Abstract
Rationale:
Inflammatory myofibroblastic tumor (IMT) is uncommon, coexistence of IMTs in the kidney and abdominal wall are more uncommon.
Patient concerns and diagnosis:
We report a 74-year-old female who presented with 6 months history of left flank pain and approximately 5 kg weight loss that were diagnosed as renal cell carcinoma and locally metastatic abdominal wall tumor.
Interventions and outcomes:
A left radical nephrectomy and excision of the abdominal wall tumor were done. The pathologic result was IMTs. After follow-up for 66 months, the patient showed no signs of tumor recurrence.
Lessons:
Coexistence of IMTs in the kidney and abdominal wall is extremely rare and is often diagnosed as malignancy. Therefore, IMTs should be considered in the diagnosis of the patient with both kidney and abdominal wall tumors.
Keywords: abdominal wall, immunohistochemistry, inflammatory myofibroblastic tumor, kidney
1. Introduction
Inflammatory myofibroblastic tumor (IMT) is a rare pathologic entity that was originally described in the lung. Extrapulmonary IMTs, including the gastrointestinal tract, urinary tract, mesentery, paratesticular tissue, etc, have also been reported.[1] In the urinary tract, it occurs most often in the bladder while rarely in the kidney.[2,3] Similarly, only 3 cases of IMTs that originate from the abdominal wall have been reported.[4–6] As far as we know, there is no report about IMTs of the kidney combined with abdominal wall in the literature previously.
Herein, we report an IMT in a 74-year-old female that was misdiagnosed as renal cell carcinoma and locally metastatic abdominal wall tumor.
2. Case presentation
In October 2012, a 74-year-old female presented with 6 months history of left flank pain and approximately 5 kg weight loss. She underwent cholecystectomy 23 years ago because of the gall bladder stone. Physical examination demonstrated slight left renal percussive pain. Basic laboratory examination was nonspecific. Ultrasonography (US) revealed a 7 cm × 8 cm slight hyperechoic mass at the upper pole of the left kidney and severe hydronephrosis, but negligence of the left abdominal wall mass due to the interference of the twelfth rib and the gas in the intestinal cavity. Computed tomography (CT) revealed a 7 cm × 8 cm heterogeneous mass attached to the spleen and pancreas and located at the upper pole of the left kidney including a 3 cm × 4 cm left abdominal wall mass. A contrast-enhanced CT scan was done (Fig. 1). The masses were significantly enhanced, indicating of malignancy. And renal cell carcinoma and locally metastatic abdominal wall tumor were diagnosed. Therefore, a left radical nephrectomy and excision of the abdominal wall tumor were planned. The upper pole of the kidney tumor is slightly harder, about 7 cm × 8 cm in size, and closely adheres to the tail of the pancreas. Considering that it is a malignant tumor, it is difficult to remove the pancreatic tail and preserve the spleen. Therefore, the combined pancreatic tail and spleen were removed. After the exploration of the abdominal wall, a solid red mass of approximately 3 cm × 4 cm was probed on the dorsal abdominal wall of the twelfth rib. The texture was slightly stiff and adhered tightly to the abdominal wall, and the abdominal wall mass was completely resected by blunt and sharp separation.
Figure 1.
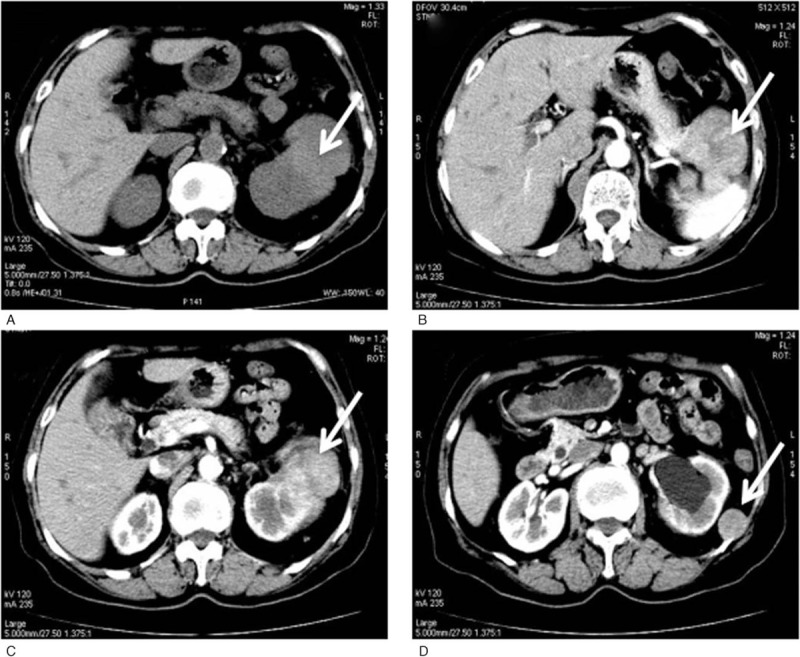
(A) CT showed a mass in the left of the kidney (arrow). (B) Contrast-enhanced CT showed the mass was attached to the spleen and pancreas tightly. (C, D) The masses were significantly enhanced.
Microscopic examination revealed typical spindle cell proliferation with inflammatory cells (Fig. 2). Immunohistochemistry showed S-100 was positive, smooth muscle actin, desmin, and ki-67 (10%) were focally positive, but cytokeratin was negative. Pathological diagnosis of IMTs in the left kidney and abdominal wall was done. The patient recovered well. CT scan at 6, 12, and 36 months showed no evidence of metastatic or recurrent disease (Fig. 3).
Figure 2.

The microscopic examination revealed a proliferation of typical spindle-shaped cells accompanied by inflammatory cells (H&E × 400).
Figure 3.
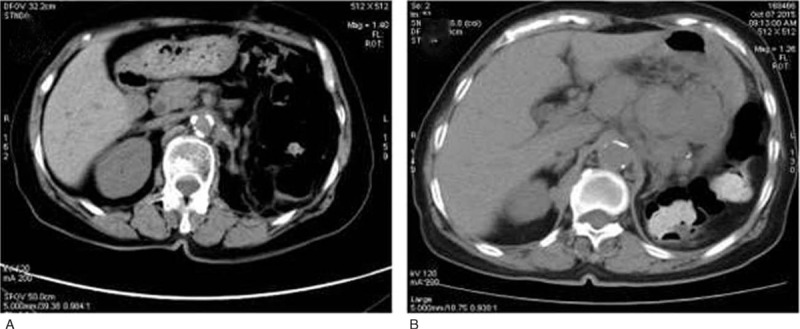
Follow-up for 6 months (A) and 36 months (B), CT imaging showed no evidence of recurrence.
3. Discussion
IMT is a rare entity that tends to aggressive behavior and local recurrence, which shows a preference for visceral soft tissue in children and young people.[7] Histologically, IMT is characterized by proliferation of typical spindle-shaped cells accompanied by inflammatory infiltration of plasma cells, eosinophils, and lymphocytes.[8] The pathogenesis and etiology of IMT are still unknown.[7] In some cases, IMT is thought to be caused by trauma and surgery-related infections, or related to other malignancies.[9,10] Some have described it to be related with chronic hepatitis B infection,[11] while others have been found it to be related with Epstein–Barr (EB) virus.[12] In our case, the patient is a nurse, nonsmoker, with no history of trauma and chronic hepatitis B infection. After the pathological report, we tested the patient's blood for EB virus and the test result was negative. According to the above results, we considered that no special history was related to the development of IMT in our case.
Generally, the symptoms depend on the size and location of the tumor. Some patients are with systemic symptoms such as fatigue, fever, or weight loss, while in the urinary tract, hematuria, flank pain, and dysuria are more common. The clinical symptoms of abdominal IMT include abdominal mass, abdominal discomfort, weight loss, and fever.[1,6] In our case, the patient had left flank pain and approximately 5 kg weight loss, which provided the clue for the further examination.
There is almost no obvious abnormality in laboratory tests.[13] US, CT, and magnetic resonance imaging may allow early diagnosis. However, the diagnosis of IMT is often delayed for its nonspecific and different clinical presentations. In our case, US and CT revealed a mass in the left kidney and a left abdominal wall mass. The tumors were significantly enhanced, which typically indicative of malignant lesions.
Surgery with radical excision is still considered to be the best treatment, although steroid therapy has been reported to regress IMT.[14] In the present case, the preoperative diagnosis was renal cell carcinoma and locally metastatic abdominal wall tumor. Because the mass was large and attached to the spleen and pancreas tightly, a left radical nephrectomy and excision of the abdominal wall tumor combined with splenectomy and the tail of pancreas resection were carried out. However, histopathological diagnosis was IMTs. After a follow-up for 66 months, the patient does not have recurrence.
As reported, the overall recurrence rate of IMT is from 2% to 60%, and the metastatic rate is no more than 5%.[15,16] However, there was no identified potential for recurrence or metastases in the renal IMTs according to the case report.[17] IMT can happen in any location, especially in abdominopelvic region, retroperitoneum, and lung.[7] In the current case, the presence of IMTs in kidney and abdominal wall may indicate a simple incidental coexistence or 1 tumor is metastases from another. To date, only IMTs of the kidney and bilateral lung nodules in a child were reported.[18] We do not know whether the abdominal wall of IMT is metastases or synchronized lesions. We consider that the occurrence of the tumors in 2 locations may be 1 tumor is metastases from another or a simple incidental coexistence. The relationship between the tumors needs further investigation in our case.
4. Conclusion
Coexistence of IMTs in the kidney and abdominal wall is extremely rare, which is easily diagnosed as renal cell carcinoma and locally metastatic abdominal wall tumor. Here, we first report a case of IMTs in the kidney and abdominal wall in the literature. We suggest that the presence of IMTs in the kidney and abdominal wall should be considered in the diagnosis of renal cell carcinoma and locally metastatic abdominal wall tumor.
Acknowledgment
We thank Gang Yuan for providing imaging support.
Author contributions
Conceptualization: Xiaokang Qi.
Data curation: Xiaokang Qi, Kunpeng Wang.
Investigation: Xiaokang Qi.
Resources: Peng Xue, Chunfang Zhang.
Software: Chengkuan Cai.
Supervision: Peng Xue, Chuanquan Tu, Kunpeng Wang.
Validation: Chunfang Zhang, Chengkuan Cai.
Writing – original draft: Yiqiu Wang.
Writing – review & editing: Yiqiu Wang, Kunpeng Wang.
Footnotes
Abbreviations: CT = computed tomography, IMT = inflammatory myofibroblastic tumor, US = ultrasonography.
YW and XQI contributed equally to this work.
Ethics approval and consent was obtained from ethics committee of the First People's Hospital of Lianyungang.
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
The authors declare that they have no competing interests.
References
- [1].Coffin CM, Watterson J, Priest JR, et al. Extrapulmonary inflammatory myofibroblastic tumor (inflammatory pseudotumor). A clinicopathologic and immunohistochemical study of 84 cases. Am J Surg Pathol 1995;19:859–72. [DOI] [PubMed] [Google Scholar]
- [2].Kovach SJ, Fischer AC, Katzman PJ, et al. Inflammatory myofibroblastic tumors. J Surg Oncol 2006;94:385–91. [DOI] [PubMed] [Google Scholar]
- [3].Larbcharoensub N, Chobpradit N, Kijvikai K, et al. Primary renal inflammatory myofibroblastic tumor. Urol Int 2006;76:94–6. [DOI] [PubMed] [Google Scholar]
- [4].Hernández LA, León TAM, Jones JM, et al. [Inflammatory myofibroblastic tumour of the abdominal wall in an adult patient]. Cir Esp 2012;90:e22. [DOI] [PubMed] [Google Scholar]
- [5].Pratap A, Tiwari A, Agarwal B, et al. Inflammatory myofibroblastic tumor of the abdominal wall simulating rhabdomyosarcoma: report of a case. Surg Today 2007;37:352–5. [DOI] [PubMed] [Google Scholar]
- [6].Yagci MA, Sezer A, Yeldan E, et al. Inflammatory myofibroblastic tumor presenting as an abdominal wall mass in an adult patient. J Cancer Res Ther 2010;6:224–6. [DOI] [PubMed] [Google Scholar]
- [7].Gleason BC, Hornick JL. Inflammatory myofibroblastic tumours: where are we now. J Clin Pathol 2008;61:428–37. [DOI] [PubMed] [Google Scholar]
- [8].Karnak I, Senocak ME, Ciftci AO, et al. Inflammatory myofibroblastic tumor in children: diagnosis and treatment. J Pediatr Surg 2001;36:908–12. [DOI] [PubMed] [Google Scholar]
- [9].Maves CK, Johnson JF, Bove K, et al. Gastric inflammatory pseudotumor in children. Radiology 1989;173:381–3. [DOI] [PubMed] [Google Scholar]
- [10].Sanders BM, West KW, Gingalewski C, et al. Inflammatory pseudotumor of the alimentary tract: clinical and surgical experience. J Pediatr Surg 2001;36:169–73. [DOI] [PubMed] [Google Scholar]
- [11].Akatsu T, Wakabayashi G, Tanimoto A, et al. Inflammatory pseudotumor of the liver masquerading as hepatocellular carcinoma after a hepatitis B virus infection: report of a case. Surg Today 2006;36:1028–31. [DOI] [PubMed] [Google Scholar]
- [12].You Y, Shao H, Bui K, et al. Epstein-Barr virus positive inflammatory pseudotumor of the liver: report of a challenging case and review of the literature. Ann Clin Lab Sci 2014;44:489–98. [PubMed] [Google Scholar]
- [13].Tarhan F, Gül AE, Karadayi N, et al. Inflammatory pseudotumor of the kidney: a case report. Int Urol Nephrol 2004;36:137–40. [DOI] [PubMed] [Google Scholar]
- [14].Li JY, Yong TY, Coleman M, et al. Bilateral renal inflammatory pseudotumour effectively treated with corticosteroid. Clin Exp Nephrol 2010;14:190–8. [DOI] [PubMed] [Google Scholar]
- [15].Pettinato G, Manivel JC, De Rosa N, et al. Inflammatory myofibroblastic tumor (plasma cell granuloma). Clinicopathologic study of 20 cases with immunohistochemical and ultrastructural observations. Am J Clin Pathol 1990;94:538–46. [DOI] [PubMed] [Google Scholar]
- [16].Patankar T, Prasad S, Shenoy A, et al. Pulmonary inflammatory pseudotumour in children. Australas Radiol 2000;44:318–20. [DOI] [PubMed] [Google Scholar]
- [17].Kapusta LR, Weiss MA, Ramsay J, et al. Inflammatory myofibroblastic tumors of the kidney: a clinicopathologic and immunohistochemical study of 12 cases. Am J Surg Pathol 2003;27:658–66. [DOI] [PubMed] [Google Scholar]
- [18].Dogan MS, Doganay S, Koc G, et al. Inflammatory myofibroblastic tumor of the kidney and bilateral lung nodules in a child mimicking Wilms tumor with lung metastases. J Pediatr Hematol Oncol 2015;37:e390–3. [DOI] [PubMed] [Google Scholar]


