Abstract
Objective:
To examine whether individual differences and day-to-day fluctuations in diabetes goal planning are associated with type 1 diabetes management during late adolescence, and whether lapses in daily diabetes goal planning are more disruptive to diabetes management among those with poorer executive functioning (EF).
Methods:
Late adolescents with type 1 diabetes (N = 236; Mean age = 17.77 years) completed survey measures assessing individual differences in levels of diabetes goal planning and adherence, as well as survey and performance-based measures of EF; glycemic control was assessed through HbA1c assays. Participants then completed a two-week daily diary, rating items measuring daily diabetes goal planning, goal effort, and adherence, and recording blood glucose tests from their glucometer at the end of each day.
Results:
Analyses of survey measures indicated that higher individual differences in diabetes goal planning were associated with better adherence and glycemic control. Analyses of daily-level data using hierarchical linear modeling indicated that adolescents displayed higher daily adherence and lower blood glucose levels on days when they had higher-than-their-average levels of daily goal planning and daily goal effort. EF moderated the association between daily goal planning and daily adherence, indicating lapses in daily goal planning were more disruptive for adolescents with poorer EF.
Conclusions:
Both individual differences and day-to-day fluctuations in diabetes goal planning are associated with diabetes management, highlighting the challenges of managing type 1 diabetes in daily life. Late adolescents with poorer EF may especially benefit from planning to attain diabetes goals on a daily basis.
Keywords: diabetes, adherence, goal striving, self-regulation, executive function, daily diary
Type 1 diabetes (T1D) management represents a complex self-regulation task that requires sophisticated skills to plan and coordinate multiple daily behaviors in order to achieve diabetes-related goals. Managing T1D is particularly challenging during late adolescence, when individuals display poorer adherence and glycemic control compared to younger and older age groups (Miller et al. 2015). Understanding the factors that contribute to T1D management during late adolescence is important because poor management contributes to elevated blood glucose (BG) levels and serious long-term complications (White et al., 2001). The difficulties of managing diabetes during this time of development may partially reflect that late adolescents are assuming individual responsibility for managing their illness while still developing the self-regulatory skills and capacities necessary to manage T1D independently (Berg et al., 2014; Suchy et al., 2016; Wiebe et al., 2014). The present study examined how aspects of self-regulation are related to T1D management during late adolescence.
Consistent with current models of self-regulation (e.g., Karoly, 2010; Mann, de Ridder, & Fujita, 2013), effective self-management of T1D involves the adoption of a diabetes goal that motivates effort and activates planning for goal attainment. In Karoly’s taxonomy of goal representations (Karoly & Ruehlman, 1995; Karoly, 2010), goal planning is a critical component of self-regulation and refers to the extent to which individuals plan to attain goals, maintain effort toward those goals, and prevent disruptions or distractions from interfering with goal progress. A substantial literature demonstrates the central role of goal planning in maintaining health behaviors and managing chronic illness (Gollwitzer & Oettingen, 2007; Karoly & Ruehlman, 1995; Mann et al., 2013).
Goal planning is likely to be quite important for managing T1D, as individuals must complete and coordinate multiple behaviors (e.g., check BG levels, count carbohydrates, adjust insulin doses) in daily life in order to keep BG levels close to a normal range. Adolescents with T1D rate diabetes goals as among their most important goals (Butler et al., 2011), describe obstacles (e.g., social stigma, inconveniences of T1D regimens) that may disrupt diabetes goal attainment, and view planning to prevent barriers from interfering as an important aspect of managing their illness (Mulvaney et al., 2011). Such findings suggest that individuals who engage in higher levels of diabetes goal planning may be more successful in managing their T1D, although this association has not yet been empirically demonstrated.
Important conceptual questions emerge when one considers the role of goal planning in T1D management. First, it is important to determine whether the potential effects of goal planning on T1D management are distinct from the effects of trait-like cognitive capacities such as executive functioning (EF). EF refers to a multifaceted construct comprised of the abilities to engage in purposeful, goal-directed, future-oriented behavior (Lezak, Howieson, Bigler, & Tranel, 2013; Suchy, 2015). The ability to make plans to achieve a goal and to prevent disruptions to goal progress inherently relies on neurocognitive processes that fall under the EF umbrella; these processes include the ability to initiate and maintain adaptive actions, to flexibly shift among ideas or tasks, and to inhibit irrelevant or maladaptive thoughts or behaviors (Suchy, 2015). Additionally, EF itself has been shown to be associated with T1D management (Duke & Harris, 2014; Suchy et al., 2016). Given that both goal planning and T1D management partially rely on EF, demonstrations of associations between diabetes goal planning and T1D management need to control for EF to determine whether the effects of goal planning occur above and beyond the influence of EF.
A second conceptual question is whether within-person day-to-day fluctuations in diabetes goal planning occur and predict daily T1D management. Goal planning and goal effort fluctuate from one day to the next (Affleck et al., 2001; Karoly, Okun, Enders, & Tennen, 2014) as one encounters obstacles or conflicting goals within the constraints and opportunities of daily life (e.g., Vancouver, Weinhardt, & Schmidt, 2010). For instance, late adolescents with T1D may be derailed in diabetes goal planning or exert less diabetes goal effort on days they are engaged in important and potentially competing social (e.g., attending a friend’s party, spending time with family) or academic (e.g., studying for an exam) activities. Because T1D is an illness that must be managed daily, such day-to-day lapses in daily diabetes goal planning or goal effort are likely to be associated with day-to-day fluctuations in T1D management.
The degree to which day-to-day goal planning fluctuations are associated with daily T1D management may vary as a function of an individual’s EF capacity. This is because goal planning facilitates goal attainment partially by minimizing the need to rapidly problem-solve in the moment as barriers to goal attainment occur (Mann et al., 2013). In the absence of planning, individuals may need to engage in problem-solving “on the fly” as obstacles emerge, increasing the demands on EF. Given this role for EF in dealing with unanticipated goal disruptions (Hall, Fong, Epp, & Elias, 2008), EF may moderate day-to-day associations between daily diabetes goal planning and daily T1D management. That is, one would expect lapses in daily diabetes goal planning to be especially problematic for those with poorer EF.
In summary, the present study examined how diabetes goal planning is associated with T1D management during late adolescence, a high risk time when individuals are still developing the self-regulation skills to manage T1D. First, we examined whether individual differences in diabetes goal planning were associated with T1D management above and beyond associations with EF capacities (Aim 1). We predicted that late adolescents with higher levels of diabetes goal planning would display better adherence and glycemic control independent of their underlying EF capacity. Second, we examined whether day-to-day fluctuations in daily goal planning and daily goal effort were associated with day-to-day fluctuations in daily T1D management (Aim 2). We predicted that on days when late adolescents reported lower than their average levels of daily goal planning and daily goal effort, they would have poorer daily adherence and BG control. Finally, we examined whether EF moderated the associations of daily goal planning and daily goal effort with daily T1D management (Aim 3). We predicted that late adolescents with poorer EF capacities would show stronger daily associations, suggesting their T1D management was more disrupted by daily lapses in goal planning. Together, these aims may identify new avenues for intervention targeting not only individuals at risk, but also the processes that facilitate T1D management in daily life.
Method
Participants
High school seniors with T1D were recruited for a two-year longitudinal study on how self-regulation and social relationships are associated with T1D management across the transition into emerging adulthood. Participants were recruited in clinic or by mail and phone from three outpatient pediatric endocrinology clinics in two southwestern US cities. Late adolescents were eligible to participate if they had been diagnosed with T1D for at least one year (M (SD) = 7.35 (3.88) years), had English as their primary language (necessary for neurocognitive testing), were in their final year of high school, lived with a parent (68.4% lived with both biological parents, 27.1% with one biological parent and 4.5% lived with adoptive parents or grandparents), would be able to have regular contact with parents over the subsequent two years (consistent with objectives of the broader study), and had no condition that would prohibit study completion (e.g., severe intellectual disability, blindness). Of the qualifying 507 individuals approached, 301 (59%) initially agreed to participate. Of these, 247 adolescents (82%) completed baseline assessments. Primary reasons for not participating included being too busy in their senior year (34%) and lack of interest (33%); 20% declined to give a reason. At one site, the Institutional Review Board (IRB) permitted data to be collected comparing those who did versus did not participate. Participants and nonparticipants did not differ on HbA1c, time since diagnosis, gender, or pump status (ps > .05). However, participants were slightly younger, M (SD) = 17.77 (.43) vs 17.91 (.48) years, t(203) = 2.274, p = .024, and more likely to be Hispanic (21% vs 11%), X2 (1) = 3.88, p = .049, than nonparticipants.
Consistent with the patient population at participating clinics, 75.2% of the full sample (N = 247) identified as non-Hispanic White, 14.2% Hispanic, 4.8% African American, and the remainder as Asian/Pacific Islander, American Indian, or more than one race. Participants were 17.76 (SD = 0.39) years old on average and 60% were female. Parents had a range of educational backgrounds, with 12.9% of mothers and 18.2% of fathers having a high school education or less, 37.2.% of mothers and 25.1% of fathers having some college or a vocational degree, and 34% of mothers and 46.3% of fathers having a bachelor’s degree or higher.
The present study analyzed data from participants who completed a daily diary protocol (N = 236). Adolescents in this subsample were 17.77 (SD = 0.39) years old on average and had been diagnosed with T1D for 7.34 (SD = 3.88) years; 62% were female, 43% used an insulin pump, and 63% were above the ADA age-specific recommendations (HbA1c < 7.5%) for glycemic control, M (SD) = 8.27 (1.62)%.
Procedure
The study was approved by the IRBs at the University of Utah, University of Texas Southwestern Medical Center at Dallas, and University of California, Merced. Procedures were developed collaboratively with and approved by staff at participating clinics. Parents provided informed consent and late adolescents provided consent or assent. Procedures involved an initial in-person research session, where participants completed performance-based measures of EF, received instructions for completing an online survey and a two-week online daily diary, and completed an HbA1c assay. Because extreme BG levels can affect cognitive performance (Desrocher & Rovet, 2004), participants checked their BG prior to cognitive testing; participants were allowed to complete testing if their BG levels were between 75 and 400. Participants who scored outside this range were asked to address the problem (e.g., get a snack, take a walk) and BG was retested every 15 minutes until it was within range. One participant was rescheduled when BG was not brought in range after three attempts. BG levels were unrelated to performance-based measures of EF, indicating these procedures were effective.
Following the in-person research session, participants received an email link to their confidential online survey with instructions to complete the survey individually. After completing the survey, a 14-day diary protocol began. On a daily basis, participants received an electronic link to a brief confidential survey, with instructions to complete the diary by the end of the day. Participants received phone calls or text messages if they had not completed the diary by 9 p.m. on a given day to encourage participation and address problems. Adolescents completed an average of 11.4 daily diaries (SD = 3.3). Adolescents were paid $50 for completing the in-person research session and online survey, and $5 for completing each daily diary.
Survey (Individual Difference) Measures
Executive Functioning - Performance Assessment.
During the in-person testing session, participants completed four subtests from the Delis-Kaplan Executive Function System battery (D-KEFS; Delis, Kaplan, & Kramer, 2001): Trail Making (Number Letter Sequencing completion time); Color-Word Interference (Inhibition and Inhibition/Switching completion times); and Verbal (Letter and Category correct responses) and Design Fluencies (number of correct responses for 3 conditions).
Generation of the EF score for use in analyses consisted of a three-step process. First, the mean of the resulting eight norm-based age-corrected scaled scores (Delis et al., 2001) was computed to create an EF composite score. Reliability in this sample was α = .84. Second, because of the hierarchical structure of cognition (Lezak et al., 2013), it was necessary to isolate EF above and beyond lower-order component processes which are known to confound performance on EF tests (Duke & Harris, 2014; Suchy et al., 2016). Six tasks from the D-KEFS battery are specifically designed to control for these confounds (i.e., Color Naming and Word Reading from the Color-Word Interference Test, and Visual Scanning, Number Sequencing, Letter Sequencing, and Motor Speed from the Trail Making Test). The mean of the norm-based age-corrected scaled scores from these scales (Delis et al., 2001) was computed to create a nonexecutive component composite score. Reliability in this sample was α = .83. Third, to remove variance due to the lower-order component processes from the EF composite (i.e., to unconfound them), an unstandardized residual for the EF composite was computed after controlling for the non-EF lower-order composite. This residual was used in all analyses. Higher values indicated better EF-performance.
IQ.
Because IQ contributes to performance on most cognitive tests, including EF (Lezak et al., 2013), it was also necessary to control for IQ to ensure that any observed effects can be attributed to the specific EF construct (Suchy et al., 2016). To generate an IQ estimate, adolescents completed the Vocabulary subtest of the Wechsler Adult Intelligence Scale-4th Edition (WAIS-IV; Wechsler, 2008) during the in-person testing session. This subtest measures word knowledge, and is a highly reliable estimate of crystallized verbal IQ (Lezak et al., 2013; Wechsler, 2008), which is distinguishable from EF (Richland & Burchinal, 2013). Split-half reliability for the Vocabulary subtest for ages 16 to 19 is excellent at .93 (Wechsler, 2008). Norm-based age-corrected scaled scores were analyzed as covariates.
Problems with Executive Functioning – Survey Assessment.
As part of the on-line survey, adolescents completed the widely used Behavior Rating Inventory of Executive Functioning-Self-Report (BRIEF) to assess a range of problems with EF in daily life. Participants rated each of 80 items on a 3-point scale (0 = never to 2 = often) to indicate the frequency of each problem over the past six months. Items were combined into a global EF composite score following manual procedures (Guy, Isquith, & Gioia, 2004). Higher scores reflected greater self-reported EF problems. Reliability in this sample was α = 0.96.
Adherence.
Participants completed the Diabetes Behavior Rating Scale (DBRS) (Iannotti et al., 2006) to measure adherence. This 37-item scale assesses adherence to the multiple behaviors required to keep BG levels in a relatively normal range (e.g., checking BG levels, counting carbohydrates, adjusting insulin dose in response to BG levels, diet, and exercise), includes items relevant to current practice recommendations and technologies (e.g., intensive therapy, insulin pump), and correlates well with more time-intensive interview measures of adherence (Iannotti et al., 2006). Manual-based scoring procedures resulted in a proportion ranging from 0 to 1, with higher scores indicating better adherence. Reliability in this sample was α = .84.
Diabetes Goal Planning.
Participants were initially asked to think about current diabetes goals they would be working on daily over the subsequent two weeks, and to provide a one-sentence description of their most important diabetes-related goal. Coding of goal content revealed the most common goals were to control BG levels (61%) and to check BG levels more often (17%); no other goal codes were described by more than 5% of participants. Participants then completed the four-item planning subscale from the Goal Systems Assessment Battery in reference to their diabetes goal (Karoly & Ruehlman, 1995; Maes & Karoly, 2005). Items described participants’ planning directed at facilitating goal attainment and preventing goal disruption (e.g., I try to plan out things I will do in small steps to reach this diabetes goal; I try not to let others get in the way of my work on this diabetes goal), and were rated using a 0 (not at all true for me) to 4 (describes me very well) point Likert-type scale. Average ratings across items were analyzed with higher scores indicating higher diabetes goal planning. Reliability in this sample was α = .78.
Glycemic control.
Glycemic control was indexed using glycated hemoglobin (HbA1c) from HbA1c assay kits obtained from and processed by CoreMedica Laboratories (www.coremedica.net). Blood samples were collected during participants’ in-person laboratory session and mailed to CoreMedica Laboratories for processing. Higher scores indicate poorer glycemic control over the preceding three to four months.
Daily Diary
To reduce burden and maintain motivation on the daily diary protocol, it was necessary to measure constructs with as few items as possible.
Daily Diabetes Goal Planning and Goal Effort.
After being reminded of their most important diabetes goal, participants rated their agreement with two items to indicate their level of effort and planning towards achieving that goal in the past 24 hours using a 1 (strongly disagree) to 5 (strongly agree) scale. Goal effort was assessed with the item “I tried very hard to make progress toward this T1D goal today” (Affleck et al., 2001) and goal planning was assessed with the item “I tried not to let other people get in the way of my work on this T1D goal today.” The daily goal planning item was selected because it had the highest loading on the 4-item goal planning subscale from the Goal System Assessment Battery that was measured in the survey portion of this study, and addresses a major social barrier that disrupts adolescent T1D management (Mulvaney et al., 2011).
Daily adherence.
Six items from the Self-Care Inventory (Lewin et al., 2009) that measure adherence behaviors that typically occur daily were adapted to index daily adherence (Berg et al., 2014): checking BG, administering insulin dose as recommended, adjusting insulin based on BG values, having quick-acting sugar available to treat reactions, eating the proper foods or counting all carbohydrates, and using pump or continuous monitor correctly (if relevant). Items were rated on a scale from 1 (did not do it at all) to 5 (did it exactly as recommended) to indicate adherence to recommendations in the past 24 hours. Scores across items were averaged to index daily adherence. Internal consistency among items was α = .84.
Daily BG Checks and Levels.
Participants reported each BG reading recorded on their glucometer at the end of each day. The number of BG checks reported each day was analyzed as a second index of daily adherence (Hood, Peterson, Rohan, & Drotar, 2009), and the average of BG levels recorded across the day was calculated to index participants’ level of daily BG control. The average daily BG level was 188.74 (SD = 60.94) mg/dl, which exceeds the 180 mg/dl level considered to be hyperglycemic. Thus, higher average values indicated poorer daily BG control.
Analysis Plan
Across all the included variables, 63% of cases had complete data; however, the missingness was relatively small for any individual, and diffuse with missing a single value as the modal pattern. To account for missing data, we generated five datasets through multiple imputation (MI; Graham, 2009). The imputation procedure included variables beyond the presented analyses to ensure an adequate ‘missing at random’ model. The additional variables reflected aspects of self-regulation (e.g., neurocognitive and self-regulation variables other than EF, emotion regulation variables, self-efficacy) and social relationship processes that may be important for diabetes management at this time of development (e.g., mother/father monitoring and relationship quality, adolescent secrecy and disclosure, peer support). These variables were related to the current study variables and were relevant to the full set of aims in the larger study. The MI procedure for the survey data was conducted in SPSS23; the procedure for the diary data was conducted separately in Mplus7.31 by specifying a cluster ID variable along with a two-level structure within the MI data generation step. In both procedures, we imputed missing data at the level of the variable (i.e., scale or subscale scores) rather than the item.
To address Aim 1, correlations were conducted to examine whether individual differences in goal planning were related to T1D outcomes (i.e., adherence and glycemic control). Hierarchical regression analyses determined whether these associations occurred above and beyond a person’s EF capacity. Separate regressions were conducted for survey and performance measures of EF. Covariates and EF were entered as predictors on Step 1, with survey measures of goal planning entered on Step 2. Covariates included variables commonly associated with T1D outcomes in prior research (i.e., IQ, illness duration, insulin pump status, and gender).
Before examining the remaining aims, we explored between- versus within-person sources of variance in the daily goal variables. Intraclass correlations (ICCs) for daily goal planning and daily goal effort were calculated using estimates obtained from unconditional (empty) models. The ICCs indicated that 46% of the variance in daily goal planning and 52% of the variance in daily goal effort was between-persons. This demonstrates that there are both between- and within-person sources of variance, and supports the examination of day-to-day fluctuations in daily goal planning and daily goal effort around an individual’s average scores across days.
To examine Aims 2 and 3, multilevel modeling using HLM7 (Raudenbush., Bryk, Cheong, Congdon, & du Toit, 2011) was conducted on diary data to determine whether day-to-day fluctuations in daily goal planning and goal effort were associated with day-to-day changes in T1D outcomes (i.e., daily adherence, daily BG checks, daily average BG level), and whether individual differences in EF moderated these associations. At Level 1, we examined within-person associations of daily goal planning and daily goal effort with each daily outcome. Random effects were specified on the intercept, as well as on each daily goal variable. At Level 2, we tested whether individual differences in the survey-measure of goal planning and in trait-level EF predicted the intercept, and whether EF moderated the Level 1 associations of daily goal planning and daily goal effort with daily T1D outcomes. Separate models were conducted for survey and performance measures of EF, and for each T1D management variable. The following model illustrates the analysis of daily adherence with EF measured by the BRIEF. Parallel analyses were conducted using performance measures of EF for each outcome:
Level 1 daily goal variables were person mean centered to reflect an individual’s daily deviations from his or her own mean, day was centered at the mid-point of the diary to estimate an average day across the two weeks; with the exception of sex which was uncentered (0 = female; 1 = male), Level 2 variables were grand mean centered to reflect an individual’s deviations from the sample mean. Thus, at Level 1 (within-person, Equation 1a), an individual i’s adherence on day t was modeled as a function of his or her daily intercept (β0i), daily slopes for daily goal planning (β1i) and daily goal effort (β2i), day (β3i), and residual variance (eti). The daily slopes reflect changes in participants’ adherence on days when they had higher levels of daily goal planning or daily goal effort than their mean across the 14 days. At Level 2 (between-person; Equation 1b), the Level 1 intercept was modeled as a function of the sample average intercept (γ00), slopes for covariates (γ01, γ02, γ03), slopes for EF (γ04) and goal planning survey scores (γ05), and random effects (u0i). The Level 2 slopes predicting the intercept reflect differences in average daily adherence as a function of individual differences in goal planning and EF. Finally, the Level 1 slopes for daily goal planning (Equation 1c) and daily goal effort (Equation 1d) were modeled as a function of individual differences in EF (γ11 and γ21) and random effects (u1i and u2i). The Level 2 slopes predicting the Level 1 slope reflect the extent to which associations of daily goal planning or daily goal effort with daily T1D outcomes differed as a function of whether the individual had higher or lower EF (compared to other participants). That is, these Level 2 coefficients (γ11 and γ21) indicate whether EF moderated Level 1 associations of daily goal effort and daily goal planning with daily T1D outcomes.
Results
Individual Differences in Survey Measures of Goal Planning and T1D Outcomes
Means and correlations among survey variables are reported in Table 1. Individuals with greater goal planning survey scores displayed better adherence and glycemic control. EF problems assessed via self-report were associated with lower levels of goal planning and poorer adherence and glycemic control, while performance measures of EF were only associated with better glycemic control. Regression analyses were conducted to determine whether individual differences in goal planning were associated with outcomes when entered after covariates and EF. Consistent with Aim 1 hypotheses, individuals with higher goal planning displayed better adherence [B (SE) = .068 (.009), ΔR2 = .197, p < .001; B (SE) = .077 (.009), ΔR2 = .276, p < .001], and better glycemic control [B (SE) = −.313 (.119), ΔR2 = .024, p < .01; −.374, B (SE) = .115, ΔR2 = .037, p < .001], after controlling for self-report and performance EF, respectively. It is notable that goal planning had a large effect on adherence, explaining 20 to 28% of the variance beyond that accounted for by the covariates and EF.
Table 1.
Correlations among individual difference measures of diabetes goal planning, executive functions, and diabetes management
| Mean (SD) | Goal Planning | EF Problems | EF Performance | HbA1c | Adherence | |
|---|---|---|---|---|---|---|
| Survey scores | ||||||
| Goal Planning | 3.062 (.833) | --- | ||||
| EF Problems (BRIEF) | 132.603 (23.358) | −.278** | ||||
| EF Performance | .025 (1.344) | −.040 | −.106** | |||
| HbA1c | 8.271 (1.627) | −.186** | .194** | −.185** | ||
| Adherence | .607 (.122) | .522** | −.345** | .073 | −.226** |
Note. EF = executive functioning; BRIEF = Behavioral Rating Inventory of Executive Functioning (higher values reflect more EF problems); EF Performance = residualized EF composite controlling for component composite (higher values reflect better EF performance);
p < .001;
p < .01;
p < .05.
Day-to-Day Fluctuations in Goal Planning, Goal Effort, and T1D Management
The next set of analyses used multilevel modeling to examine day-to-day associations of goal planning with daily T1D management. In these analyses, we initially examined whether individual differences in goal planning survey scores and EF predicted the intercept for each daily outcome (i.e., daily adherence, frequency of BG tests, average BG levels). An effect on the intercept would indicate that these individual differences predicted average levels of daily outcomes across the subsequent two-week diary (providing additional tests of Aim 1).
As reported in Table 2, individual differences in survey measures of goal planning predicted higher daily adherence, more frequent daily BG tests, and lower daily BG levels on average across the two-week diary (see rows for γ05). Consistent with results from survey data reported above, these associations occurred above and beyond individual differences in EF. In fact, although self-reported problems in EF predicted poorer average levels of daily adherence and daily BG, performance measures of EF did not predict the intercept for any daily outcome.
Table 2.
Multilevel models examining associations of daily goal planning and daily goal effort with daily diabetes outcomes moderated by individual differences in executive functions
| Predictor | Daily Adherence | Daily Frequency of BG Tests | Daily BG Mean |
|---|---|---|---|
| Analyses with Executive Functioning Problems (BRIEF) as Predictor | |||
| Intercept (γ00) | 4.109 (.050)**** | 3.644 (.130)**** | 193.809 (4.598)**** |
| EF Problems (γ04) | −.007 (.002)**** | −.008 (.004) | .467 (.155)*** |
| Survey Goal Planning (γ05) | .261 (.050)**** | .316 (.131)** | −12.319 (4.480)** |
| Daily Goal Planning (γ10) | .081 .016)**** | .086 (.042)* | −4.171 (2.071)* |
| EF Problems (γ11) | .002 (.001)*** | .000 (.002) | .001 (.085) |
| Daily Goal Effort (γ20) | .121 (.017)**** | .193 (.047)**** | −9.149 (2.037)**** |
| EF Problems (γ21) | .000 (.001) | −.000 (.002) | −.022 (.089) |
| Analyses with Performance Measure of Executive Functioning as Predictor | |||
| Intercept (γ00) | 4.114 (.051)**** | 3.643 (.137)**** | 193.700 (4.683)**** |
| EF Performance (γ04) | .040 (.033) | .065 (.085) | −2.532 (3.003) |
| Survey Goal Planning (γ05) | .307 (.048)*** | .389 (.125)*** | −16.490 (4.305)*** |
| Daily Goal Planning (γ10) | .083 (.016)**** | .090 (.041)* | −4.315 (2.068)* |
| EF Performance (γ11) | −.019 (.011)+ | −.067 (.031)* | 1.005 (1.384) |
| Daily Goal Effort (γ20) | .121 (.016)**** | .189 (.048)**** | −8.776 (2.080)**** |
| EF Performance (γ21) | −.003 (.011) | .030 (.031) | −1.702 (1.549) |
Note. Covariates (sex, years since diagnosis, IQ) were entered on the intercept in all models (covariate coefficients not displayed), and day was entered as a predictor of all level 1 outcomes (day coefficients not displayed); EF = Executive Functioning; BRIEF = Behavioral Rating Inventory of Executive Functioning (higher scores reflect more EF problems); BG = Blood glucose;
p < 001;
p < .005;
p < 01;
p < .05;
p=.081.
Aim 2 analyses associating daily goal variables with daily outcomes are reported in Table 2 (see rows for γ10 and γ20). Consistent with hypotheses, on days when late adolescents reported lower than their average levels of daily goal planning and daily goal effort, their daily adherence and BG testing frequency decreased and their daily BG levels increased.
Finally, Table 2 displays results for Aim 3 examining whether EF moderated the associations of daily goal planning and daily goal effort with daily T1D outcomes (see rows for γ11 and γ21). Self-reported problems in EF moderated associations between daily goal planning and daily adherence. As displayed in the top panel of Figure 1, the association between daily goal planning and daily adherence was stronger among those with more self-reported EF problems, suggesting their adherence was more derailed on days they showed lower than their average levels of daily goal planning. Performance measures of EF also moderated associations of daily goal planning with frequency of BG tests, and trended toward moderating associations with daily adherence. As displayed in the bottom panel of Figure 1, the association between daily goal planning and daily frequency of BG testing was again stronger among those with poorer EF, indicating that those with poorer EF were more derailed on days they had lower goal planning than usual. EF did not moderate associations between daily goal effort and daily outcomes.
Figure 1.
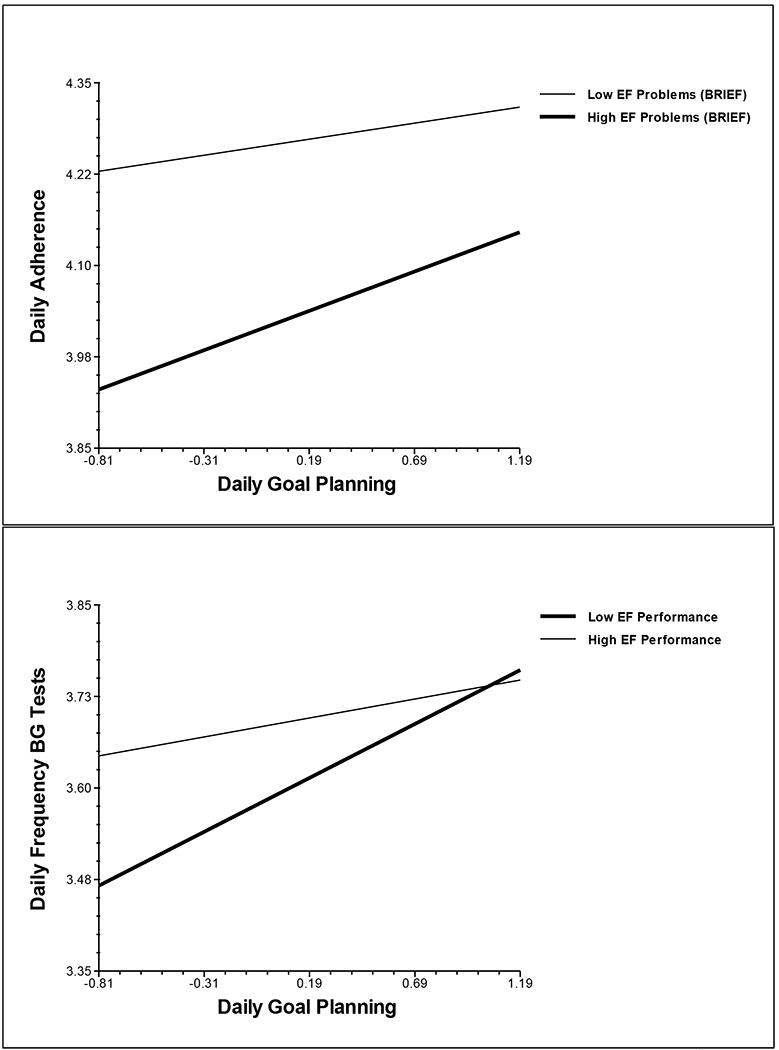
Executive functioning moderates the associations of daily goal planning with daily adherence and daily frequency of blood glucose tests.
Note. Predicted values were estimated for individuals with scores at the 25th and 75th percentile on EF and daily goal planning; EF = Executive Functioning; BRIEF = Behavioral Rating Inventory of Executive Functioning (higher scores reflect more EF problems); BG = Blood glucose.
Discussion
Diabetes goal planning appears to be an important aspect of managing T1D during late adolescence, a time of risk for poor illness management. Late adolescents who reported lower levels of diabetes goal planning displayed poorer adherence and glycemic control concurrently, as well as poorer daily adherence, less frequent daily BG checks, and poorer daily BG levels on average over the subsequent two weeks. Independent of individual differences in levels of goal planning, adolescents’ day-to-day fluctuations in daily goal planning were associated with day-to-day fluctuations in daily adherence and BG control, suggesting that even those who generally engage in goal planning can experience disruptive goal planning lapses in daily life. Finally, lapses in daily goal planning were more problematic for those with poorer EF, suggesting individuals with poorer EF may especially benefit from planning to achieve diabetes goals on a daily basis.
The associations between individual differences in diabetes goal planning and T1D management are compelling for several reasons. Associations were found both concurrently and prospectively (i.e., predicting daily management over the subsequent two week diary), and across self-report and objective measures, providing some confidence in the direction of associations and breadth of effects. Although EF underlies goal attainment (Hofmann, Schmeichel, & Baddeley, 2012), individual differences in goal planning were associated with T1D management above and beyond EF. Thus, findings of benefits for diabetes goal planning cannot be attributed solely to an individual’s EF, an index of one’s broader self-regulatory capacity. Finally, the effect sizes for associations with adherence were quite large. These findings demonstrate that late adolescents who plan more for how to achieve their diabetes goals or to prevent disruptions to goal progress may be better equipped to meet the complex challenges of T1D management.
Day-to-day fluctuations in goal planning and goal effort reveal the challenges of managing T1D in daily life. Late adolescents displayed a fair amount of variability from one day to the next in daily goal planning and effort, with only about half of the variance being between persons. Such day-to-day fluctuations were associated with important indices of T1D management. Specifically, on days participants reported greater than their average levels of daily goal planning and daily goal effort, they displayed better daily adherence and BG levels. Such fluctuations may reflect situational factors that undermine or facilitate goal planning or effort in daily life. Daily diary studies examining adults with chronic pain have identified personal and situational factors such as daily pain, fatigue, and positive or negative affect that contribute to day-to-day fluctuations in daily goal planning, goal effort, and ultimately goal progress (Affleck et al., 2001; Karoly et al., 2014; Mun, Karoly, Okun, Kim, & Tennen, 2016). Mulvaney and colleagues (2011) identified barriers to T1D management in younger adolescents, but late adolescents may experience unique daily barriers as they manage their T1D increasingly away from home and more independently from parents (Wdowik, Kendall, & Harris, 1997). Understanding the situational factors related to daily diabetes goal pursuit during late adolescence is an important area for future research, as such information may begin to identify daily processes to target in interventions.
Consistent with predictions, those with poorer EF showed stronger daily associations between goal-planning and adherence, indicating their adherence was more disrupted by daily goal-planning lapses. This moderation effect was not evident for daily goal effort, suggesting that goal effort is important across levels of EF, and pointing to some specificity in EF effects on daily goal planning per se. Theoretically, daily goal planning increases the chances of goal attainment by generating a priori scripts of possible scenarios in daily life and outlining steps for overcoming dynamically emerging barriers to success. While it may be possible to attain goals in the absence of a plan, doing so requires that an individual be able to quickly problem-solve in the moment as barriers to success emerge. Those with poorer EF may find it difficult to problem-solve effectively while “in the moment,” making it understandable that they benefit more from planning (Suchy, 2015). Future research designed to track and analyze within-day dynamics will be necessary to evaluate the accuracy of these speculations (see Karoly et al., 2014, for example).
The daily goal planning variable focused specifically on planning to keep others from interfering with one’s most important diabetes goal, which is likely to be particularly relevant for late adolescents. This item was selected because it had the highest loading on the survey goal planning measure, not because of its social focus. Different results may have been found with a different daily goal planning measure. Recent findings indicate that self- and social-regulation are intertwined, and point to the importance of regulating one’s social relationships during goal pursuit (vanDellen, Shah, Leander, Delose, & Bornstein, 2015). Daily lapses in self-regulation can occur due to a variety of social disruptions (e.g., Hofmann, Finkel, & Fitzsimons, 2015), and these may be particularly problematic during late adolescence as interactions with new social contexts outside the family become more prominent. Anticipating these social disruptions and planning for how to accomplish T1D goals in the face of social barriers may be quite important for late adolescents’ T1D management.
Results should be interpreted in the context of limitations. First, measures were primarily self-report and retrospective, and shared method variance may have influenced the findings. For example, participants’ end-of-day reports of daily goal planning or goal effort may have reflected their evaluations of the quality of their adherence that day rather than vice versa. Research designs that measure goal planning and goal effort earlier in the day before daily adherence behaviors occur will be necessary to address this issue (e.g., Karoly et al., 2014). Second, diabetes goal content was not considered in these analyses, despite the fact that the manner in which goals are framed can affect goal attainment (Mann et al., 2013). The most common diabetes goal focused on desired outcomes that require the coordination of multiple T1D management behaviors (e.g., keep blood sugar in range), which matched well to the multi-faceted measure of adherence. However, participants who had a more behavior-specific goal (e.g., take insulin before eating) may have shown a stronger association with a behavioral outcome that specifically matched their goal (e.g., adherence to insulin management only). Third, daily goal planning and effort were measured by single items to reduce participant burden and enhance diary completion rates, but this may have lowered their reliability. Fourth, the study was correlational and causal conclusions cannot be drawn. Finally, the sample was primarily non-Latino/a white, reflecting the demographic characteristics of those who develop T1D, and all participants were seniors in high school. The late adolescent context, in particular, may have affected the results. Late adolescents are managing T1D fairly independently, but are still developing the self-regulatory skills necessary to support such management (Wiebe et al., 2014). Because they commonly live at home with parents, however, parents may be able to compensate for low skill or lapses in self-regulation (Butner et al., 2017). Thus, the present findings provide a somewhat conservative test of the hypotheses and results may not generalize fully to other samples or age groups. Future research should examine the extent to which other factors such as parental support for diabetes management may explain or moderate these findings.
The present findings have implications for promoting effective T1D management during late adolescence. The finding that diabetes goal planning was associated with T1D outcomes separately from EF is important because goal planning is a skill that can be taught, while EF reflects more trait-like neurocognitive capabilities that may be less amenable to change. These findings thus suggest that late adolescents may benefit from interventions that teach diabetes goal planning skills. Assessment of individual differences in goal-planning and EF may be useful to identify those who need additional support and skill development in diabetes goal planning. Given that even individuals who engage in high levels of planning experience day-to-day lapses in diabetes goal planning, such goal planning interventions will need to consider the daily situational constraints that may disrupt diabetes goal attainment. Implementation intention interventions (e.g., developing if-then plans), for example, may be useful to teach late adolescents with T1D how to anticipate daily barriers and prevent daily disruptions to diabetes goal attainment (Gollwitzer & Oettingen, 2011). Late adolescents may also benefit from receiving planning help from family or friends, and from reducing social barriers that may disrupt daily goal planning and goal effort. Training in how to manage close relationships to support T1D (Mayberry, Berg, Harper, & Osborn, 2016) may thus be helpful. Although all individuals with T1D may benefit from better management of social relationships to support diabetes, the present findings suggest that those with poorer EF may have greater need for such interventions. These treatment implications are tentative and further research is necessary to support their development. The current findings warrant future research endeavors to understand the dynamic processes that underlie links between individual differences and day-to-day fluctuations in T1D goal planning, and ultimately to develop interventions to support more effective T1D management.
Acknowledgments
This research was supported by a grant from the National Institutes of Diabetes and Digestive and Kidney Diseases, R01 DK092939. During manuscript preparation, T.K.S was supported by a training grant from the National Cancer Institute at the National Institutes of Health CA193193. We thank Jessica Marino for help with manuscript preparation, the staff at participating endocrinology clinics, the READY Study research team, and the late adolescents who took time from their busy schedules to participate.
Contributor Information
Deborah J. Wiebe, Psychological Sciences and the Health Sciences Research Institute, University of California, Merced
Ashley C. Baker, Psychological Sciences and the Health Sciences Research Institute, University of California, Merced
Yana Suchy, Department of Psychology, University of Utah.
Tammy K. Stump, Department of Psychology, University of Utah; Department of Preventive Medicine, Northwestern University
Cynthia A Berg, Department of Psychology, University of Utah.
References
- Affleck G, Tennen H, Urrows S, Abeles M, Zautra A, & Karoly P (2001). Women’s pursuit of personal goals in daily life with fibromyalgia: A value-expectancy analysis. Journal of Consulting & Clinical Psychology, 69, 587–596. doi: 10.1037/0022-006X.69.4.587 [DOI] [PubMed] [Google Scholar]
- Berg CA, Wiebe DJ, Suchy Y, Hughes AE, Anderson JH, Godbey EI, … White PC (2014). Individual differences and day-to-day fluctuations in perceived self-regulation associated with daily adherence in late adolescents with type 1 diabetes. Journal of Pediatric Psychology, 39, 1038–1048. doi: 10.1093/jpepsy/jsu051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler J, Fortenberry KT, Berg CA, McCabe J, Blakemore T, & Wiebe DJ (2011). Early adolescents’ goals and mothers’ accuracy in predicting adolescent goals in the context of type 1 diabetes. Children’s Health Care, 40, 155–169. [Google Scholar]
- Butner JE, Berg CA, Munion AK, Turner SL, Hughes-Lansing A, Winnick JB, & Wiebe DJ (in press). Coordination of self- and parental-regulation surrounding type 1 diabetes management in late adolescence. Annals of Behavioral Medicine 10.1007/s12160-017-9922-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delis DC, Kaplan E, & Kramer JH (2001). Delis-Kaplan Executive Function System (D-KEFS). Psychological Corporation. [Google Scholar]
- Duke DC, & Harris MA (2014). Executive function, adherence, and glycemic control in adolescents with type 1 diabetes: A literature review. Current Diabetes Reports, 14, 532–542. doi: 10.1007/s11892-014-0532-y [DOI] [PubMed] [Google Scholar]
- Gollwitzer PM, & Oettingin G (2011). Planning promotes goal striving In Vohs KD & Baumeister RF (Eds.), Handbook of self-regulation (2nd Ed., pp. 162–185). New York: Guilford Press. [Google Scholar]
- Gollwitzer P, & Oettingen G (2007). The role of goal setting and goal striving in medical adherence In Park DC & Liu LL (Eds.), Medical Adherence and Aging. Social and Cognitive Perspectives (pp. 23–47). [Google Scholar]
- Graham JW (2009). Missing data analysis: Making it work in the real world. Annual Review of Psychology, 60, 549–576. doi: 10.1146/annurev.psych.58.110405.085530 [DOI] [PubMed] [Google Scholar]
- Guy SC, Isquith PK, & Gioia GA (2004). Behavioral rating inventory of executive function-self-report version: Professional manual. Lutz, FL: PAR. [Google Scholar]
- Hall PA, Fong GT, Epp LJ, & Elias LJ (2008). Executive function moderates the intention-behavior link for physical activity and dietary behavior. Psychology & Health, 23, 309–26. doi: 10.1080/14768320701212099 [DOI] [PubMed] [Google Scholar]
- Hofmann W, Finkel EJ, & Fitzsimons GM (2015). Close relationships and self-regulation: How relationship satisfaction facilitates momentary goal pursuit. Journal of Personality and Social Psychology, 109, 434–452. doi: 10.1037/pspi0000020 [DOI] [PubMed] [Google Scholar]
- Hofmann W, Schmeichel BJ, & Baddeley AD (2012). Executive functions and self-regulation. Trends in Cognitive Sciences, 16, 174–180. doi: 10.1016/j.tics.2012.01.006 [DOI] [PubMed] [Google Scholar]
- Hood KK, Peterson CM, Rohan JM, & Drotar D (2009). Association between adherence and glycemic control in pediatric type 1 diabetes: A meta-analysis. Pediatrics, 124. doi: 10.1542/peds.2009-0207 [DOI] [PubMed] [Google Scholar]
- Iannotti RJ, Schneider S, Nansel TR, Haynie DL, Plotnick LP, Clark LM, … Simons-Morton B (2006). Self-efficacy, outcome expectations, and diabetes self-management in adolescents with type 1 diabetes. Journal of Developmental and Behavioral Pediatrics, 27, 98–105. doi: 10.1097/00004703-200604000-00003 [DOI] [PubMed] [Google Scholar]
- Karoly P (2010). Goal Systems and Self‐Regulation In Hoyle RH (Ed.). Handbook of Personality and Self-Regulation, (pp. 218–242). Oxford, UK: Blackwell. [Google Scholar]
- Karoly P, Okun MA, Enders C, & Tennen H (2014). Effects of pain intensity on goal schemas and goal persuit: A daily diary study. Health Psychology, 33, 968–976. 10.1037/hea0000093.supp [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karoly P, & Ruehlman LS (1995). Goal cognition and its clinical implications: development and preliminary validation of four motivational assessment instruments. Assessment, 2, 113–129. doi: 10.1177/107319119500200202 [DOI] [Google Scholar]
- Lewin AB, LaGreca AM, Geffken GR, Williams LB, Duke DC, Storch EA, & Silverstein JH (2009). Validity and reliability of an adolescent and parent rating scale of type 1 diabetes adherence behaviors: The Self-Care Inventory (SCI). Journal of Pediatric Psychology, 34, 999–1007. doi: 10.1093/jpepsy/jsp032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lezak MD, Howieson DB, Bigler ED, & Tranel D (2013). Neuropsychological Assessment, fifth edition. Oxford University Press. [Google Scholar]
- Maes S, & Karoly P (2005). Self-regulation assessment and intervention in physical health and illness: A review. Applied Psychology: An International Review, 54, 267–299. doi: 10.1111/j.1464-0597.2005.00210 [DOI] [Google Scholar]
- Mann T, de Ridder D, & Fujita K (2013). Self-regulation of health behavior: Social psychological approaches to goal setting and goal striving. Health Psychology, 32, 487–98. doi: 10.1037/a0028533 [DOI] [PubMed] [Google Scholar]
- Mayberry LS, Berg CA, Harper KJ, & Osborn CY (2016). The design, usability, and feasibility of a family-focused diabetes self-care support mHealth intervention for diverse, low-income adults with type 2 diabetes. Journal of Diabetes Research, 2016, 13. doi: 10.1155/2016/7586385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller KM, Foster NC, Beck RW, Bergenstal RM, DuBose SN, DiMeglio L et al. , … Tamborlane WV (2015). Current state of type 1 diabetes treatment in the U.S.: Updated data from the T1D exchange clinic registry. Diabetes Care, 38, 971–978. doi: 10.2337/dc15-0078 [DOI] [PubMed] [Google Scholar]
- Mulvaney SA, Hood KK, Schlundt DG, Osborn CY, Johnson KB, Rothman RL, & Wallston KA (2011). Development and initial validation of the barriers to diabetes adherence measure for adolescents. Diabetes Research and Clinical Practice, 94, 77–83. doi: 10.1016/j.diabres.2011.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mun CJ, Karoly P, Okun MA, Kim H, & Tennen H (2016). Affect, work schemas, and work-goal striving among adults with chronic pain: A multilevel structural equation analysis. Journal of Behavioral Medicine, 39, 288–299. doi 10.1007/s10865-015-9696-4 [DOI] [PubMed] [Google Scholar]
- Raudenbush. S, Bryk A, Cheong YF, Congdon R, & du Toit M (2011). HLM 7: Linear and nonlinear modeling. Lincolnwood, IL: SSI. [Google Scholar]
- Suchy Y (2015). Executive Funtioning: A comprehensive guide for clinical practice. New York, NY: Oxford University Press. [Google Scholar]
- Suchy Y, Turner SL, Queen TL, Durracio K, Wiebe DJ, Butner J, … Berg CA (2016). The relation of questionnaire and performance-based measures of executive functioning with Type 1 diabetes outcomes among late adolescents. Health Psychology, 35, 661–669. doi: 10.1037/hea0000326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vancouver JB, Weinhardt JM, & Schmidt AM (2010). A formal, computational theory of multiple-goal pursuit: Integrating goal-choice and goal-striving processes. Journal of Applied Psychology, 95, 985–1008. doi: 10.1037/a0020628 [DOI] [PubMed] [Google Scholar]
- vanDellen MR, Shah JY, Leander NP, Delose JE, & Bornstein JX (2015). In good company: managing interpersonal resources that support self-regulation. Personality and Social Psychology Bulletin, 41, 870–882. doi: 10.1177/0146167215580778 [DOI] [PubMed] [Google Scholar]
- Wdowik MJ, Kendall PA, & Harris MA (1997). College students with diabetes: Using focus groups and interviews to determine psychosocial issues and barriers to control. The Diabetes Educator, 23, 558–562. doi: 10.1177/014572179702300507 [DOI] [PubMed] [Google Scholar]
- Wechsler D (2008). Wechsler Adult Intelligence Scale (4th ed.). San Antonio, TX: Pearson. [Google Scholar]
- White NH, Cleary PA, Dahms W, Goldstein D, Malone J, & Tamborlane WV (2001). Beneficial effects of intensive therapy of diabetes during adolescence: Outcomes after the conclusion of the Diabetes Control and Complications Trial (DCCT). Journal of Pediatrics, 139, 804–812. doi: 10.1067/mpd.2001.118887 [DOI] [PubMed] [Google Scholar]
- Wiebe DJ, Chow CM, Palmer DL, Butner J, Butler JM, Osborn P, & Berg CA (2014). Developmental processes associated with longitudinal declines in parental responsibility and adherence to type 1 diabetes management across adolescence. Journal of Pediatric Psychology, 39(5), 532–541. 10.1093/jpepsy/jsu006 [DOI] [PMC free article] [PubMed] [Google Scholar]


