. However, the results did not change and so this participant’s data was retained. No other variables had concerning skew or kurtosis.
Given that treatment was administered in a group context, between group variability was examined through Intraclass Correlations (ICC’s) to assess for any dependency in the data. The ICC’s were generally low for the outcome measures (BATs= .003, SPAI= .030, LSAS= .025, BFNE= .028)2. Therefore, to conserve power, outcome analyses were run without taking into account group membership. However, the ICC for session-by-session EQ-decentering was higher (.17), indicating that there may be issues related to dependency when examining the session-by-session data. Therefore, in the growth curve analyses examining the session-by-session data, participants were nested into their treatment groups.
The primary analyses compared treatment over time using Mixed-Effects Regression Models (MRM) in SPSS Version 23 (Hedeker & Gibbons, 2006). Separate analyses were run for each of the outcome variables across the two time points (pre-treatment and post-treatment). Models were run assuming random intercepts and slopes. In these hierarchical linear models, Level 1 models individual change over time and Level 2 models the between-subjects factors. Each MRM analysis examined the overall effect of change over time (Time) using an unstructured covariance matrix. Based on the recommendation of Feingold (2009), within-subject effect sizes (d) were calculated as the difference between post-treatment and pre-treatment means divided by the standard deviation of the pre-treatment mean. These d’s can be interpreted using Cohen’s (1988) guidelines.
To examine significant change over time, we computed the reliable change index (RCI: Jacobson & Truax, 1991) for each outcome measure. The RCI is a method of computing the statistically reliable change of a measure over time. The RCI is computed by subtracting the pretreatment score from the post-treatment score, and dividing the sum by the standard error of difference. If the absolute value of the RCI is greater than 1.96, then the change in scores is considered to be reliable (Jacobson & Truax, 1991).
To examine changes in decentering over time, session-by-session EQ-decentering was analyzed using latent growth curve modeling. Latent growth curve modeling describes growth using two parameters, the intercept and the slope. For the analyses presented here, growth curve models were run using Mplus 6 (Muthén & Muthén, 2010). In these models, missing data was handled using maximum likelihood (ML) estimation techniques and participants were nested into their treatment groups. First, an unconditional growth model was run where the intercept was set to EQ-decentering score at session 1 and the slope was linear. Next, a second model was run in which the slope rate was allowed to be freely estimated. Finally, a series of growth models were run in which the residualized gain scores of each outcome measure were regressed on the EQ-decentering intercept and slopes from the freely estimated model.
The final set of analyses examined whether change on EQ-decentering predicted outcome over and above a competing mechanism (reappraisal). For these analyses, a series of hierarchical logistic regression models examined the relations between residualized gain scores for TCQ-reappraisal (entered as step 1) and residualized gain scores for EQ-decentering (entered as step 2) and outcome. These analyses were based on the individuals who completed the post-treatment assessment. Additionally, for these analyses participants were not nested into groups to preserve power and because this nesting was not indicated for the outcome variables described above.
Missing Data
Post-treatment diagnostic interviews were conducted with 50 of 59 participants (84.7%). Additionally, 48 of 59 participants (81.4%) completed the post-treatment self-report measures. One participant did not complete the pre-treatment SPAI. At each session between 1.7% and 35.6% of participants were absent and therefore did not complete session measures (24.2% were missing per session on average). To avoid bias, all cases were included in the MRM and growth models. MRM and growth models analyze data using maximum likelihood estimation to account for missing data, which assumes that data are “missing at random.” Analyses indicated that missingness could be assumed to be completely random (Little’s MCAR chi square = 980.76, p = .52), indicating that maximum likelihood estimation was an appropriate method for analyzing these data. Because the focus of the mechanism analysis was on how decentering and reappraisal were related to treatment outcome, only participants who completed the post-treatment assessment were included in the hierarchical regressions.
Results
The means and standard deviations of all study measures at pre- and post-treatment are presented in Table 2. Over the course of therapy, four individuals began a medication for anxiety or depression by session 4; one person began a medication for anxiety or depression at session 9; one individual began Adderall at session 2; one individual used Adderall inconsistently throughout the treatment; and nine received additional therapy (check-in with previous therapists (n=2), grief counseling, trauma counseling, alcohol use counseling, career counseling, attention deficit disorder counseling, stress counseling, counseling for roommate issues (n=1 for each)).
Table 2.
Means and standard deviations (untransformed) of study measures at each time point
| Pretreatment M (SD) (N = 59) |
Posttreatment M (SD) (n = 50) |
|
|---|---|---|
| Primary Outcome | ||
|
| ||
| SAD CSR | 5.54 (0.80) | 3.77 (1.23) |
| LSAS | 121.18 (25.77) | 99.69 (22.98) |
| SPAI | 10.68 (2.68) | 7.26 (2.66) |
| BFNE | 48.91 (8.72) | 39.86 (8.67) |
| Mean SUDS | 65.83 (20.29) | 48.48 (20.37) |
| QOLI | 0.56 (1.68) | 1.04 (1.78) |
| Mechanism Measures | ||
| EQ - decentering | 35.38 (6.74) | 41.69 (7.98) |
| TCQ - reappraisal | 13.64 (3.15) | 15.03 (3.27) |
Note. SAD CSR = social anxiety disorder Clinician Severity Rating; LSAS = Liebowitz Social Anxiety Scale; SPAI = Social Phobia and Anxiety Inventory; BFNE = Brief Fear of Negative Evaluation; Mean SUDS = mean Subjective Units of Discomfort during Behavioral Avoidance Tests; QOLI = Quality of Life Inventory; EQ – decentering = decentering subscale of the Experiences Questionnaire; TCQ = Thought Control Questionnaire.
Outcome Analyses
Table 3 presents the results of the MRM models. The MRM models for clinician rated severity of SAD, self-report measures of social anxiety (SPAI, LSAS, BFNE), and SUDS during the BATS showed significant (large) effects for Time indicating that clients’ social anxiety symptoms significantly decreased across treatment. There was a significant effect for Time on the QOLI, indicating increasing quality of life; however, this effect size was small.
Table 3.
Results of the mixed effects regression models examining change across treatment
| Estimate | SE | t | p | 95% CI | da | RCI % | |
|---|---|---|---|---|---|---|---|
| SAD CSR | 80.4% | ||||||
| Intercept | 5.54 | 0.10 | 54.02 | <.001 | 5.34, 5.75 | ||
| Time | −1.76 | 0.16 | −11.08 | <.001 | −2.08, −1.44 | −2.23 | |
| LSAS | 60.7% | ||||||
| Intercept | 121.18 | 3.32 | 36.43 | <.001 | 114.52, 127.83 | ||
| Time | −21.36 | 3.19 | −6.79 | <.001 | −27.52, −14.96 | −0.81 | |
| SPAI | 69.6% | ||||||
| Intercept | 10.64 | 0.35 | 30.35 | <.001 | 9.93, 11.34 | ||
| Time | −3.39 | 0.41 | −8.21 | <.001 | −4.22, −2.56 | −1.24 | |
| BFNE | 64.3% | ||||||
| Intercept | 48.92 | 1.12 | 43.45 | <.001 | 46.66, 51.17 | ||
| Time | −9.30 | 1.27 | −7.31 | <.001 | −11.86, −6.74 | −1.28 | |
| BAT SUDS | 64.3% | ||||||
| Intercept | 65.83 | 2.62 | 25.13 | <.001 | 60.59, 71.07 | ||
| Time | −17.64 | 2.90 | −6.08 | <.001 | −23.48, −11.82 | −0.91 | |
| QOLI | 51.8% | ||||||
| Intercept | 0.56 | 0.22 | 2.60 | .01 | 0.13, 1.00 | ||
| Time | 0.51 | 0.22 | 2.29 | .03 | 0.06, 0.96 | −0.33 |
Note. Intercept is pre-treatment. Time is change from pre- to post-treatment. Participants who did not complete post-assessment are classified as not experiencing reliable change. Based on the recommendation of Feingold (2009), d’s were calculated as the difference between post-treatment and pre-treatment means divided by the standard deviation of the pre-treatment mean.
Clinical Significance
RCIs for the primary outcome measures indicated that 51.8% (29/56) to 80.4% (45/56 for CSR) of participants who completed at least one session experienced reliable change across the outcome measures. Please note that these numbers classify the 8-10 participants who did not complete a given measure as not experiencing reliable change and so these are conservative estimates of actual change. Similarly, 38.0% (19/50) of clients no longer met criteria for SAD.
Change in Decentering
To test the hypothesis that clients would report significant changes in decentering over the course of CBGT, a linear growth curve model was estimated (see Figure 2). For EQ-decentering, the intercept, or average EQ score at session 1, was 34.99 and the slope was 0.66. In other words, on average clients’ reported EQ score increased from 34.99 at session 1 to 42.25 at the end of therapy (0.66 points per sessions from sessions 1 to 12). This is a significant slope (z = 5.68, p<.001). In other words, per item EQ-decentering scores went from a 3.18 to a 3.84 over treatment. By comparison, Fresco et al. (2007) reported an average per item score of 3.45 (SD=0.49) in the decentering subscale of the EQ for a sample of college students. Furthering our examination of change in the decentering over time, a second growth model was estimated in which the shape of change was freely estimated. As is shown in Figure 2, there was little change in EQ over the first 3 sessions. However, as exposure was introduced, there was a rapid increase in decentering. Decentering scores then remained relatively consistent through the middle of therapy before increasing again at the end of treatment.
Figure 2.
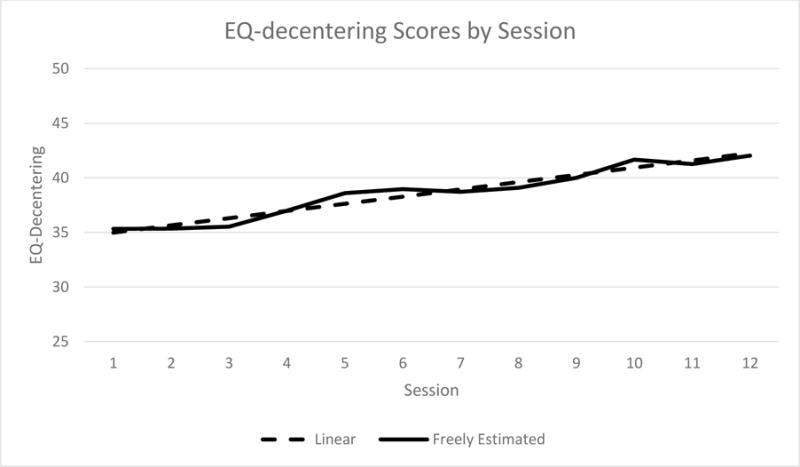
Changes in EQ-decentering scores by session
Decentering’s Relations to Outcome
A series of growth models were run where the residualized gain score for the outcome variables (SAD CSR, SPAI, LSAS, BFNE, mean SUDS, QOLI) were added as distal outcome variables to the EQ growth model where the slope was allowed to be freely estimated. The slope of EQ-decentering significantly predicted the residualized gain scores for SAD CSR, LSAS, BFNE, and QOLI while accounting for EQ-decentering scores at session 1 (p’s from .03 to .001). Contrary to expectations, the slope of EQ-decentering did not significantly predict the residualized gain scores of the SPAI or the mean SUDS ratings on the BATs while accounting for EQ-decentering scores at session 1 (p’s from .12 to .15). In other words, larger increases in decentering over the course of therapy were related to more improved clinician rated social anxiety, quality of life, and some, but not all, self-report measures of social anxiety. However, it was not related to anxiety on a behavioral avoidance task or on one self-report measures of social anxiety. Additionally, EQ-decentering scores at session 1 were not significantly related to any of the outcome measures (p’s from .47 to .96), indicating that baseline decentering levels were unrelated to outcome.
To further understand the relation between decentering and outcome, t-tests compared those with and without clinical significant SAD based on the CSR rating at post-treatment to EQ scores. Results revealed that those no longer meeting criteria for SAD had significantly more change on the EQ based on the residualized gain scores compared to those still meeting criteria for SAD (t(45)=2.93, p=.005). Those no longer meeting criteria for SAD also had significantly higher EQ scores at post-treatment (45.78) compared to those with clinically significant SAD (M = 39.24, t(46)=2.96, p=.005). However, there were no differences between those no longer meeting criteria (36.69) and those with clinically significant SAD (34.11) on the EQ at pretreatment (t(47)=1.52, p=.14).
Decentering and Reappraisal
In order to determine whether change on EQ-decentering predicts outcome over and above a competing mechanism (change in reappraisal), a series of hierarchical logistic regression models were run to examine the relations between outcome and residualized gain scores for EQ-decentering and TCQ-reappraisal where post-treatment scores on these measures were regressed on pre-treatment scores. In all six of these models (residualized gain scores for SPAI, LSAS, BFNE, SAD CSR, mean SUDS, and QOLI), the models were significantly improved upon by adding the residualized gain score for EQ-decentering to the Step 1 model that only included residualized gain of TCQ-reappraisal (R2-change from .05 to .25, p’s from .048 to < .001). With both the EQ-decentering and TCQ-reappraisal in the model (Step 2), the Betas for EQ-decentering were significant in predicting SPAI, LSAS, BFNE, and mean SUDS (p’s from .007 to <.001) with there being a trend level effect for QOLI (p=.052). Of note, the Beta for EQ-decentering in the model predicting SAD CSR was not significant (p=.12). In contrast, the Betas for TCQ-reappraisal were not significant in any of these models once EQ-decentering was in the model (p’s from .13 to .92). Together, these models indicated that decentering generally predicted outcome above and beyond reappraisal in the clients who completed the post-treatment assessment.3 Of note, the correlation between the residualized gain scores of EQ-decentering and TCQ-reappraisal was .41 (p=.005).
Discussion
Overall, this study sought to examine the role of decentering across CBGT for clients with social anxiety disorder. Before decentering can be evaluated, we first examined the efficacy of CBGT in this study. As expected, CBGT generally led to positive outcomes for the clients in this study with large effect sizes across a range of self-report, behavioral, and interviewer administered measures of social anxiety (d’s from 0.81 to 2.23), which are comparable to those reported in other studies. However, it should be noted that the effect size for quality of life was small in this study. Depending on the outcome measure used, 51.8% to 80.4% of clients experience reliable change. These numbers are consistent with other reliable change numbers for CBGT (Blanco et al., 2010; Heimberg et al., 1990; Kocovski et al., 2013). While comparisons across studies are always problematic, the lack of consistency in terms of which outcome measures are reported in which study makes this a particularly difficult comparison for social anxiety treatment studies. Therefore, this study is reporting a range of outcome measures.
Even gold-standard treatments for SAD such as CBGT fail to treat a high proportion of clients, speaking to the need to continue to improve this treatment. One approach to treatment improvement is to examine potential mechanisms of change that could be better targeted. As has been shown in other disorders, namely depression and GAD, decentering may be a potential mechanism of change in treatments of social anxiety disorder, given the attention biases that maintain social anxiety. The current study was focused on whether decentering would be associated with change following CBGT despite decentering being explicitly targeted (i.e., it is not in the explicitly in the treatment manual). While decentering was not an explicit target in CBGT, some of the elements of CBGT may promote decentering. For example, cognitive restructuring, in particular viewing thoughts as psychological events, is thought of as a distancing strategy that may promote decentering (Beck, 1979). If clients who experienced an increase in decentering were the ones that saw the most improvement in CBGT, then it may be that more explicitly promoting decentering during the course of CBGT may further enhance outcome. This study is the first step in understanding decentering’s potential role in CBGT. More research is needed to determine whether further promoting decentering does indeed lead to its increase and improved symptoms.
As preliminary evidence of decentering’s role in treatment improvement, change in decentering was significantly higher for those who no longer met criteria for SAD compared to those that retained a diagnosis of SAD at the end of treatment. In other words, those whose anxiety no longer met the clinically significant threshold at post-treatment had significantly more decentering at post-treatment when taking into account decentering at pre-treatment. This may indicate that experiencing an increase in decentering differentiates those who make and do not make improvement. However, it is important to note that decentering is likely just one of several important mechanisms as it does not perfectly differentiate those who do and who do not have SAD at the end of treatment. In particular, this model does not incorporate the clinical benefits of new learning and willingness to engage in anxiety-provoking situations that has been well-documented as important mechanisms in SAD (Craske et al., 2008). More research is needed to examine how these, and other mechanisms of action, interact to produce change. For example, does decentering foster new learning during exposure exercises by allowing a wider range of experiences to be incorporated into the fear network, do the exposure exercises foster decentering, or are decentering and new learning two separate processes? Similarly, while there is a growing body of research on the neurobehavioral basis of decentering (see Farb et al., 2007; Fresco et al., 2017; Kross et al., 2009), more research is needed in this area.
On average, decentering increased across CBGT. Scores on the decentering subscale for the EQ began at 34.99 at session one and increased to 42.25 by session 12. To put this in context, previous research has reported that an unselected undergraduate population scored an average of 37.51 (SD=3.58) on this scale (Fresco, Moore, et al., 2007). In other words, clients began treatment almost a standard deviation below this mean and ended treatment over a standard deviation above this mean, indicating that clients are experiencing more decentering at the end of treatment than the average population. Interestingly the biggest increase in decentering happened between sessions three and five, with additional change happening from approximately session nine onward. In looking at the treatment protocol, clients typically complete their first exposure exercises between sessions three and five, speaking to the potential link between exposure exercises and decentering.
We were also interested in whether decentering predicted outcome. Interestingly, this varied depending on the outcome measure used. For example the strongest association was between decentering and the BFNE. Given that the BFNE specifically measures the cognitive component of SAD (i.e., fear of negative evaluations), it may be that decentering has its greatest influence in the cognitive domain. As decentering is in fact a cognitive task, it makes sense that it would be most associated with changing cognitions. On the other hand, decentering had less of an influence on the behavioral measure (Mean SUDS on the BATs). This may in part be because of the differences in measurement. For example, there may be a bias towards responding to all self-report measures similarly.
Finally, we were interested in whether decentering would be associated with outcome over and above a competing mechanism. Specifically, in this study, we were interested in cognitive reappraisal, as this is one of the skills explicitly taught as part of CBGT. Interesting, cognitive reappraisal was inconsistently related to outcome, with the relation only reaching statistical significance on two of our measures with a third being a trend level relation. In contrast, adding decentering to the regression models significantly improved upon the cognitive reappraisal-only models for all six of our outcomes. This provides additional evidence that it may be decentering, more so than cognitive reappraisal, which is contributing to outcome. Of course, decentering is only one of several potential mechanisms (e.g., self-focused attention, reduced social cost biases, emotional processing, new learning to name a few) and the relative role of decentering compared to these other potential mechanisms needs to be evaluated. Similarly, the measure of cognitive reappraisal used in this study focused on the strategy of using cognitive reappraisal rather than assessing actual change in threat-relevant cognitions, limiting the conclusions we can make about actual changes in cognitions. More research is needed to explore the relation between cognitive restructuring and decentering, as it may be cognitive restructuring exercises that promote decentering. Thus, it is possible that cognitive restructuring may be associated with clinical benefit because it promotes decentering, rather than cognitive reappraisal. This theory needs to be more directly evaluated to better understand these relations.
As with all studies, this project has a number of limitations. Most notably, this study relied on self-report ratings of decentering. While these self-report ratings allowed for a frequent assessment of the mechanism and the EQ is the most common measure of decentering, completing a self-report measure of an internal process requires some psychological mindedness. More research is needed to understand the validity of this measurement approach and to develop non-self-report measures of this construct. Additionally, there was no comparison treatment group in this study and so it is not possible to evaluate whether these changes were specific to CBGT or to treatment in general. There were also no competency ratings to provide evidence of the quality of treatment delivered. This study provides preliminary support for the role of decentering in CBGT; however, more research is needed to evaluate decenter across treatment, in comparison with competing mechanisms, and with larger samples that will allow for a better understanding of whether there are interpersonal factors (i.e., cultural factors, personality factors) that may impact this relationship.
Taken together, this study provides preliminary support for the role of decentering in CBGT for social anxiety disorder. While more research needs to be done, particularly given some of the inconsistencies in our results, this study lends support for future investigation into the potential benefit of enhancing decentering during therapy. For example, while conducting cognitive restructuring, it may be possible for therapists to enhance the decentering aspects of the intervention to more explicitly help clients improve their decentering ability.
Highlights.
Study examined Cognitive Behavioral Group Therapy for clients with social anxiety disorder
A potential mechanism, decentering, increased over CBGT
Change in decentering predicted improvement on most, but not all outcome measures
Change in decentering predicted outcome over and above change in the competing mechanism of reappraisal
Results largely support the role of decentering in CBGT for social anxiety
Acknowledgments
This work was supported by National Institute of Mental Health Grant No. MH085060 awarded to the first author. The authors thank the large team that made this project possible. Richard Heimberg provided training to therapists. Lizabeth Roemer and Stefan Hofmann were consults. Therapists included: Shannon Sorenson, Jessica Graham LoPresti, Speshal Walker Gautier, Shruti Mukkamala, Lucas Morgan, Tory Choate, Ashley Shirai, Sarah Krill Williston, Amber Calloway, and Lauren Wadsworth, as well as the first author. Assessors included: Sarah Krill Williston, Amber Calloway, Elizabeth Eustis, Jessica Graham LoPresti, Jennifer Martinez, Tamim Mohammad, Lucas Morgan, Shruti Mukkamala, Fanny Ng, Lauren Wadsworth, Ashley Shirai, Shannon Sorenson, as well as the both authors. Additionally, we would like to thank our project managers: Dan Paulus and Megan Garrad, as well as numerous UMB undergraduate students. Finally, we would like to thank the clients. This work would not be possible without their openness, courage, and willingness.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Other efficacious treatments for social anxiety disorder include: cognitive therapy (Clark et al., 2003); Social Self-Reappraisal Therapy (Hofmann & Scepkowski, 2006); and psychopharmacological treatments such as fluoxetine and fluvoxamine (Hedges et al., 2007), to name a few.
Please note that there were convergence problems running the ICC calculations for the CSRs and QOLI. Therefore, the Mixed-Effects Regression Models involving these outcomes were run with and without participants nested into their treatment groups. The results minimally differed and so the results from the simpler models are reported here.
We also ran the series of hierarchical regressions in the reverse order with the residualized gain of EQ-decentering in step 1 and residualized gain of TCQ-reappraisal in step 2. In no cases was the R-square change score of Step 2 significant (p’s from .92 for LSAS to .13 for BFNE)
References
- Acarturk C, Cuijpers P, van Straten A, de Graaf R. Psychological treatment of social anxiety disorder: a meta-analysis. Psychological Medicine. 2009;39(2):241–254. doi: 10.1017/S0033291708003590. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Washington, DC: 2013. [Google Scholar]
- Amir N, Elias J, Klumpp H, Przeworski A. Attentional bias to threat in social phobia: facilitated processing of threat or difficulty disengaging attention from threat. Behaviour Research and Therapy. 2003;11:1325–1335. doi: 10.1016/S0005-7967(03)00039-1. [DOI] [PubMed] [Google Scholar]
- Arch JJ, Craske MG. Acceptance and commitment therapy and cognitive behavioral therapy for anxiety disorders: Different treatments, similar mechanisms? Clinical Psychology: Science and Practice. 2008;15(4):263–279. doi: 10.1111/j.1468-2850.2008.00137.x. [DOI] [Google Scholar]
- Arch JJ, Wolitzky-Taylor KB, Eifert GH, Craske M. Longitudinal treatment mediation of traditional cognitive behavioral therapy and acceptance and commitment therapy for anxiety disorders. Behaviour Research and Therapy. 2012;50:469–478. doi: 10.1016/j.brat.2012.04.007. [DOI] [PubMed] [Google Scholar]
- Baker SL, Heinrichs N, Kim HJ, Hofmann SG. The Liebowitz social anxiety scale as a self-report instrument: a preliminary psychometric analysis. Behaviour Research and Therapy. 2002;40:701–715. doi: 10.1016/S0005-7967(01)00060-2. [DOI] [PubMed] [Google Scholar]
- Bar-Haim Y, Lamy D, Bakermans-Kranenburg MJ, van Ijzendoorn MH. Threat-related attentional bias in anxious and nonanxious individuals: A meta-analytic study. Psychological Bulletin. 2007;133(1):1–24. doi: 10.1037/0033-2909.133.1.1. [DOI] [PubMed] [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. New York, NY: Guilford Press; 1979. [Google Scholar]
- Bernstein A, Hadash Y, Lichtash Y, Tanay G, Shepherd K, Fresco DM. Decentering and related constructs: A critical review and metacognitive processes model. Perspectives on Psychological Science. 2015;10:599–617. doi: 10.1177/1745691615594577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bieling PJ, Hawley LL, Bloch RT, Corcoran KM, Levitan RD, Young LT, MacQueen GM, Segal ZV. Treatment-specific changes in decentering following mindfulness-based cognitive therapy versus antidepressant medication or placebo for prevention of depressive relapse. Journal of Consulting and Clinical Psychology. 2012;80:365–372. doi: 10.1037/a0027483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop SR, Lau M, Shapiro S, et al. Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice. 2004;11:230–241. doi: 10.1093/clipsy/bph077. [DOI] [Google Scholar]
- Brown TA, DiNardo PA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV (ADIS-IV) San Antonio, TX: Psychological Corporation; 1994. [Google Scholar]
- Brown TA, DiNardo PA, Lehmann CL, Campbell LA. Reliability of DSM-IV anxiety and mood disorders: Implications for the classification of emotional disorders. Journal of Abnormal Psychology. 2001;110(1):49–58. doi: 10.1037/0021-843X.110.1.49. [DOI] [PubMed] [Google Scholar]
- Castonguay LG. Psychotherapy, psychopathology, research and practice: Pathways of connections and integration. Psychotherapy Research. 2011;21:125–140. doi: 10.1080/10503307.2011.563250. [DOI] [PubMed] [Google Scholar]
- Clark DM, Wells AA. A cognitive model of social phobia. In: Heimberg RG, Liebowitz MR, Hope DA, Schneier FR, editors. Social Phobia: Diagnosis, assessment, and treatment. New York, NY: Guilford Press; 1995. pp. 69–93. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Craske MG, Kircanski K, Zelikowsky M, Mystkowski J, Chowdhury N, Baker A. Optimizing inhibitory learning during exposure therapy. Behaviour Research and Therapy. 2008;46(1):5–27. doi: 10.1016/j.brat.2007.10.003. [DOI] [PubMed] [Google Scholar]
- Davis JI, Gross JJ, Ochsner KN. Psychological distance and emotional experience: what you see is what you get. Emotion. 2011;11:438–444. doi: 10.1037/a0021783. [DOI] [PubMed] [Google Scholar]
- Fedoroff IC, Taylor S. Psychological and pharmacological treatments of social phobia: A meta-analysis. Journal of Clinical Psychopharmacology. 2001;21:311–324. doi: 10.1097/00004714-200106000-00011. [DOI] [PubMed] [Google Scholar]
- Feingold A. Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychological Methods. 2009;14:43–53. doi: 10.1037/a0014699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feske U, Chambless DL. Cognitive behavioral versus exposure only treatment for social phobia: a meta-analysis. Behavior Therapy. 1995;26:695–720. doi: 10.1016/S00057894(05)80040-1. [DOI] [Google Scholar]
- Fox E, Russo R, Bowles R, Dutton K. Do threatening stimuli draw or hold visual attention in subclinical anxiety? Journal of Experimental Psychology. 2001;130:681–700. doi: 10.1037/0096-3445.130.4.681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fresco DM, Coles ME, Heimberg RG, Leibowitz MR, Hami S, Stein MB, Goetz D. The Liebowitz Social Anxiety Scale: A comparison of the psychometric properties of self-report and clinician-administered formats. Psychological Medicine. 2001;31:1025–1035. doi: 10.1017/S0033291701004056. [DOI] [PubMed] [Google Scholar]
- Fresco DM, Moore MT, van Dulmen MHM, Segal ZV, Ma SH, Teasdale JD, Williams JMG. Initial psychometric properties of the experiences questionnaire: Validation of a self-report measure of decentering. Behavior Therapy. 2007;38:234–246. doi: 10.1016/j.beth.2006.08.003. [DOI] [PubMed] [Google Scholar]
- Fresco DM, Roy AK, Adelsberg S, Seeley S, García-Lesy E, Liston C, Mennin DS. Distinct functional connectivities predict clinical response with Emotion Regulation Therapy. Frontiers in Human Neuroscience. 2017 doi: 10.3389/fnhum.2017.00086. [DOI] [PMC free article] [PubMed]
- Fresco DM, Segal ZV, Buis T, Kennedy S. Relationship of posttreatment decentering and cognitive reactivity to relapse in major depression. Journal of Consulting and Clinical Psychology. 2007;75(3):447–455. doi: 10.1037/0022-006X.75.3.447. [DOI] [PubMed] [Google Scholar]
- Frisch MB, Cornell J, Villanueva M, Retzlaff PJ. Clinical validation of the quality of life inventory. a measure of life satisfaction for use in treatment planning and outcome assessment. Psychological Assessment. 1992;4:92–101. doi: 10.1037/1040-3590.4.1.92. [DOI] [Google Scholar]
- Gould RA, Buckminster S, Pollack MH, Otto MW, Yap L. Cognitive-behavioral and pharmacological treatment for social phobia: A meta-analysis. Clinical Psychology: Science and Practice. 1997;4:291–306. doi: 10.1111/j.1468-2850.1997.tb00123.x. [DOI] [Google Scholar]
- Hackmann A, Surawy C, Clark DM. Seeing yourself through others’ eyes: A study of spontaneously occurring images in social phobia. Behavioural and Cognitive Psychotherapy. 1998;26:3–12. doi: 10.1017/S1352465898000022. [DOI] [Google Scholar]
- Hayes SC. Acceptance and Commitment Therapy, Relational Frame Theory, and the third wave of behavior therapy. Behavior Therapy. 2004;35:639–665. doi: 10.1016/S0005-7894(04)80013-3. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy, second edition: The process and practice of mindful change. New York: The Guilford Press; 2011. [Google Scholar]
- Hayes-Skelton SA, Calloway A, Roemer L, Orsillo SM. Decentering as a potential common mechanism across two therapies for generalized anxiety disorder. Journal of Consulting and Clinical Psychology. 2015 doi: 10.1037/a0038305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes-Skelton S, Graham J. Decentering as a common link among mindfulness, cognitive reappraisal, and social anxiety. Behavioural and Cognitive Psychotherapy. 2012;1:1–12. doi: 10.1017/S1352465812000902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes-Skelton SA, Roemer L, Orsillo SM. A randomized clinical trial comparing an Acceptance Based Behavior Therapy to Applied Relaxation for generalized anxiety disorder. Journal of Consulting and Clinical Psychology. 2013;81:761–773. doi: 10.1037/a0032871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedeker D, Gibbons RD. Longitudinal Data Analysis. Hoboken, N.J: Wiley; 2006. [Google Scholar]
- Heimberg RG. Cognitive–behavioral treatment of social phobia in a group setting: A treatment manual. State University of New York; Albany: 1991. Unpublished manuscript. [Google Scholar]
- Heimberg RG. Cognitive-behavioral therapy for social anxiety disorder: Current status and future directions. Biological Psychiatry. 2002;51(1):101–108. doi: 10.1016/S0006-3223(01)01183-0. [DOI] [PubMed] [Google Scholar]
- Heimberg RG, Becker RE. Cognitive-behavioral group therapy for social phobia: Basic mechanisms and clinical strategies. New York, NY: The Guilford Press; 2002. [Google Scholar]
- Heimberg RG, Liebowitz MR, Hope DA, Schneier FR, Holt CS, Welkowitz LA, Juster HR, Campeas R, Bruch MA, Cloitre M, Fallon B, Klein DF. Cognitive behavioral group therapy vs. phenelzine therapy for social phobia: 12-week outcome. Archives of General Psychiatry. 1998;55:1133–1141. doi: 10.1001/archpsyc.55.12.1133. [DOI] [PubMed] [Google Scholar]
- Heimberg RG, Salzman D, Holt CS, Blendell K. Cognitive behavioral group treatment for social phobia: effectiveness at five-year follow-up. Cognitive Therapy and Research. 1993;17:325–339. doi: 10.1007/BF01177658. [DOI] [Google Scholar]
- Heinrichs N, Hofmann SG. Information processing in social phobia: a critical review. Clinical Psychology Review. 2001;21:751–770. doi: 10.1016/S0272-7358(00)00067-2. [DOI] [PubMed] [Google Scholar]
- Herbert JD, Cardaciotto LA. Acceptance and mindfulness-based approaches to anxiety. New York, NY: Springer; 2005. An acceptance and mindfulness-based perspective on social anxiety disorder; pp. 189–212. [Google Scholar]
- Herzberg KN, Sheppard SC, Forsyth JP, Crede M, Earleywine M, Eifert GH. The believability of anxious feelings and thoughts questionnaire (BAFT): a psychometric evaluation of cognitive fusion in a nonclinical and highly anxious community sample. Psychological Assessment. 2012;24:877–891. doi: 10.1037/a0027782. [DOI] [PubMed] [Google Scholar]
- Hirsch CR, Mathews A. Impaired positive inferential bias in social phobia. Journal of Abnormal Psychology. 2000;109:705–712. doi: 10.1037/0021-843X.109.4.705. [DOI] [PubMed] [Google Scholar]
- Hoge EA, Bui E, Goetter E, Robinaugh DJ, Ojserkis RA, Fresco DM, Simon NM. Change in decentering mediates improvement in anxiety in mindfulness-based stress reduction for generalized anxiety disorder. Cognitive Therapy and Research. 2015;39:228–235. doi: 10.1007/s10608-014-9646-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Heinrichs N. Differential effect of mirror manipulation on self-perception in social phobia subtypes. Cognitive Therapy and Research. 2003;27:131–142. doi: 10.1023/A:1023507624356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hope DA, Heimberg RG, Juster HR, Turk CL. Managing social anxiety: A cognitive-behavioral therapy approach (Client workbook) New York: Oxford Press; 2000. [Google Scholar]
- Hope DA, Heimberg RG, Bruch MA. Dismantling cognitive-behavioral group therapy for social phobia. Behavior Research and Therapy. 1995;33:637–650. doi: 10.1016/0005-7967(95)00013-N. [DOI] [PubMed] [Google Scholar]
- Hope DA, VanDyke M, Heimberg RG, Turk CL, Fresco DM. Cognitive-behavioral therapy for social anxiety disorder: Therapist adherence scale (unpublished) [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59(1):12–19. doi: 10.1037/0022-006X.59.1.124. [DOI] [PubMed] [Google Scholar]
- Katzelnick DJ, Kobak KE, Henk HJ, Greist JH, Davidson JR, Schneier FR, Stein MB, Helstad CP. American Journal of Psychiatry. 2001;158(12):1999–2007. doi: 10.1176/aapi.ajp.158.12.1999. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Walters EE. Lifetime prevalence and age-of- onset distributions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.7.768. [DOI] [PubMed] [Google Scholar]
- Kocovski D, Benger M, Shlik J, Bradwejn J. Randomized trial of a meditation-based stress reduction program and cognitive behavior therapy in generalized social anxiety disorder. Behavior Research and Therapy. 2007;45:2518–2526. doi: 10.1016/j.brat.2007.04.011. [DOI] [PubMed] [Google Scholar]
- Kocovski NL, Fleming JE, Hawley LL, Huta V, Antony MM. Mindfulness and acceptance-based group therapy versus traditional cognitive behavioral group therapy for social anxiety disorder: a randomized controlled trial. Behavior Research and Therapy. 2013;51:889–898. doi: 10.1016/j.brat.2013.10.007. [DOI] [PubMed] [Google Scholar]
- Kross E, Ayduk Ö. Making meaning out of negative experiences by self-distancing. Current Directions in Psychological Science. 2011;20:187–191. [Google Scholar]
- Kross E, Davidson M, Weber J, Ochsner K. Coping with emotions past: The neural bases of regulating affect associated with negative autobiographical memories. Biological Psychiatry. 2009;65:361–366. doi: 10.1016/j.biopsych.2008.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau MA, Bishop SR, Segal ZV, Buis T, Anderson ND, Carlson L, Shapiro S, Carmody J, Abbey S, Devins G. The Toronto mindfulness scale: Development and validation. Journal of Clinical Psychology. 2006;62:1445–1467. doi: 10.1002/jclp.20326. [DOI] [PubMed] [Google Scholar]
- Leary MR. A brief version of the Fear of Negative Evaluation Scale. Personality and Social Psychology Bulletin. 1983;9:371–375. doi: 10.1177/0146167283093007. [DOI] [Google Scholar]
- Liebowitz MR. Social phobia. Modern Problems of Pharmacopsychiatry. 1987;22:141–173. doi: 10.1159/000414022. [DOI] [PubMed] [Google Scholar]
- Masuda A, Price M, Anderson PL, Wendell JW. Disordered eating-related cognition and psychological flexibility as predictors of psychological health among college students. Behavior Modification. 2010;34:3–15. doi: 10.1007/s10862-011-9252-7. [DOI] [PubMed] [Google Scholar]
- Mennin DS, Ellard KK, Fresco DM, Gross JJ. United we stand: emphasizing commonalities across cognitive-behavioral therapies. Behavior Therapy. 2013;44:234–248. doi: 10.1016/j.beth.2013.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mogg K, Bradley BP. Selective orienting of attention to masked threat faces in social anxiety. Behavior Research and Therapy. 2002;40:1403–1414. doi: 10.1016/s0005-7967(02)00017-7. [DOI] [PubMed] [Google Scholar]
- Naragon-Gainey K, DeMarree KG. Structure and validity of measures of decentering and defusion. Psychological Assessment. 2017;29:935–954. doi: 10.1037/pas0000405. [DOI] [PubMed] [Google Scholar]
- Norton AR, Abbott MJ, Norberg MM, Hunt C. A systematic review of mindfulness and acceptance-based treatments for social anxiety disorder. Journal of Clinical Psychology. 2015;71(4):283–301. doi: 10.1002/jclp.22144. [DOI] [PubMed] [Google Scholar]
- Orsillo SM, Roemer L, Block J, Tull MT. Acceptance, Mindfulness, and Cognitive Behavioral Therapy: Comparisons, Contrasts and Application to Anxiety. In: Hayes SC, Follette VM, Linehan MM, editors. Mindfulness and acceptance: Expanding the cognitive-behavior tradition. New York: Guilford Press; 2004. [Google Scholar]
- Rapee RM, Heimberg RG. A cognitive-behavioral model of anxiety in social phobia. Behavior Research & Therapy. 1997;35:741–756. doi: 10.1016/S0005-7967(97)00022-3. [DOI] [PubMed] [Google Scholar]
- Safran JD, Segal ZV. Interpersonal process in cognitive therapy New. York: Basic Books; 1990. [Google Scholar]
- Schneier FR, Johnson J, Hornig CD, Liebowitz MR, Weissman MM. Social phobia comorbidity and morbidity in an epidemiologic sample. Archives of General Psychiatry. 1992;49:282–288. doi: 10.1001/archpsyc.1992.01820040034004. [DOI] [PubMed] [Google Scholar]
- Schneier FR, et al. Functional impairment in social phobia. Journal of Clinical Psychiatry. 1994;55:322–331. doi: 10.1192/bjp.172.1.70. [DOI] [PubMed] [Google Scholar]
- Spurr JM, Stopa L. Self-focused attention in social phobia and social anxiety. Clinical Psychology Review. 2002;22:947–975. doi: 10.1016/S0272-7358(02)00107-1. [DOI] [PubMed] [Google Scholar]
- Taylor CT, Bomyea J, Amir N. Attentional bias away from positive social information mediates the link between social anxiety and anxiety vulnerability to a social stressor. Journal of Anxiety Disorders. 2010;24:403–408. doi: 10.1016/j.janxdis.2010.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S. Meta-analysis of cognitive-behavioral treatment for social phobia. Journal of Behavior Therapy and Experimental Psychiatry. 1996;27:1–9. doi: 10.1016/0005-7916(95)00058-5. [DOI] [PubMed] [Google Scholar]
- Teasdale J. Emotional processing, three modes of mind and the prevention of relapse in depression. Behaviour Research and Therapy. 1999;37:S53–S77. doi: 10.1016/s0005-7967(99)00050-9. [DOI] [PubMed] [Google Scholar]
- Teasdale JD, Moore RG, Hayhurst H, Pope M, Williams S, Segal ZV. Metacognitive awareness and prevention of relapse in depression: empirical evidence. Journal of Consulting and Clinical Psychology. 2002;70:275–287. doi: 10.1037//0022-006x.70.2.275. [DOI] [PubMed] [Google Scholar]
- Treanor M. The potential impact of mindfulness on exposure and extinction learning in anxiety disorders. Clinical Psychology Review. 2011;31:617–625. doi: 10.1016/j.cpr.2011.02.003. [DOI] [PubMed] [Google Scholar]
- Turner SM, Beidel DC, Dancu CV. SPAI: Social phobia and anxiety inventory manual. Multi-Health Systems; New York: 1996. [Google Scholar]
- Turner SM, McCanna M, Beidel DC. Validity of the social avoidance and distress and fear of negative evaluation scales. Behaviour Research and Therapy. 1987;25:113–115. doi: 10.1016/0005-7967(87)90081-7. [DOI] [PubMed] [Google Scholar]
- Wells A, Davies MI. The thought control questionnaire: A measure of individual differences in the control of unwanted thoughts. Behaviour Research and Therapy. 1994;32:871–878. doi: 10.1177/0145445511398344. [DOI] [PubMed] [Google Scholar]
- Wells A, Papageorgiou C. Brief cognitive therapy for social phobia: a case series. Behavior Research & Therapy. 2001;39:713–720. doi: 10.1016/S0005-7967(00)00036-X. [DOI] [PubMed] [Google Scholar]
- Zettle RD, Rains JC, Hayes SC. Processes of change in acceptance and commitment therapy and cognitive therapy for depression: A mediation reanalysis of Zettle & Rains. Behavior Modification. 2011;35:265–283. doi: 10.1177/0145445511398344. [DOI] [PubMed] [Google Scholar]


