Abstract
Purpose of review
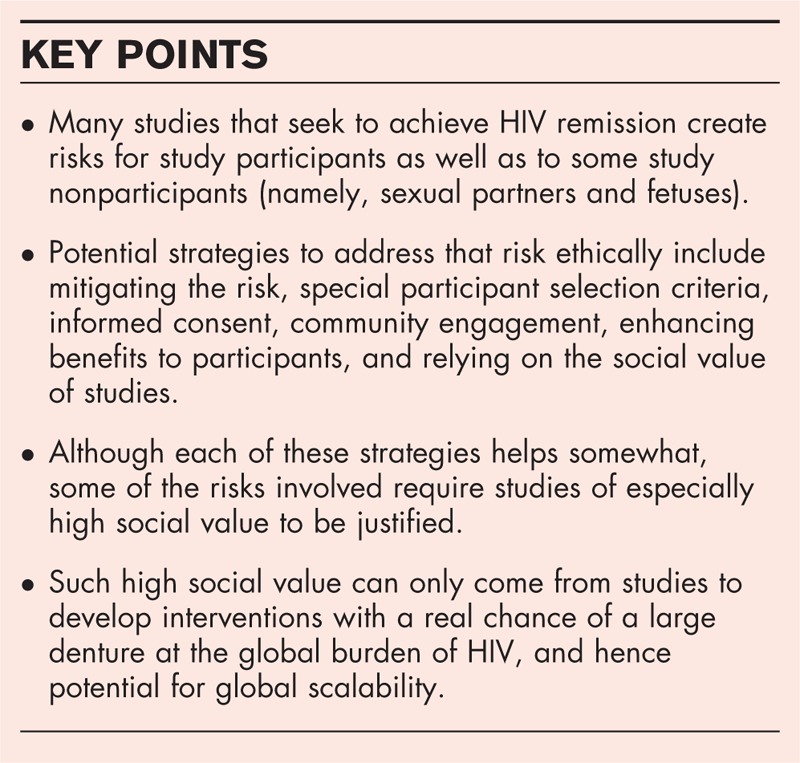
Several promising experimental pathways exist for long-term control of HIV in the absence of antiretroviral therapy (HIV ‘remission’) and are now being tested in early clinical studies. These studies can be invasive and pose a host of distinctive risks to participants, as well as to nonparticipants, especially to participants’ fetuses, and sexual partners.
Recent findings
Ethical analyses of these studies have mainly focused on the risks to study participants. They recommend, and some investigators implement, procedures to mitigate risks for participants or to offset them with direct, indirect, and nonmedical benefits. They also suggest ways to keep participants’ consent highly voluntary and informed. Rarely do ethicists propose keeping the social value of studies high. Of these recommended responses, only the latter, rarer proposals help address the risk to nonparticipants, as would some novel ways to address that risk.
Summary
HIV remission studies pose a number of ethical dilemmas. Many current investigative approaches put the participant at significant risk, but well established guidelines exist for mitigating this risk. Ethical issues that are not being fully addressed include risk to nonparticipants and the need to consider the societal value of studies, for example, their prospective impact on the global HIV burden.
Video abstract
Keywords: analytic treatment interruption, HIV cure-related studies, human subjects research, immunotherapy, research ethics
INTRODUCTION
A sterilizing cure – complete eradication of all replication-competent HIV in an individual – has most likely been achieved in one case; however, this case would be challenging to replicate and, with current technology, impossible to scale. Therefore, current HIV cure-related research focuses primarily on achieving a long-term functional cure, or ‘remission’. We define remission as undetectable viremia for a given period (yet to be defined) without antiretroviral therapy (ART), and without either CD4+ T-cell loss or HIV symptoms or potential for HIV transmission [1▪▪].
An ethical challenge in many early-phase HIV cure-related studies is the high risk to individual participants from toxicity, invasive diagnostics, and analytical treatment interruptions (ATIs). These risks accrue to individuals who are typically otherwise healthy and stable on ART, in contrast, for example, to risky early-phase studies of cancer [1▪▪,2,3,4▪]. There is no standard set of ethical guidelines governing these risks to the individual, but current guidelines apply to any experimental therapy.
In this perspective, we summarize these standard risks, but also discuss issues that are more unique to studies of HIV remission. For example, as there is no standard biomarker for a remission study, many if not most studies include an ATI, which poses risks not only to the participant but also to his or her sexual partners. In addition, as the main beneficiaries of any remission strategy are expected to be those who cannot access life-long ART, it seems reasonable to advocate for a scalable intervention that can be distributed globally when deciding which strategies to pursue.
Box 1.
no caption available
PERSONAL RISK
The risks of remission studies accrue to active arm participants, placebo arm participants, and nonparticipants, including sexual partners and fetuses.
Risk for active arm participants
Risks to active study participants in remission studies come from toxicities and invasive diagnostic exams, as well as ATIs. First, many of the drugs currently trialed for HIV remission have known toxicities. This is accentuated by the growing appreciation that rapidly emerging advances in cancer immunotherapy have direct implications for achieving an HIV remission [4▪]. In particular, checkpoint inhibitors such as anti-programmed death-1 (anti-PD-1) – now standard care for metastatic melanoma and other cancers – are being carefully moved into the HIV remission arena. Anti-PD-1 therapy can cause autoimmune diseases of the skin, gut, and other organs, and fatal reactions are possible [5,6]. Other interventions for boosting immune response in cancer and potentially in HIV (either for a sterilizing cure or for remission) involve the use of gene modified T cells and gene editing approaches; known and unknown toxicities are major concerns for these approaches as well [7]. Combination therapies are now seen as the most promising approaches [8], but create an added layer of uncertainty – how do partly known effects interact? [9]. Additional risks and burdens come from invasive diagnostics.
In the absence of a viable biomarker for the reservoir, many cure-related trialists are appropriately measuring the impact of their intervention by interrupting ART. In sterilizing cure studies, in which the goal is to simply determine if an active infection persists, the resulting complications are theoretically manageable with frequent monitoring and a clear plan to resume ART should the virus rebound [10]. But in remission studies, the goal is not to determine if the virus is present, but rather to determine if the immune system can respond to the rebounding viremia and eventually bring it down to low or undetectable levels. These so-called set-point ATI studies need to allow for a period of high-level viremia that is expected to be transient [6]. Thus, in many remission studies, ART resumption might be preceded by adverse results, for example, acute retroviral syndrome, selection of drug-resistant HIV, immunodeficiency and irreversible harm to immune system, and reseeding of the reservoir [11▪]. It should be noted, however, that recent studies indicate that when treatment interruptions are done carefully and in a monitored setting, they need not be associated with either the emergence of a drug-resistant virus, or manifest expansion of the viral reservoir [10,12–15].
Risk for placebo arm participants
A placebo arm can be key to interpretable findings, and hence to defensible research. Yet participants in placebo arms of remission trials can face the risks of diagnostics or of ATI with no therapeutic prospect from the intervention being tested [16▪]. Placebo arms are easiest to justify when there is no risk for those randomized to that arm from diagnostics and no ATI is planned. But some assume that when an ATI is unavoidable, placebo arms are illegitimate [17], whereas others only recommend proceeding with special care [16▪]. No consensus exists on that question [16▪].
Risk for sexual partners
Interrupting therapy and allowing even transient episodes of high-level viremia poses clear risks to nonparticipants. A study participant's ATI and the acute viremia that results in some remission studies deprive his or her sexual partner(s) of a highly efficacious protection from infection [18]. It thus exposes them (and their other sexual partners, and their partners, and so forth) to the risk of being infected.
Risk for fetuses
A study participant's ATI would also deprive her fetus of the protective effect of ART and put it at risk of becoming infected with HIV. In some gene therapy remission studies, germ-line changes that would risk fetuses and even their progeny are also possible.
PROPOSED ETHICAL RESPONSES TO THE RISK
Several strategies seek to address ethically the risks from remission studies to each of these populations (refer to Table 1 for a summary of the discussion).
Table 1.
Summary of discussion
| Risk | ||||
| Attempted ethical responses to the risk | Affecting active arm participants | Affecting placebo arm participants | Affecting sexual partners | Affecting fetuses |
| Mitigation risk for participants | ✓ | ✓ | – | – |
| Mitigating risk for nonparticipants | ? | ? | ✓ | ✓ |
| Special selection criteria | ✓ | ✓ | ✓ | ✓ |
| Informed consent | ✓ | ✓ | ? | ? |
| Community engagement | ? | ? | – | ? |
| Enhanced benefits | ✓ | ✓ | – | ? |
| Social value | ✓ | ✓ | ✓ | ✓ |
The table lists attempted ethical responses to risks from remission studies and categorizes how relevant each response is to the risks to various populations.
Mitigating risk to participants
The most obvious ethical response to a risk is to build in safeguards that reduce the hazard that any adverse event will occur or contain its consequences [19–21]. Many strategies have been proposed to reduce the risk faced by study participants. These include, among other things, very intense mathematical modeling and greater use of animal models before turning to human participants [19]; excluding invasive diagnostics from the study procedures [22]; replacing intense, one-time administration of large doses of toxic interventions with a gradual increase in dosing [9]; frequent monitoring and, in the case of ATIs, predetermined CD4+ and HIV RNA thresholds for resumption of ART [11▪,16▪]; and preparing to provide new lines of ART should drug resistance emerge [16▪]. For mitigating risk to placebo arm participants, one strategy is strict reliance on historical controls [17], though it risks confounding study results.
As important as mitigating risk to participants is, it does not address the ethical complications arising from risk to nonparticipants.
Mitigating risk to nonparticipants
Much less standard in research ethics is addressing risk from trials to people who are nonparticipants [23], nevertheless some strategies do exist. For example, in HIV remission studies with an ATI that put sexual partners of participants at risk for transmission, study procedures may include counseling on safe sex practices or provision of preexposure prophylaxis to stable sexual partners of study participants [11▪]. Isolating study participants whilst deemed infectious is regularly used in challenge studies [24], and bioethicists have proposed isolation for infectious disease research more broadly [25]. However, in the HIV context, isolation may curb personal liberty too much compared with the magnitude of risk.
A common strategy for averting transmission to fetuses is excluding pregnant women from the study and asking ones of a reproductive age to use two forms of contraception. But this strategy may dissuade female patients from participating in studies.
Special selection criteria for study participation
Many studies try to avoid risk by recruiting participants who are at low risk [e.g., in the case of remission studies with an ATI, excluding candidates with a history of centers for disease control and prevention category C clinical events (1993) or those with cutaneous Kaposi's sarcoma [11▪]]. Again, this strategy need not address protection of nonparticipants (except when the exclusion criterion serves both purposes, e.g., excluding from these studies candidates with a record of a high viral load setpoint). Significantly, other studies respond to the risk by focusing recruitment on candidates who are in important ways at high risk. A high portion of remission studies [26] and about half of current gene-therapy-based HIV cure-related studies [26], are specifically done in HIV-infected cancer patients. First, as described earlier, similar strategies are being used to fight cancer [6], and there is greater hope for a therapeutic effect for cancer, HIV, or both, in that population. Second, one could argue that if worst comes to worst, it is ethically preferable to have shortened the life of a terminal or highly advanced patient (because of her cancer comorbidity) than the life of someone who is otherwise healthy. Indeed, a bold proposal is to focus specifically on patients who are at the end of their lives [27▪].
Informed consent
With fully informed consent, it can be possible, rational, and permissible for a person to sacrifice selfish interests for the sake of a noble cause [28]. Taking risks in HIV-cure-related studies is a case in point [21,29▪] – as is sacrificing a kidney for others. There are many indications that people living with HIV (PLWHIV) are enthusiastic to contribute to cure-related research [30,31,32▪], and this is anecdotally familiar to many investigators.
Evoking the notion of a ‘therapeutic misconception’ in clinical studies, some commentators have warned, however, that cure study participants may be subject to a ‘curative misconception’ [33,34]. By that suggestive term they may have meant that study participants could be overoptimistic about the chance for and the benefits of being cured, of the paucity of study-borne side effects, or of the investigators’ goal to promote participants’ clinical interests. Additional work warned that consent forms in cure-related research can be misleading [35,36].
Activists and ethicists have implored for trusting cure-related study participants to make highly intelligent decisions on what is acceptable to them, both in general [37,38▪] and in remission studies with an ATI in particular [39▪]. Interviews may suggest that participants in cure trials have been informed [32▪] and remain satisfied with their decision to participate in hindsight, even after suffering from side effects [37,39▪]. Even PLWHIV who express theoretical high willingness to contribute to cure research seem responsive to risks and benefits [32▪,40].
Nevertheless, two specific complications about reliance on personal consent arise in remission studies. First, only empirical investigation can rule out the possibility of what one may call ‘curative misconception #2’: both PLWHIV [41,42] and cure-related trial participants [30,31] are excited about a sterilizing cure far more than about mere remission. It is not impossible that in risky remission studies, some of the eagerness to participate reflects confusion between the two types of ‘cure-related’ research [43]. In other words, a misconception of remission studies as sterilizing cure ones may turn out to help drive participation in the former. Inasmuch as that is the case, remission study participants’ consent would be less than fully informed, somewhat undermining its justificatory contribution.
A second complication can arise even when a candidate participant's consent is fully informed and voluntary. The participant's consent does not address the ethical challenge of risk created to nonparticipants, for example, to the participant's sexual partners.
Community engagement
To address risk to nonparticipants, some of the ethics literature proposes community engagement [25], and it has become common to interview PLWHIV and community advisory boards on these matters [16▪]. However, in the area of risk of infection to nonparticipants like unstable sexual partners, the relevant community would need to be a large group of uninfected individuals, which is not a community that is easily reached or that has representatives.
Enhanced benefits
Several bioethicists recommend offsetting any remaining risks in cure-related studies by appealing to or enhancing the many potential indirect benefits of study participation, both medical and nonmedical [40,42,44]. This has been proposed for addressing the risks from ATI studies [39▪,45▪].
But these indirect benefits would be to the participants, and not necessarily to the party at risk. For example, a sexual partner at risk does not get anything when a participant gains in her medical care, social standing, or financial standing from trial participation.
Social value
To ensure that risks to all parties in HIV remission studies and cure-related research in general are justified, it remains necessary to ensure that these studies serve a very urgent social purpose, one that justifies placing some individuals at serious risks as is often unavoidable in this enterprise. Leading antiutilitarian ethicists have opined that great importance for other individuals’ health can also be near-sufficient for justification [46,47,48▪▪]. Here, satiating our scientific curiosity or making nonreplicable medical breakthroughs is not enough. We need to ensure that cure-related research in general and remission research in particular continues to pursue strategies that have potential for scalability on a global level, and a real chance of one day making a large dent at the global burden of HIV. Nowadays, HIV-infected individuals who are able to access, tolerate, and adhere to ART can expect to have a near-normal life span. A curative strategy that rids HIV-infected people with access to ART of the inconvenience, stigma, and personal costs still associated with taking it would be of value; however, the potential to generate immense societal value, and the surest ethical justification, belongs to trialing strategies that, if successful, would help promote access for the nearly 50% of PLWHIV around the world who are currently not accessing ART [49]. For this reason, and because the nature of the disease differs between rich countries and low and middle-income countries [50▪▪], there is an ethical imperative to test remission strategies in low and middle-income countries [49,50▪▪].
CONCLUSION
The strategies that would work for each type of population at risk are summarized in Table 1. As the table indicates, an unavoidable source of justification for the risks of HIV remission studies is the societal value of that science. This has practical implications for the choice of which strategies to prioritize for research and which countries to test them in.
Acknowledgements
We would like to thank Rebecca Kahn for her assistance with the study.
Solicited contribution for the issue: ‘Progress in achieving long-term HIV remission’ (eds. Jean-Daniel Lelièvre and Timothy Henrich).
Financial support and sponsorship
The current work was supported by NIAID grant NIAID grant R01AI114617 (HIV cure studies: risk, risk perception, and ethics), the amfAR Institute for HIV Cure Research (amfAR 109301), and the Delaney AIDS Research Enterprise (DARE; A127966).
Conflicts of interest
S.G.D. receives research support from Merck, Gilead, and ViiV Healthcare and is a scientific board member for Bryologix and Enochian. Rest of the authors have no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
Supplementary Material
REFERENCES
- 1▪▪.Deeks SG, Lewin SR, Ross AL, et al. International AIDS Society global scientific strategy: towards an HIV cure 2016. Nat Med 2016; 22:839–850. [DOI] [PMC free article] [PubMed] [Google Scholar]; A multidisciplinary, international group of experts working in the HIV cure arena defined ‘cure’, described current research and the ethical issues surrounding it, and developed a global strategy for HIV cure research.
- 2.Eyal N, Kuritzkes DR. Challenges in clinical trial design for HIV-1 cure research. Lancet 2013; 382:1464–1465. [DOI] [PubMed] [Google Scholar]
- 3.Evans D. What would you do to cure HIV? POZ. 2011; New York, USA: Susan Levey, Smart + Strong, Available from: http://www.aidsmeds.com/articles/hiv_cure_ethics_2042_20510.shtml. [Cited 2018]. [Google Scholar]
- 4▪.Rasmussen TA, Anderson JL, Wightman F, Lewin SR. Cancer therapies in HIV cure research. Curr Opin HIV AIDS 2017; 12:96–104. [DOI] [PMC free article] [PubMed] [Google Scholar]; Describes therapies for treatment of cancer that are now being tested in HIV remission studies, noting their toxicity risks.
- 5.Topalian SL, Hodi FS, Brahmer JR, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med 2012; 366:2443–2454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cousins S. Could cancer research hold the key to a cure for HIV? BMJ 2017; 358:j3905. [DOI] [PubMed] [Google Scholar]
- 7.Stan R, Zaia JA. Practical considerations in gene therapy for HIV cure. Curr HIV/AIDS Rep 2014; 11:11–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perreau M, Banga R, Pantaleo G. Targeted immune interventions for an HIV-1 cure. Trends Mol Med 2017; 23:945–961. [DOI] [PubMed] [Google Scholar]
- 9.Reeves DB, Duke ER, Hughes SM, et al. Antiproliferative therapy for HIV cure: a compound interest approach. Sci Rep 2017; 7:4011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clarridge KE, Blazkova J, Einkauf K, et al. Effect of analytical treatment interruption and reinitiation of antiretroviral therapy on HIV reservoirs and immunologic parameters in infected individuals. PLoS Pathog 2018; 14:e1006792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11▪.Garner SA, Rennie S, Ananworanich J, et al. Interrupting antiretroviral treatment in HIV cure research: scientific and ethical considerations. J Virus Erad 2017; 3:82–84. [DOI] [PMC free article] [PubMed] [Google Scholar]; A review of ethical issues in analytical treatment interruption (ATI) cure-related research, focused primarily on risks to participants.
- 12.Rothenberg MK, Keele BF, Wietgrefe SW, et al. Large number of rebounding/founder HIV variants emerge from multifocal infection in lymphatic tissues after treatment interruption. Proc Natl Acad Sci U S A 2015; 112:E1126–E1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bar KJ, Salantes DB, Zheng Y, et al. Brief ATI does not alter the size or composition of the latent HIV-1 reservoir. Poster session presented at: Conference on Retroviruses and Opportunistic Infections; 4–7 March 2018; Boston, MA. [Google Scholar]
- 14.Calin R, Hamimi C, Lambert-Niclot S, et al. Treatment interruption in chronically HIV-infected patients with an ultralow HIV reservoir. AIDS 2016; 30:761–769. [DOI] [PubMed] [Google Scholar]
- 15.Strogin Z, Sharaf R, VanBelzen DJ, et al. Effect of short-term ART interruption on levels of integrated HIV DNA. J Virol 2018; 92:e00285-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16▪.Dubé K, Evans D, Dee L, et al. ‘We need to deploy them very thoughtfully and carefully’: perceptions of analytical treatment interruptions in HIV cure research in the United States – a qualitative inquiry. AIDS Res Hum Retroviruses 2018; 34:67–79. [DOI] [PMC free article] [PubMed] [Google Scholar]; Interviews with people living with HIV (PLWHIV), clinician–researchers, and bioethicists/policy makers on ATIs, suggesting no consensus on when ATIs can be deployed in cure-related research and, among PLWHIV, great apprehension about ATIs in research.
- 17.Martin GE, Gossez M, Williams JP, et al. Posttreatment control or treated controllers? Viral remission in treated and untreated primary HIV infection. AIDS 2017; 31:477–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med 2011; 365:493–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dresser R. First-in-human HIV-remission studies: reducing and justifying risk. J Med Ethics 2017; 43:78–81. [DOI] [PubMed] [Google Scholar]
- 20.Dubé K, Sylla L, Dee L, et al. Research on HIV cure: mapping the ethics landscape. PLoS Med 2017; 14:e1002470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eyal N. How to keep high-risk studies ethical: classifying candidate solutions. J Med Ethics 2017; 43:74–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Niessl J, Baxter AE, Kaufmann DE. Tools for visualizing HIV in cure research. Curr HIV/AIDS Rep 2018; 15:39–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shah SK, Kimmelman J, Lyerly AD, et al. Bystander risk, social value, and ethics of human research. Science 2018; 360:158–159. [DOI] [PubMed] [Google Scholar]
- 24.Cohen J. Studies that intentionally infect people with disease-causing bugs are on the rise. Science 2016; Available from: http://www.sciencemag.org/news/2016/05/studies-intentionally-infect-people-disease-causing-bugs-are-rise. [Cited 2016]. [Google Scholar]
- 25.Battin MP, Francis LP, Jacobson JA, Smith CB. Battin MP, Francis LP, Jacobson JA, Smith CB. The ethics of research in infectious disease: experimenting on this patient, risking harm to that one. The patient as victim and vector: ethics and infectious disease. New York: Oxford UP; 2009. 164–183. [Google Scholar]
- 26.Treatment Action Group. Research toward a cure trials. 2018; New York, USA: Treatment Action Group, Available from: http://www.treatmentactiongroup.org/cure/trials. [Cited 10 April 2018]. [Google Scholar]
- 27▪.Gianella S, Taylor J, Brown TR, et al. Can research at the end-of-life be a useful tool to advance HIV cure? AIDS 2017; 31:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]; Suggests that to give researchers a better understanding of the HIV reservoir and how it might be eradicated, it could make ethical sense to conduct studies at the very end of patients’ lives.
- 28.Eyal N. Informed consent. In: Stanford encyclopedia of philosophy [Internet]. Fall 2012 Edition. Edited by Zalta EN (editor). 2011. Available from: https://plato.stanford.edu/entries/informed-consent/#Bib [Accessed 1 July 2018]. [Google Scholar]
- 29▪.Buchak L. Why high-risk, nonexpected-utility-maximising gambles can be rational and beneficial: the case of HIV cure studies. J Med Ethics 2017; 43:90–95. [DOI] [PubMed] [Google Scholar]; Argues philosophically that there are many rational approaches to risk, and that foregoing the safety of reliance on antiretroviral therapy to contribute to risky cure-related research can be perfectly rational.
- 30.McMahon JH, Elliott JH, Roney J, et al. Experiences and expectations of participants completing an HIV cure focused clinical trial. AIDS 2015; 29:248–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McMahon JH, Lau J, Hagenauer M, et al. Experiences and expectations of participants completing HIV cure focused clinical trials. Poster presented at: IAS HIV Cure & Cancer Forum; 22–23 July 2017; Paris, France. [Google Scholar]
- 32▪.Dubé K, Evans D, Sylla L, et al. Willingness to participate and take risks in HIV cure research: survey results from 400 people living with HIV in the US. J Virus Erad 2017; 3:40–50.e21. [DOI] [PMC free article] [PubMed] [Google Scholar]; An online survey of PLWHIV in the United States, seeking to quantify willingness to participate in risky HIV-cure-related research, indicating that enthusiasm to participate in HIV-cure-related trials is sensitive to the level of risk and perceived benefits of participation.
- 33.Tucker JD, Rennie S. Social and Ethical Working Group on HIV Cure. Social and ethical implications of HIV cure research. AIDS 2014; 28:1247–1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Annas GJ. Cure research and consent: the Mississippi Baby, Barney Clark, Baby Fae and Martin Delaney. J Med Ethics 2017; 43:104–107. [DOI] [PubMed] [Google Scholar]
- 35.Henderson GE. The ethics of HIV ‘cure’ research: what can we learn from consent forms? AIDS Res Hum Retroviruses 2015; 31:56–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dubé K, Henderson GE, Margolis DM. Framing expectations in early HIV cure research. Trends Microbiol 2014; 22:547–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Evans D. An activist's argument that participant values should guide risk equations in HIV cure research. J Med Ethics 2017; 43:100–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38▪.Preau M, Doumergue M, Protiere C, et al. Acceptability of HIV cure-related trials: the challenges for physicians and people living with HIV (ANRS-APSEC). AIDS Care 2018; 30:914–920. [DOI] [PubMed] [Google Scholar]; Discussions with stakeholder groups confirm that PLWHIV consider multiple factors about participating in HIV-cure-related research, concluding that they can make intelligent decisions on what is acceptable to them.
- 39▪.Henderson G, Peay H, Kroon E, et al. The ethics of treatment interruption trials in HIV cure research: addressing the conundrum of risk/benefit assessment. J Med Ethics 2018; 44:270–276. [DOI] [PMC free article] [PubMed] [Google Scholar]; Interviews with participants of an HIV-cure-related study with an ATI in Thailand reveal sometimes-surprising benefits that participants perceive in cure-related study participation, concluding that ethicist and investigator worries about risks from ATIs and from toxicities in cure-related studies are exaggerated.
- 40.Dubé K, Taylor J, Sylla L, et al. ‘Well, it's the risk of the unknown... right?’: a qualitative study of perceived risks and benefits of HIV cure research in the United States. PLoS One 2017; 12:e0170112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Verdult F. Psychosocial benefits of an HIV cure. Paper presented at IAS towards an HIV Cure Pre-Conference Symposium; 20–21 July 2012; Washington, DC, USA. [Google Scholar]
- 42.Sylla L, Evans D, Taylor J, et al. If we build it, will they come? Perceptions of HIV cure-related research by people living with HIV in four U.S. cities: a qualitative focus group study. AIDS Res Hum Retroviruses 2018; 34:56–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dubé K, Luter S, Lesnar B, et al. Use of ‘eradication’ in HIV cure-related research: a public health debate. BMC Public Health 2018; 18:245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Largent EA. For love and money: the need to rethink benefits in HIV cure studies. J Med Ethics 2017; 43:96–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45▪.Eyal N. What can the lived experience of participating in risky HIV cure-related studies establish? J Med Ethics 2018; 44:277–278. [DOI] [PMC free article] [PubMed] [Google Scholar]; Questions how much PLWHIVs’ and cure-related study participants’ perceptions of benefits in cure-related studies show that these studies benefit them on balance.
- 46.Kumar R. Contractualist reasoning, HIV cure clinical trials, and the moral (ir)relevance of the risk/benefit ratio. J Med Ethics 2017; 43:124–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kamm FM. The morality of risks in research: reflections on Kumar. J Med Ethics 2017; 43:128–131. [DOI] [PubMed] [Google Scholar]
- 48▪▪.Wikler D. Must research benefit human subjects if it is to be permissible? J Med Ethics 2017; 43:114–117. [DOI] [PMC free article] [PubMed] [Google Scholar]; Succinctly shows that the law-governing federally funded research in the US permits studies that are on balance risky to participants: the potential benefits to society should also enter into the calculation.
- 49.Brown R, Evans NG. The social value of candidate HIV cures: actualism versus possibilism. J Med Ethics 2017; 43:118–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50▪▪.Rossouw T, Tucker JD, van Zyl GU, et al. Barriers to HIV remission research in low- and middle-income countries. J Int AIDS Soc 2017; 20:21521. [DOI] [PMC free article] [PubMed] [Google Scholar]; Points out differences in the nature of the epidemic between rich countries and endemic low-income and middle-income ones, calling for more remission research in the latter.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


