Abstract
The objective of this study was to evaluate the association between serum vitamin D deficiency and age-related macular degeneration (AMD) in Koreans through a clinical case–control pilot study. The study included 96 patients: 30 with late AMD, 32 with early AMD, and 34 normal controls. The patients with late AMD were divided into 2 subgroups based on the presence or absence of subretinal fibrosis on optical coherence tomography (OCT) images. We measured 25-hydroxyvitamin D levels in the serum of all patients during the same season to rule out seasonal variation of serum vitamin D level. Serum vitamin D deficiency was defined as a serum 25-hydroxyvitamin D level below 20 ng/mL. Serum vitamin D deficiency had a tendency to increase the risk of early AMD, although with borderline significance [odds ratio (OR) = 3.59; 95% confidence interval (95% CI) 0.95–13.58; P = .060]. It was significantly associated with a greater risk of late AMD (OR = 3.61; 95%CI 1.04–12.51; P = .043). Among the 2 subgroups of patients with late AMD, those with subretinal fibrosis present on the OCT images showed a greater risk of serum vitamin D deficiency than the normal controls (OR = 7.54; 95% CI 1.34–42.51). However, there was no significant association between serum vitamin D deficiency and late AMD without subretinal fibrosis (OR = 1.89; 95% CI 0.40–8.92). Serum vitamin D deficiency may increase the risk of early and late AMD in Koreans, and may also be associated with subretinal fibrosis in this population.
Keywords: 25-hydroxyvitamin D, age-related macular degeneration, serum vitamin D deficiency, subretinal fibrosis
1. Introduction
Age-related macular degeneration (AMD) is one of the main causes of blindness in individuals over 60 years of age in developed countries.[1] The prevalence of AMD has gradually increased in Koreans.[2]
The exact cause of AMD is currently unknown, but it is known to be a multifactorial disease that is influenced by both genetic and environmental factors.[3] Specifically, age, smoking history, and family history of AMD are causative factors for AMD.[4] Other potential risk factors include exposure of the eye to sunlight, cardiovascular disease, dietary fat intake, and dietary antioxidant intake.[5]
Clinically, AMD is characterized by drusen formation, as well as by changes in retinal pigment epithelial cells, both of which are visible on fundus examination. Furthermore, AMD can be subdivided into wet and dry forms, depending on the presence of choroidal neovascularization (CNV).
Vitamin D is a circulating steroid hormone that counteracts inflammation,[6] angiogenesis,[7] and fibrosis.[8] Recently, inflammation has been found to play a role in the pathogenesis of AMD.[9] Therefore, inflammation, angiogenesis, and fibrosis—the 3 processes that are ameliorated by vitamin D—are all involved in AMD pathogenesis and disease progression. Indeed, several studies have shown a direct association between serum vitamin D level and AMD.[10–14]
When compared with other races, Koreans have differences in serum vitamin D levels and the progression type of AMD. Serum vitamin D levels are lower in Koreans than in other races.[10] Moreover, old age has generally been suggested as a risk factor for vitamin D deficiency because the cutaneous synthesis of vitamin D declines with age.[15–17] However, according to the Korea National Health and Nutrition Examination Survey (KNHANES) in 2008, serum vitamin D concentration gradually increases from the age of 20 to 70 years in Koreans.[18] Furthermore, in Koreans, exudative forms of AMD are more prevalent than atrophic forms, such as progressive AMD, when compared with other races.[2] In advanced AMD, subretinal fibrosis occurs, and this is associated with irreversible damage to the retinal architecture, as well as severe vision loss. In some patients, dry AMD progresses to wet AMD, and some cases of wet AMD progress to fibrotic forms. As mentioned above, vitamin D counteracts fibrosis.
A study has been performed on the correlation between serum vitamin D level and AMD in Koreans by using the data from the KNHANES.[10] However, in this study, the patients were categorized on the basis of fundus photographs only, as they are the only available retinal imaging examination results in the KNHANES data. Therefore, we conducted a clinical case–control pilot study to evaluate the association between serum vitamin D deficiency and AMD. Furthermore, we investigated the correlation between subretinal fibrosis and serum vitamin D deficiency in Koreans.
2. Methods
2.1. Participants
This study included patients who had visited Kangdong Sacred Heart hospital, Seoul, Korea, due to a decrease in visual acuity from May 2014 to June 2014 and during June 2018. All patients were older than 50 years and had not been diagnosed as having a cardiovascular disease (this included hypertension and diabetes mellitus). We categorized the participants into 3 groups as follows: the late AMD group, early AMD group, and those without any macular degeneration (normal control group). Initially, 143 patients were enrolled (56 cases without any macular degeneration, 49 with early AMD, and 38 with late AMD). Among them, we excluded patients with any other diseases that involved systemic inflammation, as well as those with autoimmune diseases, vitamin D absorption problems, chronic renal failure, liver disease, or parathyroid disease based on the medical records in our hospital. In addition, we excluded patients with C-reactive protein (CRP) levels above 1 mg/dL and those who were taking vitamin D supplements. Of the 56 patients without any macular degeneration, 22 were excluded. These exclusions were due to the presence of other diseases that could affect serum vitamin D level (n = 9), the use of vitamin D supplements (n = 10), or high CRP levels (n = 3). Of the 49 patients in the early AMD group, 17 were excluded. This was due to the presence of other diseases that could affect serum vitamin D level (n = 4), the use of vitamin D supplements (n = 7), or high CRP levels (n = 6), leaving 32 patients who were included in the study. Of the 38 patients with late AMD, 8 were excluded. This was due to the presence of other diseases that could affect the serum vitamin D level (n = 2), the use of vitamin D supplements (n = 3), or high CRP levels (n = 3). Finally, a total of 96 participants (normal control group: n = 34, early AMD group: n = 32, late AMD group: n = 30) were eligible for inclusion in this study. The study protocol was reviewed and approved by the institutional review board of the Kangdong Sacred Heart hospital (IRB No. 2015–03–002). Informed consent was confirmed by the IRB. Informed consent was obtained from all individual participants included in the study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
2.2. Diagnosis of early and late AMD
Patients with decreased visual acuity due to cataract without any macular degeneration were included in the normal control group.
Patients were included in the early AMD group only if they belonged to stage 1 to 3 of the Clinical Age related Maculopathy Staging (CARMS) system[19] — CARMS 1: no drusen or < 10 small drusen without pigment abnormalities; CARMS 2: ≥ 10 small drusen or < 15 medium drusen, accompanied by pigment abnormalities associated with AMD; CARMS 3: ≥ 15 medium drusen or any large drusen, with or without retinal pigment epithelial detachment.
Late AMD was identified when CNV and drusen were visible on fluorescence angiography (Topcon TRC-50DX; Paramus, NJ), with retinal pigment epithelium abnormality on fundus photography. Patients with late AMD were subdivided into 2 groups by the presence of subretinal fibrosis on the optical coherence tomography (OCT; Spectralis, Heidelberg, Germany) images correlated with the findings on fundus photographs (whitish, fibrous lesion beneath the retina). The subretinal fibrosis present on the OCT was defined as a hyperreflective area located between the sensory retina and retinal pigment epithelium. One group did not show subretinal fibrosis on the OCT (Subgroup1); the other group showed subretinal fibrosis on the OCT (Subgroup2). The retinal diagnosis was made by 2 trained ophthalmologists.
2.3. Data collection and measurements
We measured 25-hydroxyvitamin D (vitamin D) in the serum of all patients during the same season, to correct for the seasonal variation of serum vitamin D levels. 25-hydoxyvitamin D was measured using the ADIVA Centaur XP immunoassay system (Siemens Healthcare Diagnostics, Erlangen, Germany). Venous blood samples were obtained in an evacuated container. Serum specimens were immediately frozen at −80°C. Estimations of serum 25-hydroxyvitamin D level were performed within 2 weeks of collection. All serum analyses were performed properly and promptly.
All patients also completed a questionnaire, which asked them about their smoking status, duration of exposure to sunlight, and the use of sunglasses while out of doors. This was done to exclude other factors that might have affected serum 25-hydroxyvitamin D levels. We analyzed the duration of exposure to the sunlight in patients who were exposed for ≤ 5 hours daily—considering the latitude of South Korea, as well as the skin type of the Korean people, this is thought to be the cut-off point for the correlation between sunlight exposure and vitamin D synthesis.[20] Vitamin D deficiency was defined as serum 25-hydroxyvitamin D level below 20 ng/mL.[21] Followed by the results of the KNHANES, prevalence of early and late AMD is increased in Korean people who are aged 65 years and over.[22] Hence, we divided the patients according to whether they were younger or older than 65 years.
2.4. Statistical analysis
Statistical analyses were performed using SPSS software, version 20.0 for Windows (IBM Corp, Armonk, NY). We estimated the odds ratios (ORs) and 95% confidence intervals (95% CIs) in order to evaluate the association between serum vitamin D deficiency and AMD. Moreover, to rule out other confounding factors that could have interfered with the association between AMD and serum vitamin D deficiency, we used multiple logistic regression analysis. Statistical significance was defined as a P < .05.
3. Results
A total of 96 patients were enrolled in our study (normal control group: n = 34, early AMD group: n = 32, late AMD group: n = 30). Among the patients with late AMD, 15 patients were included in subgroup 1 and 15 in subgroup 2.
Statistically significant differences were observed among the 3 groups (normal control group, early AMD group, and late AMD group) in terms of the ratio of males to females (P = .020), age (P < .001), duration of exposure to sunlight (P = .002), and 25-hydroxyvitamin D levels (P < .001; Table 1; P values calculated using the Chi-square test and the Kruskal–Wallis test). We analyzed the data using multiple logistic regression to rule out the effects of other confounding factors that may have interfered with the association between AMD and serum vitamin D deficiency. After the multiple logistic regression analysis between the normal control group and each AMD group, serum vitamin D deficiency had a tendency to increase the risk of early AMD, although with borderline significance (OR = 3.59; 95% CI 0.95–13.58; P = .060; Table 2). Serum vitamin D deficiency was also significantly associated with a greater risk of late AMD (OR = 3.61; 95% CI 1.04–12.51; P = .043; Table 3).
Table 1.
Demographics of the study participants.
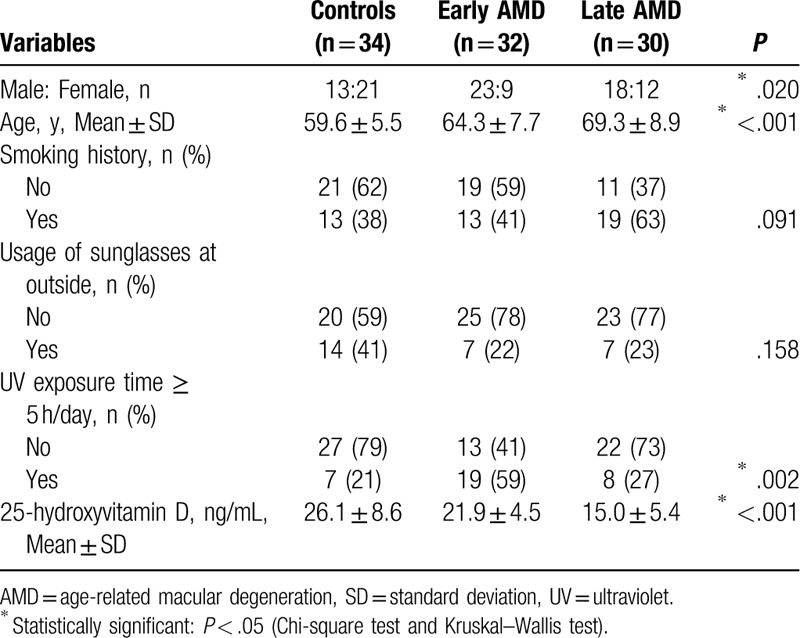
Table 2.
Multiple logistic regression analysis between the control group and early age-related macular degeneration group.
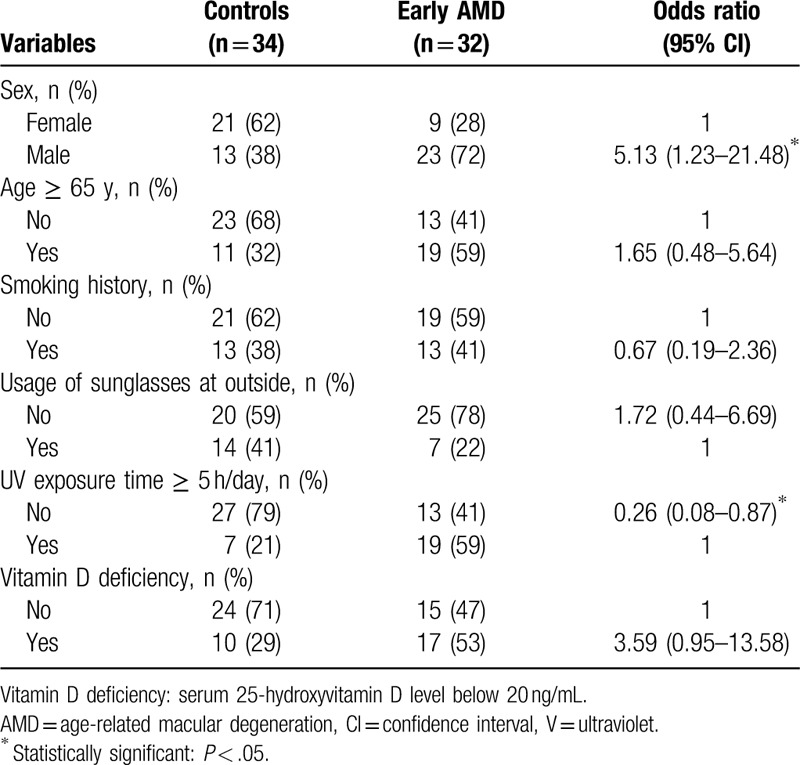
Table 3.
Multiple logistic regression analysis between the control group and late age-related macular degeneration group (Subgroups 1 and 2).
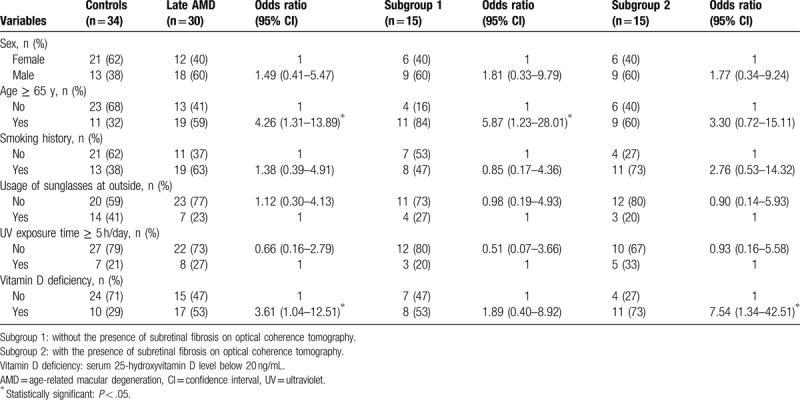
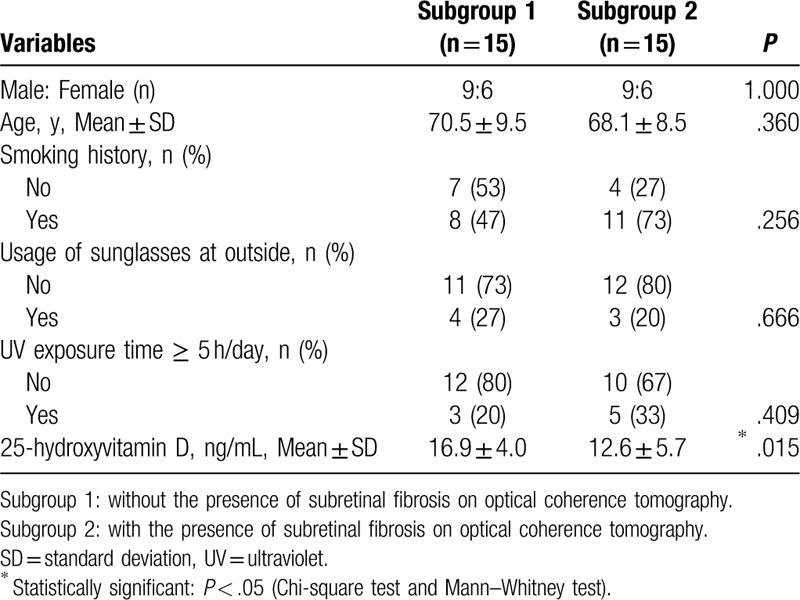
With specific regard to the patients with late AMD, statistically significant differences were observed between Subgroups 1 and 2 in terms of 25-hydroxyvitamin D levels (P = .015; Table 4; P values calculated by the Chi-square test and the Mann–Whitney test). As before, we analyzed the data using multiple logistic regression analysis to rule out the effects of other confounding factors that may have interfered with the association between AMD and serum vitamin D deficiency. In the multiple logistic regression analysis, patients with late AMD who showed subretinal fibrosis on the OCT had a significantly greater risk for serum vitamin D deficiency than the normal control group (OR = 7.54; 95% CI 1.34–42.51; Table 3). However, there was no significant association between serum vitamin D deficiency and late AMD without subretinal fibrosis (OR = 1.89; 95% CI 0.40–8.92; Table 3).
Table 4.
Demographics of the subgroups with late age-related macular degeneration.
4. Discussion
Our study has some differences in terms of the study design and the results obtained, when compared with previous studies that described the correlation between serum vitamin D level and AMD in Koreans and in other races.[10–14]
Previous studies categorized patients on the basis of funduscopic photographs.[10–14] However, in our study, we distinguished patients who visited our hospital using fundus photography, fluorescence angiography, and OCT. Hence, we could categorize the patients more specifically; for example, patients with late AMD were divided into 2 subgroups depending on the presence of subretinal fibrosis on the OCT images.
In our study, statistically significant differences were observed between the controls and late AMD patients with subretinal fibrosis on the OCT, in terms of the number of patients with serum vitamin D deficiency. However, there were no statistically significant differences between the controls and the late AMD patients without subretinal fibrosis on OCT, in terms of the number of patients with serum vitamin D deficiency. Singh et al[23] reported that alterations in the complement system are associated with subretinal fibrosis. Oxidative stress, which is induced by the aging process, as well as by environmental factors, may damage retinal cells, causing inflammation, increased levels of extracellular matrix degrading proteins, and release of growth factors that are thought to be associated with fibrosis.[24] Vitamin D counteracts these changes. Therefore, serum vitamin D deficiency may be associated with subretinal fibrosis in Koreans.
In our study, serum vitamin D deficiency had a tendency to increase the risk of early AMD, although with borderline significance, even though the number of patients who were exposed to sunlight for more than 5 hours was significantly greater in the early AMD group than the controls and the late AMD group. This is one of the major differences between our results and those of previous studies on the correlation between serum vitamin D level and AMD.[10–14] A previous study in Koreans reported that the prevalence of early AMD increased with higher 25-hydroxyvitamin D levels.[10] It suggested that early AMD may be influenced by the adverse effects of ultraviolet (UV) sunlight exposure rather than vitamin D, a byproduct of sun exposure. However, many inflammatory cells have a receptor for vitamin D,[25] and inflammatory bowel disease is associated with low plasma vitamin D levels.[26] Furthermore, multiple sclerosis has been associated with elevated plasma vitamin D levels.[27] Finally, inflammation is induced by cytokines and immunoglobulins that are secreted from T-cells and B-cells; such inflammation is suppressed by vitamin D.[28] In previous studies regarding inflammation and AMD pathogenesis, immunologic components have been found within drusen, including immunoglobulins, complement factors, and fibrinogen.[29] In 1 study, treatment of aged mice using vitamin D reduced inflammation and amyloid beta deposition in the retina.[30] Therefore, on the basis of these findings and the results of our study, serum vitamin D deficiency may be associated with early AMD in Koreans.
As we mentioned before, exudative forms of AMD, such as progressive type of AMD, are more prevalent among Koreans than the atrophic forms.[2] The exact cause of this is not yet known. It may be attributed to the differences in genetic and environmental factors between Koreans and people of other races. In a study that investigated the genetic factors associated with exudative AMD in Koreans, no significant differences were found compared with other races.[31] Serum vitamin D levels are lower in Koreans than in people of other races.[10] In our study, serum vitamin D deficiency was more strongly associated with late AMD than with early AMD. Vitamin D inhibits angiogenesis by reducing the expression of vascular endothelial growth factor, as well as by inhibiting matrix metallopeptidase 9, which is thought to play a role in CNV.[32] Therefore, the lower serum vitamin D level in Koreans than in other races may be one of the environmental factors responsible for the higher prevalence of exudative forms of AMD among Koreans.
According to the KNHANES in 2008, the Korean population has a higher serum vitamin D concentration in the age group of late AMD cases than in the age group of controls.[18] Considering this fact, the results of our study, which showed that there are more patients with serum vitamin D deficiency in the late AMD group than the control group, are meaningful.
Nonetheless, our study had some limitations. First, we used a small number of patients to confirm our hypothesis; however, our study did yield statistically significant data despite the small number of patients. As a number of patients were excluded from the study during the selection procedure, the study sample cannot be considered representative of the general Korean population. Second, there were differences between the different groups in our study in terms of the ratio of male to female participants, as well as the age distribution. Despite this, our study revealed a significant inverse association between serum vitamin D deficiency and AMD by using multiple logistic regression analysis. Third, we did not consider the dietary vitamin D intake of the participants. Our body obtains vitamin D in 2 main ways—absorption of UV radiation by the skin and absorption from foods. However, less vitamin D is obtained from food than from exposure to UV radiation. Fourth, in our study, when compared with other groups, the early AMD group had a greater number of patients with UV exposure time greater than 5 hours per day. However, the number of patients with serum vitamin D deficiency were greater in the early AMD group than in the normal control group, although the difference was only borderline significant. We should ask additional questions to the patients to confirm whether they were actually exposed to the sunlight during the exposure time to sunlight (e.g., regarding the usage of sunblock cream, wearing long clothing, or carrying a parasol). These factors could be the cause of lower levels of serum vitamin D in the early AMD group than the normal control group, despite there being a greater number of patients with a UV exposure time of more than 5 hours per day in the early AMD group.
In conclusion, serum vitamin D deficiency may increase the risk of early and late AMD in Koreans. It may also be associated with subretinal fibrosis in this population. Additional large population studies are needed to confirm these results as well as to elucidate the underlying mechanisms.
Author contributions
Conceptualization: Sung Pyo Park.
Data curation: Kyoung Lae Kim, Sung Pyo Park.
Formal analysis: Kyoung Lae Kim, Sung Pyo Park.
Funding acquisition: Sung Pyo Park.
Investigation: Kyoung Lae Kim, Sung Pyo Park.
Methodology: Sung Pyo Park.
Project administration: Sung Pyo Park.
Resources: Sung Pyo Park.
Software: Sung Pyo Park.
Supervision: Sung Pyo Park.
Validation: Sung Pyo Park.
Visualization: Kyoung Lae Kim, Sung Pyo Park.
Writing – original draft: Kyoung Lae Kim, Sung Pyo Park.
Writing – review & editing: Sung Pyo Park.
Footnotes
Abbreviations: AMD = age-related macular degeneration, CARMS = Clinical Age Related Maculopathy Staging, CI = confidence interval, CNV = choroidal neovascularization, CRP = C-reactive protein, KNHANES = Korea National Health and Nutrition Examination Survey, OCT = optical coherence tomography, OR = odds ratio, Vitamin D = 25-hydroxyvitamin D.
Funding/support: This study was supported by the Hallym University Research Fund (HURF-2015–46). The funding organization had no role in the design or implementation of this study.
The authors declare that they have no conflict of interest.
References
- [1].Kawasaki R, Yasuda M, Song SJ, et al. The prevalence of age related macular degeneration in Asians: a systematic review and meta-analysis. Ophthalmology 2010;117:921–7. [DOI] [PubMed] [Google Scholar]
- [2].Park SJ, Lee JH, Woo SJ, et al. Age-related macular degeneration: prevalence and risk factors from Korean National Health and Nutrition Examination Survey, 2008 through 2011. Ophthalmology 2014;121:1756–65. [DOI] [PubMed] [Google Scholar]
- [3].Montezuma SR, Sobrin L, Seddon JM. Review of genetics in age related macular degeneration. Semin Ophthalmol 2007;22:229–40. [DOI] [PubMed] [Google Scholar]
- [4].Klein R, Peto T, Bird A, et al. The epidemiology of age-related macular degeneration. Am J Ophthalmol 2004;137:486–95. [DOI] [PubMed] [Google Scholar]
- [5].Fletcher AE, Bentham GC, Agnew M, et al. Sunlight exposure, antioxidants, and age-related macular degeneration. Arch Ophthalmol 2008;126:1396–403. [DOI] [PubMed] [Google Scholar]
- [6].Pittas AG, Harris SS, Stark PC, et al. The effects of calcium and vitamin D supplementation on blood glucose and markers of inflammation in nondiabetic adults. Diabetes Care 2007;30:980–6. [DOI] [PubMed] [Google Scholar]
- [7].Albert DM, Scheef EA, Wang S, et al. Calcitriol is a potent inhibitor of retinal neovascularization. Invest Ophthalmol Vis Sci 2007;48:2327–34. [DOI] [PubMed] [Google Scholar]
- [8].Firrincieli D, Braescu T, Housset C, et al. Illuminating liver fibrosis with vitamin D. Clin Res Hepatol Gastroenterol 2014;38:5–8. [DOI] [PubMed] [Google Scholar]
- [9].Anderson DH, Mullins RF, Hageman GS, et al. A role for local inflammation in the formation of drusen in the aging eye. Am J Ophthalmol 2002;134:411–31. [DOI] [PubMed] [Google Scholar]
- [10].Kim EC, Han K, Jee D. Inverse relationship between high blood 25-hydroxyvitamin D and late stage of age-related macular degeneration in a representative Korean population. Invest Ophthalmol Vis Sci 2014;5:4823–31. [DOI] [PubMed] [Google Scholar]
- [11].Itty S, Day S, Lyles KW, et al. Vitamin D deficiency in neovascular versus non-neovascular age-related macular degeneration. Retina 2014;34:1779–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Singh A, Falk MK, Subhi Y, et al. The association between plasma 25-hydroxyvitamin D and subgroups in age-related macular degeneration: a cross-sectional study. PLoS One 2013;8:e70948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].McKay GJ, Young IS, McGinty A, et al. Associations between serum vitamin D and genetic variants in vitamin D pathways and age-related macular degeneration in the European Eye Study. Ophthalmology 2017;124:90–6. [DOI] [PubMed] [Google Scholar]
- [14].Millen AE, Nie J, Sahli MW, et al. Vitamin D status and prevalent early age-related macular degeneration in African Americans and Caucasians: the Atherosclerosis Risk in Communities (ARIC) Study. J Nutr Health Aging 2017;21:772–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Holick MF. Vitamin D deficiency. N Engl J Med 2007;357:266–81. [DOI] [PubMed] [Google Scholar]
- [16].MacLaughlin J, Holick MF. Aging decreases the capacity of human skin to produce vitamin D3. J Clin Invest 1985;76:1536–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Mithal A, Wahl DA, Bonjour JP, et al. Global vitamin D status and determinants of hypovitaminosis D. Osteoporos Int 2009;20:1807–20. [DOI] [PubMed] [Google Scholar]
- [18].Choi HS, Oh HJ, Choi H, et al. Vitamin D insufficiency in Korea: a greater threat to younger generation: the Korea National Health and Nutrition Examination Survey (KNHANES) 2008. J Clin Endocrinol Metab 2011;96:643–51. [DOI] [PubMed] [Google Scholar]
- [19].Seddon JM, Sharma S, Adelman RA. Evaluation of the clinical age-related maculopathy staging system. Ophthalmology 2006;113:260–6. [DOI] [PubMed] [Google Scholar]
- [20].Matthias W, Michael FH. Sunlight and Vitamin D. Dermatoendocrinology 2013;5:51–108. [Google Scholar]
- [21].Dawson-Hughes B, Heaney RP, Holick MF, et al. Estimates of optimal vitamin D status. Osteoporos Int 2005;16:713–6. [DOI] [PubMed] [Google Scholar]
- [22].Cho BJ, Heo JW, Kim TW, et al. Prevalence and risk factors of age-related macular degeneration in Korea: the Korea National Health and Nutrition Examination Survey 2010-2011. Invest Ophthalmol Vis Sci 2014;24:1101–8. [DOI] [PubMed] [Google Scholar]
- [23].Singh A, Faber C, Falk M, et al. Altered expression of CD46 and CD59 on leukocytes in neovascular age-related macular degeneration. Am J Ophthalmol 2012;154:193–9. [DOI] [PubMed] [Google Scholar]
- [24].Biernacka A, Dobaczewski M, Frangogiannis NG. TGF-beta signaling in fibrosis. Growth Fact 2011;29:196–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Lin AM, Chen KB, Chao PL. Antioxidative effect of vitamin D3 on zinc induced oxidative stress in CNS. Ann NY Acad Sci 2005;1053:319–29. [DOI] [PubMed] [Google Scholar]
- [26].Joseph AJ, George B, Pulimood AB, et al. 25 (OH) vitamin D level in Crohn's disease: association with sun exposure & disease activity. Indian J Med Res 2009;130:133–7. [PubMed] [Google Scholar]
- [27].Munger KL, Levin LI, Hollis BW, et al. Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis. JAMA 2006;296:2832–8. [DOI] [PubMed] [Google Scholar]
- [28].Bikle D. Non-classic actions of vitamin D. J Clin Endocrinol Metab 2009;94:26–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Johnson LV, Ozaki S, Staples MK, et al. A potential role for immune complex pathogenesis in drusen formation. Exp Eye Res 2000;70:441–9. [DOI] [PubMed] [Google Scholar]
- [30].Lee V, Rekhi E, Hoh Kam J, et al. Vitamin D rejuvenates aging eyes by reducing inflammation, clearing amyloid beta and improving visual function. Neurobiol Aging 2012;33:2382–9. [DOI] [PubMed] [Google Scholar]
- [31].Kim NR, Kang JH, Kwon OW, et al. Association between complement factor H gene polymorphisms and neovascular age-related macular degeneration in Koreans. Invest Ophthalmol Vis Sci 2008;49:2071–6. [DOI] [PubMed] [Google Scholar]
- [32].Steen B, Sejersen S, Berglin L, et al. Matrix metalloproteinases and metalloproteinase inhibitors in choroidal neovascular membranes. Invest Ophthalmol Vis Sci 1998;39:2194–200. [PubMed] [Google Scholar]


