Abstract
The aim of the present study was to evaluate the diagnostic accuracy of low-radiation-dose and low-contrast-dose (double low-dose) coronary computed tomography angiography (CTA) for coronary artery stenosis in patients with suspected coronary artery disease (CAD).
Totally 88 patients with suspected CAD were divided in the routine and double low-dose groups. Subjective image quality (IQ) was scored and diagnostic performance for detecting ≥50% stenosis was determined with the invasive coronary angiography. IQ and diagnostic performance were analyzed and compared between the 2 groups.
There was no significant difference in the IQ of coronary artery between the routine and double low-dose groups, with good inter-observer agreement for the IQ. There were no significant differences in the sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic accuracy on the per-patient, per-vessel, or per-segment level between the routine and double low-dose groups. The contrast medium injection volume in the double low-dose group was reduced by 37.1% compared with the routine-dose group. The effective dose in the double low dose was reduced by 44.5% compared with the routine-dose group.
Double low-dose coronary CTA with IR can acquire satisfactory IQ and have high diagnostic sensitivity, specificity, and accuracy for the detection of coronary artery stenosis.
Keywords: contrast medium volume, coronary artery disease, computed tomography angiography, prospective electrocardiographic gating, radiation dose
1. Introduction
With the rapid development of multi-slice spiral computed tomography (CT), the diagnostic sensitivity, specificity, and accuracy of coronary CT angiography (CTA) to detect the coronary heart diseases have been significantly improved, which has become an irreplaceable method for the disease screening.[1] Recently, the high radiation dose and the carcinogenic potential of coronary CTA have attracted increasing attention. Numerous studies have investigated the value of low-radiation-dose coronary artery CTA in the diagnosis of coronary heart diseases.[2–4] However, most of these studies have not involved the comparison with the routine-dose coronary CTA. It could not be confirmed whether the reduced radiation dose lead to decreased diagnostic accuracy of CAD. In addition, these studies mainly focus on reducing the radiation dose, in which the reduction in the contrast medium volume has been rarely concerned. Actually, high contrast medium volume might result in increased risk for iodinated contrast-induced nephropathy, which is one of the most common causes of acute renal failure. Therefore, it is of great importance and significance to reduce the contrast medium volumes in coronary CTA.[5]
In recent years, the double low-dose coronary CTA has become a research hotspot, and the studies have been mainly focusing on the image quality (IQ).[6,7] However, the exhaustive evaluation of IQ is impossible, and it is indeed unnecessary. In addition, it could not help to find out whether the coronary CTA with decreased contrast and radiation doses would jeopardize the disease diagnosis. In this study, the diagnostic value of double low-dose coronary CTA for coronary artery diseases (CADs) was investigated, in the comparison with the routine-dose coronary CTA.
2. Materials and methods
2.1. Study patients
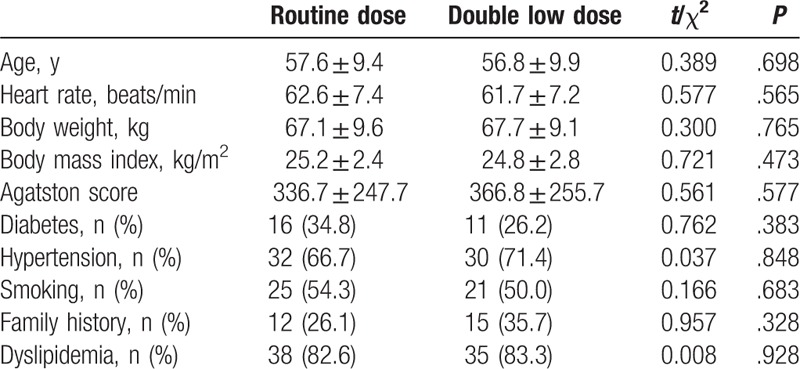
Totally 208 patients who admitted to our hospital from December 2014 to May 2015 were initially included in this study. The heart rate (HR) should be ≤70 beats/min during scanning, and the patients with the HR >70 beats/min were orally given β-blocker prior to the scanning. In these patients, 96 cases underwent the invasive coronary angiography (ICA) examination within 2 weeks of coronary CTA. Exclusion criteria were as follows: patients with the body mass index (BMI) > 30 kg/m2; cardiac index < 2.5 L/min/m2; previous coronary artery bypass grafting; hypersensitivity to the iodine-containing contrast medium; nephropathy with the serum creatinine level > 120 μmol/L; untreated hyperthyroidism; or pregnancy. In these subjects, 8 patients were excluded due to the previous coronary artery bypass grafting (n = 2), creatinine clearance rate ≤ 120 μmol/L (n = 2), allergic reactions to iodinated contrast medium (n = 1), or HR >70 beats/min during the scanning (n = 3). Therefore, totally 88 patients (48 males and 40 females) were finally included in the analysis. These 88 patients were randomly divided into the routine-dose group (n = 46) and the double low-dose group (n = 42). The study protocol was approved by the local ethics committee, and written informed consents were obtained from all the patients. General information of these included patients is given in Table 1.
Table 1.
Baseline information of included patients.
2.2. Contrast medium injection protocol
High concentration (350 mgI/mL) of contrast medium (Ultravist, iopromide; Bayer Schering Pharma, Berlin, Germany) was applied herein. Contrast medium was administered with a Dual Shot mechanical power injector (MedRad Inc, Indianola, IN), via a 20-gauge cannula inserted into the antecubital vein. After the delivery of contrast medium, 30 mL saline was injected at the same flow rate. For the routine-dose group, 70 mL contrast medium was intravenously injected at the flow rate of 5 mL/s. For the double low-dose group, the contrast medium dose was determined based on the body weight and BMI. Coefficient of 0.7 mL/kg was applied for the underweight and normal patients (BMI ≤ 25 kg/m2), while 0.6 mL/kg was used for the overweight and obese patients (25 kg/m2 < BMI ≤ 30 kg/m2). In the low-dose group, fixed injection duration (10 seconds) was used, and the contrast medium flow rate was determined according to the following formula:
2.3. CT examination
The CT scanning was performed on a 256-row multi-detector CT scanner (Brilliance iCT; Philips Healthcare, Cleveland, OH). Automatic bolus tracking (Bolus Pro; Philips Healthcare) was used for the region of interest in the descending aorta. CT data acquisition was initiated under the full inspiration at 6 seconds after the predetermined signal attenuation threshold of 120 and 90 Hounsfield units (HUs), for the routine- and low-dose groups, respectively. Patients from the routine-dose group were scanned by the conventional protocol, with 120 kVp, 150 mAs, and a 0.27-second gantry rotation (prospectively electrocardiography [ECG] triggered). On the contrary, patients from the low-dose groups were scanned by the conventional protocol, with 100 kVp, 150 mAs, and a 0.27-second gantry rotation (prospectively ECG triggered). Imaging trigger was centered on the physiologic cardiac phase of ventricular diastasis corresponding to 75% of the R–R interval.
2.4. CT data reconstruction and image analysis
The fourth generation of IR algorithm (iDose4; Philips Healthcare) was used to reconstruct the images. The IR levels of L4 were used to compensate for the noise increase due to the dose reduction of 50%.[8,9] All images were reconstructed using a standard cardiac kernel and a cosmic filter (XCB), with the matrix size of 1024 × 1024.
2.5. Coronary CTA and ICA date analysis
Coronary segments were divided into 15 segments, according to the American Heart Association (AHA) reporting system. If present, the intermediate artery (ramus intermedius) was designated as Segment 16, and considered to belong to the left anterior descending (LAD) artery.[10] Coronary CTA data analysis was performed by 2 blinded and independent observers with 10-year experience in coronary CTA. A 4-point scoring system was applied: 1 = non-diagnostic (blurred vessel wall or severe artifacts, impairing accurate evaluation); 2 = fair (moderate artifacts, but acceptable for diagnosis); 3 = good (minor artifacts, with good diagnostic quality); and 4 = excellent (free of artifacts, with unrestricted evaluation). The presence of >50% luminal stenosis was evaluated on the per-patient, per-vessel, and per-segment levels by both the observers, and consensus agreement should be reached.
On the contrary, ICA was performed according to the conventional Judkins technique. At least 5 views from the left coronary artery and 3 views from the right coronary artery were visually evaluated for luminal stenosis >50% by the consensus agreement of 2 experienced cardiologists, who were blinded to the coronary CTA results. Coronary artery segments were defined according to the AHA reporting system, similar to the coronary CTA.
2.6. Statistical analysis
The SPSS 17.0 software was used for statistical analysis. The ICA was considered as the gold standard, and the sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic accuracy of the coronary CTA were calculated on the segment-, vessel-, and patient-based levels. Coronary segments < 1.5 mm, and those unable to be evaluated, were not included in the analysis. When the stenosis in a coronary artery segment was more than 50%, the coronary artery branch and the patients were regarded as positive. Comparison for the IQ and diagnostic accuracy between the 2 groups were performed with the Chi-squared test. P < .05 was considered statistically significant.
3. Results
3.1. Qualitative image analysis of coronary arteries
Qualitative image analysis was first performed for the coronary arteries. The 2 radiologists showed very good consistency in subjective scoring (Kappa=0.80). Our results showed that there were no significant differences in the subjective scores of all the qualitative analyses, between the routine- and low-dose groups (χ2 = 0.4450; P = .5047; Table 2). These results suggest that compared with the routine-does CT protocol, the low-radiation-dose and low-contrast-dose protocols do not affect the quality of coronary artery imaging.
Table 2.
Image quality of coronary segments in the 2 groups.

3.2. Diagnostic accuracy of coronary CTA for CAD
To evaluate the value of double low-dose coronary CTA in the diagnosis of CAD, it was compared with the routine-dose coronary CTA for the detection of coronary artery stenosis in patients with suspected CADs. There was a good interobserver agreement (Kappa = 0.81) for the detection of coronary stenosis between these 2 observers. Using ICA as the reference standard, both the routine- and double low-dose groups showed good sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic accuracy in the segment-, vessel-, and patient-based analyses, with no significant differences between these 2 groups (Table 3 and Fig. 1).
Table 3.
Diagnostic accuracy of coronary computed tomography angiography for the detection of coronary artery disease.
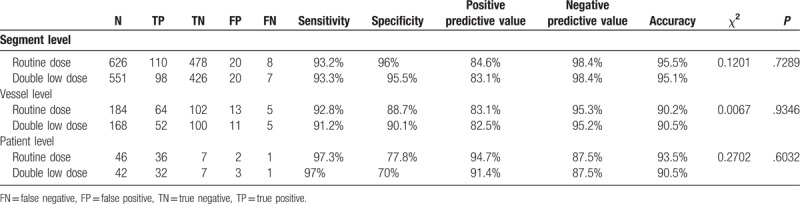
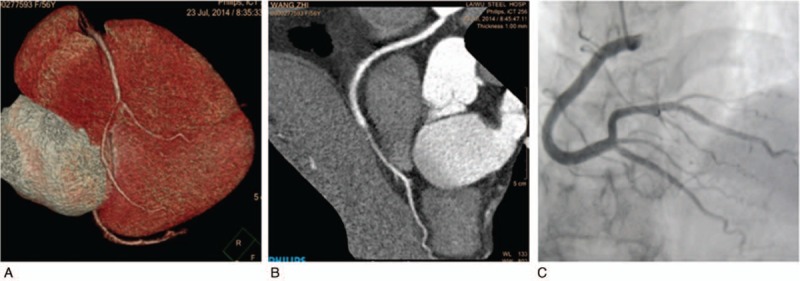
Figure 1.

Prospectively gated transaxial (PGT) 256-slice coronary computed tomography angiography (CTA) in a 69-year-old man with chest pain. PGT 256-slice coronary CTA (effective radiation dose, 1.01 mSv) was performed in a 69-year-old man (weighing 70.0 kg; body mass index, 26.5 kg/m2) with chest pain. Totally 42 mL contrast medium (350 mgI/mL) was delivered, at the injection rate of 4.2 mL/s. (A) Curved multiplanar reformation of left anterior descending (LAD) showed significant stenosis in the proximal segment caused by the mixed plaque. (B) Catheter angiography of the LAD.
In details, for the routine-dose group, 598 segments were correctly recognized, while 8 segments failed to show the presence of significant stenosis (false negative) and 20 segments were incorrectly diagnosed as significant narrowing (false positive). The incorrect diagnosis was due to the dense calcification in 18 segments (13 false-positive and 5 false-negative cases) and motion artifacts in 6 segments (4 false-positive and 2 false-negative cases), respectively. Moreover, 2 segments were misdiagnosed as stenosis (false positive) because of the poor filling of blood vessels, while 1 segment was misdiagnosed (false positive) because of the transient spasm of the right coronary. Furthermore, another segment failed to show the presence of significant stenosis (false negative) in the proximal of posterior descending artery.
On the contrary, for the double low-dose group, the coronary CTA correctly recognized 524 segments, which was consistent with the results of the ICA, while 7 segments failed to show the presence of significant stenosis (false negative) and 20 segments were incorrectly diagnosed as significant narrowing (false positive). The incorrect diagnosis was due to the dense calcification in 17 segments (13 false-positive and 4 false-negative cases; Fig. 2), motion artifacts in 5 segments (3 false-positive and 2 false-negative cases), and poor filling of blood vessels in 4 segments (3 false-positive and 1 false-negative cases; Fig. 3). Moreover, 1 segment was misdiagnosed as stenosis (false positive) because of the compression caused by the crossing-over of the cardiac vein and the low luminal density. Taken together, these results suggest that double low-dose coronary CTA could provide equally high diagnostic value as with routine-dose CTA.
Figure 2.

Prospectively gated transaxial (PGT) 256-slice coronary computed tomography angiography (CTA) in a 72-year-old man with chest pain. PGT 256-slice coronary CTA (effective radiation dose, 1.02 mSv) was performed in a 72-year-old man (weighing 70.0 kg; body mass index, 24.2 kg/m2) with chest pain. Totally 49 mL contrast medium (350 mgI/mL) was delivered at the injection rate of 4.9 mL/s. Curved multiplanar reformation of the left anterior descending (A) and right coronary artery (RCA; B) showed significant stenosis in the proximal segment caused by calcified plaque, which were false positive according to the catheter angiography (C, D).
Figure 3.
Prospectively gated transaxial (PGT) 256-slice coronary computed tomography angiography (CTA) in a 56-year-old man with chest pain. PGT 256-slice coronary CTA (effective radiation dose, 1.28 mSv) was performed in a 56-year-old man (weighing 67.0 kg; body mass index, 27.2 kg/m2) with chest pain. Totally 40 mL contrast medium (350 mgI/mL) was delivered at the injection rate of 4.0 mL/s. (A, B) Volume-rendering curved multiplanar reformation of the right coronary artery (RCA) showed significant stenosis in the distal segment caused by poor blood filling. (C) Catheter angiography of the RCA.
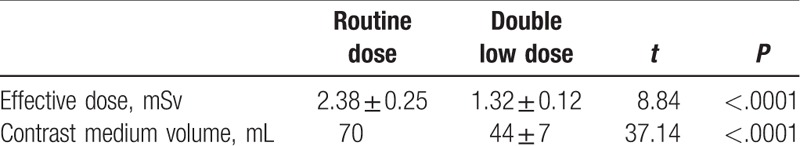
3.3. Radiation doses and contrast medium volume of routine- and double low-dose groups
The radiation doses and contrast medium volume for the routine- and double low-dose groups were then investigated. For the routine-dose group, 36 patients were triggered at 75% of the R–R interval, without ±5% buffer, while ±5% buffer was used in 10 patients. For the double low-dose group, 35 patients were triggered at 75% of the R–R interval without ± 5% buffer, while ± 5% buffer was used in 7 patients. Moreover, the contrast medium injection volume in the double low-dose group (44 ± 5 mL) was reduced by 37.1%, compared with the routine-dose group (70 mL). The effective dose in the double low-dose group (1.32 ± 0.12 mSv) was reduced by 44.5%, compared with the routine-dose group (2.38 ± 0.25 mSv) (Table 4). These results suggest that the double low-dose protocol obviously reduces the radiation dose and contrast dose, compared with the routine-dose protocol.
Table 4.
Effective dose and contrast medium volume for the 2 groups.
4. Discussion
In the present study, our results showed that the double low-dose protocol led to 44.5% reduction in the radiation dose and 37.1% reduction in the contrast dose, compared with the routine-dose group. Moreover, double low-dose provided satisfactory IQ, and had high sensitivity, specificity, and diagnostic accuracy in patients with suspected CAD. There were no significant differences in the quantitative image and diagnostic accuracy analysis between these 2 groups.
Lembcke et al[7] have suggested that, with the decreased contrast dose, intracoronary attenuation of coronary artery would be significantly reduced. However, most reports believe that the adequate vascular opacification remains critical in the coronary CTA.[11,12] It is important to ensure the adequate vascular opacification of coronary artery follows the decreased contrast dose. The use of low-tube-voltage technique allows reduced radiation dose while effectively increases the contrast enhancement, with the disadvantage of increased image noise.[13,14] However, the contrast-to-noise ratio (CNR) could not be affected by the increased image noise, because the low kVp scanning also increases the contrast enhancement via an increasing photoelectric effect.[15] Recent clinical studies concerning the cardiac CT have suggested that 80 or 100 kVp scanning is suitable for the reduced radiation dose.[16–19] Our results showed that the protocol involving 100 kVp tube voltage was suitable for the contrast dose reduction at about 37.1% in the cardiac CT on a 256-slice CT scanner. There was no significant difference in the IQ between double low- and routine-dose groups, and the image qualifying rate of these 2 groups were higher than the international level (96.8%).[20,21] In the routine-dose group, incorrect diagnosis was due to the dense calcification in 18 segments (64.3%), which was the cause in 17 segments (63%) for the double low-dose group. Obviously, dense calcification represented the primary cause for misdiagnosis.
It has been proposed that severe calcification can significantly reduce the diagnostic accuracy of coronary CTA for CAD.[22,23] Due to the relatively small sample size in our study, the patients with different calcium scores were not subjected to the subgroup analysis. However, the calcium scores were compared between these 2 groups. Our results showed that there was no significant difference in the calcium scores between these 2 groups, which could avoid the influence of different calcification levels on the diagnosis. Wang et al[24] have showed no improvements in the diagnostic value of coronary CTA with IR versus FBP, although the reduced calcium blooming could be achieved with the use of IR. Our results were consistent with those from Scheffel et al.[25] They have reported improvements in the overall IQ and CNR using the model-based IR technique, compared with FBP. The IQ is getting uniformly worse in the presence of calcification, and no improvement is achieved in reducing calcium blooming with the use of IR. Proportions of misdiagnosed patients with calcification were the same for these 2 groups, indicating that the double low-dose coronary CTA examination did not increase the calcification artifact in the diagnosis for CAD.
Among the misdiagnosed segments in these 2 groups, 11 segments were caused by the motion artifact, in which 6 cases belonged to the routine-dose group (4 false-positive and 2 false-negative cases), and 5 cases belonged to the double low-dose group (3 false-positive and 2 false-negative cases). Sudden acceleration of HR in patients is the main factor leading to motion artifact. Consequently, for the patients with relatively large fluctuation in the HR, β-blocker was suggested prior to the scanning (even though the HR of those patients was <70 beats/min), to avoid the sudden HR acceleration during the examination.
Our results showed that there were 6 coronary artery segments misdiagnosed because of the poor blood filling in these 2 groups, in which 4 segments belonged to the double low-dose group and 2 segments belonged to the routine-dose group. Although there were more cases misdiagnosed because of the poor blood filling in the double low-dose group than the routine-dose group, it was difficult to confirm whether it was related to the decreased contrast dose due to the limited subject sizes herein. Additionally, 4 out of the 6 misdiagnosed segments occurred on the left circumflex (LCX), we speculated that it would be related to the cardiac compression. LCX is closer to the heart, which could easily induce poor blood filling, because it is more anfractuous than the LAD and the right coronary artery (RCA). Consequently, further researches are still needed to find out whether the decreased contrast dose is one of the possible reasons for the poor blood vessel filling.
These were some limitations of this study. First, this was a single-center study, with relatively limited sample size. The enrolled patients had already undergone ICA, which might lead to selection bias with medium to high disease prevalence. This patient population was not typical for what was reported in the previous literature concerning coronary CTA. Second, only the luminal diameter narrowing >50% of the coronary artery was defined as the diagnostic criterion herein. Grouping was not performed based on the light, moderate, and severe grades of vascular stenosis. Third, the imaging protocol and reconstruction parameters were not individually adapted based on the information from the calcium scoring images. The IQ improvement was not focused on, and the potential benefits of sharper reconstruction kernels on the reduced blooming in the calcification areas were not investigated.
In conclusion, our results showed that the combination of 100 kVp prospectively ECG-triggered CTA with low contrast dose (about 40–50 mL, 350 mgI/mL) could acquire satisfactory IQ and showed high sensitivity, specificity, and accuracy in diagnosing the patients with suspected CAD. These findings might contribute the disease diagnosis with coronary CTA in clinic.
Author contributions
Conceptualization: Lei Song.
Data curation: Zhenqiang Wang.
Formal analysis: Jun Zhao.
Methodology: Zhaogui Ba, Feixue Zhang.
Resources: Wei Zhang, Yonghua Zhang.
Software: Huaying Lv, Yonghua Zhang.
Supervision: Lei Song.
Writing – original draft: Wei Zhang.
Writing – review & editing: Lei Song.
Footnotes
Abbreviations: AHA = American Heart Association, BMI = body mass index, CAD = coronary artery disease, CNR = contrast-to-noise ratio, CTA = computed tomography angiography, HR = heart rate, ICA = invasive coronary angiography, IQ = image quality, LCX = left circumflex, RCA = right coronary artery.
WZ and ZB contributed equally to this work.
This study was supported by the Key R&D Program of Shandong Province (Public Welfare Special Project; no: 2017GSF218100).
The authors have no conflicts of interest to disclose.
References
- [1].George RT, Arbab-Zadeh A, Cerci RJ, et al. Diagnostic performance of combined noninvasive coronary angiography and myocardial perfusion imaging using 320-MDCT: the CT angiography and perfusion methods of the CORE320 multicenter multinational diagnostic study. AJR Am J Roentgenol 2011;197:829–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Sun ML, Lu B, Wu RZ, et al. Diagnostic accuracy of dual-source CT coronary angiography with prospective ECG-triggering on different heart rate patients. Eur Radiol 2011;21:1635–42. [DOI] [PubMed] [Google Scholar]
- [3].Stehli J, Fuchs TA, Bull S, et al. Accuracy of coronary CT angiography using a submillisievert fraction of radiation exposure. J Am Coll Cardiol 2014;64:772–80. [DOI] [PubMed] [Google Scholar]
- [4].Layritz C, Schmid J, Achenbach S, et al. Accuracy of prospectively ECG-triggered very low-dose coronary dual-source CT angiography using iterative reconstruction for the detection of coronary artery stenosis: comparision with invasive catheterization. Eur Heart J Cardiocasc Imaging 2014;15:1238–45. [DOI] [PubMed] [Google Scholar]
- [5].Yang WJ, Chen KM, Liu B, et al. Contrast media volume optimization in high-pitch dual-source CT coronary angiography: feasibility study. Int J Cardiovasc Imaging 2013;29:245–52. [DOI] [PubMed] [Google Scholar]
- [6].Nakaura T, Kidoh M, Sakaino N, et al. Low contrast-and low radiation does protocol for cardiac CT of thin adults at 256-row CT: usefulness of low tube voltage scans and the hybrid iterative reconstruction algorithm. Int J Cardiovasc Imaging 2013;29:913–23. [DOI] [PubMed] [Google Scholar]
- [7].Lembcke A, Schwenke C, Hein PA, et al. High-pitch dual-source CT coronary angiography with low volumes of contrast medium. Eur Radiol 2014;24:120–7. [DOI] [PubMed] [Google Scholar]
- [8].Hou Y, Ma Y, Fan W, et al. Diagnostic accuracy of low-dose 256-slice multi-detector coronary CT angiography using iterative reconstruction in patients with suspected coronary artery disease. Eur Radiol 2014;24:3–11. [DOI] [PubMed] [Google Scholar]
- [9].Hou Y, Xu S, Guo W, et al. The optimal dose reduction level using iterative reconstruction with prospective ECG-triggered coronary CTA using 256-slice MDCT. Eur J Radiol 2012;81:3905–11. [DOI] [PubMed] [Google Scholar]
- [10].Hou Y, Liu X, Xv S, et al. Comparisons of image quality and radiation dose between iterative reconstruction and filtered back projection reconstruction algorithms in 256-MDCT coronary angiography. AJR Am J Roentgenol 2012;199:588–94. [DOI] [PubMed] [Google Scholar]
- [11].Cademartiri F, Mollet NR, Lemos PA, et al. Higher intracoronary attenuation improves diagnostic accuracy in MDCT coronary angiography. AJR Am J Roentgenol 2006;187:W430–3. [DOI] [PubMed] [Google Scholar]
- [12].Cademartiri F, Maffei E, Palumbo AA, et al. Influence of intra-coronary enhancement on diagnostic accuracy with 64-slice CT coronary angiography. Eur Radiol 2008;18:576–83. [DOI] [PubMed] [Google Scholar]
- [13].Nakayama Y, Awai K, Fumama Y, et al. Abdomimal CT with low tube voltage:preliminary observations about radiation dose, contrast enhancement, image quality, and noise. Radiology 2005;237:945–51. [DOI] [PubMed] [Google Scholar]
- [14].Wang W, Zhao YE, Qi L, et al. Prospectively ECG-triggered high-pitch coronary CT angiography at 70 kVp with 30 mL contrast agent: an intraindividual comparison with sequential scanning at 120 kVp with 60 mL contrast agent. Eur J Radiol 2017;90:97–105. [DOI] [PubMed] [Google Scholar]
- [15].Takx RAP, Krissak R, Fink C, et al. Low-tube-voltage selection for triple-rule-out CTA: relation to patient size. Eur Radiol 2017;27:2292–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Zhang C, Zhang Z, Yan Z, et al. 320-row CT coronary angiography: effect of 100-kV tube voltages on image quality, contrast volume, and radiation dose. Int J Cardiovasc Imaging 2011;27:1059–68. [DOI] [PubMed] [Google Scholar]
- [17].LaBounty TM, Leipsic J, Poulter R, et al. Coronary CT angiography of patients with a normal body mass index using 80 kVp versus 100 kVp: a prospective, multicenter, multivendor randomized trial. AJR Am J Roentgenol 2011;197:W860–7. [DOI] [PubMed] [Google Scholar]
- [18].Sun G, Hou YB, Zhang B, et al. Application of low tube voltage coronary CT angiography with low-dose iodine contrast agent in patients with a BMI of 26-30 kg/m2. Clin Radiol 2015;70:138–45. [DOI] [PubMed] [Google Scholar]
- [19].Mangold S, Wichmann JL, Schoepf UJ, et al. Diagnostic accuracy of coronary CT angiography using 3rd-generation dual-souce CT and automated tube voltage selection:Clinical application in a non-obese and obese patient population. Eur Radiol 2017;27:2298–308. [DOI] [PubMed] [Google Scholar]
- [20].Zhu XM, Zhu YS, Xu H, et al. Dual-source CT coronary angiography involving injection protocol with iodine load tailored to patient body weight and body mass index: estimation of optimal contrast material dose. Acta Radiol 2013;54:149–55. [DOI] [PubMed] [Google Scholar]
- [21].Sabarudin A, Sun ZH, Ng KH. Coronary computed tomography angiography with prospective electrocardiography triggering: asystematic review of inage quality and radiation dose. Singapore Med J 2013;54:15–23. [DOI] [PubMed] [Google Scholar]
- [22].Abdulla J, Pederen KS, Budoff M, et al. Influence of coronary calcification on the diagnostic accuracy of 64-slice computed tomography coronary angiography: a systematic review and meta-analysis. Int J Cardiovasc Imaging 2012;28:943–53. [DOI] [PubMed] [Google Scholar]
- [23].Ahn SJ, Kang DK, Sun JS, et al. Accuracy and predictive value of coronary computed tomography angiography for the detection of obstructive coronary heart disease in patients with and Agaston calcium score above 400. J Comput Assist Tomogr 2013;37:387–94. [DOI] [PubMed] [Google Scholar]
- [24].Wang R, Schoepf UJ, Wu RZ, et al. Diagnostic accuracy of coronary CT angiography: comparison of filtered back projection and iterative reconstruction with different strengths. J Comput Assist Tomogr 2014;38:179–84. [DOI] [PubMed] [Google Scholar]
- [25].Scheffel H, Stolzmann P, Scheffel CL, et al. Coronary artery plaques: cardiac CT with model-based and adaptive-statistical iterative reconstruction technique. Eur Radiol 2012;81:e363–9. [DOI] [PubMed] [Google Scholar]


