Abstract
Objective:
To assess the comparative effectiveness of alternative incentive-based interventions to promote HIV testing among men.
Design:
Randomized clinical trial.
Methods:
We enumerated four Ugandan parishes and enrolled men ≥18 years. Participants were randomized to six groups that received incentives of varying type and amount for HIV testing at a 13-day community health campaign. Incentive types were: gain-framed (control): participants were told they would receive a prize for testing; loss-framed: participants were told they had won a prize, shown several prizes, asked to select one, then told they would lose the prize if they did not test; lotteries: those who tested had a chance to win larger prizes. Each incentive type had a low and high amount (~US$1 and US$5/participant). The primary outcome was HIV testing uptake at the community health campaign.
Results:
Of 2,532 participants, 1,924 (76%) tested for HIV; 7.6% of those tested were HIV-positive. There was no significant difference in testing uptake in the two lottery groups (78%; p=0.076) or two loss-framed groups (77%; p=0.235) vs. two gain-framed groups (74%). Across incentive types, testing did not differ significantly in high-cost (76%) vs. low-cost (75%; p=0.416) groups. Within low-cost groups, testing uptake was significantly higher in the lottery (80%) vs. gain-framed (72%; p=0.009) group.
Conclusions:
Overall, neither offering incentives via lotteries nor framing incentives as losses resulted in significant increases in HIV testing compared to standard gain-framed incentives. However, when offering low-cost incentives to promote HIV testing, providing lottery-based rewards may be a better strategy than gain-framed incentives.
Keywords: HIV testing, Incentives, Lotteries, Loss aversion, Randomized-controlled trial, Men, Uganda
Introduction
Knowledge of one’s HIV status is a critical first step in accessing HIV prevention and treatment services and is essential for realizing the potential of antiretroviral therapy (ART)-based prevention. Achieving high testing coverage is also imperative for meeting the UNAIDS 90-90-90 targets to end the AIDS epidemic, which begin with a goal of 90% of HIV-infected persons knowing their status by 2020.[1] However, despite expansion of HIV testing services in sub-Saharan Africa nearly half of HIV-infected people remain unaware of their status.[2] Men in particular are more likely to have never having tested for HIV.[2] The impacts of this disparity include delayed entry into HIV care, delayed ART start and higher mortality among men compared to women.[3–5] Late or non-diagnosis with HIV infection also results in missed opportunities for HIV prevention. Interventions that can boost testing uptake among men are therefore urgently needed.
Economic incentives have been shown to promote a number of health behaviors.[6–8] Such incentives have a conventional economic rationale as they reduce the cost of undertaking a health behavior, as well as a behavioral economics rationale because they address individuals’ tendency to delay behaviors for which costs may be immediate whereas benefits may lie in the future. For HIV testing, the immediate costs may include transportation to testing sites, stigma, and anxiety about obtaining test results, whereas benefits, such as maintaining health with ART and reducing transmission to sexual partners, may be more distant. Indeed, providing small economic incentives has been shown to achieve increases in various HIV prevention-related behaviors including HIV testing, antenatal clinic visits by HIV-positive women, and medical male circumcision.[9–11]
However, most incentive-based approaches to promote health behaviors, particularly in resource-limited settings, have relied on standard, gain-framed incentives (providing a small reward for carrying out a behavior) and have not utilized additional insights from behavioral economics that may yield better results at comparable or lower cost. For example, as people generally pay greater attention to the magnitude of a reward than the probability of winning, offering lotteries with low probabilities of winning large prizes may be more appealing than gain-framed incentives, at equivalent per-person programmatic cost.[12] Additionally, people display loss aversion in their decision-making: gaining something of value is less motivating than losing something of equal value. [12] In a few trials in the United States, incentive-based interventions using lotteries and loss aversion have been shown to promote behaviors such as smoking cessation, weight loss, and physical activity.[13–15] Yet these alternative incentive types have rarely been attempted in low-income countries, and their effectiveness compared to gain-framed incentives for HIV testing is unknown.
To identify practical interventions that can increase HIV testing rates and test behavioral economics theories in the field, we conducted a randomized trial to assess the comparative effectiveness of alternative incentive-based interventions.
Methods
We conducted a 3×2 factorial, randomized trial to study the comparative effectiveness of novel incentive strategies at high and low incentive amounts, informed by behavioral economics, to promote HIV testing among men living in rural Uganda (NCT:02890459).
From April-June 2016, we enrolled participants from villages in four rural parishes in Mbarara District, Uganda. The parishes are geographically adjacent to one another and fall within the catchment area of one PEPFAR-supported government clinic where HIV treatment and other health services are available. We first enumerated residents of the study communities via a door-to-door census of all households; 13,971 residents were enumerated. All census participants provided verbal informed consent in their preferred language with fingerprint confirmation of agreement. We also performed digital biometric fingerprint measurements (U.are.u 4500 Reader, Digital Persona, Crossmatch, FL, USA) of all available household members.
We offered enrollment to all census-enumerated, adult (≥18 years) men who had been living in the community for ≥6 months in the year prior to enumeration and had no intention of moving away from the community in the next three months (N=2,784). Men who agreed to participate and provided written informed consent were administered a baseline questionnaire regarding their health, socioeconomic status, and HIV testing history.
Participants chose pre-printed scratch cards from several offered by study staff to unveil study group allocation. Daily tallies of randomization scratch cards distributed and returned to the study offices were kept and compared to enrollment numbers to ensure that no more than one scratch card was distributed for each participant. Participants were randomized (by block randomization, with block size = 30 and allocation sequence computer-generated prior to initiation of trial enrollment by study investigators) to six groups that received incentives of varying types and amounts for free HIV antibody testing at multi-disease community health campaigns (CHCs) in their communities over two-weeks in June-July 2016 (Figure 1). Such CHCs represent a form of rapid, large-scale community-based health service delivery that has been implemented in other Ugandan and Kenyan communities.[16, 17] A total of 13 CHC days were held throughout the four parishes, and all community members including women and children could receive CHC services.
Figure 1.
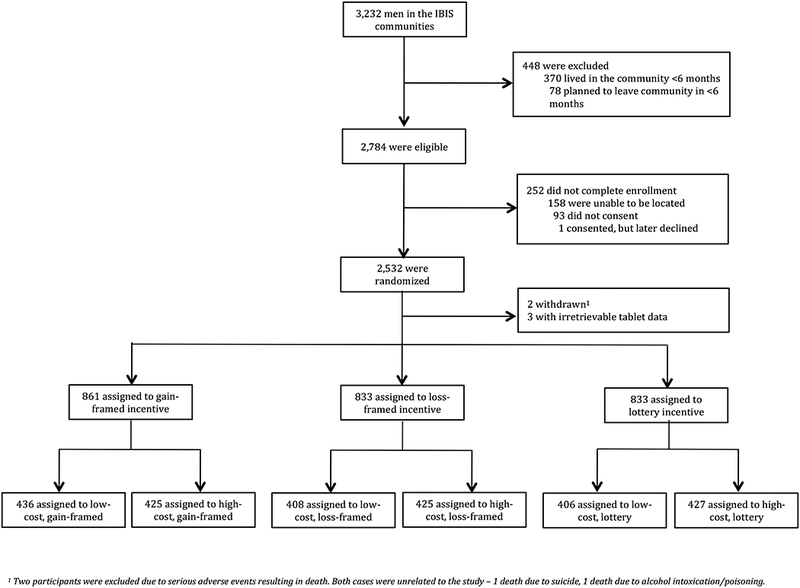
Trial CONSORT diagram with assessment for eligibility and randomization.
The three incentive types for study participants were: 1) standard, gain-framed incentives (control); 2) loss-framed incentives; and 3) lottery-based incentives. Participants randomized to gain-framed incentives were told they would receive a small prize, such as a washbasin or hoe, if they came to the CHC for HIV testing (they could choose the prize at the CHC). Participants randomized to loss-framed incentives were congratulated at the time of enrollment and told they had won a small prize. They were then shown photos of various prizes, asked to consider and choose the prize they wanted, and then given a card containing a photo of the prize they chose. Finally, they were told they would lose that prize if they did not come for HIV testing. Participants randomized to lottery-based incentives were told that if they participated in HIV testing they would automatically enter a lottery and have a chance to instantly win large prizes such as mobile phones and bicycles at the campaign. Probabilities of winning lottery prizes ranged from 1 in 10 to 1 in 25, with higher value prizes having lower probability. Lottery scratch cards were used at the campaign, so that when a participant in the lottery group completed participation in the health campaign, including testing for HIV, he could select one scratch card that indicated if he had won a prize or not. Appendix 1 provides further detail on these incentive types.
Each incentive type had a low and high amount, with a per-participant cost (from the program perspective) of about US$1 and US$5 respectively. Though the value of a reward and receiving an award may be on the same causal pathway in which incentives promote behavior change, the expected value (amount) of the reward is independent from the incentive type (i.e. gain-framed, loss-framed or lottery), and as such, we considered it justifiable to compare three incentive types at two amounts using a 3×2 factorial trial design. For the low-cost and high-cost lotteries, prizes and corresponding probabilities of winning them were selected in such a way as to ensure per-participant costs of US$1 and US$5 respectively. All prizes were chosen in consultation with village leaders, and were distributed after HIV testing and counseling was completed. Lottery participants were given a scratch card that either revealed a prize or thanked the participant for coming to the campaign.
At the CHC, point-of-care rapid HIV antibody testing was performed by finger-prick blood collection using test kits and a serial testing algorithm based on Uganda Ministry of Health guidelines.[18] Additional CHC services included pre- and post-test HIV counseling, screening of adults for hypertension, diabetes mellitus, malaria (if attendee reported fever) and tuberculosis (by sputum microscopy, if attendee reported cough for >2 weeks), and vitamin A and deworming treatment for children <5 years, as we have previously described.[16] The streamlined delivery of services at CHCs allows for large numbers of individuals to be tested over a short duration of time, as prior studies have shown.[19, 20]
The primary outcome was participation in HIV testing at the CHC. Participant identification and CHC attendance were verified by fingerprint biometric measurement at the campaign. A secondary outcome was HIV positivity among participants who tested for HIV.
We used χ2 tests to make a pre-specified comparison of the primary outcome in the loss-framed vs. gain-framed groups and lottery vs. gain-framed groups. We hypothesized that HIV testing uptake in the alternative incentive groups would be higher than uptake in the two gain-framed groups. Additionally, separately at the low and high incentive amounts, we used the χ2 test to compare testing uptake in each of the alternative incentive groups to the gain-framed incentive group. In accordance with the factorial trial design, we also estimated a modified Poisson regression model with robust error variance that included interaction terms between incentive type and incentive amount.
For the secondary outcome of HIV positivity among participants who tested for HIV at the CHC, we used χ2 tests to perform similar comparisons. Consistent with the theory that risk-seeking individuals would prefer lotteries, we hypothesized that the proportion of testers who tested HIV-positive would be higher in the lottery incentive groups than the gain-framed groups. To account for multiple hypothesis testing in the analysis of primary and secondary outcomes, we used a Bonferroni correction with resulting p-values of 0.01 (for five tests in the 3×2 factorial design, with an initial criterion for significance of alpha=0.05).
We used regression models to perform subgroup analyses that compared HIV testing uptake in the alternative incentive types to the gain-framed incentive among men considered highest priority for HIV testing based on prior testing and sexual behavior. Subgroups included participants who had or had not tested for HIV in the 12 months prior to enrollment, and those with multiple (>1) or one self-reported sexual partners. Additional subgroups we examined were participants with above- and below-median income. We used modified Poisson regression models with robust error variances and adjusted for incentive cost. As above, we used a Bonferroni correction with resulting p-values of 0.008 for the subgroup analyses (for six comparisons, with an initial criterion of significance of alpha=0.05)
Power calculations were used to determine the minimum detectable effect sizes in comparisons of HIV testing uptake among the three incentive types. We estimated that with 3,000 participants, there would be 80% power to detect absolute differences of at least 6 percentage points in HIV testing uptake between the gain-framed incentive groups and either of the two alternative incentive groups (α=0.05, two-sided), assuming HIV testing uptake as low as 30% in the gain-framed groups. In addition, there would be 80% power to detect absolute differences of at least 9 percentage points in testing uptake between the low-cost, gain-framed incentive group and each of the other five intervention groups.
The Makerere University School of Medicine Research and Ethics Committee (Uganda), the Ugandan National Council on Science and Technology, and the University of California San Francisco (UCSF) Committee on Human Research (USA) approved the study protocol. The UCSF Committee on Human Research served as the institutional review board of record for investigators from the University of North Carolina and the University of Pennsylvania (USA).
Results
Overall, 2,532 participants (91% of enumerated men who met eligibility criteria) were enrolled and randomized; 2,527 (99.8%) had full data available for analysis (Figure 1). Demographic and economic characteristics of participants did not differ significantly across study groups (Table 1). Among all participants, the median age was 36 years and farming was the most common occupation (51%). Participants’ median daily wage was US$1 (IQR: $0.60-$1.80). Prior testing history did not vary by study group: 78% (1,959/2,527) reported ever HIV testing and 48% (1,218/2,527) reported HIV testing in the 12 months prior to enrollment.
Table 1.
Participant demographics and characteristics.
| Incentive type | Gain-framed |
Loss-framed |
Lottery |
p-value1 | |||||
|---|---|---|---|---|---|---|---|---|---|
| Low-cost | High-cost | Low-cost | High-cost | Low-cost | High-cost | ||||
| No. of participants enrolled | 436 (17) | 425 (17) | 408 (16) | 425 (17) | 406 (16) | 427 (17) | - | ||
| Age2 [mean (SD)] | 38 (15) | 37 (15) | 40 (17) | 39 (16) | 39 (16) | 39 (16) | 0.345 | ||
| Education | 0.484 | ||||||||
| Primary or less | 305 (70) | 316 (75) | 295 (75) | 316 (75) | 298 (74) | 327 (77) | |||
| Secondary | 92 (21) | 85 (20) | 85 (20) | 72 (17) | 78 (19) | 72 (17) | |||
| More than secondary | 39 (9) | 23 (5) | 23 (5) | 37 (9) | 30 (7) | 28 (6) | |||
| Marital status | 0.949 | ||||||||
| Married/cohabitating | 289 (66) | 288 (68) | 275 (67) | 300 (70) | 270 (66) | 297 (70) | |||
| Single | 121 (28) | 111 (26) | 106 (26) | 97 (23) | 108 (27) | 105 (24) | |||
| Separated/divorced/widowed | 26 (6) | 26 (6) | 27 (7) | 28 (7) | 28 (7) | 25 (6) | |||
| Occupation | 0.566 | ||||||||
| Agriculture/farming | 221 (51) | 215 (51) | 202 (50) | 214 (50) | 204 (50) | 231 (54) | |||
| Manual labor | 109 (25) | 110 (26) | 110 (26) | 110 (26) | 115 (28) | 105 (25) | |||
| Business/sales/services | 46 (11) | 57 (13) | 50 (12) | 44 (10) | 49 (12) | 55 (13) | |||
| Professional | 20 (5) | 11 (3) | 11 (3) | 24 (6) | 12 (3) | 9 (2) | |||
| Student | 25 (6) | 19 (5) | 17 (4) | 13 (3) | 13 (3) | 17 (4) | |||
| Unemployed | 14 (3) | 12 (3) | 10 (2) | 17 (4) | 12 (3) | 9 (2) | |||
| Other | 1 (<1) | 1 (<1) | 0 (0) | 3 (1) | 1 (<1) | 1 (<1) | |||
| Daily Wage (USD)2, 3 | 0.507 | ||||||||
| Median (IQR) | 0.99 (0.60–1.79) | 0.90 (0.60–1.50) | 0.90 (0.60–2.39) | 0.99 (0.60–1.79) | 0.90 (0.48–1.79) | 1.20 (0.60–2.39) | |||
| Parish | 0.612 | ||||||||
| Mabira | 125 (29) | 119 (28) | 119 (28) | 128 (30) | 118 (29) | 123 (29) | |||
| Ruhunga | 155 (35) | 141 (33) | 134 (33) | 133 (31) | 144 (36) | 137 (32) | |||
| Katyazo | 131 (30) | 130 (31) | 135 (33) | 138 (33) | 129 (32) | 139 (33) | |||
| Itara | 25 (6) | 35 (8) | 19 (5) | 25 (6) | 14 (3) | 28 (7) | |||
| Has ever had an HIV test | 335 (77) | 323 (76) | 326 (80) | 330 (78) | 320 (79) | 325 (76) | 0.681 | ||
| HIV test in the past 12 months | 197 (45) | 204 (48) | 200 (49) | 200 (47) | 199 (49) | 218 (51) | 0.639 | ||
Data are n (%), unless otherwise specified;
Chi-square tests for equality across groups, unless otherwise specified;
ANOVA for equality across groups;
Average exchange rate during enrollment period: 3,344 UGX = 1 USD.
Over the 13 CHC days, 1,924 (76%) participants tested for HIV. HIV prevalence among all participants tested was 7.6% (146/1924). Among HIV-infected participants, 74/146 (51%) self-reported being newly diagnosed with HIV at the CHC: 23/146 (16%) self-reported no prior HIV testing, and 51 (35%) reported last testing HIV negative. Compared to HIV testing uptake in the two gain-framed groups (74%), there was no significant difference in testing uptake in the two lottery groups (78%; p=0.076) or two loss-framed groups (77%; p=0.235). Across incentive types, there was no significant difference in testing uptake in high-cost (~$5) vs. low-cost (~$1) per participant groups (77% vs. 75%, respectively; p=0.416; see Table 2).
Table 2.
HIV Testing at a multi-disease community health campaign (CHC) by randomized trial group: incentive type and cost.
| Incentive Type | N | Tested for HIV | % | p-value | HIV-positive, among tested | % | p-value | CD4+ cells/μL (IQR) |
|---|---|---|---|---|---|---|---|---|
| Gain-framed Incentive | 861 | 638 | 74% | Ref | 60 | 9.4% | Ref | 519 (386–661) |
| Loss-framed Incentive | 833 | 638 | 77% | 0.235a | 37 | 5.8% | 0.015a | 393 (279–519) |
| Lottery Incentive | 833 | 648 | 78% | 0.076a | 50 | 7.7% | 0.279a | 446 (300–647) |
| Low-cost Incentive (~$US1) | 1,250 | 943 | 75% | Ref | 78 | 8.3% | Ref | 446 (332–625) |
| High-cost Incentive (~$US5) | 1,277 | 981 | 77% | 0.416b | 69 | 7.0% | 0.307 | 444 (322–664) |
Compared to gain-framed;
Compared to low-cost incentives
IQR=Interquartile range
Among participants in the low-cost groups, testing uptake was significantly higher in the lottery group than the gain-framed incentive group (80% vs. 72%; p=0.009). There was no significant difference in testing uptake in the low-cost, loss-framed group (75%) compared to the low-cost, gain-framed group (72%; p=0.256; Figure 2). Among participants in the high-cost groups, HIV testing uptake in the lottery (76%) and loss-framed (78%) groups were not significantly different than in the gain-framed group (76%). In regression analyses that included interaction terms between incentive type and cost (Table 3), HIV testing uptake was significantly higher at low costs in the lottery group compared to the gain-framed incentive group (adjusted relative risk, aRR, 1.11; 95% CI 1.03–1.20). At high costs, however, lottery rewards were not more effective than gain-framed incentives.
Figure 2.
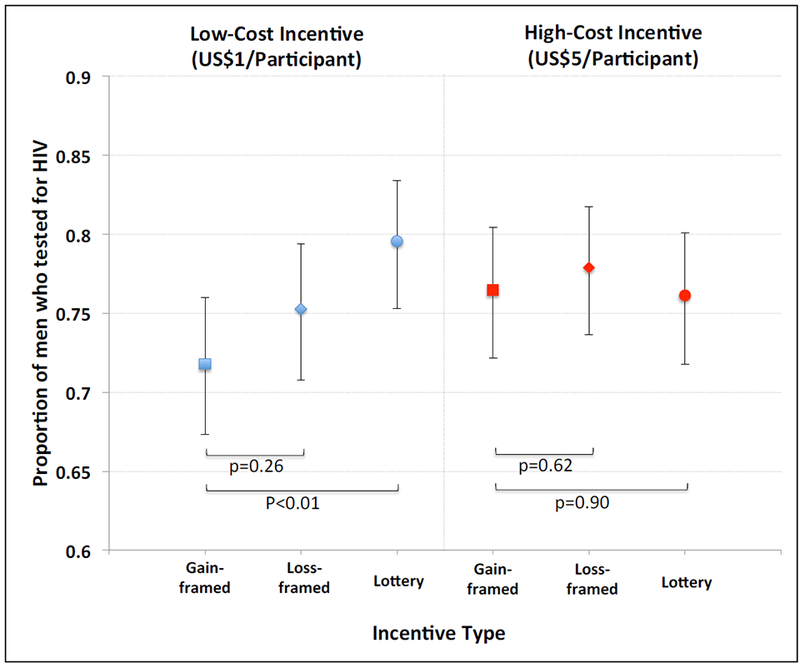
HIV testing uptake among men participating in a 3×2 factorial, randomized trial of novel incentive strategies (lottery-based incentives and loss-framed incentives) vs. standard, gain-framed incentives, with men in each incentive type arm randomized to high- vs. low-cost per participant incentive amount.
Table 3.
HIV Testing at a multi-disease community health campaign (CHC) by randomized trial group, with the low-cost, gain-framed incentive group as the reference group in the adjusted model, comparing incentive type and cost.
| Tested for HIV at CHC | |
|---|---|
| aRR (95% CI) | |
| Incentive type | |
| Gain-framed, low-cost | Ref. |
| Loss-framed, low-cost | 1.05 (0.97 – 1.14) |
| Lottery, low-cost | 1.11 (1.03–1.20)* |
| Incentive cost | |
| Low-cost | Ref. |
| High-cost | 1.07 (0.98 – 1.20) |
| Interaction of incentive type and cost | |
| High-cost × Loss-framed | 0.97 (0.87 – 1.08) |
| High-cost × Lottery | 0.95 (0.80 – 1.00) |
| Observations | 2,527 |
p<0.01
aRR= adjusted relative risk.
CI=Confidence Interval.
Ref=Reference group.
For the secondary outcome of HIV-positive testing among participants, there was no significant difference in HIV-positivity among testers in the lottery and gain-framed groups (7.7% vs. 9.4%; p=0.279), or in the proportion of participants newly diagnosed with HIV among testers in the lottery and gain-framed groups (4.8% vs. 4.4%; p=0.735). However, significantly fewer participants in the loss-framed groups tested HIV-positive than in the gain-framed groups (5.8% vs. 9.4%; p=0.015). In addition, significantly fewer participants in the loss-framed groups were newly diagnosed with HIV than in the gain-framed groups (2.4% vs. 4.4%; p=0.044).
Subgroup analyses revealed that among participants who had not tested for HIV in the 12 months prior to enrollment, HIV testing uptake was higher in the lottery groups than the gain-framed incentive groups, but did not reach statistical significance at p<0.008 (aRR 1.15, 95% CI: 1.03–1.28, p=0.012). There was no such difference when comparing the loss-framed groups to the gain-framed groups (aRR 1.06, 95% CI: 0.94–1.19). No significant differences were found by incentive type in a similar regression model among participants who had tested for HIV in the prior 12 months. A higher likelihood of HIV testing in the lottery group was also observed among participants reporting one sexual partner (aRR 1.12, 95% CI: 1.02–1.22, p=0.015), and participants with above-median daily income (aRR 1.13, 95% CI: 1.01–1.27, p=0.027), but neither was statistically significant at p<0.008. A similar trend, also not statistically significant, was observed among participants reporting multiple (>1) sexual partners and below-median daily wages (Supplementary Table 4).
Discussion
In this large randomized trial comparing two novel incentive interventions to standard, gain-framed incentives in rural Uganda, HIV testing uptake among adult men was not significantly higher when incentives were offered via lottery or framed as losses, compared to gain-framed incentives, or when the per-participant cost of incentives was increased from $1 to $5. However, in a pre-specified sub-group analysis, lottery-based incentives with per-participant costs of US$1 achieved 80% testing uptake among adult men and significantly higher testing uptake than gain-framed incentives (72%) of comparable cost – suggesting a potential benefit of lotteries over standard gain-framed approaches at low incentive values. The findings are timely and relevant given the 90-90-90 targets recently established by UNAIDS[1] and the common reliance of many donors, governments, and programs on low-cost, gain-framed incentives to promote health behaviors.[21] They suggest that countries and programs providing HIV testing services and not reaching priority populations could consider offering low-cost lottery-based incentives, rather than higher incentive amounts, in order to maximize uptake of services.
The incentive interventions tested in this study were chosen to leverage insights from behavioral economics and improve upon gain-framed incentives commonly used to promote health behaviors. While the latter approach has shown promise, studies have rarely assessed whether alternative incentive types can deliver better “bang for the buck”. Few studies have directly compared lottery incentives to gain-framed incentives: most have taken place in high-income countries with higher-cost incentives than those used in our study, and only one has focused on HIV testing.[14, 15, 22] These studies have found variable results, with one showing that lottery-based incentives were more effective in promoting weight loss in the United States[14] while another found that gain-framed incentives were more effective in promoting Chlamydia screening in the United Kingdom.[23] A trial in Lesotho compared lottery-based incentives for obtaining negative sexually transmitted infection test results every four months over two years to a control condition of no incentives and found a reduction in HIV incidence among lottery participants. However this trial did not compare the lottery intervention to other incentive strategies.[24] In one randomized trial, gain-framed and lottery-based incentives provided to households resulted in greater HIV testing uptake than no incentives among children from these households in Zimbabwe; the gain-framed and lottery incentive groups had similar HIV testing uptake, though the two incentive types were not directly compared.[22] The study most comparable to ours found that lottery-based incentives with per-participant costs of US$12.50 were less effective at increasing medical male circumcision in Kenya than equivalent gain-framed incentives.[25] In contrast, we found that low-cost lotteries may be more effective at promoting HIV testing among men than gain-framed incentives of equivalent cost. Encouragingly, we also found a potential signal that lotteries worked better among men who had not tested for HIV recently, a high priority population. However, the operational complexity of implementing novel incentive approaches, such as lotteries, merits consideration, and may also explain, in part, heterogeneity in the effectiveness of lotteries in different settings.
Interestingly, we found the lottery approach was more effective than a gain-framed approach at low incentive amounts but not at higher amounts. One explanation for this differential effect could be the “peanuts effect,”[26] as people may be more drawn to a lottery-based reward when the alternative is a small gain-framed incentive but not when the alternative is a large gain-framed reward. With rewards of higher amounts, a gain-framed incentive (i.e. a “sure thing”) becomes relatively more appealing than a gamble (or lottery). Our study offers the first field-based experimental evidence for this theory. Our findings indicate that for screening tests that can be conducted rapidly, keeping incentive amounts low and changing incentive design to lotteries may be more cost-effective than increasing the incentive amounts. Going forward, the question of how to scale lotteries for health outcomes in the public sector also merits consideration. Though the feasibility of implementing lotteries in the public sector is beyond the scope of our trial, lotteries and other games of chance are common in sub-Saharan Africa, with national lotteries held in Uganda (https://www.billionlotto.co.ug) and Kenya (https://mylotto.co.ke). Our study provides further supporting evidence that leveraging lotteries for health, in this case using a scratch card system to promote HIV testing, is feasible and acceptable in a rural African setting.
Although loss-framed incentives resulted in higher HIV testing uptake than gain-framed incentives at both incentive amounts, the differences in uptake were not statistically significant. Loss aversion as a motivating factor for behavior change has been well described and has served as a basis for deposit contract interventions that seek to impact behaviors such as smoking and exercise.[13, 15] Yet such interventions typically have low uptake and there are obvious barriers to implementing them in low-income settings. A key challenge therefore is to find novel ways to leverage loss aversion in incentive-based interventions. We attempted to address this challenge by enhancing ‘virtual’ ownership of incentive prizes and framing them as losses rather than gains. The limited impact of this approach may have been a result of an insufficient sense of true ownership of the incentive prizes. Loss framing may also be more effective for daily behaviors for which it is possible to establish a virtual endowment and provide regular notification about any losses incurred.[15] Other approaches to leveraging loss aversion to promote health behavior change are needed.
Offering testing services at multi-disease community health campaigns may partially explain the high levels of testing we observed. There is strong evidence that community-based HIV testing can achieve higher testing coverage than facility-based testing.[27, 28] However, men have had lower-than desired testing uptake in prior community-based approaches. HIV testing uptake among men at similar campaigns implemented in the study region, either without incentives (52%)[20] or with minimal incentives worth $0.20 per-participant (64%)[16] was lower than testing uptake among men in this study, all of whom received some incentive (76%). Though there is room for improvement even in the group with highest HIV testing uptake (80%), our findings show that the right types of incentives can offset barriers to testing for many men and achieve high testing coverage in campaigns.
Our study has limitations. First, although we attempted to leverage loss aversion, whether participants in loss-framed groups felt they were truly “losing” something already “owned” by not testing remains unknown. Ongoing qualitative analyses will explore this further. Relatedly, fidelity to the loss-framed intervention was not assessed in all interactions, as research assistants enrolled participants privately in their homes. However, standardized scripts were used and frequent retraining occurred. Second, since HIV status of untested participants is unknown, we are unable to fully evaluate differences in identification of HIV-infected persons by incentive strategy. However, the lack of differences in baseline demographics, socio-economic status, and self-reported HIV risk behavior across groups is reassuring, and suggests HIV prevalence in each group was similar. Also, as newly diagnosed HIV was based on self-report, we may have over-estimated new diagnoses identified at the campaign. Third, by design, the study did not include a control arm that offered no incentives for testing, as we believe there is ample evidence that standard forms of incentives can increase HIV testing uptake.[29, 30] Instead, we sought to address the more novel question of how to optimize incentive interventions. Based on the far lower testing uptake by men in a community-based testing campaign that we previously conducted without incentives in neighboring communities (52% of adult men tested)[20], we anticipate testing uptake among men would have been substantially lower without incentives in our study community. Fourth, our trial may have been underpowered to detect small but significant differences in HIV testing uptake across the study arms. Although we aimed to enroll 3,000 men, fewer than 3,000 adult male residents of the study community met inclusion criteria. Finally, the feasibility of implementing these novel incentive strategies on a larger scale remains untested and is a promising area for policy innovation.
In summary, in this large trial comparing the novel approaches of lottery-based and loss-framed incentives to gain-framed incentives, low-cost lottery-based incentives were significantly more effective in increasing HIV testing uptake among men than gain-framed incentives of comparable cost. Offering lottery-based rewards that have a low per-person cost is a promising way for programs to achieve high HIV testing coverage among men. Such forms of incentives warrant further consideration by donors, governments, and programs that seek to address demand-side barriers to utilization of various other types of health services as well.
Supplementary Material
Acknowledgements
We thank the residents of the study communities for their generous participation in our study. We gratefully acknowledge the contributions of Jane Kabami, Edith Biira, Medius Teriyeitu and Hellen Nakato from the Infectious Diseases Research Collaboration in Mbarara, Uganda. This work was supported by a grant (R01MH105254) from the National Institute of Mental Health (NIMH) at the National Institutes of Health.
Conflicts of Interest and Source of Funding:
All authors report grants from National Institutes of Health (NIH) during the conduct of the study. GC, DK, DH, JK, MK and HT report grants from NIH outside the submitted work. None of the authors have been paid by a pharmaceutical company or other agency to write this manuscript. None of the authors have any other conflicts of interest.
Footnotes
Contributors: GC and HT contributed to the study design, data analysis and interpretation, literature search, tables, figures, and writing of the manuscript. GC had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. ES, AN, and DE contributed to trial implementation, data analysis and interpretation, tables, figures, and writing of the manuscript. DK, DH, JK and MK contributed to the study design, data interpretation, and writing of the manuscript. CC contributed to the data interpretation of the manuscript.
References
- 1.90-90-90 An ambitious treatment target to help end the AIDS epidemic. UNAIDS; In; 2014. [Google Scholar]
- 2.UNAIDS. Prevention Gap Report In. New York: UNAIDS; 2016. [Google Scholar]
- 3.Braitstein P, Boulle A, Nash D, Brinkhof MW, Dabis F, Laurent C, et al. Gender and the use of antiretroviral treatment in resource-constrained settings: findings from a multicenter collaboration. J Womens Health (Larchmt) 2008; 17(1):47–55. [DOI] [PubMed] [Google Scholar]
- 4.Muula AS, Ngulube TJ, Siziya S, Makupe CM, Umar E, Prozesky HW, et al. Gender distribution of adult patients on highly active antiretroviral therapy (HAART) in Southern Africa: a systematic review. BMC public health 2007; 7:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cornell M, Schomaker M, Garone DB, Giddy J, Hoffmann CJ, Lessells R, et al. Gender differences in survival among adult patients starting antiretroviral therapy in South Africa: a multicentre cohort study. PLoS medicine 2012; 9(9):e1001304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Volpp KG, Troxel AB, Pauly MV, Glick HA, Puig A, Asch DA, et al. A randomized, controlled trial of financial incentives for smoking cessation. The New England journal of medicine 2009; 360(7):699–709. [DOI] [PubMed] [Google Scholar]
- 7.Lagarde M, Haines A, Palmer N. Conditional cash transfers for improving uptake of health interventions in low- and middle-income countries: a systematic review. JAMA : the journal of the American Medical Association 2007; 298(16):1900–1910. [DOI] [PubMed] [Google Scholar]
- 8.Banerjee AV, Duflo E, Glennerster R, Kothari D. Improving immunisation coverage in rural India: clustered randomised controlled evaluation of immunisation campaigns with and without incentives. BMJ 2010; 340:c2220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thornton R The Demand for, and Impact of, Learning HIV Status. American Economic Review 2008; 98(5):1829–1863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yotebieng M, Thirumurthy H, Moracco KE, Kawende B, Chalachala J, Wenzi L, et al. Conditional cash transfers increase retention in care and uptake of PMTCT services: A randomized controlled trial. The Lancet HIV 2016; 3(2):e85–e93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thirumurthy H, Masters SH, Rao S, Bronson M, Lanham M, Omanga E, et al. Effect of Providing Conditional Economic Compensation on Uptake of Voluntary Medical Male Circumcision in Kenya. JAMA : the journal of the American Medical Association 2014; 312(7):703–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kahneman D, Tversky A. Prospect theory: an analysis of decision under risk. Econometrica 1979; 47(2):263–291. [Google Scholar]
- 13.Halpern SD, French B, Small DS, Saulsgiver K, Harhay MO, Audrain-McGovern J, et al. Randomized trial of four financial-incentive programs for smoking cessation. The New England journal of medicine 2015; 372(22):2108–2117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Volpp KG, John LK, Troxel AB, Norton L, Fassbender J, Loewenstein G. Financial incentive-based approaches for weight loss: a randomized trial. JAMA 2008; 300(22):2631–2637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Patel MS, Asch DA, Rosin R, Small DS, Bellamy SL, Heuer J, et al. Framing Financial Incentives to Increase Physical Activity Among Overweight and Obese Adults: A Randomized, Controlled Trial. Annals of internal medicine 2016; 164(6):385–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chamie G, Clark TD, Kabami J, Kadede K, Ssemmondo E, Steinfeld R, et al. A hybrid mobile approach for population-wide HIV testing in rural east Africa: an observational study. Lancet HIV 2016; 3(3):e111–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lugada E, Millar D, Haskew J, Grabowsky M, Garg N, Vestergaard M, et al. Rapid Implementation of an Integrated Large-Scale HIV Counseling and Testing, Malaria, and Diarrhea Prevention Campaign in Rural Kenya. PLoS ONE 2010; 5(8):e12435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Uganda. Ministry of Health. 2005. Uganda national policy guidelines for HIV voluntary counselling and testing. Kampala: Ministry of Health. In. [Google Scholar]
- 19.Chamie G, Clark TD, Kabami J, Kadede K, Ssemmondo E, Steinfeld R, et al. A hybrid mobile approach for population-wide HIV testing in rural east Africa: an observational study. Lancet HIV 2016; 3(3):e111–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chamie G, Kwarisiima D, Clark TD, Kabami J, Jain V, Geng E, et al. Leveraging rapid community-based HIV testing campaigns for non-communicable diseases in rural Uganda. PLoS One 2012; 7(8):e43400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Performance-Based Incentives Primer for USAID Missions In: US Agency for International Development (USAID). Washington D.C. Available at: http://pdf.usaid.gov/pdf_docs/Pnadx747.pdf. Last accessed on May 1, 2017; 2010. [Google Scholar]
- 22.Kranzer K, Simms V, Bandason T, Dauya E, McHugh G, Munyati S, et al. Economic incentives for HIV testing by adolescents in Zimbabwe: a randomised controlled trial. Lancet HIV 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Niza C, Rudisill C, Dolan P. Vouchers versus lotteries: what works best in promoting Chlamydia screening? A cluster randomized controlled trial. Applied Economic Perspectives and Policy 2014; 36(1):109–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nyqvist M, Corno L, de Walque D, Svensson J. Using Lotteries to Incentivize Safer Sexual Behavior: Evidence from a Randomized Controlled Trial on HIV Prevention. Policy Research Working Paper of Human Development and Public Services Team, Development Research Group, World Bank 2015; (7215). [Google Scholar]
- 25.Thirumurthy H, Masters SH, Rao S, Murray K, Prasad R, Zivin JG, et al. The Effects of Providing Fixed Compensation and Lottery-Based Rewards on Uptake of Medical Male Circumcision in Kenya: A Randomized Trial. Journal of acquired immune deficiency syndromes (1999) 2016; 72 Suppl 4:S299–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weber BJ, Chapman GB. Playing for peanuts: why is risk seeking more common for low-stakes gambles? . Organ Behav Hum Decis Process 2005; 91:31–46. [Google Scholar]
- 27.Sharma M, Ying R, Tarr G, Barnabas R. Systematic review and meta-analysis of community and facility-based HIV testing to address linkage to care gaps in sub-Saharan Africa. Nature 2015; 528(7580):S77–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Suthar AB, Ford N, Bachanas PJ, Wong VJ, Rajan JS, Saltzman AK, et al. Towards universal voluntary HIV testing and counselling: a systematic review and meta-analysis of community-based approaches. PLoS medicine 2013; 10(8):e1001496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee R, Cui RR, Muessig KE, Thirumurthy H, Tucker JD. Incentivizing HIV/STI testing: a systematic review of the literature. AIDS Behav 2014; 18(5):905–912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McGovern ME, Herbst K, Tanser F, Mutevedzi T, Canning D, Gareta D, et al. Do gifts increase consent to home-based HIV testing? A difference-in-differences study in rural KwaZulu-Natal, South Africa. International journal of epidemiology 2016; 45(6):2100–2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


