Abstract
STUDY QUESTION
Is there an association between physical and sexual abuse occurring in childhood or adolescence and risk of laparoscopically-confirmed endometriosis?
SUMMARY ANSWER
Early life sexual and physical abuse was associated with an increased risk of endometriosis.
WHAT IS KNOWN ALREADY
Previous studies have reported that physical and sexual abuse are associated with chronic pelvic pain (CPP). However, only one study has examined the association between childhood physical abuse and laparoscopically-confirmed endometriosis, and did not observe an association with endometriosis risk.
STUDY DESIGN, SIZE, DURATION
Prospective cohort study using data collected from 60 595 premenopausal women from 1989 to 2013 as part of the Nurses’ Health Study II cohort.
PARTICIPANTS/MATERIALS, SETTING, METHODS
Participants completed an exposure to violence victimization questionnaire in 2001. Cases were restricted to laparoscopically-confirmed endometriosis. Cox proportional hazards models were used to calculate rate ratios (RR) and 95% confidence intervals (CI).
MAIN RESULTS AND THE ROLE OF CHANCE
Three thousand three hundred and ninety-four cases of laparoscopically-confirmed endometriosis were diagnosed during 24 years of follow-up. Compared to those reporting no physical or sexual abuse, the risk of endometriosis was greater among those who experienced severe physical abuse (RR = 1.20; 95% CI = 1.06, 1.37) or severe sexual abuse (RR = 1.49; 95% CI = 1.24, 1.79). There was a 79% increased risk of laparoscopically-confirmed endometriosis for women reporting severe-chronic abuse of multiple types (95% CI = 1.44, 2.22). The associations between abuse and endometriosis were stronger among women presenting without infertility, a group that was more likely to have been symptomatic with respect to pain.
LIMITATIONS, REASONS FOR CAUTION
The violence exposure was recalled by the study participants and thus is subject to misclassification as well as recall bias for the cases who were diagnosed prior to 2001. However, our results were similar in a sensitivity analysis including only endometriosis cases incident after their violence history report. In addition, residual or unmeasured confounding is a possibility; however, we were able to adjust for a variety of potential early life confounders. Finally, selection bias is also a possibility if those who chose to return the violence questionnaire did so based jointly on abuse history and endometriosis risk.
WIDER IMPLICATIONS OF THE FINDINGS
Early life sexual and physical abuse was associated with an increased risk of endometriosis. Severity, chronicity and accumulation of types of abuse were associated with greater risk. Understanding the mechanisms underlying these relations may better define the biologic impacts of abuse and the related pathophysiology of endometriosis.
STUDY FUNDING/COMPETING INTEREST(s)
This work was supported by National Institute of Child Health and Human Development [Grant numbers HD48544, HD52473, HD57210 and CA50385] and the Atlanta Clinical and Translational Science Institute [Grant number ULRR025008]. The Nurses’ Health Study II is supported by the National Institutes of Health grant UM1 CA176726 from the National Cancer Institute. H.R.H. is supported by the National Cancer Institute, National Institutes of Health [Grant number K22 CA193860]. Authors report no conflict of interest.
Keywords: endometriosis, epidemiology, abuse, early life, pain
Introduction
Endometriosis affects about 10% of all reproductive-aged women, with signs and symptoms that include chronic pelvic pain and infertility (Halis et al., 2004; Sinaii et al., 2007). The etiology of endometriosis is not known, however, the implantation hypothesis is the most widely accepted (Sampson, 1927), supported by observations that retrograde menstruation and intraperitoneal spillage of viable endometrial cells occur frequently in cycling women and more commonly in those with genital outflow tract obstruction (Halme et al., 1984; Kruitwagen et al., 1991; Ugur et al., 1995). Retrograde menstruation and increased exposure to menstrual flow (lower parity, short menstrual cycle interval, earlier menarche, lean body mass) have been identified as risk factors for endometriosis (Giudice et al., 2004; Missmer et al., 2004a,b). Abuse during childhood and adolescence is a significant and major health problem in developing and industrialized countries (Jenny, 2008; Brown et al., 2009), with the Centers for Disease Control of the United States recognizing child abuse and neglect as childhood stressors that impact long-term health (Middlebrooks et al., 2008) and could play a role in the etiology and/or clinical signs of endometriosis through influences on inflammation (Bertone-Johnson et al., 2012), menstrual cycle characteristics (Kruitwagen et al., 1991; Romito et al., 2003; Zabin et al., 2005; Paras et al., 2009; Wise et al., 2009; Boynton-Jarrett et al., 2011), or chronic pelvic pain (Heim et al., 1998, 1999; Wuest, et al., 2008).
Few studies have examined the association between early life abuse and endometriosis. In a cross-sectional study among a headache clinic population, childhood maltreatment was common among women with pain conditions including endometriosis (Tietjen et al., 2010). A clinical case-report attributed endometriosis in a young woman to her adverse childhood experiences (Harrison et al., 2005). However, a recent study among women undergoing surgery for a variety of gynecologic conditions (e.g. pelvic mass, pelvic pain, irregular mense, infertility, tubal ligation) found no association between childhood physical abuse and endometriosis (Schliep et al., 2016). Previous studies have been among clinic-based populations, which limits their generalizability. In this study, we investigated whether physical and sexual abuse occurring in childhood and adolescence was associated with risk of laparoscopically-confirmed endometriosis in the Nurses’ Health Study II (NHSII) cohort, which includes a sample of women from across the United States.
Materials and methods
Ethical approval
This study was approved by the Institutional Review Board (IRB) of Brigham and Women’s Hospital.
Study population
The NHSII is an ongoing prospective cohort that was established in 1989 when 116 429 female registered nurses, ages 25–42, completed a questionnaire that collected information on demographic and lifestyle factors, anthropometric variables, and disease history. Follow-up questionnaires are sent biennially to participants updating information. Further details on the study have been provided elsewhere (Solomon et al., 1997).
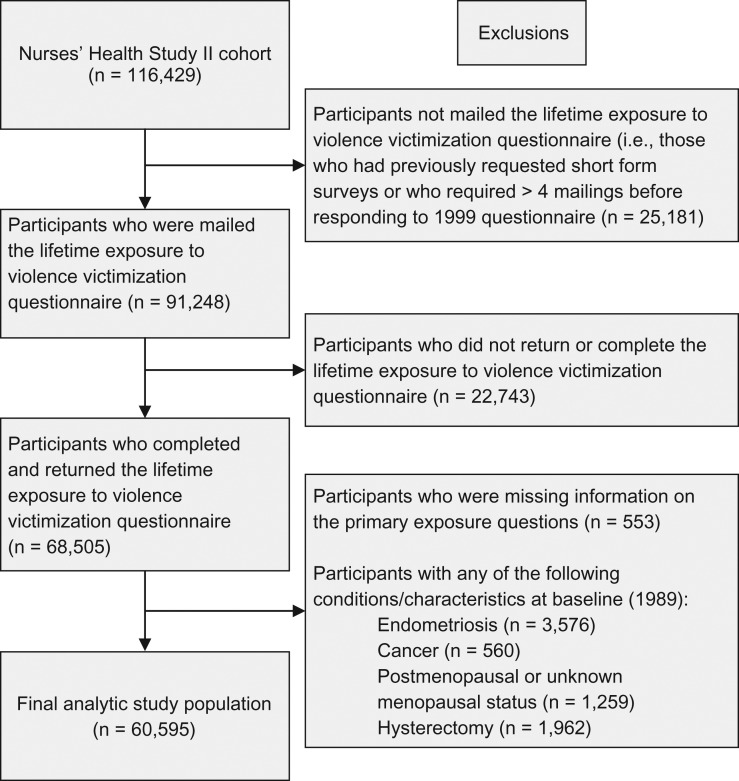
A questionnaire on lifetime exposure to violence victimization was sent to 91 248 study participants in 2001 (excluding those who had previously requested short form surveys or who required more than four mailings before responding to the 1999 questionnaire). Due to the potential safety concerns regarding mailing the questions, the IRB allowed only a single reminder postcard for those who did not immediately respond. Questionnaires were received from 68 505 women (a 75% response rate) (Boynton-Jarrett et al., 2011). Participants were excluded if they reported a history of endometriosis, infertility or cancer (other than non-melanoma skin cancer) before 1989 (cohort baseline). The analytical cohort was limited to women who were premenopausal and had intact uteri as endometriosis is rarely first diagnosed among postmenopausal women or subsequent to a hysterectomy. After these exclusions, 60 595 women remained (Fig. 1).
Figure 1.
Description of eligible study population and exclusions at baseline (1989).
Assessment of childhood and adolescent exposure to violence
The violence questionnaire covered three time periods: up to 11 years of age (childhood), 11–17 years of age (adolescence), and adulthood. We used the questionnaire to assess three types of abuse: ‘harsh and punitive parenting,’ physical abuse and sexual abuse.
Harsh and punitive parenting
Exposure to abuse in childhood was assessed using the Childhood Trauma Questionnaire (CTQ) short form (Bernstein et al., 1994). Abuse was assessed with the following five items: ‘People in my family hit me so hard that it left me with bruises and marks,’ ‘The punishments I received seemed cruel,’ ‘I was punished with a belt, a board, a cord, or some other hard object’, ‘People in my family said hurtful or insulting things to me,’ and ‘yelled and screamed at me.’ All items are rated on a 5-point Likert scale according to frequency (1 = never, 2 = rarely, 3 = sometimes, 4 = often, or 5 = very often), and a total CTQ score was derived by summing across items. The CTQ also included a single question to assess social support: ‘There was someone in my family who helped me feel that I was important or special’ and was rated as described above.
Physical abuse
Physical abuse by a parent, step-parent or adult guardian was assessed with the revised Conflict Tactics Scale (CTS) (Straus et al., 1995). Categories of physical activity abuse severity were created based on item factor loadings from principal-components factor analysis and the reported frequency of abuse of each item based on a 4-point scale according to frequency (1=never, 2=once, 3=a few times, 4=more than a few times) (Boynton-Jarrett et al., 2011). Physical abuse was categorized into four groups based on five questions: None, Mild (being ‘pushed, grabbed, or shoved’ at any frequency, or being ‘kicked, bitten, or punched’ once or ‘hit with something’ once), Moderate (being ‘hit with something’ more than once or ‘physically attacked’ once), Severe (being ‘kicked, bitten, or punched’ or ‘physically attacked’ more than once, or ‘choked or burned’ ever). Participants also reported whether their parent(s) or guardians spanked them for discipline (up to age 11). When spanking was examined in the context of a summary measure to capture physical and sexual abuse it did not load on either of the abuse factors and thus was considered to be empirically distinct from abuse, so those who reported only exposure to spanking for discipline were included in the reference group (Boynton-Jarrett et al., 2011).
Sexual abuse
Sexual abuse was measured by questions modified from the Sexual Experiences Survey (SES) (Koss et al., 1982). Participants reported frequency of the following exposures on a 3-point scale (never, once, more than once): ‘were you ever touched in a sexual way’ or ‘forced into any sexual activity’ by an adult or an older child, separately for childhood and adolescence. Sexual abuse was categorized into three groups: Mild (sexual touching), Moderate (forced sexual activity during either childhood [up to 11 years of age] or adolescence [11–17 years of age]), Severe (forced sexual activity during both childhood and adolescence) (Boynton-Jarrett et al., 2011).
Cumulative physical and sexual abuse history
A latent construct of cumulative violence exposure has previously been created in the NHSII using a principle component factor analysis methodology with oblique (promax) rotation (Hatcher, 1994; Boynton-Jarrett et al., 2011). Boynton-Jarrett et al. applied this factor analysis to the childhood and adolescent items in the CTS and the SES to create a summary measure capturing both chronicity and severity of physical and sexual abuse. Cumulative violence was categorized into five groups: Mild/Moderate Single Type, Mild-Multiple or Severe-Single Type(s), Moderate-Chronic or -Multiple Types, Severe-Chronic or –Multiple Types, and Severe Chronic and Multiple Types. The item related to spanking for discipline did not load on either of the abuse factors and was not included in this cumulative exposure variable. Categorization of this summary measure is described in Supplemental Table SI. A more detailed description of the types of abuse included in the cumulative abuse categories can be found elsewhere (Boynton-Jarrett et al., 2011; Riley et al., 2010).
Definition of endometriosis
Starting in 1993, participants were asked on each biennial questionnaire if they ‘had ever had physician-diagnosed endometriosis’ and if so, the date of diagnosis (before September 1989, September 1989–May 1991, etc. which corresponded to the follow-up periods) and whether it had been confirmed by laparoscopy. The validity of self-reported endometriosis in this cohort has been described previously (Missmer et al., 2004a,b). Briefly, a supplementary questionnaire, including permission to review medical records, was mailed to 200 women who were randomly selected from the then 1766 cases who had reported an incident diagnosis (response rate = 92%; n = 184). A diagnosis of endometriosis was confirmed by medical records in 96% of those who reported laparoscopic confirmation. However, a review of the medical records of those without laparoscopic confirmation indicated a clinical diagnosis of endometriosis in only 54%. In addition, a diagnosis of endometriosis at the time of hysterectomy was confirmed in 80% of the cases, but endometriosis was the primary indication for hysterectomy in only 6% of those for whom an indication was available. The primary indication for hysterectomy within our population was uterine fibroids, which have previously been associated with history of abuse. Therefore, we did not include as cases women whose initial diagnosis of endometriosis was incidentally made during a hysterectomy as this could erroneously create a case group that was a mix of endometriosis and uterine fibroids. Thus, we restricted our definition of incident diagnosis of endometriosis to women who reported laparoscopic confirmation of their diagnosis.
Statistical analyses
Participants contributed follow-up time from return of the 1989 baseline questionnaire, until report of laparoscopically-confirmed endometriosis, menopause, hysterectomy, cancer diagnosis (except non-melanoma skin cancer), loss to follow-up, death, or until return of the 2013 questionnaire. Multivariable Cox proportional hazards regression models with age and questionnaire period as the time scale were used to estimate hazard ratios (HR) and 95% confidence intervals (CI) using the corresponding no abuse category as the reference group.
We considered two covariate-adjusted models for each association between abuse and endometriosis; the first adjusted for early life characteristics (i.e. prior to or contemporaneous with abuse) (model 1; potential confounders) and the second additionally adjusted for adult characteristics (model 2; potential mediators). In model one, we adjusted for age, race, somatogram at age 5 (Stunkard et al., 1983), maternal education, paternal education, home ownership, and household income. In model two we further adjusted for the following characteristics that could vary between early life and development of endometriosis and that might be affected by abuse, which we considered potential mediators: body mass index (BMI), physical activity, age at menarche, cycle length between ages 18–22, oral contraceptive (OC) use, parity, infertility, grams of alcohol per week, smoking pack-years, adult physical abuse and adult sexual abuse (McFarlane et al., 1992). In model three, we further adjusted for social support in childhood. Covariates were updated whenever new information was available from the biennial questionnaires.
Since women with endometriosis who have not reported infertility are more likely to have been symptomatic with respect to pain (otherwise they would not have undergone laparoscopic surgery), while women reporting infertility are more likely asymptomatic and may have been diagnosed with endometriosis during an infertility evaluation, we examined if the associations were modified by fertility status (defined as attempting to conceive for >12 months without success). We also assessed effect modification by social support in childhood (very often/often, sometimes/rarely/never), as research suggests that parental or caretaker support may protect against or ameliorate the potential negative impacts of victimization.(Repetti et al., 2002) Effect modification was assessed with a likelihood ratio tests comparing models with the exposure variable, potential modifier, and the interaction terms to those with the main effects only. In sensitivity analyses, the study start was redefined such that participants contributed person-time from return of the violence victimization questionnaire in 2001, thus including only cases of endometriosis that were incident after the violence victimization questionnaire was complete to gauge the impact of recall bias. Statistical analyses were performed using SAS Version 9.4 (SAS Institute Inc., Cary, NC).
Results
During 875 622 person-years of follow-up contributed by 60 595 women, 3394 incident cases of laparoscopically-confirmed endometriosis were reported. Thirty-two percent of women reported some level of child/adolescent physical abuse only, 12% reported child/adolescent sexual abuse only, and 21% reported child/adolescent physical and sexual abuse (Table I). Women who experienced abuse had a slightly higher BMI and were more likely to smoke (Table II). The distribution of risk factors for endometriosis between the violence questionnaire responders vs. non-responders did not differ appreciably (Supplemental Table SII).
Table I.
Prevalence of abuse in childhood and adolescence (reported in 2001) among Nurses’ Health Study II participants (n = 60 595).
| N (%) | |
|---|---|
| Abuse Type | |
| None | 21 256 (35.1) |
| Physical Abuse only | 19 443 (32.1) |
| Sexual Abuse only | 7197 (11.9) |
| Physical and Sexual Abuse | 12 699 (21.0) |
| Abuse Severity | |
| Severity of Physical Abuse | |
| None | 28 453 (47.0) |
| Mild Physical Abuse | 11 387 (18.8) |
| Moderate Physical Abuse | 15 745 (26.0) |
| Severe Physical Abuse | 5010 (8.3) |
| Severity of Sexual Abuse | |
| None | 40 699 (67.2) |
| Sexual Touching as Child or Adolescent | 13 382 (22.1) |
| Forced Sexual Activity as Child or Adolescent | 4985 (8.2) |
| Forced Sexual Activity as Child & Adolescent | 1529 (2.5) |
| Childhood Trauma Scale Scorea | |
| 5 (None) | 6946 (11.5) |
| 6–10 | 32 594 (53.8) |
| 11–15 | 13 745 (22.7) |
| 16–20 | 5191 (8.6) |
| 21–25 | 2119 (3.5) |
| Cumulative Abuse Historyb | |
| No Exposure to Violence | 21 256 (35.1) |
| Mild/Moderate Single Type | 22 712 (37.5) |
| Mild-Multiple Types or Severe-Single Type | 9203 (15.2) |
| Moderate-Chronic or-Multiple Types | 4589 (7.6) |
| Severe-Chronic or-Multiple Types | 1714 (2.8) |
| Severe-Chronic and Multiple Types | 1121 (1.8) |
aExposure to ‘harsh and punitive parenting’ in childhood (prior to age 11) was assessed using items from the Childhood Trauma Questionnaire short form.
bSummary of childhood and adolescent physical abuse measured by the Revised Conflict Tactics Scale and sexual abuse measured by the Sexual Experiences Survey.
Table II.
Baseline characteristics according to total abuse in childhood/adolescence among Nurses’ Health Study II participants (n = 60 595).
| Characteristic | Cumulative exposure to violence in early lifea | |||||
|---|---|---|---|---|---|---|
| No abuse (n = 21 256) | Mild/Moderate or Single (n = 22 712) | Mild-multiple or Severe-single (n = 9203) | Moderate-chronic or multiple (n = 4589) | Severe-chronic or multiple (n = 1714) | Severe chronic and multiple (n = 1121) | |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |
| BMI | 23.6 (4.6) | 23.8 (4.8) | 24.2 (5.0) | 24.4 (5.4) | 24.7 (5.6) | 25.3 (6.1) |
| Parity | 1.40 (1.20) | 1.45 (1.21) | 1.47 (1.21) | 1.43 (1.20) | 1.47 (1.19) | 1.43 (1.24) |
| Physical activity (METs/week) | 24.0 (34.5) | 24.2 (34.9) | 23.6 (34.3) | 26.1 (38.0) | 26.3 (39.4) | 31.1 (45.1) |
| Alcohol intake (g/day) | 3.0 (5.7) | 3.3 (6.2) | 3.5 (6.6) | 3.4 (6.5) | 3.1 (6.1) | 3.0 (5.8) |
| % | % | % | % | % | % | |
| Race | ||||||
| White | 96 | 95 | 94 | 93 | 93 | 90 |
| Cigarette smoking | ||||||
| Never | 73 | 67 | 62 | 56 | 56 | 54 |
| Past | 18 | 22 | 24 | 27 | 27 | 27 |
| Current | 9 | 11 | 13 | 16 | 17 | 19 |
| Age at menarche | ||||||
| <12 | 23 | 23 | 26 | 26 | 30 | 30 |
| 12 | 31 | 31 | 30 | 30 | 26 | 29 |
| 13 | 29 | 28 | 27 | 26 | 26 | 23 |
| >13 | 18 | 18 | 17 | 19 | 18 | 19 |
| Menstrual cycle length at age 18 | ||||||
| <26 days | 10 | 10 | 11 | 12 | 13 | 15 |
| 26–31 days | 65 | 67 | 66 | 66 | 65 | 62 |
| 32–50 days | 19 | 18 | 18 | 16 | 16 | 16 |
| >51 days | 6 | 5 | 5 | 6 | 7 | 7 |
| Oral contraceptive use | ||||||
| Ever | 81 | 83 | 86 | 86 | 87 | 87 |
| Never | 19 | 17 | 14 | 14 | 13 | 13 |
| Infertility | ||||||
| Yes | 16 | 16 | 16 | 17 | 18 | 19 |
| No | 84 | 84 | 84 | 83 | 82 | 81 |
aThe violence measure incorporated abuse type (physical and/or sexual abuse), chronicity and severity. MET; metabolic equivalent.
Severity of physical abuse, sexual abuse and the CTQ score were positively associated with the incidence of endometriosis in a dose–response manner. Both physical and sexual abuse history were associated with a higher incidence of endometriosis compared to those who never reported abuse. In the fully adjusted model, we observed an increased risk of endometriosis with exposure to physical abuse only (HR, 1.10; 95% CI, 1.01–1.20) and sexual abuse only (HR, 1.15; 95% CI, 1.03–1.30). The highest risk of endometriosis was observed among women with a combination of physical and sexual abuse history (HR, 1.31; 95% CI 1.19–1.45) (Table III).
Table III.
Hazard ratios of laparoscopically-confirmed endometriosis according to severity, chronicity and type of violence exposure in childhood/adolescence among Nurses’ Health Study II participants (1989–2013, n = 60 595).
| Abuse characteristics | Woman-years | Cases | Hazard Ratio (95% confidence interval) | |||
|---|---|---|---|---|---|---|
| Age-adjusted | Model 1a | Model 2b | Model 3c | |||
| Abuse Type | ||||||
| None | 315616 | 1066 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Physical Abuse only | 280916 | 1071 | 1.13 (1.03–1.23) | 1.12 (1.03–1.22) | 1.13 (1.03–1.23) | 1.10 (1.01–1.20) |
| Sexual Abuse only | 102278 | 407 | 1.17 (1.04–1.31) | 1.16 (1.04–1.31) | 1.16 (1.04–1.31) | 1.15 (1.03–1.30) |
| Physical and Sexual Abuse | 176813 | 850 | 1.41 (1.29–1.55) | 1.39 (1.27–1.52) | 1.36 (1.24–1.50) | 1.31 (1.19–1.45) |
| Abuse Severity | ||||||
| Severity of Physical Abuse | ||||||
| None | 417894 | 1473 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Mild Physical abuse | 165887 | 604 | 1.03 (0.94–1.14) | 1.03 (0.94–1.13) | 1.03 (0.94–1.14) | 1.02 (0.92–1.12) |
| Moderate Physical abuse | 224079 | 984 | 1.24 (1.14–1.34) | 1.23 (1.14–1.34) | 1.24 (1.14–1.34) | 1.20 (1.11–1.31) |
| Severe Physical Abuse | 67762 | 333 | 1.39 (1.24–1.57) | 1.36 (1.20–1.53) | 1.28 (1.13–1.44) | 1.20 (1.06–1.37) |
| Ptrend | <.0001 | <.0001 | <.0001 | <.0001 | ||
| Severity of Sexual Abuse | ||||||
| None | 596532 | 2137 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Sexual Touching as Child or Adol | 189465 | 787 | 1.15 (1.06–1.25) | 1.15 (1.06–1.25) | 1.14 (1.05–1.24) | 1.13 (1.04–1.23) |
| Forced Sexual Activity as Child or Adol | 69604 | 345 | 1.38 (1.23–1.55) | 1.35 (1.20–1.51) | 1.30 (1.16–1.47) | 1.28 (1.13–1.43) |
| Forced Sexual Activity as Child & Adol | 20022 | 125 | 1.69 (1.41–2.02) | 1.64 (1.37–1.97) | 1.56 (1.30–1.87) | 1.49 (1.24–1.79) |
| Ptrend | <.0001 | <.0001 | <.0001 | <.0001 | ||
| Childhood Trauma Scale Scored | ||||||
| 5 (None) | 99621 | 316 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| 6–10 | 480247 | 1677 | 1.09 (0.97–1.23) | 1.09 (0.96–1.23) | 1.13 (1.00–1.28) | 1.12 (0.99–1.27) |
| 11–15 | 197006 | 869 | 1.38 (1.21–1.56) | 1.36 (1.20–1.55) | 1.38 (1.21–1.58) | 1.35 (1.18–1.55) |
| 16–20 | 71619 | 394 | 1.68 (1.45–1.95) | 1.65 (1.42–1.91) | 1.64 (1.41–1.91) | 1.58 (1.35–1.85) |
| 21–25 | 27128 | 138 | 1.60 (1.30–1.95) | 1.54 (1.26–1.89) | 1.52 (1.24–1.86) | 1.46 (1.18–1.80) |
| Ptrend | <.0001 | <.0001 | <.0001 | <.0001 | ||
| Cumulative Abuse Historye | ||||||
| No Exposure to Violence | 315616 | 1066 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Mild/Moderate Single Type | 328063 | 1252 | 1.12 (1.03–1.22) | 1.12 (1.03–1.22) | 1.13 (1.04–1.23) | 1.12 (1.03–1.21) |
| Mild-Multiple or Severe-Single Type(s) | 131011 | 532 | 1.21 (1.08–1.34) | 1.19 (1.08–1.33) | 1.19 (1.07–1.33) | 1.17 (1.05–1.30) |
| Moderate-Chronic or-Multiple Types | 63765 | 323 | 1.48 (1.31–1.68) | 1.45 (1.28–1.65) | 1.41 (1.24–1.60) | 1.36 (1.19–1.55) |
| Severe-Chronic or-Multiple Types | 23052 | 121 | 1.53 (1.27–1.85) | 1.49 (1.23–1.80) | 1.40 (1.15–1.70) | 1.34 (1.10–1.62) |
| Severe-Chronic and Multiple Types | 14115 | 100 | 2.05 (1.67–2.52) | 1.98 (1.61–2.44) | 1.89 (1.53–2.34) | 1.79 (1.44–2.22) |
| Ptrend | <.0001 | <.0001 | <.0001 | <.0001 | ||
Note: Adol=adolescent.
aModel 1: Adjusted for age (months), race (white, black, Asian, multiple races, other/unknown), somatogram at age 5 (figure 1, 2, 3, 4 or ≥5), mother’s education (less than high school, completed high school, more than high school), father’s education (less than high school, completed high school, more than high school), home ownership in infancy (no, yes), and household income in 2001 (<$50 000, $50 000–$99 999, ≥$100 000).
bModel 2: Adjusted for all variables in Model 1 and BMI (<19, 19–20.4, 20.5–21.9, 22–24.9, 25–29.9, ≥30), physical activity (METS/week <3, 3–<9, 9–<18, 18–<27, 27–<42, ≥42), age at menarche (<10, 10, 11, 12, 13, 14, 15, >15), cycle length between ages 18–22 (<26 days, 26–31 days, 32–50 days, >50 days and irregular cycles), OCP use (never, past, current), parity (nulliparous, 1, 2, 3, >3), infertility (no, yes), grams of alcohol per week (0, >0–<5, 5–<10, 10–<15, ≥15), smoking pack-years (0, >0–5, >5–10, >10–15, >15–20, ≥20), adult physical abuse (none, any), and adult sexual abuse (none, any).
cModel 3: Adjusted for all variables in Model 2 and social support during childhood (very often, often, sometimes, rarely, never).
dExposure to ‘harsh and punitive parenting’ in childhood (prior to age 11) was assessed using items from the Childhood Trauma Questionnaire short form
eSummary of childhood and adolescent physical abuse measured by the Revised Conflict Tactics Scale and sexual abuse measured by the Sexual Experiences Survey.
When we considered severity of physical abuse, we observed an increased risk of endometriosis in women with history of moderate (HR, 1.20; 95% CI, 1.11–1.31) and of severe physical abuse (HR, 1.20; 95% CI, 1.06–1.37). When we evaluated severity of sexual abuse by exposure time period, we observed the highest risk for endometriosis among women with history of forced sexual activity during both childhood and adolescence (HR, 1.49; 95% CI, 1.24–1.79). Results were analogous when we repeated our analyses using the CTS score (Table III).
Cumulative abuse history – which captures type, severity, and chronicity of abuse – was also observed to be associated with risk of endometriosis (Table III). Compared to those who never reported abuse events (physical or sexual), there was a 12% greater risk of endometriosis for women reporting one episode of mild/moderate abuse (95% CI, 1.03–1.21), a 17% greater risk (95% CI, 1.05–1.30) for mild-multiple or severe-single type of abuse, a 36% greater risk (95% CI, 1.19–1.55) for moderate-chronic or-multiple types of abuse, a 34% greater risk (95% CI, 1.10–1.62) for severe-chronic or multiple types of abuse, and a 79% greater risk (95% CI, 1.44–2.22) for those with severe-chronic abuse and multiple types of abuse.
The associations between abuse and endometriosis differed by infertility history with interactions observed for sexual abuse (pinteraction < 0.0001) and cumulative abuse history (pinteraction = 0.01). For sexual abuse, the magnitude of the effects was increased considerably among those who never reported infertility with a HR of 1.72 for those reporting forced sexual abuse as a child and adolescent (95% CI, 1.41–2.11). Similar results were observed for cumulative abuse history with increased risks of endometriosis for all levels of cumulative abuse categories among women who never reported infertility (Table IV). Among those who reported infertility, the risk for endometriosis was not increased in the fully adjusted models for any form of abuse; although there was the suggestion of increased risks for physical and cumulative abuse but of a lesser magnitude than observed among the women who never reported infertility.
Table IV.
Hazard ratios of laparoscopically-confirmed endometriosis and abuse severity (physical abuse or sexual abuse) and cumulative abuse history, stratified by infertility history among Nurses’ Health Study II participants (1989–2013).
| Ever reported infertility (n = 655) | Never reported infertility (n = 2622) | phetd | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases | Woman- years | Model 1a HR (95% CI) |
Model 2b HR (95% CI) |
Model 3c RR (95% CI) |
Cases | Woman- years | Model 1a HR (95% CI) |
Model 2b HR (95% CI) |
Model 3c HR (95% CI) |
||
| Physical Abuse | |||||||||||
| None | 290 | 19641 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1132 | 383606 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 0.30 |
| Mild | 129 | 8196 | 1.15 (0.92–1.43) | 1.16 (0.93–1.46) | 1.13 (0.90–1.41) | 457 | 151592 | 1.02 (0.91–1.14) | 1.03 (0.92–1.15) | 1.01 (0.91–1.13) | |
| Moderate | 178 | 10683 | 1.17 (0.96–1.43) | 1.26 (1.03–1.55) | 1.22 (0.99–1.50) | 772 | 205780 | 1.25 (1.14–1.37) | 1.24 (1.13–1.36) | 1.21 (1.10–1.33) | |
| Severe | 58 | 3745 | 1.16 (0.85–1.56) | 1.25 (0.91–1.71) | 1.16 (0.84–1.61) | 261 | 61323 | 1.40 (1.22–1.60) | 1.33 (1.15–1.52) | 1.25 (1.08–1.45) | |
| Ptrend | 0.11 | 0.02 | 0.09 | <.0001 | <.0001 | <.0001 | |||||
| Sexual abuse | |||||||||||
| None | 455 | 28155 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1614 | 547479 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | <0.0001 |
| Sexual Touching as Child or Adolescent | 131 | 9140 | 0.94 (0.77–1.15) | 0.98 (0.80–1.21) | 0.96 (0.78–1.19) | 624 | 173634 | 1.20 (1.09–1.31) | 1.19 (1.08–1.30) | 1.18 (1.07–1.29) | |
| Forced Sexual Activity as Child or Adol | 55 | 3806 | 0.93 (0.69–1.25) | 1.07 (0.79–1.45) | 1.03 (0.75–1.40) | 276 | 63101 | 1.45 (1.28–1.65) | 1.41 (1.23–1.60) | 1.38 (1.21–1.57) | |
| Forced Sexual Activity as Child & Adol | 14 | 1164 | 0.86 (0.50–1.49) | 0.90 (0.51–1.57) | 0.83 (0.47–1.46) | 108 | 18086 | 1.90 (1.56–2.31) | 1.80 (1.47–2.20) | 1.72 (1.41–2.11) | |
| Ptrend | 0.42 | 0.99 | 0.70 | <.0001 | <.0001 | <.0001 | |||||
| Cumulative abusee history | |||||||||||
| None | 228 | 14687 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 806 | 289441 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 0.01 |
| Mild/Moderate Single Type | 247 | 15448 | 1.05 (0.87–1.27) | 1.07 (0.88–1.30) | 1.04 (0.85–1.27) | 963 | 301878 | 1.13 (1.03–1.24) | 1.14 (1.04–1.25) | 1.13 (1.03–1.24) | |
| Mild-multiple or Severe Single Types | 91 | 6524 | 0.97 (0.75–1.25) | 1.09 (0.84–1.42) | 1.04 (0.80–1.36) | 420 | 119673 | 1.24 (1.10–1.40) | 1.24 (1.10–1.40) | 1.22 (1.08–1.37) | |
| Moderate-Chronic or Multiple Types | 58 | 3438 | 1.2 (0.88–1.64) | 1.38 (1.00–1.91) | 1.30 (0.93–1.80) | 250 | 57989 | 1.49 (1.29–1.72) | 1.46 (1.26–1.69) | 1.41 (1.21–1.64) | |
| Severe-Chronic or Multiple Types | 19 | 1364 | 1 (0.61–1.63) | 1.10 (0.66–1.82) | 1.01 (0.60–1.68) | 98 | 20696 | 1.61 (1.3–1.99) | 1.55 (1.25–1.92) | 1.49 (1.20–1.86) | |
| Severe Chronic and Multiple Types | 12 | 803 | 1.16 (0.63–2.12) | 1.29 (0.69–2.41) | 1.14 (0.61–2.16) | 85 | 12625 | 2.3 (1.83–2.88) | 2.15 (1.71–2.71) | 2.05 (1.62–2.59) | |
| Ptrend | 0.51 | 0.11 | 0.33 | <.0001 | <.0001 | <.0001 | |||||
Note: HR = hazard ratio; CI = 95% confidence interval; Adol = adolescent.
aModel 1: Adjusted for age (months), race (white, black, Asian, multiple races, other/unknown), somatogram at age 5 (figure 1, 2, 3, 4 or ≥5), mother’s education (less than high school, completed high school, more than high school), father’s education (less than high school, completed high school, more than high school), home ownership in infancy (no, yes), and household income in 2001 (<$50 000, $50 000–$99 999, ≥$100 000).
bModel 2: Adjusted for all variables in Model 1 and BMI (<19, 19–20.4, 20.5–21.9, 22–24.9, 25–29.9, ≥30), physical activity (METS/week <3, 3–<9, 9–<18, 18–<27, 27–<42, ≥42), age at menarche (<10, 10, 11, 12, 13, 14, 15, >15), cycle length between ages 18–22 (<26 days, 26–31 days, 32–50 days, >50 days and irregular cycles), OC use (never, past, current), parity (nulliparous, 1, 2, 3, >3), infertility (no, yes), grams of alcohol per week (0, >0–<5, 5–<10, 10–<15, ≥15), smoking pack-years (0, >0–5, >5–10, >10–15, >15–20, ≥20), adult physical abuse (none, any), and adult sexual abuse (none, any).
cModel 3: Adjusted for all variables in Model 2 and social support during childhood (very often, often, sometimes, rarely, never).
dLikelihood ratio test (LRT) P-values, tests for heterogeneity between physical abuse, sexual abuse, and cumulative abuse, and infertility.
eSummary of childhood and adolescent physical abuse measured by the Revised Conflict Tactics Scale and sexual abuse measured by the Sexual Experiences Survey.
No statistically or clinically interactions were observed by social support in childhood for any of the abuse exposures (all pinteraction > 0.05).
In sensitivity analyses, the associations were not impacted by recall bias, as we observed similar associations, with less stable effect estimates in the most extreme categories of abuse due to small numbers, between abuse and endometriosis risk when we restricted analyses to include only cases of endometriosis reported (n = 584) following return of the 2001 violence questionnaire (Table V).
Table V.
Hazard ratios of laparoscopically-confirmed endometriosis according to severity, chronicity, and type of violence exposure in childhood/adolescence among Nurses’ Health Study II participants (2001–2013, n = 38 322).
| Abuse characteristics | Woman-years | Cases | Hazard ratio (95% confidence interval) | ||
|---|---|---|---|---|---|
| Model 1a | Model 2b | Model 3c | |||
| Abuse Type | |||||
| None | 96232 | 186 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Physical Abuse only | 83049 | 161 | 1.02 (0.82–1.26) | 1.01 (0.82–1.26) | 0.98 (0.79–1.22) |
| Sexual Abuse only | 29364 | 81 | 1.43 (1.10–1.86) | 1.44 (1.11–1.88) | 1.42 (1.09–1.85) |
| Physical and Sexual Abuse | 49965 | 156 | 1.60 (1.28–1.98) | 1.59 (1.27–1.99) | 1.50 (1.19–1.89) |
| Abuse Severity | |||||
| Severity of Physical Abuse | |||||
| None | 125596 | 267 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Mild Physical abuse | 49574 | 99 | 0.96 (0.76–1.21) | 0.95 (0.75–1.21) | 0.93 (0.74–1.18) |
| Moderate Physical abuse | 65044 | 172 | 1.24 (1.02–1.50) | 1.23 (1.01–1.49) | 1.17 (0.96–1.43) |
| Severe Physical Abuse | 18396 | 46 | 1.17 (0.85–1.60) | 1.09 (0.79–1.51) | 0.97 (0.69–1.36) |
| Ptrend | 0.05 | 0.10 | 0.38 | ||
| Severity of Sexual Abuse | |||||
| None | 179281 | 347 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Sexual Touching as Child or Adol | 54274 | 146 | 1.37 (1.13–1.67) | 1.39 (1.14–1.69) | 1.37 (1.12–1.67) |
| Forced Sexual Activity as Child or Adol | 19865 | 74 | 1.92 (1.49–2.48) | 1.92 (1.48–2.49) | 1.86 (1.43–2.42) |
| Forced Sexual Activity as Child & Adol | 5190 | 17 | 1.56 (0.95–2.58) | 1.40 (0.84–2.32) | 1.40 (0.85–2.32) |
| Ptrend | <0.0001 | <0.0001 | <0.0001 | ||
| Childhood Trauma Scale Scored | |||||
| 5 (None) | 28910 | 52 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| 6–10 | 144916 | 291 | 1.08 (0.81–1.46) | 1.11 (0.82–1.49) | 1.10 (0.82–1.49) |
| 11–15 | 57844 | 164 | 1.55 (1.13–2.13) | 1.55 (1.13–2.13) | 1.50 (1.08–2.08) |
| 16–20 | 20090 | 68 | 1.77 (1.22–2.54) | 1.73 (1.20–2.51) | 1.58 (1.07–2.33) |
| 21–25 | 6851 | 9 | 0.72 (0.35–1.48) | 0.68 (0.33–1.39) | 0.60 (0.29–1.25) |
| Ptrend | 0.001 | 0.005 | 0.07 | ||
| Cumulative Abuse Historye | |||||
| No Exposure to Violence | 96232 | 186 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Mild/Moderate Single Type | 96764 | 198 | 1.07 (0.87–1.31) | 1.08 (0.88–1.32) | 1.06 (0.86–1.30) |
| Mild-Multiple or Severe-Single Type(s) | 37910 | 106 | 1.47 (1.15–1.87) | 1.47 (1.15–1.88) | 1.42 (1.11–1.82) |
| Moderate-Chronic or-Multiple Types | 17982 | 71 | 1.95 (1.47–2.57) | 1.96 (1.47–2.60) | 1.84 (1.37–2.47) |
| Severe-Chronic or-Multiple Types | 6184 | 13 | 1.11 (0.63–1.96) | 1.06 (0.60–1.88) | 0.99 (0.55–1.76) |
| Severe-Chronic and Multiple Types | 3538 | 10 | 1.42 (0.74–2.73) | 1.36 (0.70–2.63) | 1.23 (0.63–2.39) |
| Ptrend | <0.0001 | 0.0001 | 0.002 | ||
Note: Adol = adolescent.
aModel 1: Adjusted for age (months), race (white, black, Asian, multiple races, other/unknown), somatogram at age 5 (figure 1, 2, 3, 4 or ≥5), mother’s education (less than high school, completed high school, more than high school), father’s education (less than high school, completed high school, more than high school), home ownership in infancy (no, yes), household income in 2001 (<$50 000, $50 000–$99 999, ≥$100 000), and social support during childhood (very often, often, sometimes, rarely, never).
bModel 2: Adjusted for all variables in Model 1 and BMI (<19, 19–20.4, 20.5–21.9, 22–24.9, 25–29.9, ≥30), physical activity (METS/week <3, 3–<9, 9–<18, 18–<27, 27–<42, ≥42), age at menarche (<10, 10, 11, 12, 13, 14, 15, >15), cycle length between ages 18–22 (<26 days, 26–31 days, 32–50 days, >50 days and irregular cycles), OCP use (never, past, current), parity (nulliparous, 1, 2, 3, >3), infertility (no, yes), grams of alcohol per week (0, >0–<5, 5-<10, 10–<15, ≥15), smoking pack years (0, >0–5, >5–10, >10–15, >15–20, ≥20), adult physical abuse (none, any), and adult sexual abuse (none, any).
cModel 3: Adjusted for all variables in Model 2 and social support during childhood (very often, often, sometimes, rarely, never).
dExposure to ‘harsh and punitive parenting’ in childhood (prior to age 11) was assessed using items from the Childhood Trauma Questionnaire short form
eSummary of childhood and adolescent physical abuse measured by the Revised Conflict Tactics Scale and sexual abuse measured by the Sexual Experiences Survey.
Discussion
In this large cohort study, we observed an association between exposure to violence during childhood and adolescence and endometriosis risk. Both physical and sexual abuse were associated with endometriosis risk, with abuse severity, chronicity and accumulation of types of abuse each associated with increasing risk in a dose–response manner. In addition, we observed strong evidence that the association differed by fertility status, with a robust association among women who never reported infertility.
Reproductive factors, including early and late age at menarche and early onset of perimenopause have been associated with violence (Allsworth et al., 2001; Wise et al., 2009). In addition, a previous study within the NHSII cohort reported an association between abuse during childhood/adolescence and uterine fibroids (Boynton-Jarrett et al., 2011). To our knowledge this is the second and largest study to evaluate the association between adverse childhood/adolescent experiences and incidence of laparoscopically-confirmed endometriosis. Schliep et al. examined the association between childhood and adult physical abuse and adult sexual abuse, and risk of gynecologic disorders among 495 women scheduled to undergo a diagnostic and/or therapeutic laparoscopy or laparotomy. No association was observed between any of the types of abuse examined and laparoscopically-confirmed endometriosis, fibroids, or ovarian cysts, while an association was observed between child and adult physical abuse and higher risk of pelvic adhesions. Limitations of this study included that only women who were undergoing gynecologic surgery, with surgical indications including pelvic pain (42%), pelvic mass (15%), irregular menses (12%), uterine fibroids (10%), tubal ligation (10%) and infertility (7%), were included in the study population. Thus in calculating effect estimates, the analysis compared women with endometriosis to women without endometriosis, but these women were not ‘healthy’ women. Rather, these women without endometriosis had gynecologic pathology indicating their surgery. For example, fibroids, adhesions or ovarian cysts and some of these conditions (e.g. fibroids) have been previously associated with childhood trauma (Boynton-Jarrett et al., 2011). In contrast to this clinic and surgical-based population, the population-based reference group used by our study may explain the differing associations observed.
Previous studies have reported that physical and sexual abuse are associated with chronic pelvic pain (CPP) (Heim et al., 1998, 1999; Wuest et al., 2008). Among women who have laparoscopically-confirmed endometriosis, women who have not reported infertility are more likely to have been symptomatic with respect to pain while a large portion of women reporting infertility are likely asymptomatic and may have been diagnosed with endometriosis during an infertility evaluation. These women may have infertility as a result of endometriosis or, alternatively, the finding of endometriosis upon an infertility work-up with laparoscopic surgery may be incidental. Because of the differences in symptoms and clinical presentation between fertile and infertile women we treated infertility as an effect modifier and observed an interaction by fertility status. Among women who never reported infertility, increased risks of endometriosis were observed for each measure of abuse, with the strongest increased risks observed for sexual abuse and cumulative abuse history. In contrast, among women who reported infertility, no association was observed with sexual abuse, and slightly increased risks of endometriosis were observed with physical and cumulative abuse. However, these results were based on small numbers in this group, and a null association cannot be excluded. Abuse during childhood has been associated with sub-fertility (Harville et al., 2013; Jacobs et al., 2015). It is plausible that the suggestion of greater risk of endometriosis within this infertile group, among whom pain was often not the indication for diagnosis, is driven by an association between abuse during childhood and fertility dysregulation independent of endometriosis.
Early life abuse may influence endometriosis through both its impact on pain symptoms and infertility diagnosis. Exposure to childhood stressors has been associated with neuroendocrine disruptions, including altered functioning of the hypothalamic–pituitary–adrenal axis and elevated cortisol levels (Teicher et al., 2003), impacting regulation of hypothalamic gonadotropin-releasing hormone and associated with earlier natural menopause (Allsworth et al., 2001). Although, our findings of a stronger association between abuse and endometriosis that presents with pain symptoms are consistent with previous studies that indicate early life stress may be related to the development of pain syndromes including fibromyalgia, CFS, chronic pelvic pain and vulvodynia (Heim et al., 1998, 1999, 2009; Low et al., 2012; Nater et al., 2011; Ross, 2005; Weissbecker et al., 2006; Wuest et al., 2008).
Our findings of a stronger association between early life abuse and pain-associated endometriosis suggest that the mechanism(s) underlying the association between abuse and endometriosis could share similarities with CPP and other pain syndromes. A growing body of literature suggests that early traumatic experiences induce persistent sensitization of the central stress response systems, including dysregulation of the hypothalamic–pituitary–adrenal (HPA) axis (Heim et al., 1998, 2004). Aberration in the HPA axis leading to hypocortisolism has been suggested to result in a symptom triad of high stress sensitivity, fatigue and pain (Heim et al., 2000; Fries et al., 2005). In the context of endometriosis this is supported by reports that women with endometriosis have lower levels of salivary cortisol than healthy volunteers (Petrelluzzi et al., 2008; Quinones et al., 2015). In addition, early life traumatic stress, either through hypocortisolism or other mechanisms, has also been associated with the inflammatory response (Suzuki et al., 1997; Nguyen et al., 1998; Deak et al., 2005; Pace et al., 2006, 2012; Okuyama et al., 2007; Bauer et al., 2010; Brenhouse et al., 2011; Bertone-Johnson et al., 2012). Whether the pain symptoms associated with endometriosis are directly attributable to endometriotic lesions has not been determined, however, regardless of the mechanisms underlying the chronic pain in endometriosis, inflammation has been suggested to play an important role in the relationship between pain and endometriosis (Stratton et al., 2011).
Limitations of our study need to be considered. Our study population was primarily Caucasian female nurses who were middle-aged (36–53 years) when answering the violence questionnaire. The violence exposure was recalled by the study participants and thus is subject to misclassification, and recall bias for the cases who were diagnosed prior to 2001. In addition, selection bias is also a possibility if those who chose to return the violence questionnaire did so based jointly on abuse history and endometriosis risk. However, our results were similar in a sensitivity analysis including only endometriosis cases incident after their violence history report. In addition, adult recall of childhood abuse has been shown to be valid (Widom et al., 1996) and the levels of abuse reported by our participants are consistent with national surveys (Briere et al., 2003).
The strengths of the study include its prospective design across 24 years of follow-up among a large cohort with excellent response rates, detailed information on abuse history, many important covariates updated at 2-year intervals, and over 3000 laparoscopically-confirmed cases of endometriosis. We hypothesized that reproductive factors, including menstrual cycle length, age at menarche, OC use, parity, age at first birth and adult abuse could be potential mediators for the association between abuse and endometriosis. However, this association remained with little attenuation even after adjustment for early life, lifestyle, reproductive factors, and adult abuse.
Within this large prospective cohort of female nurses, we observed a strong, dose–response association between severity and chronicity of abuse in childhood and adolescence and endometriosis risk that was independent of demographic and potential confounding factors. Much of the literature relating childhood abuse to adult pain experiences describes an increased incidence of medically unexplained symptoms and focuses on healthcare seeking behavior and ‘psychogenic’ symptoms (Moeller et al., 1993; Adler et al., 1989; Finestone et al., 2000). The findings of this study are therefore of particular importance as they highlight the association between a history of childhood/adolescence abuse and a pathology commonly associated with chronic pain in women. Whilst psychosocial factors may still contribute, an increased focus on the potential underlying biologic mechanisms is necessary to fully understand these relationships.
Supplementary Material
Acknowledgements
We are indebted to the participants of the Nurses’ Health Study II for their outstanding dedication. We thank Katy Vincent, DPhil, BSc, MBBS, MRCOG, from Nuffield Department of Obstetrics & Gynaecology, University of Oxford, for her critical comments on the manuscript.
Authors’ roles
Dr Missmer conceptualized and designed the study, acquired data, interpreted the analyses, and reviewed and revised the manuscript. Dr Bertone-Johnson provided administrative, technical, and material support and reviewed and revised the manuscript. Dr Boynton-Jarrett acquired data and reviewed and revised the manuscript. Dr Rich-Edwards conceptualized and designed the study, acquired data, and reviewed and revised the manuscript. Ms. Vitonis acquired data, conducted statistical analyses, interpreted the analyses, and reviewed and revised the manuscript. Dr Wieser conceptualized and designed the study, conducted statistical analyses, interpreted the analyses, and drafted and finalized the manuscript. Dr Harris conducted statistical analyses, interpreted the analyses, and drafted and finalized the manuscript.
Funding
This work was supported by National Institute of Child Health and Human Development [Grant numbers HD48544, HD52473, HD57210 and CA50385] and the Atlanta Clinical and Translational Science Institute [Grant number ULRR025008]. The Nurses’ Health Study II is supported by the National Institutes of Health grant UM1 CA176726 from the National Cancer Institute. H.R.H. is supported by the National Cancer Institute, National Institutes of Health [Grant number K22 CA193860].
Conflict of interest
None.
References
- Adler RH, Zlot S, Hurny C, Minder C. Engel’s ‘Psychogenic Pain and the Pain-Prone Patient:’ a retrospective, controlled clinical study. Psychosom Med 1989;51:87–101. [DOI] [PubMed] [Google Scholar]
- Allsworth JE, Zierler S, Krieger N, Harlow BL. Ovarian function in late reproductive years in relation to lifetime experiences of abuse. Epidemiology 2001;12:676–681. [DOI] [PubMed] [Google Scholar]
- Bauer ME, Wieck A, Lopes RP, Teixeira AL, Grassi-Oliveira R. Interplay between neuroimmunoendocrine systems during post-traumatic stress disorder: a minireview. Neuroimmunomodulation 2010;17:192–195. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, Sapareto E, Ruggiero J. Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry 1994;151:1132–1136. [DOI] [PubMed] [Google Scholar]
- Bertone-Johnson ER, Whitcomb BW, Missmer SA, Karlson EW, Rich-Edwards JW. Inflammation and early-life abuse in women. Am J Prev Med 2012;43:611–620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boynton-Jarrett R, Rich-Edwards JW, Jun HJ, Hibert EN, Wright RJ. Abuse in childhood and risk of uterine leiomyoma: the role of emotional support in biologic resilience. Epidemiology 2011;22:6–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenhouse HC, Andersen SL. Nonsteroidal anti-inflammatory treatment prevents delayed effects of early life stress in rats. Biol Psychiatry 2011;70:434–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briere J, Elliott DM. Prevalence and psychological sequelae of self-reported childhood physical and sexual abuse in a general population sample of men and women. Child Abuse Negl 2003;27:1205–1222. [DOI] [PubMed] [Google Scholar]
- Brown DW, Riley L, Butchart A, Meddings DR, Kann L, Harvey AP. Exposure to physical and sexual violence and adverse health behaviours in African children: results from the Global School-based Student Health Survey. Bull World Health Organ 2009;87:447–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deak T, Bordner KA, McElderry NK, Barnum CJ, Blandino P Jr., Deak MM, Tammariello SP. Stress-induced increases in hypothalamic IL-1: a systematic analysis of multiple stressor paradigms. Brain Res Bull 2005;64:541–556. [DOI] [PubMed] [Google Scholar]
- Finestone HM, Stenn P, Davies F, Stalker C, Fry R, Koumanis J. Chronic pain and health care utilization in women with a history of childhood sexual abuse. Child Abuse Negl 2000;24:547–556. [DOI] [PubMed] [Google Scholar]
- Fries E, Hesse J, Hellhammer J, Hellhammer DH. A new view on hypocortisolism. Psychoneuroendocrinology 2005;30:1010–1016. [DOI] [PubMed] [Google Scholar]
- Giudice LC, Kao LC. Endometriosis. Lancet 2004;364:1789–1799. [DOI] [PubMed] [Google Scholar]
- Gould DA, Stevens NG, Ward NG, Carlin AS, Sowell HE, Gustafson B. Self-reported childhood abuse in an adult population in a primary care setting. Prevalence, correlates, and associated suicide attempts. Arch Fam Med 1994;3:252–256. [DOI] [PubMed] [Google Scholar]
- Halis G, Arici A. Endometriosis and inflammation in infertility. Ann N Y Acad Sci 2004;1034:300–315. [DOI] [PubMed] [Google Scholar]
- Halme J, Hammond MG, Hulka JF, Raj SG, Talbert LM. Retrograde menstruation in healthy women and in patients with endometriosis. Obstet Gynecol 1984;64:151–154. [PubMed] [Google Scholar]
- Harrison V, Rowan K, Mathias J. Stress reactivity and family relationships in the development and treatment of endometriosis. Fertil Steril 2005;83:857–864. [DOI] [PubMed] [Google Scholar]
- Harville EW, Boynton-Jarrett R. Childhood social hardships and fertility: a prospective cohort study. Ann Epidemiol 2013;23:784–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatcher L. A Step-by-Step Approach to using SAS for Factor Analysis and Structural Equation Modeling. Cary, NC: SAS Institute, Inc, 1994. [Google Scholar]
- Heim C, Ehlert U, Hanker JP, Hellhammer DH. Abuse-related posttraumatic stress disorder and alterations of the hypothalamic-pituitary-adrenal axis in women with chronic pelvic pain. Psychosom Med 1998;60:309–318. [DOI] [PubMed] [Google Scholar]
- Heim C, Ehlert U, Hanker JP, Hellhammer DH. Psychological and endocrine correlates of chronic pelvic pain associated with adhesions. J Psychosom Obstet Gynaecol 1999;20:11–20. [DOI] [PubMed] [Google Scholar]
- Heim C, Ehlert U, Hellhammer DH. The potential role of hypocortisolism in the pathophysiology of stress-related bodily disorders. Psychoneuroendocrinology 2000;25:1–35. [DOI] [PubMed] [Google Scholar]
- Heim C, Nater UM, Maloney E, Boneva R, Jones JF, Reeves WC. Importance of studying the contributions of early adverse experience to neurobiological findings in depression. Neuropsychopharmacology 2004;29:641–648. [DOI] [PubMed] [Google Scholar]
- Heim C, Plotsky PM, Nemeroff CB. Childhood trauma and risk for chronic fatigue syndrome: association with neuroendocrine dysfunction. Arch Gen Psychiatry 2009;66:72–80. [DOI] [PubMed] [Google Scholar]
- Jacobs MB, Boynton-Jarrett RD, Harville EW. Adverse childhood event experiences, fertility difficulties and menstrual cycle characteristics. J Psychosom Obstet Gynaecol 2015;36:46–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenny C. Medicine discovers child abuse. JAMA 2008;300:2796–2797. [DOI] [PubMed] [Google Scholar]
- Koss MP, Oros CJ. Sexual Experiences Survey: a research instrument investigating sexual aggression and victimization. J Consult Clin Psychol 1982;50:455–457. [DOI] [PubMed] [Google Scholar]
- Kruitwagen RF, Poels LG, Willemsen WN, Jap PH, Thomas CM, Rolland R. Retrograde seeding of endometrial epithelial cells by uterine-tubal flushing. Fertil Steril 1991;56:414–420. [DOI] [PubMed] [Google Scholar]
- Low LA, Schweinhardt P. Early life adversity as a risk factor for fibromyalgia in later life. Pain Res Treat 2012;2012:140832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarlane J, Parker B, Soeken K, Bullock L. Assessing for abuse during pregnancy. Severity and frequency of injuries and associated entry into prenatal care. JAMA 1992;267:3176–3178. [DOI] [PubMed] [Google Scholar]
- Middlebrooks J, Audage N. The Effects of Childhood Stress on Health Across the Lifespan. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injry Prevention and Control, 2008. [Google Scholar]
- Missmer SA, Hankinson SE, Spiegelman D, Barbieri RL, Marshall LM, Hunter DJ. Incidence of laparoscopically confirmed endometriosis by demographic, anthropometric, and lifestyle factors. Am J Epidemiol 2004. a;160:784–796. [DOI] [PubMed] [Google Scholar]
- Missmer S, Hankinson S, Spiegelman D, Barbieri R, Malspeis S, Willett W, Hunter D. Reproductive history and endometriosis among premenopausal women. Obstet Gynecol 2004. b;104:965–974. [DOI] [PubMed] [Google Scholar]
- Moeller TP, Bachmann GA, Moeller JR. The combined effects of physical, sexual, and emotional abuse during childhood: long-term health consequences for women. Child Abuse Negl 1993;17:623–640. [DOI] [PubMed] [Google Scholar]
- Nater UM, Maloney E, Heim C, Reeves WC. Cumulative life stress in chronic fatigue syndrome. Psychiatry Res 2011;189:318–320. [DOI] [PubMed] [Google Scholar]
- Nguyen KT, Deak T, Owens SM, Kohno T, Fleshner M, Watkins LR, Maier SF. Exposure to acute stress induces brain interleukin-1beta protein in the rat. J Neurosci 1998;18:2239–2246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okuyama K, Ohwada K, Sakurada S, Sato N, Sora I, Tamura G, Takayanagi M, Ohno I. The distinctive effects of acute and chronic psychological stress on airway inflammation in a murine model of allergic asthma. Allergol Int 2007;56:29–35. [DOI] [PubMed] [Google Scholar]
- Pace TW, Mletzko TC, Alagbe O, Musselman DL, Nemeroff CB, Miller AH, Heim CM. Increased stress-induced inflammatory responses in male patients with major depression and increased early life stress. Am J Psychiatry 2006;163:1630–1633. [DOI] [PubMed] [Google Scholar]
- Pace TW, Wingenfeld K, Schmidt I, Meinlschmidt G, Hellhammer DH, Heim CM. Increased peripheral NF-kappaB pathway activity in women with childhood abuse-related posttraumatic stress disorder. Brain Behav Immun 2012;26:13–17. [DOI] [PubMed] [Google Scholar]
- Paras ML, Murad MH, Chen LP, Goranson EN, Sattler AL, Colbenson KM, Elamin MB, Seime RJ, Prokop LJ, Zirakzadeh A. Sexual abuse and lifetime diagnosis of somatic disorders: a systematic review and meta-analysis. JAMA 2009;302:550–561. [DOI] [PubMed] [Google Scholar]
- Petrelluzzi KFS, Garcia MC, Petta CA, Grassi-Kassisse DM, Spadari-Bratfisch RC. Salivary cortisol concentrations, stress and quality of life in women with endometriosis and chronic pelvic pain. Stress 2008;11:390–397. [DOI] [PubMed] [Google Scholar]
- Quinones M, Urrutia R, Torres-Reveron A, Vincent K, Flores I. Anxiety, coping skills and hypothalamus-pituitary-adrenal (HPA) axis in patients with endometriosis. J Reprod Biol Health 2015;3:1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Repetti RL, Taylor SE, Seeman TE. Risky families: family social environments and the mental and physical health of offspring. Psychol Bull 2002;128:330–366. [PubMed] [Google Scholar]
- Riley EH, Wright RJ, Jun HJ, Hibert EN, Rich-Edwards JW. Hypertension in adult survivors of child abuse: observations from the Nurses’ Health Study II. J Epidemiol Community Health 2010;64:413–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romito P, Crisma M, Saurel-Cubizolles MJ. Adult outcomes in women who experienced parental violence during childhood. Child Abuse Negl 2003;27:1127–1144. [DOI] [PubMed] [Google Scholar]
- Ross CA. Childhood sexual abuse and psychosomatic symptoms in irritable bowel syndrome. J Child Sex Abus 2005;14:27–38. [DOI] [PubMed] [Google Scholar]
- Sampson JA. Peritoneal endometriosis due to menstrual dissemination of endometrial tissue into the peritoneal cavity. Am J Obstet Gynecol 1927;14:442–469. [Google Scholar]
- Schliep KC, Mumford SL, Johnstone EB, Peterson CM, Sharp HT, Stanford JB, Chen Z, Backonja U, Wallace ME, Buck Louis GM. Sexual and physical abuse and gynecologic disorders. Hum Reprod 2016;31:1904–1912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simoens S, Dunselman G, Dirksen C, Hummelshoj L, Bokor A, Brandes I, Brodszky V, Canis M, Colombo GL, DeLeire T et al. The burden of endometriosis: costs and quality of life of women with endometriosis and treated in referral centres. Hum Reprod 2012;27:1292–1299. [DOI] [PubMed] [Google Scholar]
- Simoens S, Hummelshoj L, D'Hooghe T. Endometriosis: cost estimates and methodological perspective. Hum Reprod Update 2007;13:395–404. [DOI] [PubMed] [Google Scholar]
- Sinaii N, Cleary SD, Younes N, Ballweg ML, Stratton P. Treatment utilization for endometriosis symptoms: a cross-sectional survey study of lifetime experience. Fertil Steril 2007;87:1277–1286. [DOI] [PubMed] [Google Scholar]
- Solomon CG, Willett WC, Carey VJ et al. A prospective study of pregravid determinants of gestational diabetes mellitus. JAMA 1997;278:1078–1083. [PubMed] [Google Scholar]
- Stratton P, Berkley KJ. Chronic pelvic pain and endometriosis: translational evidence of the relationship and implications. Hum Reprod Update 2011;17:327–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straus M, Hamby DH, Boney-McCoy S, Sugraman DB. The revised conflict tactics scales (CTS2). J Fam Issues 1995;17:283–316. [Google Scholar]
- Stunkard A, Sorensen T, Schulsinger F. Use of the Danish Adoption Register for the study of obesity and thinness In: Kety SRL, Sideman S et al. (eds). The Genetics of Neurological and Psychiatric Disorders. New York City: Raven Press, 1983, 115–120. [PubMed] [Google Scholar]
- Suzuki E, Shintani F, Kanba S, Asai M, Nakaki T. Immobilization stress increases mRNA levels of interleukin-1 receptor antagonist in various rat brain regions. Cell Mol Neurobiol 1997;17:557–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teicher MH, Andersen SL, Polcari A, Anderson CM, Navalta CP, Kim DM. The neurobiological consequences of early stress and childhood maltreatment. Neurosci Biobehav Rev 2003;27:33–44. [DOI] [PubMed] [Google Scholar]
- Tietjen GE, Brandes JL, Peterlin BL, Eloff A, Dafer RM, Stein MR, Drexler E, Martin VT, Hutchinson S, Aurora SK et al. Childhood maltreatment and migraine (part III). Association with comorbid pain conditions. Headache 2010;50:42–51. [DOI] [PubMed] [Google Scholar]
- Ugur M, Turan C, Mungan T, Kuscu E, Senoz S, Agis HT, Gokmen O. Endometriosis in association with mullerian anomalies. Gynecol Obstet Invest 1995;40:261–264. [DOI] [PubMed] [Google Scholar]
- Weissbecker I, Floyd A, Dedert E, Salmon P, Sephton S. Childhood trauma and diurnal cortisol disruption in fibromyalgia syndrome. Psychoneuroendocrinology 2006;31:312–324. [DOI] [PubMed] [Google Scholar]
- Widom C, Shepard R. Accuracy of adult recollections of childhood victiization: part I. Childhood physical abuse. Psychol Assess 1996;8:412–421. [Google Scholar]
- Wise LA, Palmer JR, Rothman EF, Rosenberg L. Childhood abuse and early menarche: findings from the black women’s health study. Am J Public Health 2009;99:S460–S466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wuest J, Merritt-Gray M, Ford-Gilboe M, Lent B, Varcoe C, Campbell JC. Chronic pain in women survivors of intimate partner violence. J Pain 2008;9:1049–1057. [DOI] [PubMed] [Google Scholar]
- Zabin LS, Emerson MR, Rowland DL. Childhood sexual abuse and early menarche: the direction of their relationship and its implications. J Adolesc Health 2005;36:393–400. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.