Abstract
Background:
It aimed to observe the effect of electro-acupuncture on the improvement of psychiatric symptoms, as well as anxiety and depression in methamphetamine (MA) addicts during abstinence using randomized controlled trials.
Methods:
All patients in the present study received compulsory drug detoxification in Shanghai Drug Rehabilitation Center. All patients were enrolled consecutively from June 2014 to February 2015; data collection was completed in March 2015. According to the randomized, single-blind and control principle, 68 men MA addicts were randomly divided into 2 groups: electro-acupuncture (EA) and sham electro-acupuncture (sham-EA) groups. Patients were given 20 minutes EA or sham-EA treatment every Monday, Wednesday, and Friday, with a total of 4 weeks. Positive and Negative Syndrome Scale (PANSS), Hamilton Anxiety Scale (HAMA), and Hamilton Depression Scale (HAMD) were used to evaluate the patients’ psychotic symptoms, anxiety and depression before treatment and after receiving treatment with 1 to 4 weeks, respectively.
Results:
EA could effectively improve the symptoms of psychosis, anxiety, and depression during abstinence in patients with MA addiction. In terms of PANSS score, the scores for positive symptoms and general psychopathological symptoms in patients after receiving 1 to 4 weeks of treatment were significantly decreased compared with the control group, while the score for negative symptoms was significantly decreased after receiving 2 and 4 weeks of treatment. For the HAMA score, the psychotic anxiety scores in patients receiving 1 to 4 weeks of treatment were significant lower than the control group. In terms of HAMD score, there was a significant reduction in anxiety/somatization and sleep disturbance scores after the 4 weeks of EA treatment.
Conclusion:
Electroacupuncture helps to improve psychiatric symptoms and anxiety and depression in MA addicts during abstinence, and promote rehabilitation of patients.
Keywords: abstinence, electroacupuncture, methamphetamine, psychotic symptoms
1. Introduction
Amphetamines are the most rapidly growing new psychoactive substances in the world in recent years.[1] Its representative drug methamphetamine (MA) has a similar chemical structure with the catecholamine neurotransmitters.[2] MA mainly acts on the central nervous system, can make people feel excitation and produce fantasy, where multiple ingestion can even lead to drug addiction. Discontinuation of MA can cause confusion, anxiety, violence, insomnia and a series of clinical symptoms, and high doses can produce toxic effects.[3] During abstinence of MA addiction, patients are prone to psychotic symptoms, as well as anxiety, depression, and other negative symptoms, which are one of the prominent manifestations in the early stage of abstinence of MA addiction, but also are an important factor of maintaining and inducing relapse of methamphetamine. MA is prone to producing mental dependence and insignificant manifestations of physical dependence, where 60% to 80% of MA addicts appeared auditory hallucination, visual hallucination, and other psychiatric symptoms during the use of MA.[4] At present, it is thought that the psychotic symptoms caused by MA addiction may occur in acute and chronic poisoning and abstinence periods, which manifest most significantly in abusers who are severely addictive, and may even lead to insanity and schizophrenia.[5,6] At the same time, patients may appear sleep disorders, anxiety, depression, decline in energy, and vitality and other manifestations during abstinence of MA.[7] Studies have revealed that the abstinence symptoms in MA addicts is closely related to the patients’ psychological factors, the most prominent of which is anxiety and depression after abstinence, and a prolonged abuse of MA will worsen mental illness in patients,[8] of which anxiety and depression symptoms are important factors that cause cravings.
Currently, drug detoxifications show an unsatisfactory curative effect for amphetamine-type drugs, and are mostly limited to symptomatic treatment, such as cognitive behavioral therapy and inspirational motivation, etc.[9] There is a lack of a drug that has been approved by Food and Drug Administration for treatment of methamphetamine addiction. Clinically, antipsychotics are more commonly used for the treatment of MA addicts, while typical antipsychotics have many adverse reactions. At present, atypical antipsychotic drug olanzapine (serotonin—dopamine antagonist) is more extensively studied. Patients with symptoms such as anxiety are treated with clonazepam, and those with depression are given paroxetine, while those with hallucinations or delusions are given a combination of risperidone and risperidone, etc.[10] Although the patients’ symptoms can be improved after receiving targeted treatment, there are deficiencies such as poor efficacy and prone to varying degrees of adverse reactions, etc.
Research on acupuncture detoxification started from the treatment of opioids addiction. Studies have found that acupuncture, as an adjuvant therapy for detoxification, shows a good efficacy for the treatment of abstinence symptoms after morphine addiction.[11] Compared with drug treatment, acupuncture detoxification has no side effects, no dependence, and no drug interaction. We have hypothesized that amphetamine addiction have a similar mechanism with opioids addiction. In our earlier study, we applied EA for the treatment of MA addiction, and the results also confirmed that EA could improve MA abstinence symptoms.[12] However, clinical acupuncture treatment for psychiatric symptoms that predispose to MA during addiction abstinence has not been reported yet. Hence, based on the results of our earlier study, this article aimed to investigate the clinical efficacy of acupuncture for the treatment of psychiatric symptoms as well as anxiety and depression appeared during MA abstinence period.
2. Materials and methods
2.1. Study design and participants
This randomized trial was conducted in Shanghai Drug Rehabilitation Centre. The study design was clinical randomized single-blind control method. Eligible MA abstinence patients who were admitted from June 2014 to February 2015 were assigned into EA group (n = 34) and sham EA group (n = 34) according to the random number method generated using SPSS18.0 software (SPSS Inc., Chicago, IL). All the patients signed informed consent. The study was approved by the Institutional Review Board of Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine (Shanghai, China). Informed consent was obtained from all individual participants included in the study.
Inclusion criteria: Patients who were diagnosed according to the amphetamines dependence described in the Diagnostic and Statistical Manual of Mental Disorders (the 5th edition) (DSM-V).[13] Adult man aged 18 to 60 years old. More than 3 months of MA abuse, more than 6 months of dependence history. Methamphetamine positive in urinalysis, and receiving natural abstinence therapy for <1 week. Prior to enrolment, positive and negative symptom scale score ≥60 points. Patients who agreed to reject any other treatment that might affect the result of this trial during the study period. Patients who had never received acupuncture treatment. Patients who signed informed consent.
Exclusion criteria: Patients with serious heart, liver, lung, kidney diseases, or hematological diseases. Patients with severe liver disease, veneral diseases, AIDS, and other infectious diseases. Patients with severe digestive disease and athrepsia. Patients with serious trauma that was not healed. Patients with psychiatric history. Patients with major psychosis. Patients who could not discontinue other treatment that might affect the efficacy judgement of the present treatment.
Rejection and withdrawal criteria: Patients who terminated the treatment due to acupuncture fainting and other adverse reactions. Patients who were not able to continue treatment due to involvement in criminal cases would be considered withdrawal from the study. Patients who terminated the treatment due to other irresistible non-treatment factors would be considered withdrawal from the study (Fig. 1).
Figure 1.
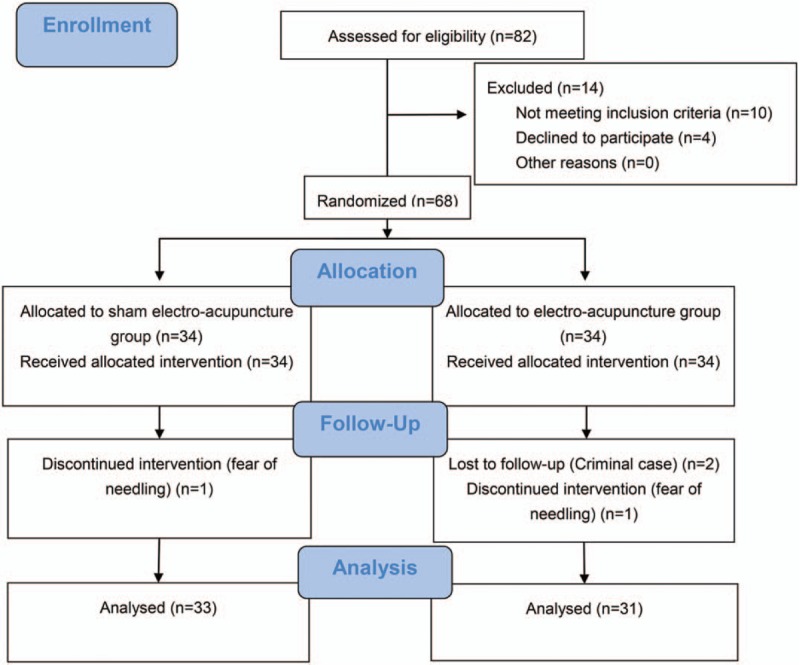
Study flow diagram.
2.2. Intervention
Acupuncture was performed by a trained traditional Chinese medicine practitioner. Patients were required to relax in a sitting position. Hands of the operator and acupuncture points were routinely disinfected with 75% alcohol. In the EA group, the needle (a disposable tube needle, 0.18 mm × 25 mm, Suzhou Medical Appliance Factory, China) was inserted via a tube. The acupoints included bilateral Jia ji (T5, L2), bilateral Nei gui (PC6) and Shen men (HT7), bilateral Zu san li (ST36) and San yin jiao (SP6). Acupoints were selected according to nomenclature and location of acupuncture points[14] (Fig. 2). Among them, the needles were inserted 6 to 10 mm into Nei guan and Shen men, and 10 to 15 mm into other acupoints. After Deqi was achieved, the bilateral traditional huatuojiaji points (T5, L2) were connected to the EMS Professional (model: G6805-II, Shanghai Medical Electronic Instrument Factory, China), current range of 10 to 30 mA, continuous wave, electro-acupuncture stimulation frequency 2 Hz. The electro-acupuncture stimulation intensity was adjusted to a value the patients would not feel discomfort. The needles were retained for 20 minutes. The same needles and insertion methods were adopted in the sham-EA group, but the needles were inserted with a depth of <5 mm. The needles were inserted from 20 mm away from the T5, L2 jiaji points, and 10 mm away from other acupoints. Needles were not manipulated after insertion, and there was no Deqi, for which the EA instrument was connected but not energized.[15] Patients were given EA treatment on Monday, Wednesday, and Friday for continuously 4 weeks, a total of 12 times of treatment. During treatment, if the patient appeared fainting and other adverse reactions, treatment should be terminated immediately and be addressed. In addition, patients of both groups were given a 1-hour health education every Friday afternoon during the treatment period. All patients were coercive, and were not given psychological counseling and other treatment. Communication between researchers and patients was limited to the need for acupuncture and assessment of scales.
Figure 2.
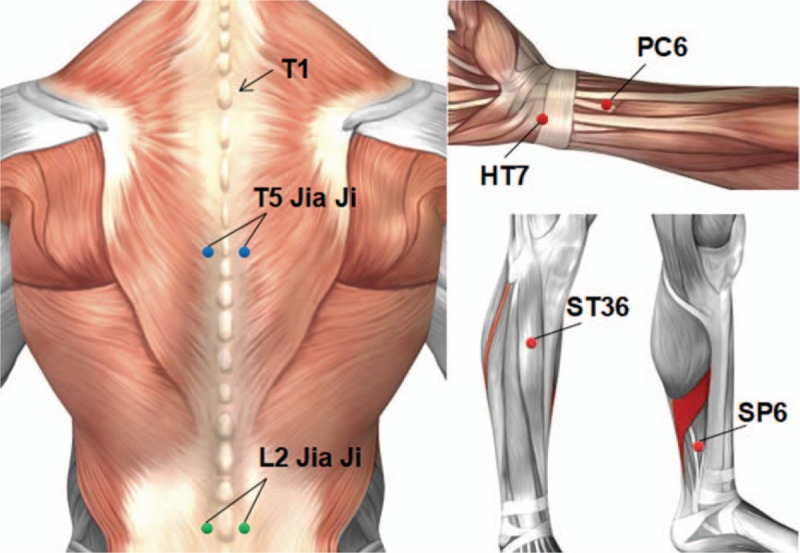
The anatomic locations of acupuncture sites.
2.3. Measurement
Positive and Negative Syndrome Scale (PANSS) was used to assess the psychiatric symptoms of MA addicts after abstinence. It consisted of 33 items and was divided into 3 subscales: positive symptoms, negative symptoms, and general psychopathological symptoms, as well as 3 supplemental items. The psychiatric symptoms were assessed using 7 grades, where grade 1 to grade 7 referred to no symptom to very severe symptoms. In addition, Hamilton Anxiety Scale (HAMA) scale was used to assess anxiety symptoms. It consisted of 2 subscales: psychic anxiety and somatic anxiety, in which the symptoms were assessed using 5 grades, where grade 0 to grade 4 referred to no symptom to extremely severe symptoms. Hamilton Depression (HAMD) scale was used to assess the depression symptoms. It included 7 subscales: anxiety/somatization, weight, cognitive impairment, diurnal variation, blockage, sleep disorders, and hopelessness, in which the symptoms were assessed using 5 grades, where grade 0 to grade 4 referred to no symptom to extremely severe symptoms.
Scales were assessed by 2 fixed staffs who did not participate in EA treatment. Before the start of the clinical trial, the operators received 1-week of scale evaluation training by experts, so as to uniform evaluation term and standardize the evaluation process. The 3 scales were evaluated before treatment, at the 1st, 2nd, 3rd, and 4th days of treatment, once a week for a total of 5 times. At the same time, all the adverse events that occurred during the acupuncture operation were recorded.
2.4. Statistical analysis
Before the start of the study, power analysis (Ψ = 2.52) was performed based on the MA abstinence symptoms assessment in MA-dependent patients in our preclinical studies, so as to determine the size of the sample. Statistical analyses were performed using SPSS18.0 software. Measurement data were expressed as mean ± standard deviation ( ). Data in accordance with normality and homogeneity of variance were analyzed using one-way Analysis of Variance (ANOVA) and Least-Significant Difference (LSD) test, while those not in accordance with normality and homogeneity of variance were analyzed using Kruskal–Wallis H test and Nemenyi test. The scores of each scale were analyzed using repeated measurement data analysis of variance, multivariate analysis of variance, and LSD test. While category data (such as marital status and education level) were analyzed using chi-square test. A difference with P < .05 was considered statistically significant.
). Data in accordance with normality and homogeneity of variance were analyzed using one-way Analysis of Variance (ANOVA) and Least-Significant Difference (LSD) test, while those not in accordance with normality and homogeneity of variance were analyzed using Kruskal–Wallis H test and Nemenyi test. The scores of each scale were analyzed using repeated measurement data analysis of variance, multivariate analysis of variance, and LSD test. While category data (such as marital status and education level) were analyzed using chi-square test. A difference with P < .05 was considered statistically significant.
3. Results
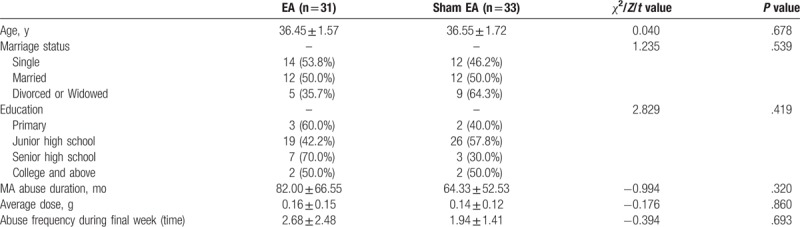
A total of 68 patients who were accordance with the inclusion criteria and signed informed consent were enrolled. Among them, there were 4 withdrawal patients, 2 referral patients due to criminal cases, and 2 acupuncture fainting patients, which resulted in a total of 64 patients who actually completed the study (31 cases of the EA group and 33 cases of the sham-EA group). There was no significant differences in demographic characteristics, duration of MA abuse, average dose for each time of MA abuse, and abuse frequency in the final week between the EA and sham-EA groups (P > .05, Table 1).
Table 1.
Baseline data.
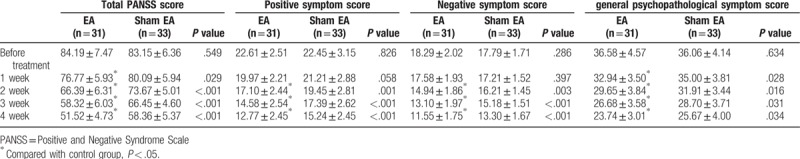
In terms of total PANSS score for MA addicts after abstinence, the PANSS score of the EA group was significantly lower than that of the sham-EA group after 1 to 4 weeks of treatment (P < .05). With the prolongation of treatment time, the PANSS score of the EA group was even more significantly declined. Meanwhile, in terms of the PANSS positive symptom score and the PANSS negative symptom score, the curative effect showed significant difference after receiving 2 to 4 weeks of treatment (P < .05). For general psychopathological symptom score, the curative effect showed significant difference after receiving 1 to 4 weeks of treatment (P < .05) (Table 2).
Table 2.
Comparison of total PANSS score ( , point).
, point).
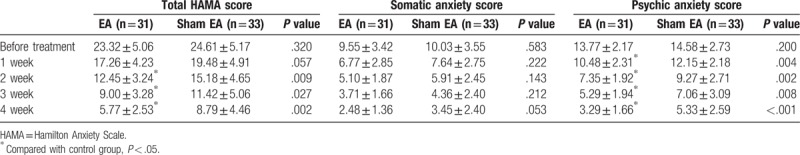
In terms of HAMA score for MA addicts after abstinence, the score of the EA group was significantly lower than that of the sham-EA group after receiving 2 to 4 weeks of treatment (P < .05). With the prolongation of treatment time, the HAMA score of the EA group was even more significantly declined. In terms of HAMA somatic anxiety score, there was no significant difference between the 2 groups (P > .05). In terms of the HAMA psychic anxiety score, the score of EA group was significantly lower than that of the sham-EA group after receiving 1 to 4 weeks of treatment (P < .05) (Table 3).
Table 3.
Comparison of total HAMA score ( , point).
, point).
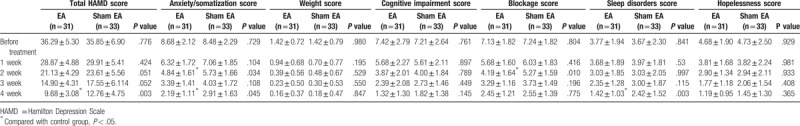
In terms of HAMD score for MA addicts after abstinence, the score of the EA group was significantly lower than that of the sham-EA group after receiving 4 weeks of treatment (P < .05). In terms of HAMD anxiety/ somatization score, the curative effect of the EA group was better than that of the sham-EA group after receiving 2 and 4 weeks of treatment (P < .05). For the HAMD blockage score, the curative effect of the EA group was better than that of the sham-EA group after receiving 2 weeks of treatment (P < .05), but it did not show significant difference after receiving 3 weeks and 4 weeks of treatment (P > .05). For the HAMD sleep disorders score, the curative effect of the EA group was better than that of the sham-EA group after receiving 4 weeks of treatment (P < .05). There were no significant differences in HAMD weight, cognitive impairment, and hopelessness between the 2 groups (Table 4).
Table 4.
Comparison of total HAMD score ( , point).
, point).
4. Safety
MA addicts enrolled in this clinical trial were adult men, which excluded the adverse reactions such as somatic symptoms and emotional symptoms that appeared in menstrual cycle in women during the acupuncture period, which further ensured the consistency of the findings. During the acupuncture treatment, the patients did not have other complications that needed treatment. And there was no bleeding, hematoma, and infection at the acupuncture point.
5. Discussion
MA abstinence symptoms are different from those of opioid addiction drugs. The main feature is that a long-term exposure is prone to causing psychotic symptoms, as well as the associated anxiety, depression, and other emotional symptoms. Effective improvement of psychiatric symptoms as well as anxiety, depression, and other negative symptoms appearing during MA abstinence are the key factors to promote rehabilitation and inhibit relapse of MA addicts.
Currently, there are few reports on the clinical research of acupuncture for amphetamine-type drugs and lack of clinical evidence. Amphetamine-induced psychotic disorders are similar to paranoid schizophrenia, and are also referred to as “amphetamine-induced psychosis.”[16] There is already evidence that acupuncture can effectively improve the symptoms of schizophrenia patients. For example, acupuncture can improve the clinical core symptoms of schizophrenia as well as anxiety and depression.[15,17] Some data have revealed that acupuncture can improve both the positive and negative symptoms of chronic schizophrenia.[18] In the meantime, a good sleep can improve memory and daily living ability.[19] Meanwhile, sleep disorder is not conducive to mental rehabilitation in patients with schizophrenia.[20] Acupuncture can effectively improve the quality of life of patients with mental illness, especially sleep quality,[21] thereby to correct their psychiatric symptoms.[20] A clinical study showed that acupuncture and anti-schizophrenia drug paliperidone had similar efficacy in improving sleep disorders in schizophrenia patients.[20] Acupuncture can play a positive regulatory role in the drug treatment process, which can promote restoration of normal body function. Patients with drug addiction tend to choose acupuncture treatment.[22] The intervention of acupuncture can reduce the psychological perplexity[23] and increase confidence in drug treatment,[24] which is also a manifestation of “regulation of mental activity” of acupuncture. In the present study, we found that during the 4-week EA treatment, EA intervention could significantly improve the patient's psychotic symptoms (including positive, negative, and general psychopathological symptoms) as well as anxiety and depression symptoms. However, the EA had a slower effect in improving depression symptoms. The patients’ depression symptoms were improved until the 4th week of treatment, which mainly manifested in aspects of anxiety/somatization and sleep disorders.
In terms of the MA addiction mechanism, it is generally believed that the MA addiction is associated with dopamine and other neurotransmitters in the central nervous system.[25–27] Meanwhile, the acupuncture precisely can have a function of two-way benign regulation, which can adjust the excitatory and inhibitory processes in the cerebral cortex through the nervous, endocrine and immune systems, thereby to balance various neurotransmitters between brain neuronal synapses, and thus improve the abstinence symptoms after drug addition,[28] and reduce the relapse rate.[29] Hence, we hypothesize that acupuncture may be used as an adjunct to MA addicts during abstinence to improve their psychotic symptoms, anxiety and depression after MA withdrawal.
Our previous studies have found that heroin addicts may appear tenderness points beside the T5 and L2 spines, and their abstinence symptoms can be improved by puncturing Jiaji point with electro-acupuncture.[12] The T5, L2 Jiaji point is on the one hand near to the Governor Vessel, on the other hand transverse the Ping xin shu (BL15) and Shen shu (BL27), and thus has a function of tranquilizing and sedating the mind. Meanwhile, Nei guan (PC6) and Shen men (HT7) can regulate the mind by combination with Zu san li (ST36) and San yin jiao (SP6). Therefore, we selected this combination of points for treatment of abstinence symptoms after MA addition.
In summary, patients receiving EA showed a more significant improvement in abstinence symptoms than those without undergoing EA, which compensates for the deficiency of acupuncture for treatment of MA addiction, and provides scientific basis for acupuncture treatment as an adjunctive therapy during withdrawal from MA.
The present study has some limitations. First, depressive symptoms after MA addition were not satisfactorily improved. Hence, selection of points to improve the depressive symptoms during abstinence in MA addicts will be one of the key directions of our subsequent studies. Second, the present study only enrolled a small sample size with a short observation time. Third, it is important to compare with other current clinical treatments used in MA addiction to demonstrate the efficacy of EA treatment. This is another direction we will focus on next.
Acknowledgment
Thanks to Daqing Shi, Nursing Department, of the Shanghai Drug Abstinence Rehabilitation Center and all the staffs of the Squadrons 3,4 and 5 for their support and assistance to the present study. Thanks to Ke Wang, associate professor of Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine for his help in the writing.
Author contributions
Conceptualization: Liang Zeng, Wenguang Hou.
Data curation: Liang Zeng, Ying Tao, Lei Zong, Lei Yu.
Formal analysis: Liang Zeng, Ying Tao, Wenguang Hou, Lei Zong, Lei Yu.
Funding acquisition: Lei Zong, Wenguang Hou.
Project administration: Lei Zong, Wenguang Hou.
Writing – original draft: Liang Zeng.
Writing – review & editing: Ying Tao, Wenguang Hou, Lei Zong, Lei Yu.
Footnotes
Abbreviations: DSM-V = Diagnostic and Statistical Manual of Mental Disorders (the 5th edition), EA = electro-acupuncture, HAMA = Hamilton Anxiety Scale, HAMD = Hamilton Depression Scale, MA = methamphetamine, PANSS = Positive and Negative Syndrome Scale, sham-EA = sham electro-acupuncture.
This study was funded by Traditional Chinese Medicine Research Project of Shanghai Health and Family Planning Commission (No. 2014LP106A) and Three-year Action Plan for Further Accelerating Traditional Chinese Medicine Development (No. ZY3-JSFC-1-1023).
The authors declare that they have no conflict of interest.
References
- [1].Miliano C, Serpelloni G, Rimondo C, et al. Neuropharmacology of New Psychoactive Substances (NPS): focus on the rewarding and reinforcing properties of Cannabimimetics and Amphetamine-Like Stimulants. Front Neurosci 2016;10:153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Eugenin EA, Greco JM, Frases S, et al. Methamphetamine alters blood brain barrier protein expression in mice, facilitating central nervous system infection by neurotropic Cryptococcus neoformans. J Infect Dis 2013;208:699–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Rusyniak DE. Neurologic manifestations of chronic methamphetamine abuse. Psychiatr Clin North Am 2013;36:261–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Mahoney JJ, 3rd, Kalechstein AD, De La Garza R, 2nd, et al. Presence and persistence of psychotic symptoms in cocaine- versus methamphetamine-dependent participants. Am J Addict 2008;17:83–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Grant KM, LeVan TD, Wells SM, et al. Methamphetamine-associated psychosis. J Neuroimmune Pharmacol 2012;7:113–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Zarrabi H, Khalkhali M, Hamidi A, et al. Clinical features, course and treatment of methamphetamine-induced psychosis in psychiatric inpatients. BMC Psychiatry 2016;16:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Ren Q, Ma M, Yang C, et al. BDNF-TrkB signaling in the nucleus accumbens shell of mice has key role in methamphetamine withdrawal symptoms. Transl Psychiatry 2015;5:e666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Zorick T, Nestor L, Miotto K, et al. Withdrawal symptoms in abstinent methamphetamine-dependent subjects. Addiction 2010;105:1809–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Hoffmann L, Schumann N, Fankhaenel T, et al. Methamphetamine use in Central Germany: protocol for a qualitative study exploring requirements and challenges in healthcare from the professionals’ perspective. BMJ Open 2016;6:e011445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Farnia V, Shakeri J, Tatari F, et al. Randomized controlled trial of aripiprazole versus risperidone for the treatment of amphetamine-induced psychosis. Am J Drug Alcohol Abuse 2014;40:10–5. [DOI] [PubMed] [Google Scholar]
- [11].Han JS, Zhang RL. Suppression of morphine abstinence syndrome by body electroacupuncture of different frequencies in rats. Drug Alcohol Depend 1993;31:169–75. [DOI] [PubMed] [Google Scholar]
- [12].Liang Y, Xu B, Zhang XC, et al. [Comparative study on effects between electroacupuncture and auricular acupuncture for methamphetamine withdrawal syndrome]. Zhongguo Zhen Jiu 2014;34:219–24. [PubMed] [Google Scholar]
- [13].American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-V). Arlington,VA: American Psychiatric Association; 2013. [Google Scholar]
- [14].State Bureau of Quality Technical Supervision. GB/T 12346-2006, Nomenclature and location of acupuncture points (released on September 18, 2006, and implemented on December 1, 2006) (in Chinese). [Google Scholar]
- [15].Jing C, Gaohua W, Ling X, et al. Electro-acupuncture versus sham electro-acupuncture for auditory hallucinations in patients with schizophrenia: a randomized controlled trial. Clin Rehabil 2009;23:579–88. [DOI] [PubMed] [Google Scholar]
- [16].Franken IH, Hendriks VM. Screening and diagnosis of anxiety and mood disorders in substance abuse patients. Am J Addict 2001;10:30–9. [DOI] [PubMed] [Google Scholar]
- [17].Reshef A, Bloch B, Vadas L, et al. The effects of acupuncture treatment on sleep quality and on emotional measures among individuals living with schizophrenia: a Pilot Study. Sleep Disord 2013;2013:327820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Bosch P, Staudte H, van den Noort M, et al. A case study on acupuncture in the treatment of schizophrenia. Acupunct Med 2014;32:286–9. [DOI] [PubMed] [Google Scholar]
- [19].Noort MV, Struys E, Perriard B, et al. Schizophrenia and depression: the relation between sleep quality and working memory. Asian J Psychiatr 2016;24:73–8. [DOI] [PubMed] [Google Scholar]
- [20].Bosch P, van den Noort M, Staudte H, et al. Schizophrenia and depression: a systematic review of the effectiveness and the working mechanisms behind acupuncture. Explore (NY) 2015;11:281–91. [DOI] [PubMed] [Google Scholar]
- [21].Huang Y, Zheng Y. [Sleep disorder of schizophrenia treated with shallow needling: a randomized controlled trial]. Zhongguo Zhen Jiu 2015;35:869–73. [PubMed] [Google Scholar]
- [22].Ashton H, Nodiyal A, Green D. Acupuncture or counselling: outcomes and predictors of treatment choice in a non-statutory addiction service. J Subst Use 2009;14:151–60. [Google Scholar]
- [23].Bergdahl L, Berman AH, Haglund K. Patients’ experience of auricular acupuncture during protracted withdrawal. J Psychiatr Ment Health Nurs 2014;21:163–9. [DOI] [PubMed] [Google Scholar]
- [24].Bernstein KS. The experience of acupuncture for treatment of substance dependence. J Nurs Scholarsh 2000;32:267–72. [DOI] [PubMed] [Google Scholar]
- [25].Harris DS, Boxenbaum H, Everhart ET, et al. The bioavailability of intranasal and smoked methamphetamine. Clin Pharmacol Ther 2003;74:475–86. [DOI] [PubMed] [Google Scholar]
- [26].Newton TF, De La Garza R, 2nd, Fong T, et al. A comprehensive assessment of the safety of intravenous methamphetamine administration during treatment with selegiline. Pharmacol Biochem Behav 2005;82:704–11. [DOI] [PubMed] [Google Scholar]
- [27].Kim MR, Kim SJ, Lyu YS, et al. Effect of acupuncture on behavioral hyperactivity and dopamine release in the nucleus accumbens in rats sensitized to morphine. Neurosci Lett 2005;387:17–21. [DOI] [PubMed] [Google Scholar]
- [28].White A. Trials of acupuncture for drug dependence: a recommendation for hypotheses based on the literature. Acupunct Med 2013;31:297–304. [DOI] [PubMed] [Google Scholar]
- [29].Cui CL, Wu LZ, Li YJ. Acupuncture for the treatment of drug addiction. Int Rev Neurobiol 2013;111:235–56. [DOI] [PubMed] [Google Scholar]


