Abstract
No official spirometry reference values for Chinese are available.
To establish new Chinese reference values and prediction equations for lung parameters in Chinese individuals of 10 to 81 years of age.
Pulmonary functions were measured according to the American Thoracic Society criteria in 1457 subjects from the Zhejiang coastal province (China). The subjects were 10 to 81 years of age, nonsmokers, and without chronic or acute diseases. Multiple stepwise linear regression analysis was performed for each parameter against age, height, weight, and body mass index (BMI; kg/m2) for males and females separately.
Most lung function variables were nonlinear with age and showed a plateau in younger adults, with a decline after 31 to 35 years. All spirometric data of men were higher than those of women except breathing frequency and forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC). All measured lung function parameters were strongly correlated to age, height, weight, and BMI. The highest correlation being to height in both men and women except for tidal volume and expiratory reserve volume among women. Based on previous studies, Caucasians men from the USA and Switzerland had higher FVC and FEV1 than in the present study, but only slightly higher than American blacks, British, Pakistani, and Singapore; an inverse trend was observed for Malay and Indians. Similar relationships were observed for women. The relationship between height and lung function parameters was nonlinear, with the variance of lung function parameters increasing with increasing height. For each sex, the z scores differed significantly by BMI (P < .001).
This study provides spirometry equations that can be used for Chinese individuals.
Keywords: healthy, lung function, never-smoking, reference values, Southeast China
1. Introduction
Normal lung function values are influenced by many factors, including age, height, body mass index (BMI, kg/m2), sex, ethnic origin, physical activity, environmental conditions, altitude, tobacco smoking, and socioeconomic status.[1–4] Recent studies presented equations for many populations in the world, but the Asian populations were only represented by Japanese, Indian, and Caucasian Australasian individuals.[5–7] Caucasian references may be inappropriate for Chinese.[8]
The results of pulmonary function tests in an individual are compared with those of healthy individuals. Therefore, the reference values will influence the treatment decisions, which will have important implications for the patients and the healthcare system. Several sets of normal values had been published over the last decades with considerably variable subject characteristics.[9–17] As a result, healthcare has been forced to adopt reference values derived from several different lung function studies. In Europe and America, the lung functions values and prediction equations are mostly derived from white and black individuals,[18–21] and these values cannot be used for the evaluation of Asian people, especially Chinese residing abroad and/of expatriates of Chinese origin. Since international guidelines discourage the use of spirometry reference equations excluding age, height, and race, there is a need to collect lung function data from Chinese individuals.[22]
The wide range of geographical and climatic conditions in a large country such as China may be associated with regional differences in lung function in healthy people. Failure to consider these ethnic and geographic differences in lung function could lead to errors in diagnosis and disease classification. Several reference values for Chinese populations have been published in the English literature,[8,13,14,23–27] but the available data did not include the influence of sex and age, except 1 study.[26] In addition, embarrassingly, no official reference values for Chinese are available.[8]
Therefore, the aim of this study was to establish new Chinese reference values and prediction equations for lung parameters such as forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1), and peak expiratory flow in individuals of 10 to 81 years of age. In addition, this study assessed the differences in lung function parameters using the new values and those from Caucasians from different parts of the world. It is critical to have appropriate standard values for lung function parameters. This would help diagnose various ailments, sometimes in early stage. Such values depend on many factors, and it is of great importance to acquire those specific to the Chinese population.
2. Methods
2.1. Reference population
Using the stratified-multi-steps-cluster sampling method, 101,182 males and females aged ≥10 yrs from urban and suburban areas (2 cities and 2 counties) of Zhejiang Province were invited to participate in the Chinese Body Physiological Constants Study between September 2016 and July 2017. From these subjects, individuals with any chronic disease were excluded, leaving 38,449 individuals. Among them, never-smokers were selected, leaving 12,142 individuals. Then, the exclusion criteria were applied: history of bronchodilators or antibiotics; common cold or acute bronchitis at spirometry measurement; cough, wheezing, or phlegm at spirometry measurement; history of asthma; history of chronic obstructive pulmonary disease of chronic bronchitis; or history of any lung disease, lung surgery, or pulmonary embolism.[21] After applying these criteria, 1457 individuals (749 males and 708 females) were available for analysis. Never-smokers were defined as subjects with a cumulative smoking history of <1 pack/yr (a pack/yr is defined as years of smoking × the number of cigarettes smoked per day divided by 20). Because of the very small proportion of non-Chinese people in Zhejiang Province, no exclusion was made based on race or nationality. The study was approved by the Ethics Committee of Kunming Medical College of Yunnan province of China.[11,23] Written informed consent was obtained from all subjects before examination.
2.2. Stratification
The 1457 subjects were divided into 17 age categories: 10 to 11, 12 to 13, 14 to 15, 16 to 17, 18 to 19, 20 to 22, 23 to 25, 26 to 30, 31 to 35, 36 to 40, 41 to 45, 46 to 50, 51 to 55, 56 to 60, 61 to 65, 66 to 70, ≥71 years.[21,28]
2.3. Evaluation of spirometric parameters
The pulmonary capacity tests included tidal volume (VT), breathing frequency (BF), expiratory reserve volume (ERV), inspiratory capacity, and vital capacity. The indices for pulmonary ventilatory tests consisted of FEV1, minute ventilation volume, FVC, FEV1%, and maximal voluntary ventilation. The indices for small airway function tests included peak expiratory flow rate (PEF); expiratory flow rates at 25%, 50%, and 75% (FEF25%, FEF50%, and FEF75%, respectively); and mid expiratory flow (MMEF75/25).[29]
During the time of data collection, “the Chinese Body Physiological Constants” team was equipped with Portable Pulmonary Function Equipment (Master Screen Rotary, Lab4.52, Jaeger, Germany). The equipment was calibrated at least once daily using a 3-L cylinder. The manipulator also performed a daily biological control by assessing the manipulator's own lung function. The manipulator initially went through formal training and was then continuously monitored during the entire study by the head of the project.
The participants were seated and wore a nose clip. Extension or flexion of the neck was avoided. Height and weight were measured bare foot, without clothes, and with standardized equipment. Barometer pressure, temperature, and relative humidity were registered every morning. Tests were performed in the sitting position according to American Thoracic Society guidelines without nose clips after an oral instruction by the technician. The participants were assisted by a specially trained pulmonary function technician during the course of start, duration, and end.[11,21,22,29]
2.4. Statistical analysis
All data were analyzed using SPSS 17.0 for Windows (IBM, Armonk, NY). Continuous data were expressed as mean ± standard deviation. Sex-specific regression equations for predicted reference values of pulmonary function in various powers and interactions were formulated based on age, height, weight, and BMI. Two-sided P values <0.05 were considered statistically significant.
3. Results
3.1. Characteristics of the study population
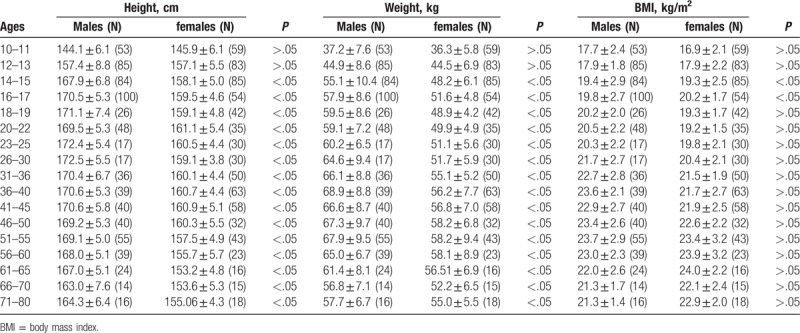
The characteristics of the study population are shown in Table 1. Of the 1457 subjects, there were 749 males and 708 females. There were few elderly people >71 years. In general, males were taller and heavier than their female counterparts for the same age groups, but the BMI has no difference.
Table 1.
Demographic data of the subjects of 10 to 80 years.
3.2. Spirometry data
Spirometry data are presented in Tables 2 to 4 (males) and Tables 5 to 7 (females). When scrutinizing the plots, most lung function variables were nonlinear with age and showed a plateau in younger adults, with a decline after 31 to 35 years. The linearity of decline of spirometric values varied with age. All spirometric data of men were higher than those of women except BF and FEV1/FVC (Fig. 1).
Table 2.
Pulmonary capacity data of males among different age groups.
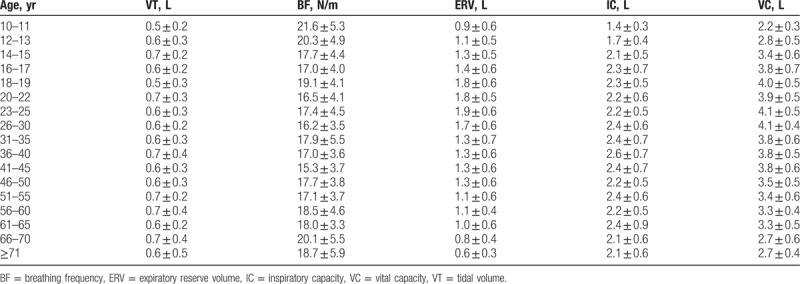
Table 4.
Small airway function data of males among different age groups.
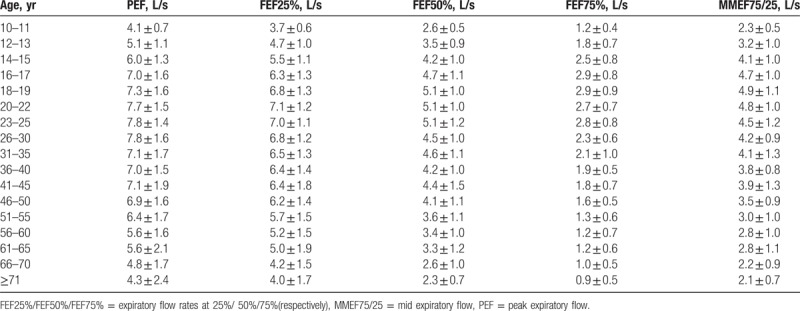
Table 5.
Pulmonary capacity data of females among different age groups.
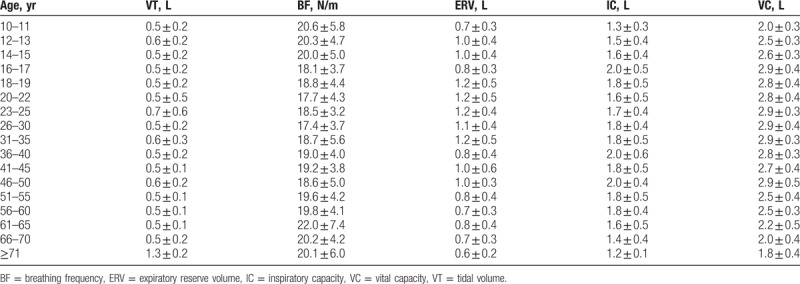
Table 7.
Small airway function data of females among different age groups.
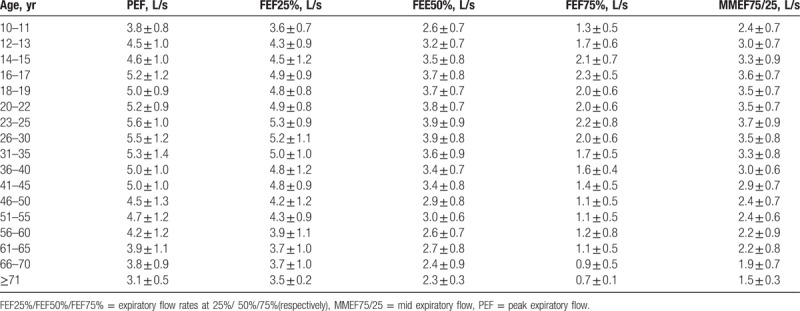
Figure 1.
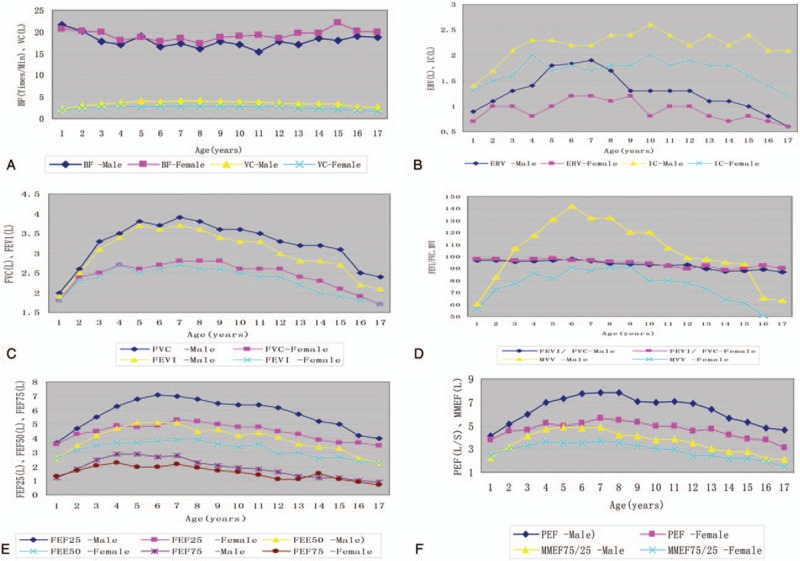
Spirometry data of all subjects across the 17 age categories, with 95% confidence. ERV = expiratory reserve volume, FEV1 = forced expiratory volume in 1 second, FVC = forced vital capacity, IC = inspiratory capacity, MVV = maximal voluntary ventilation, PEF = peak expiratory flow, VT = tidal volume.
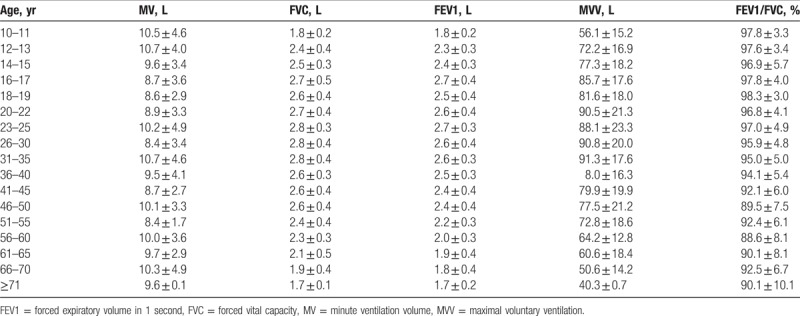
Table 3.
Pulmonary ventilation data of males among different age groups.
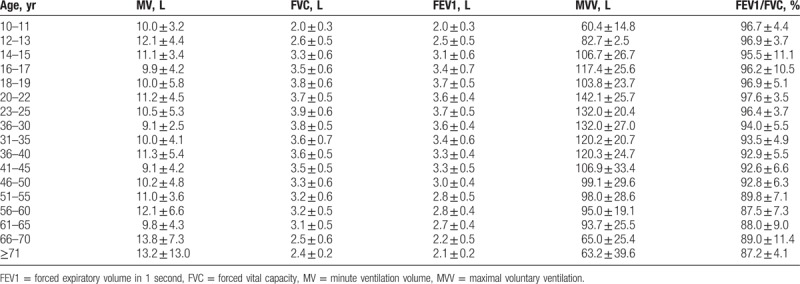
Table 6.
Pulmonary ventilation data of females among different age groups.
3.3. Prediction equations
All measured lung function parameters were strongly correlated to age, height, weight, and BMI. The highest correlation being to height in both men and women except for VT and ERV among females (Tables 8 and 9).
Table 8.
Prediction equations for the lung function variables of females.
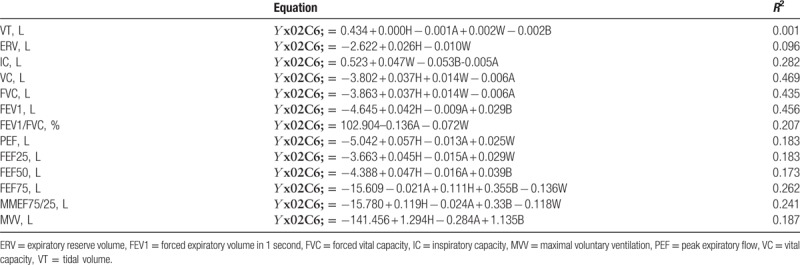
Table 9.
Prediction equations for the lung function variables of males.
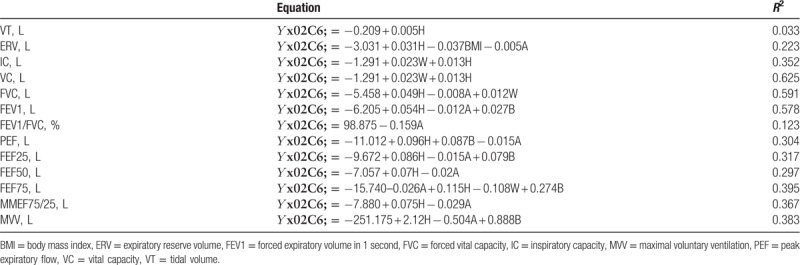
3.4. Comparisons with other populations
The predicted values of various pulmonary function measurements obtained from these regression equations for subjects of 30 years and height of 1.65 m for men and 1.55 m for women were compared with those from other studies.[3,14,21,30–34] Caucasians males from the USA and Switzerland had higher FVC and FEV1 than in the present study, but only slightly higher than American blacks, British, Pakistani, and Singapore; an inverse trend was observed for Malay and Indians (Fig. 2). Similar relationships were observed for women.
Figure 2.
Comparison of mean FVC and FEV1 in males and females using values from different populations. FEV1 = forced expiratory volume in 1 second, FVC = forced vital capacity.
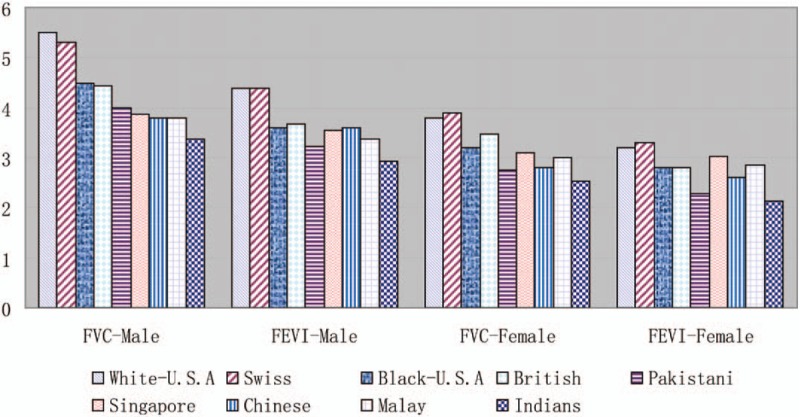
3.5. Association between height and lung function
Graphic analysis of raw data revealed that the relationship between height and lung function parameters was nonlinear, with the variance of lung function parameters increasing with increasing height (Fig. 3).
Figure 3.
Height dependency of mean values of lung function variables, Q1: ≤150 cm; Q2: 151–160 cm; Q3: 161–170 cm; Q4: 171–180 cm; Q5: >180 cm. ERV = expiratory reserve volume, FEV1 = forced expiratory volume in 1 second, FVC = forced vital capacity, IC = inspiratory capacity, MVV = maximal voluntary ventilation, PEF = peak expiratory flow, VT = tidal volume.
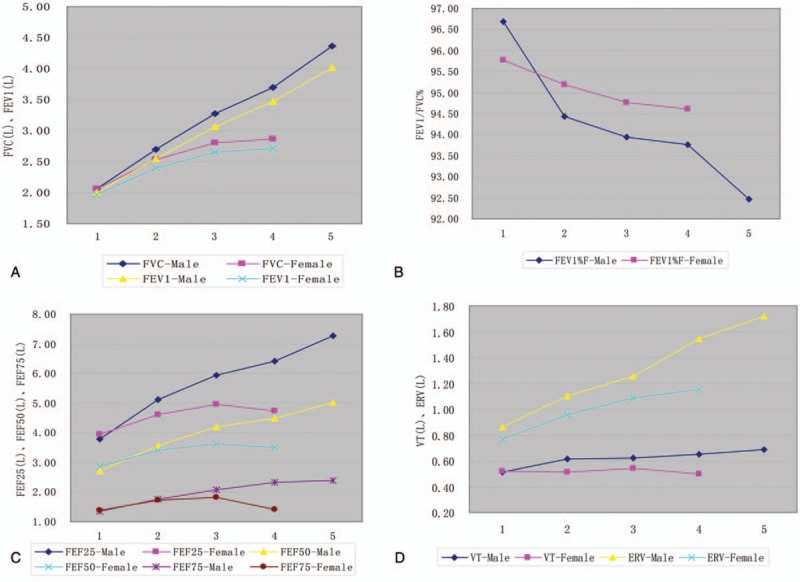
3.6. Association between BMI and lung function
The relationships between BMI and FEV1 and FVC were observed by plotting the z scores for each of the 5 quintiles of BMI (Fig. 4). For each sex, the z scores differed significantly by BMI (P < .001), being the greatest in the middle quintile ranges and lowest at the extremes. A different pattern was observed for FEV1% (P < .001).
Figure 4.
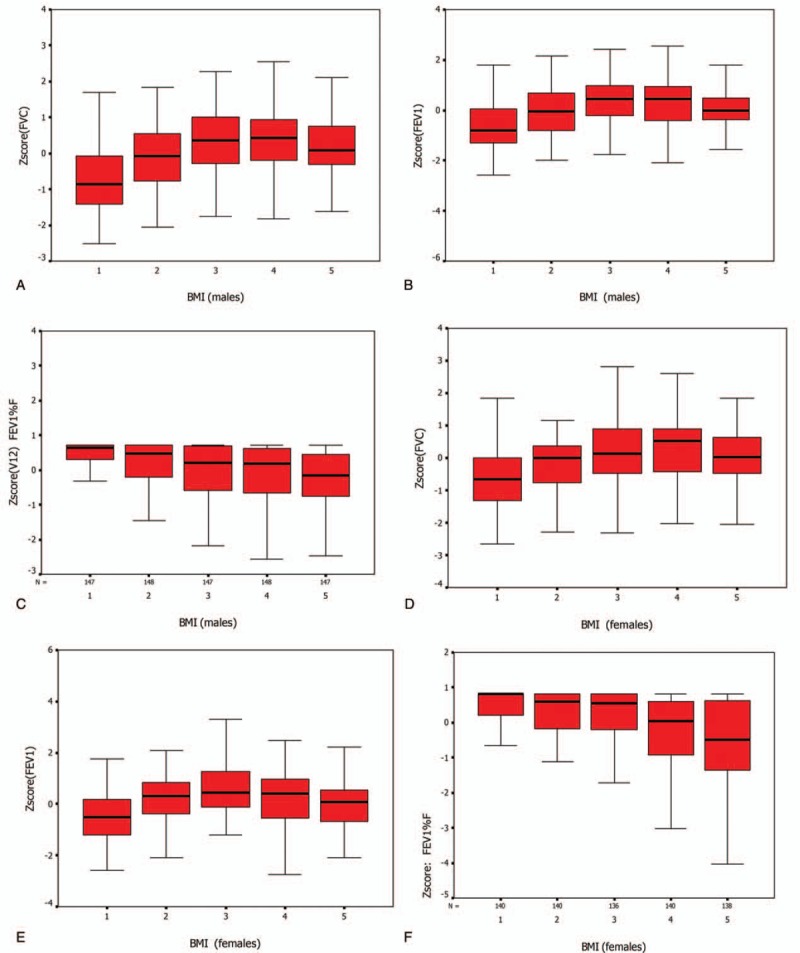
Z score (observed—predicted/SD about regression line) means and 95% confidence intervals for FEV1, FVC, and FEV1% for Chinese men and women by BMI quintile. In males: Q1: ≤17.94; Q2: 17.95–19.66; Q3: 19.67–21.59; Q4: 21.6–23.64; Q5: 23.65–30.78; in females: Q1: ≤17.94; Q2: 17.95–19.53; Q3: 19.54–20.89; Q4: 20.9–22.94; Q5: 22.94–31.4. BMI = body mass index, FEV1 = forced expiratory volume in 1 second, FVC = forced vital capacity.
4. Discussion
Embarrassingly, no official spirometry reference values for Chinese are available. Several reference values for Chinese populations have been published in the English literature,[8,13,14,23–27] but the available data did not include the influence of sex and age, except 1 study.[26] Therefore, the aim of the present study was to establish new Chinese reference values and prediction equations for lung parameters in Chinese individuals of 10 to 81 years of age. The results provide spirometry equations that can be used for Chinese individuals. The results also show that these equations are different from those derived from various populations around the globe.[3,14,21,30–34]
Lung function depends on a variety of individual, behavioral, and environmental factors.[1–4] It is obvious that these characteristics changed with the 1978 Chinese economic reform. Therefore, it is natural that the lung function values changed in the last 2 decades, making older references values obsolete.[35] Indeed, the values of FVC and FEV1 were different from those from earlier studies.[14–17] Although differences in equipment or methodology may explain some of these variations, much of it appears to be real and must therefore be due to other causes such as socioeconomic changes. Therefore, new data are necessary. The present study represents one of the largest evaluations to date of lung function among Chinese living in mainland China.[8,13,14,23–27] In addition to the large sample, strengths of the study include the use of a common manual of operations in all sites that incorporated well-recognized, standardized procedures and strict attention to quality control. These quality controls, based on repetitive measurements, showed no systematic differences among populations.[36]
In spite of the limitations of the sampling design, this large, well-characterized cohort provides useful insights into patterns of lung function among rural workers, industrial workers, teachers, students, and civil servant in the Zhejiang province of China. At the time this study was designed, it was impractical to attempt a true random sampling of local residents. Therefore, our choice of sampling frames within each geographic area was ultimately dictated by the practical realities of being able to carry out this large field trial with the lowest costs possible. Therefore, we consider that the population used for this study is likely to be no more or less representative of the general population of southeast China mainland.[12,37,38]
The lung function data and prediction equations were derived from 1457 healthy, nonsmoking, Chinese males and females who were living in Zhejiang Province. Establishing regression equations to predict various measurements of normal lung function on a regional basis in a country like China is pertinent because of the wide variations in geography, climate, food habits, and ethnic groups among different regions. Defining should variations is important for the treatment of patients with various illness.[39] Within a given age and height for both sexes, the average age-height adjusted values were consistently higher in males than in females, as supported by previous studies.[8,14,15,26,27] The prediction equations from the European Community for Coal and Steel, which were confirmed by the European Community Respiratory Health Survey, are commonly used in many of countries.[40,41] Approximately 97% of the residents of these countries are Caucasian. With globalization, many Chinese are emigrating to other countries, and lung function equations for Chinese individuals are needed. For these reasons, reference equations should be formulated for Chinese.[42,43]
Finally, the observed differences in lung function may in part reflect differences in BMI. The relationship between FVC, FEV1, and BMI was curvilinear. Lung function appears to increase with BMI at least through the first 60 percentiles of the population. This could be due, at least in part, to the abdominal distribution of body fat, which impedes the maximal expansion of the lungs.[44]
The present study is not without limitations. No infants (<10 years of age) were included. In addition, there were few elderly people ≥71 years. Therefore the applications of reference equations to this age group should be made with caution. No chest radiographic examinations were performed, which might have resulted in the inclusion of some patients with asymptomatic lung diseases of the restrictive type. The potential effect of altitude (8–43.2 m above sea level) was not tested simply because the Zhejiang province is a coastal region without mountains. Therefore, altitude should not be a confounding variable in the present study, as opposed to studies that included individuals living at high altitude.[45–47] Additional study is necessary to address these issues.
In conclusion, the present study provides spirometry reference values and equations that can be used for Chinese individuals.
Acknowledgments
The authors express special appreciation for the support of all the participants in Zhejiang Province, China.
Author contributions
Conceptualization: Chunlin Gao, Xiang Zhang, Zhongming Li.
Data curation: Chunlin Gao, Xiang Zhang, Dan Wang, Zhimin Wang, Jintao Li.
Formal analysis: Chunlin Gao, Xiang Zhang, Dan Wang, Zhimin Wang, Jintao Li, Zhongming Li.
Funding acquisition: Zhongming Li.
Project administration: Zhongming Li.
Writing – original draft: Chunlin Gao, Xiang Zhang.
Writing – review and editing: Dan Wang, Zhimin Wang, Jintao Li, Zhongming Li.
Footnotes
Abbreviations: BF = breathing frequency, BMI = body mass index, ERV = expiratory reserve volume, FEV1 = forced expiratory volume in 1 second, FVC = forced vital capacity, IC = inspiratory capacity, MV = minute ventilation volume, MVV = maximal voluntary ventilation, PEF = peak expiratory flow, VC = vital capacity, VT = tidal volume.
CLG and XZ contributed equally to this work.
Funding: This study was funded by the Special Fund for Key Basic Research Project of the Ministry of National Science and Technology of China (2001DA30031 and 2002DIA40018), National Natural Science Foundation of China (814601922), and Applied Basic Research of Yunnan Province (2017FE468-189).
The authors have no conflicts of interest to disclose.
References
- [1].Ostrowski S, Barud W. Factors influencing lung function: are the predicted values for spirometry reliable enough? J Physiol Pharmacol 2006;57(suppl 4):263–71. [PubMed] [Google Scholar]
- [2].Quanjer PH, Hall GL, Stanojevic S, et al. Age- and height-based prediction bias in spirometry reference equations. Eur Respir J 2012;40:190–7. [DOI] [PubMed] [Google Scholar]
- [3].Stanojevic S, Wade A, Stocks J, et al. Reference ranges for spirometry across all ages: a new approach. Am J Respir Crit Care Med 2008;177:253–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Al-Riyami BM, Al-Rawas OA, Hassan MO. Normal spirometric reference values for Omani children and adolescents. Respirology 2004;9:387–91. [DOI] [PubMed] [Google Scholar]
- [5].Quanjer PH, Stanojevic S, Cole TJ, et al. Multi-ethnic reference values for spirometry for the 3-95-yr age range: the global lung function 2012 equations. Eur Respir J 2012;40:1324–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Quanjer PH, Brazzale DJ, Boros PW, et al. Implications of adopting the Global Lungs Initiative 2012 all-age reference equations for spirometry. Eur Respir J 2013;42:1046–54. [DOI] [PubMed] [Google Scholar]
- [7].Hall GL, Thompson BR, Stanojevic S, et al. The Global Lung Initiative 2012 reference values reflect contemporary Australasian spirometry. Respirology 2012;17:1150–1. [DOI] [PubMed] [Google Scholar]
- [8].Jian W, Gao Y, Hao C, et al. Reference values for spirometry in Chinese aged 4-80 years. J Thorac Dis 2017;9:4538–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Jones AY, Dean E, Lam PK, et al. Discordance between lung function of chinese university students and 20-year-old established norms. Chest 2005;128:1297–303. [DOI] [PubMed] [Google Scholar]
- [10].Kumar A, Pannu BK, Manchanda KC, et al. Pulmonary function tests in healthy male Punjabi children (10-19 years of age). Indian J Chest Dis Allied Sci 1992;34:191–5. [PubMed] [Google Scholar]
- [11].Lung function testing: selection of reference values, interpretative strategies. American Thoracic Society. Am Rev Respir Dis 1991;144:1202–18. [DOI] [PubMed] [Google Scholar]
- [12].Vollmer WM, Tsai R, Wu Y, et al. Patterns of lung function in asymptomatic nonsmoking men and women in the People's Republic of China. Ann Epidemiol 2002;12:295–302. [DOI] [PubMed] [Google Scholar]
- [13].Yang TS, Peat J, Keena V, et al. A review of the racial differences in the lung function of normal Caucasian, Chinese and Indian subjects. Eur Respir J 1991;4:872–80. [PubMed] [Google Scholar]
- [14].Chia SE, Wang YT, Chan OY, et al. Pulmonary function in healthy Chinese, Malay and Indian adults in Singapore. Ann Acad Med Singapore 1993;22:878–84. [PubMed] [Google Scholar]
- [15].Neukirch F, Chansin R, Liard R, et al. Spirometry and maximal expiratory flow-volume curve reference standards for Polynesian, European, and Chinese teenagers. Chest 1988;94:792–8. [DOI] [PubMed] [Google Scholar]
- [16].Da Costa JL. Pulmonary function studies in healthy Chinese adults in Singapore. Am Rev Respir Dis 1971;104:128–31. [DOI] [PubMed] [Google Scholar]
- [17].Ching B, Horsfall PA. Nomograms for forced expiratory volume and forced vital capacity in normal Cantonese subjects. Mod Med Asia 1978;14:47–9. [PubMed] [Google Scholar]
- [18].Sterk PJ, Fabbri LM, Quanjer PH, et al. Standardized challenge testing with pharmacological, physical and sensitizing stimuli in adults. Eur Respir J 1993;6(suppl 16):53–83. [DOI] [PubMed] [Google Scholar]
- [19].Quanjer PH, Tammeling GJ, Cotes JE, et al. Lung volumes and forced ventilatory flows. Report Working Party Standardization of Lung Function Tests, European Community for Steel and Coal. Official Statement of the European Respiratory Society. Eur Respir J Suppl 1993;16:5–40. [PubMed] [Google Scholar]
- [20].Roca J, Burgos F, Sunyer J, et al. References values for forced spirometry. Group of the European Community Respiratory Health Survey. Eur Respir J 1998;11:1354–62. [DOI] [PubMed] [Google Scholar]
- [21].Kuster SP, Kuster D, Schindler C, et al. Reference equations for lung function screening of healthy never-smoking adults aged 18–80 years. Eur Respir J 2008;31:860–8. [DOI] [PubMed] [Google Scholar]
- [22].Standardization of Spirometry, 1994 Update. American Thoracic Society. Am J Respir Crit Care Med 1995;152:1107–36. [DOI] [PubMed] [Google Scholar]
- [23].Wang XR, Yano E, Wang M, et al. Pulmonary function in long-term asbestos workers in China. J Occup Environ Med 2001;43:623–9. [DOI] [PubMed] [Google Scholar]
- [24].Ip MS, Karlberg EM, Karlberg JP, et al. Lung function reference values in Chinese children and adolescents in Hong Kong. I. Spirometric values and comparison with other populations. Am J Respir Crit Care Med 2000;162:424–9. [DOI] [PubMed] [Google Scholar]
- [25].Ip MS, Ko FW, Lau AC, et al. Updated spirometric reference values for adult Chinese in Hong Kong and implications on clinical utilization. Chest 2006;129:384–92. [DOI] [PubMed] [Google Scholar]
- [26].Zhang J, Hu X, Shan G. Spirometry reference values for population aged 7–80 years in China. Respirology 2017;22:1630–6. [DOI] [PubMed] [Google Scholar]
- [27].Wu Y, Zhang Z, Gang B, et al. Predictive equations for lung function based on a large occupational population in North China. J Occup Health 2009;51:471–7. [DOI] [PubMed] [Google Scholar]
- [28].Baynard T, Pitetti KH, Guerra M, et al. Age-related changes in aerobic capacity in individuals with mental retardation: a 20-yr review. Med Sci Sports Exerc 2008;40:1984–9. [DOI] [PubMed] [Google Scholar]
- [29].Chen L, Zhao M, Han SM. Testing and analyzing the lung functions in the normal population in Hebei Province [in Chinese]. Zhongguo Yi Xue Ke Xue Yuan Xue Bao 2004;26:463–6. [PubMed] [Google Scholar]
- [30].Korotzer B, Ong S, Hansen JE. Ethnic differences in pulmonary function in healthy nonsmoking Asian-Americans and European-Americans. Am J Respir Crit Care Med 2000;161:1101–8. [DOI] [PubMed] [Google Scholar]
- [31].Neder JA, Nery LE, Peres C, et al. Reference values for dynamic responses to incremental cycle ergometry in males and females aged 20 to 80. Am J Respir Crit Care Med 2001;164:1481–6. [DOI] [PubMed] [Google Scholar]
- [32].Langhammer A, Johnsen R, Gulsvik A, et al. Forced spirometry reference values for Norwegian adults: the Bronchial Obstruction in Nord-Trondelag Study. Eur Respir J 2001;18:770–9. [DOI] [PubMed] [Google Scholar]
- [33].Aggarwal AN, Gupta D, Behera D, et al. Applicability of commonly used Caucasian prediction equations for spirometry interpretation in India. Indian J Med Res 2005;122:153–64. [PubMed] [Google Scholar]
- [34].Gillum RF. Chronic obstructive pulmonary disease in blacks and whites: pulmonary function norms and risk factors. J Natl Med Assoc 1991;83:393–401. [PMC free article] [PubMed] [Google Scholar]
- [35].Du J. Economic reforms and health insurance in China. Soc Sci Med 2009;69:387–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Roberts CM, MacRae KD, Winning AJ, et al. Reference values and prediction equations for normal lung function in a non-smoking white urban population. Thorax 1991;46:643–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].An epidemiological study of cardiovascular and cardiopulmonary disease risk factors in four populations in the People's Republic of China. Baseline report from the P.R.C.-U.S.A. Collaborative Study. People's Republic of China--United States Cardiovascular and Cardiopulmonary Epidemiology Research Group. Circulation 1992;85:1083–96. [DOI] [PubMed] [Google Scholar]
- [38].Data from USA-PRC Collaborative Study of Cardiovascular and Cardiopulmonary Epidemiology U.S. Department of Health and Human Services, Public Health Service. Bethesda: National Institutes of Health; 1992. [Google Scholar]
- [39].Vijayan VK, Kuppurao KV, Venkatesan P, et al. Pulmonary function in healthy young adult Indians in Madras. Thorax 1990;45:611–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Roche N, Dalmay F, Perez T, et al. FEV1/FVC and FEV1 for the assessment of chronic airflow obstruction in prevalence studies: do prediction equations need revision? Respir Med 2008;102:1568–74. [DOI] [PubMed] [Google Scholar]
- [41].Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J 2005;26:948–68. [DOI] [PubMed] [Google Scholar]
- [42].Schnabel E, Nowak D, Brasche S, et al. Association between lung function, hypertension and blood pressure medication. Respir Med 2011;105:727–33. [DOI] [PubMed] [Google Scholar]
- [43].Marek W, Marek E, Muckenhoff K, et al. Time for new reference values for ventilatory lung function. Eur J Med Res 2009;14(suppl 4):140–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Clinical Guidelines on the Identification, Evaluation, Treatment of Overweight, Obesity in Adults—The Evidence Report. National Institutes of Health. Obes Res 1998;6(suppl 2):51S–209S. [PubMed] [Google Scholar]
- [45].Brandli O, Schindler C, Kunzli N, et al. Lung function in healthy never smoking adults: reference values and lower limits of normal of a Swiss population. Thorax 1996;51:277–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Heath D, Williams DR. The lung at high altitude. Invest Cell Pathol 1979;2:147–56. [PubMed] [Google Scholar]
- [47].White NW, Hanley JH, Lalloo UG, et al. Review and analysis of variation between spirometric values reported in 29 studies of healthy African adults. Am J Respir Crit Care Med 1994;150:348–55. [DOI] [PubMed] [Google Scholar]


