Abstract
Background:
Acupuncture is widely used for postherpetic neuralgia (PHN) in China but its effect is unclear. We aim to evaluate the effect and safety of acupuncture for PHN.
Methods:
The Cochrane Skin Group Trials Register, The Cochrane Central Register of Controlled Trials, MEDLINE, Embase, the Chinese Biomedical Literature Database, the China National Knowledge Infrastructure, and the gray literature were searched. Randomized controlled trials (RCTs) comparing acupuncture alone versus no treatment/another active therapy/sham acupuncture, or comparing acupuncture with another active therapy versus the same active therapy were included.
Results:
Seven RCTs comparing acupuncture versus pharmacologic therapy were included. Meta-analysis was conducted for acupuncture's effect on PHN evaluating by pain intensity. Results from 2 RCTs showed that compared with pharmacologic therapy, acupuncture was better in decreasing the pain intensity measured by visual analog scale score (mean difference: 1.80, 95% confidence interval 1.72–1.87; P < .001). The limitations of the study are as follows: only trials comparing acupuncture versus pharmacologic therapy were included and all of the included trials were performed in China.
Conclusion:
There was not enough evidence to suggest that acupuncture was superior to pharmacologic therapy in improving global impression or life quality. No adverse effects about acupuncture were reported. In all, acupuncture is safe and might be effective in pain relieving for patients with PHN. Given the low quality of included studies, the results are not conclusive and more large-scale RCTs with high quality are needed.
Keywords: acupuncture, meta-analysis, postherpetic neuralgia, systematic review
1. Introduction
Definition of postherpetic neuralgia (PHN) varies worldwide. In most countries and areas, it refers to a persistence of pain at the site of the skin lesions and is usually defined as pain persisting for over 3 or 4 months after rash healing.[1,2] In China, PHN usually refers to pain persistence for over 3 months after herpes zoster (HZ).[3]
The risk factors for PHN include prodromal pain, severe acute pain, severe rash, and ophthalmic involvement. Besides, older age is significantly associated with the incidence of PHN.[4] It is estimated that 10% to 15% of patients who have shingles will experience PHN.[5] But among patients older than 50 years, the incidence of PHN could reach 83%.[6]
The PHN has serious impact on the patients’ general health, psychologic health, and social and economic well-being.[7] It is the most common complication following acute HZ and has been called the most feared complication.[8] It has been considered a health care problem for its severity and chronicity.[9]
The PHN is often refractory to treatment.[5] First-line treatments for PHN include tricyclic antidepressants, gabapentin and pregabalin, and the topical lidocaine 5% patch. Opioids, tramadol, capsaicin cream, and the capsaicin 8% patch are recommended as either second- or third-line therapies in different guidelines.[2] But these pharmacologic therapies could bring a high incidence of adverse events, such as sedation, xerostomia, confusion, dysrhythmia, weight gain, dizziness, somnolence, fatigue, and ataxia.[10–12] Most important of all, the effectiveness of pharmacologic therapies is limited[13] with the satisfactory analgesia to only approximately 50% patients.[14] More effective pain management are needed.[15]
In Traditional Chinese Medicine (TCM), HZ is called snake strand score for its wriggly appearance. The recordings about HZ could be seen in the books more than 1000 years ago and from that time Chinese began to treat this disease with herb or acupuncture. Many acupuncture methods have been used to relieve the pain after HZ, such as fire needle, auricular needle, bloodletting, cupping, warm needling, etc. An English guideline of acupuncture for HZ has been published in 2013, in which various acupuncture methods for HZ and PHN have been introduced in detail and recommended.[3] Though many clinical trials showed that the pain could be relived effectively by acupuncture for patients with PHN, there were only 3 reviews on needling for PHN published in Chinese. One is a literature review.[16] One[17] reviewed the effect of fire needle for PHN. In this review including 9 randomized controlled trials (RCTs), 5 trials compared fire needle versus another kind of acupuncture method. Of the other 4 trials, 1 trial[18] compared fire needle plus point injection versus ibuprofen codeinetablets, 1 trial[19] compared fire needle and an oral medicine versus point injection, and the other 2 trials[20,21] included patients in or just after the acute stage of HZ. None of the 9 trials meet our inclusion criteria and we do not think the review used a reasonable methodology as well. The other review[22] only collected information about Jiaji points combined with surrounding needling for PHN and had the same methodologic problems. Thus, the effect and safety of acupuncture for PHN is unclear till now.
Our systematic review aimed to rigorously evaluate the effect and safety of acupuncture for PHN. The protocol[23] of this review has been registered on PROSPERO (http://www.crd.york.ac.uk/PROSPERO) and the ID is CRD42014009555.
2. Method
2.1. Study selection
2.1.1. Search terms
We searched registered trials in The Cochrane Skin Group Trials Register and The Cochrane Central Register of Controlled Trials (from inception to October 30, 2017), and all journal articles in MEDLINE, Embase, the Chinese Biomedical Literature Database (CBM), and the China National Knowledge Infrastructure (CNKI) (from inceptions to October 30, 2017).
For the gray literature, the New York Academy of Medicine Grey Literature Report (www.greylit.org), the Electronic Theses Online Service through the British Library (http://ethos.bl.uk), and the academic dissertation databases and conference paper databases in CBM and CNKI.
The search strategy used both subject heading and keywords. The search terms used were grouped using the condition (“PHN” or “postherpetic neuralgia” or “herpes zoster” or “shingles”) and intervention (“acupuncture” or “needle” or “needling” or “electro-acupuncture” or “cupping” or “moxibustion” or “pricking” or “pyonex” or “bloodletting”). The search strategy was used as follows:
-
1.
Randomized controlled trial
-
2.
Controlled clinical trial
-
3.
Randomized
-
4.
Placebo
-
5.
Trial
-
6.
1 or 2 to 6
-
7.
PHN
-
8.
Postherpetic neuralgia
-
9.
Herpes zoster
-
10.
Shingles
-
11.
7 or 8 to 10
-
12.
Acupuncture
-
13.
Needle
-
14.
Needling
-
15.
Cupping
-
16.
Moxibustion
-
17.
Pricking
-
18.
Pyonex
-
19.
Bloodletting
-
20.
Electroacupuncture
-
21.
12 or 13 to 20
2.1.2. Inclusion and exclusion criteria
We included studies based on our review protocol published in 2014 and preliminary searches. Studies were eligible if they were randomized controlled trials, included participants with PHN (pain persisting for 3 months after the onset of the rash), compared acupuncture versus another active therapy or no intervention or sham/placebo acupuncture, or compared acupuncture with another active therapy versus the same active therapy.
Studies were omitted if they compared one acupuncture method versus another kind of acupuncture method or inactive treatment, for example, the herbal decoction. Though acupuncture usually refers to inserting needles into the skin, the therapy here is defined as the traditional Chinese acupuncture methods, including body acupuncture, scalp acupuncture, electroacupuncture, pyonex, cupping, bloodletting, moxibustion, warm needling, etc. Studies were excluded if they evaluated the effect of laser needle and hydro-acupuncture therapy; for these, interventions are not traditional Chinese acupuncture methods.
The primary outcome measure was the change of pain intensity from the baseline, measured by visual analog scale (VAS), numerical rating scale (NRS), McGill pain score, or other rating scales. Secondary outcomes included life quality measures, patients reported outcomes, safety measures, and global impression (the number of participants whose symptoms improved after treatment).
2.2. Data extraction
Two review authors (YW and WL) extracted data independently using a standard form containing prespecified outcomes. Data had been collected but not reported would be clarified from the trial authors. The titles and abstracts of all identified articles were screened first. Full text of articles which needed to be assessed further was retrieved. Differences of opinions were discussed or consulted with a third review author (ZL). The included trial data were processed according to the Cochrane Handbook for Systematic Review of Interventions.[24]
2.3. Assessment of risk of bias in included studies
The Cochrane Collaboration's “Risk of Bias” tool[24] was used to assess methodologic quality of the included studies by 2 review authors (WP and JZ) independently. Six domains of bias were considered as follows: sequence generation, allocation concealment, blinding (or masks), incomplete data assessment, selective outcome reporting, and other sources of bias. The funnel plot would be used to assess the reporting bias if more than 10 trials were included.
2.4. Data analysis
Analyses were conducted based on available data from the included studies relevant to the comparisons and outcomes. For missing data, the trial authors were contacted. If the original data could not be offered, the analysis would be based on the available data. The meta-analysis was conducted with the Revman 5.3 software. To estimate the heterogeneity, the Chi-squared test was used and the I2 statistic over 50% showed the existence of heterogeneity.
For the primary outcome (pain intensity), the mean difference (MD) with 95% confidence interval (CI) was calculated with mean and standard deviation. For the secondary outcomes (life quality measures, patient reported outcomes, and safety measures), MD with 95% CI was calculated for the continuous variables, and the risk ratio with 95% CI was calculated for the dichotomous variables. The fixed-effect model was used, if there was no heterogeneity. Otherwise, we used a random-effect model. We have no prespecified plan of sensitivity analysis or subgroup analysis. Sensitivity analysis would be conducted to explore the impact of deviations to the findings if necessary.
All analyses were based on previous published studies, no ethical approval and patient consent are required.
3. Results
3.1. Study selection
The initial search identified 752 studies, and 692 records were identified after duplicates were removed. Of the 692 studies, 672 studies were excluded by reading the titles and abstracts because they were not randomized controlled trials or the duration was <3 months after the onset of HZ or they compared acupuncture with other therapy versus a third therapy. Full texts of 20 possibly eligible studies were assessed and 13 studies were excluded (Table 1) and 7 studies (Table 2) were included finally.
Table 1.
Characteristics of excluded studies.
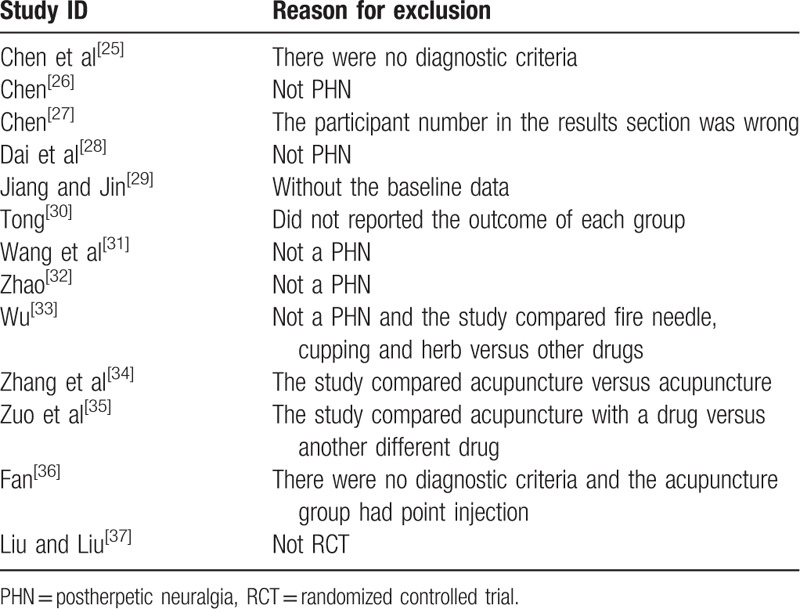
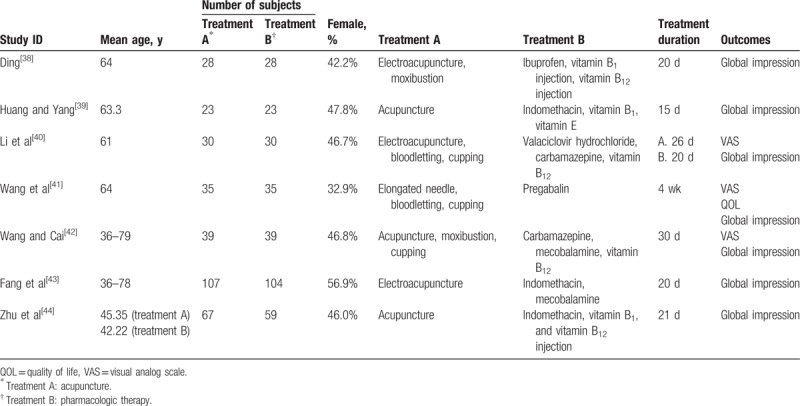
Table 2.
Characteristics of included studies.
3.2. Study description
Seven trials were included at last and all studies were performed in China and were published in Chinese.[38–44] The 7 trials were single-center randomized controlled studies without follow-up period. The duration of the intervention was ranged from 15 to 30 days.
3.2.1. Participants
The 7 included trials involved 647 participants in total, including 332 males and 315 females. All of the participants were included in the statistical analysis.
3.2.2. Intervention
Three trials used 3 acupuncture methods (elongated needle and bloodletting and cupping,[22] electroacupuncture and bloodletting and cupping,[21] body acupuncture and the plum needle and cupping[40]). Three trials used 1 acupuncture method alone[39,43,44] and another trail[38] used the combination of electroacupuncture and moxibustion. All studies compared acupuncture with pharmacologic therapy.
3.2.3. Outcomes
3.2.3.1. Primary outcome
The primary outcome was assessed in 3 studies.[40–42] They only reported the VAS score at baseline and after treatment. The VAS score change from baseline after treatment was calculated using the formula recommended by the Cochrane Handbook[24]:
3.2.3.2. Secondary outcomes
For the secondary outcomes (the life quality, patient reported outcomes, safety, and global impression), 1 study[41] assessed the subscale of the WHOQOL-100 scale, 2 studies[38,44] reported treat-related adverse events, and no studies described patient reported outcomes. All of the 7 studies reported the global impression (numbers of participants improved in pain intensity).
3.2.4. Risk of bias within studies
Two reviewers (WL and JZ) used the Risk of Bias tool recommended by the Cochrane Handbook to evaluate the quality of the included studies. When there were disagreements, the third reviewer was consulted. Only 2 trials[41,42] reported the random sequence generation method (the random number table). Five studies did not report the random sequence generation method and all 7 included studies did not report the allocation concealment, which resulted to an unclear risk. As the included studies focused on acupuncture, blinding of the acupuncturists was not possible. But all 7 studies did not blind the participants or outcome assessors either. We rated all the 7 studies as having a high risk in this domain. Of the 7 trials, no withdrawals or dropouts were reported and we found no selective reporting. No trials reported the sample size calculation. The risk of bias summary table is presented in Figure 1.
Figure 1.
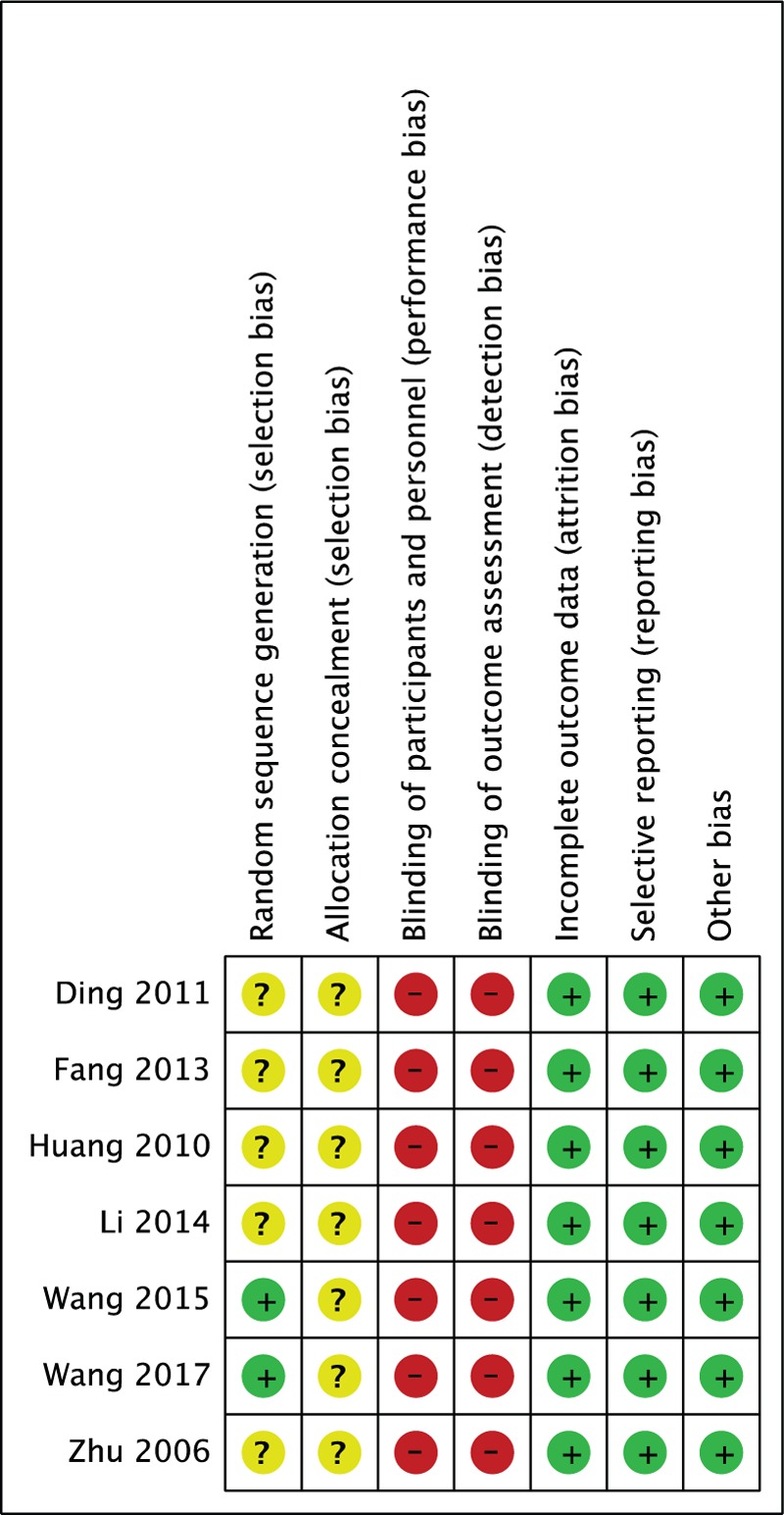
Risk of bias summary.
3.3. Effects of interventions
There were no trials comparing acupuncture versus no intervention or placebo/sham acupuncture, or comparing acupuncture with active therapy versus the same active therapy. All of the 7 included trials compared acupuncture versus pharmacologic therapy.
3.3.1. Pain intensity
Three studies[40–42] involving 208 participants reported pain intensity measured by VAS score. One[40] compared electroacupuncture, bloodletting and cupping versus valaciclovir hydrochloride, carbamazepine and vitamin B12. One study[41] compared elongated needle, bloodletting and cupping versus pregabalin. And another study[42] compared body acupuncture, plum needle and cupping versus carbamazepine, mecobalamine and vitamin B12. Acupuncture seemed to be better in relieving pain than pharmacologic therapy with a significant difference (MD: 2.09, 95% CI 1.19–2.98; P < .001). But the heterogeneity was high (I2 = 88%, P = .0003) was high (Fig. 2).
Figure 2.
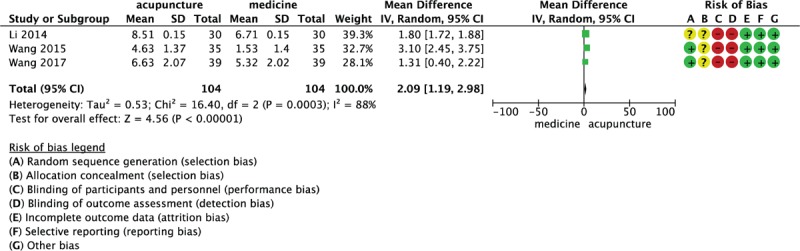
Forest plot of 3 randomized controlled trials comparing acupuncture versus pharmacologic therapy on the visual analog scale score using a random model.
We conducted a sensitivity analysis. When the trial Wang et al[41] was deleted from the analysis, the heterogeneity decreased (I2 = 10%, P = .29). Still, there was significant difference between the acupuncture group and the pharmacologic therapy group (MD: 1.80, 95% CI 1.72–1.87; P < .001) (Fig. 3). The heterogeneity may be come from the control method it (Wang 2015) used. It set pregabalin alone as the control intervention while other included trials all had more than one kind of drugs in the pharmacologic therapy group. The use of pregabalin alone might result in a much smaller decrease of the VAS score in the pharmacologic therapy group compared to other included trials.
Figure 3.
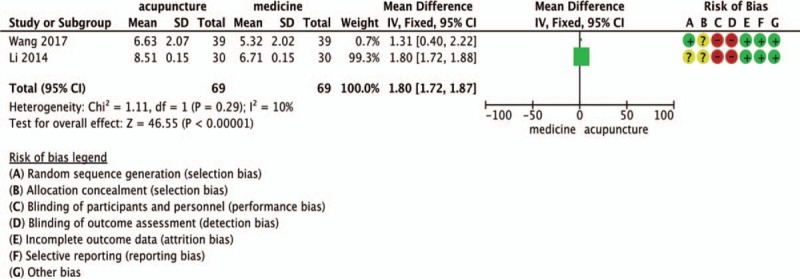
Forest plot of 2 randomized controlled trials comparing acupuncture versus pharmacologic therapy on the visual analog scale score using a fixed model.
3.3.2. Global impression
All of the 7 included trials involved 647 participants reported the number of patients who had improvement in pain intensity after treatment. But the standards for improvement in pain intensity were different among studies. Among the 7 studies, 4 studies[40–43] made their standards according to TCM diagnosis standards (TCM Standards of Diagnosis and Syndrome[45] or The Disease Diagnosis and Improvement Standards[46]) and considered over 20% reduction[43] in VAS score or obvious pain reduction[40] or any pain reduction[41,42] as effective. One study[39] considered any reduction in VAS score as effective, 1 study[38] considered over 30% improvement in VAS score as effective and the other one[44] considered ≥2 points reduction in VAS score as effective.
The TCM diagnosis and treatment standards were not quantified standards. Words used to describe the standards were like “pain relieving obviously was considered effective” or “any pain relieving after treatment was considered effective.” Actually, it was not clear how much the pain intensity was improved for each participant among studies. Hence, the results of 4 trials[40–43] based on those TCM standards could not be combined and analyzed. For Huang and Yang,[39] setting any reduction in VAS score as a standard was groundless. According to the China Consensus on the PHN[47] and the study conducted by Tamara,[48] over 30% reduction in VAS score or a at least 2-point reduction in VAS score was considered of clinical significance. So, it was reasonable for Ding[38] and Zhu et al[44] reporting the number of participants with over 30% improvement and a at least 2-point reduction in VAS score, respectively. The responder rate in the acupuncture and pharmacologic groups of the 2 trials was 100% and 85.7%, respectively, in Ding and 83.6% and 66.1%, respectively, in Zhu et al. Significant difference between the acupuncture group and the pharmacologic therapy group was reported in both the 2 trials, but the value of between-group difference was not described.
3.3.3. The QOL scale
Only 1 trial[41] involving 70 participants reported this outcome. The trial compared the elongated needle, bloodletting and cupping versus pregabalin. The authors chose 6 items relevant to pain to evaluate the life quality of participants. And participants of the acupuncture group seemed to be improved better than those in the pharmacologic therapy group (MD: 3.78, 95% CI 2.59–4.97; P < .001).
3.3.4. Safety issue
In the 7 included studies, 2 studies reported stomach discomforts in the pharmacologic therapy group in 5 cases[38] (ibuprofen, vitamin B1 injection, and vitamin B12 injection, 28 subjects) and 8 cases[44] (indomethacin, vitamin B1 injection, and vitamin B12 injection, 59 subjects), respectively. No adverse effects were reported in the acupuncture group.
4. Discussion
In this review, we identified 7 studies and synthesized information from 2 studies. There were no studies comparing acupuncture versus no intervention or placebo/sham acupuncture, so the specific effect of acupuncture for PHN was not clear. And there were no trials comparing acupuncture with an active therapy versus the same active therapy, whether acupuncture could work as an adjuvant therapy to reinforce the effect of other active therapy was not clear either. All of the 7 included trials compared acupuncture versus pharmacologic therapy. The pharmacologic therapy used included the α2-δ ligand pregabalin, the antiviral agent valaciclovir hydrochloride, the anticonvulsant carbamazepine, and vitamin B. The results showed that compared with the pharmacologic therapy, acupuncture might be better at decreasing the pain intensity measured by VAS score. But the methodologic quality of included studies was very low.
Of the 7 included studies, 3 studies[40–42] reported pain intensity measured by VAS score. Two trials[40,42] were finally included in the meta-analysis with a low heterogeneity (I2 = 10%), and the results favored acupuncture (MD: 1.80, 95% CI 1.72–1.87; P < .001) compared with pharmalogic therapy (valaciclovir hydrochloride, carbamazepine, mecobalamine, and vitamin B12). For the outcome of global impression, all 7 studies reported number of participants with symptom improved. Given the nonquantitative and different responder rate standards adopted in the 7 trials, it was difficult to combine and analyze the information in a meta-analysis. Though the standards were reasonable in Zhu et al and Ding and their results favored acupuncture in an effective rate, more trials were needed to support the conclusion. For the outcome of life quality, only 1 study[41] with 70 participants reported the QOL score, elongated needle and bloodletting seemed to result in a higher improvement in QOL score compared to pregabalin. Two trials[38,44] reported stomach discomfort in the pharmacologic therapy group in 5 and 8 cases, respectively, and no trials reported the adverse effects of acupuncture.
In the 7 included RCTs, the sample sizes ranged from 46 to 211 and the treatment durations were from 15 to 30 days. Three trials[39,43,44] used 1 acupuncture method, 1 trial[38] used 2, and the other 3 trials[40–42] used 3 acupuncture methods as a combination. Two trials[41,42] reported using a random number table to generate the randomized sequence and all of the 7 trials did not report randomization concealment. As no included trials conducted sample size calculation, it was not sure whether there was enough power to detect the between-group difference. And the lack of blinding of the participants and outcome assessor might result in bias in the outcomes. The quality of those studies was low and the risk of bias was relatively high. In the trial performed by Li et al,[40] the treatment durations of the acupuncture group (26 days) and pharmacologic therapy group (20 days) were different. We conducted a sensitivity analysis, the P-value was the same before and after deleting the trial. So, the trial was included at last.
Three reviews published in Chinese existed before. Beside of methodologic defects, they only reviewed 1 or 2 certain acupuncture methods for PHN. Compared with the 3 existed reviews,[16,17,22] our study conducted a wider search. It screened all kinds of acupuncture methods and comparators, not only fire needle or Jiaji points. We adopted strict inclusion criteria, exclusion criteria, and recognized tool to evaluate the quality of included studies, and a meta-analysis was performed. Though the quality of the included studies was low, the existing evidence of acupuncture for PHN was systematically reviewed and analyzed.
The limitation about this review mainly came from the included studies. First, as there were many methodologic defects in the included studies, we must be careful in terms of the results explanation. Second, there were no studies comparing acupuncture versus no intervention or sham acupuncture, the specific effect of acupuncture could not be explored. Third, all the included studies were conducted in China, it was not sure whether the results were the same for participants in areas beyond China. And the acupuncture methods used in included trials are complex. Limited by the number of RCTs included in this review, it is difficult to conduct subgroup analysis according to different types of acupuncture method. But the results may change with the conducting of more trials.
5. Conclusion
Acupuncture is safe, but its effect in pain relieving for PHN was not conclusive given the methodologic defects in the included studies. For the life quality and global impression, the available data were too few to suggest that acupuncture is useful. More large-scale, high-quality RCTs are needed. Trials with sham/placebo acupuncture or blank control should be conducted to detect whether the effect of acupuncture is the specific effect or the placebo effect.
Author contributions
Investigation: Zhishun Liu.
Methodology: Yang Wang, Wang Li, Weina Peng, Jing Zhou, Zhishun Liu.
Validation: Zhishun Liu.
Visualization: Zhishun Liu.
Writing – original draft: Yang Wang, Weina Peng.
Writing – review & editing: Yang Wang, Wang Li, Jing Zhou, Zhishun Liu.
Footnotes
Abbreviations: CBM = the Chinese Biomedical Literature Database, CI = confidence interval, CNKI = the China National Knowledge Infrastructure, HZ = herpes zoster, MD = mean difference, NRS = numerical rating scale, PHN = postherpetic neuralgia, RCT = randomized controlled trial, TCM = Traditional Chinese Medicine, TSQM = the Treatment Satisfaction with Medication Questionnaire, VAS = visual analog scale.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Wang J, Zhu Y. Different doses of gabapentin formulations for postherpetic neuralgia: a systematical review and meta-analysis of randomized controlled trials. J Dermatol Treat 2017;28:65–77. [DOI] [PubMed] [Google Scholar]
- [2].Argoff CE. Review of current guidelines on the care of postherpetic neuralgia. Postgrad Med 2011;123:134–42. [DOI] [PubMed] [Google Scholar]
- [3].Liu ZS, Peng WN, Liu BY, et al. Clinical practice guideline of acupuncture for herpes zoster. Chin J Integr Med 2013;19:58–67. [DOI] [PubMed] [Google Scholar]
- [4].Forbes HJ, Thomas SL, Smeeth L, et al. A systematic review and meta-analysis of risk factors for postherpetic neuralgia. Pain 2016;151:30–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].FDA. FDA Approves New Drug Treatment for Long-Term Pain Relief After Shingles Attacks. Silver Spring, MD: U S Food and Drug Administration (FDA); 2009. [Google Scholar]
- [6].Yawn BP, Saddier P, Wollan PC, et al. A population-based study of the incidence and complication rates of herpes zoster before zoster vaccine introduction. Mayo Clin Proc 2007;82:1341–9. [DOI] [PubMed] [Google Scholar]
- [7].NICE. NICE clinical guideline. Neuropathic pain: the pharmacological management of neuropathic pain in adults in non-specialist settings. National Institute for Health and Clinical Excellence. Available at: http://www.nice.org.uk/guidance/CG96. Accessed June 5, 2010. [Google Scholar]
- [8].Hanania MM, Brietstein D. Postherpetic neuralgia: a review. Cancer Invest 1997;15:165–7. [DOI] [PubMed] [Google Scholar]
- [9].Baron R, Wasner G. Prevention and treatment of postherpetic neuralgia. Lancet 2006;367:186–8. [DOI] [PubMed] [Google Scholar]
- [10].Friesen KJ, Falk J, Alessi-Severini S, et al. Price of pain: population-based cohort burden of disease analysis of medication cost of herpes zoster and postherpetic neuralgia. J Pain Res 2016;9:543–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Christo PJ, Hobelmann G, Maine DN. Post-herpetic neuralgia in older adults. Drugs Aging 2007;24:1–9. [DOI] [PubMed] [Google Scholar]
- [12].Rowbotham M, Harden N, Stacey B, et al. Gabapentin for the treatment of postherpetic neuralgia: a randomized controlled trial. JAMA 1998;280:1837–42. [DOI] [PubMed] [Google Scholar]
- [13].Rice AS, Maton S. Postherpetic Neuralgia Study Group. Gabapentin in postherpetic neuralgia: a randomised, double blind, placebo controlled study. Pain 2001;94:215–24. [DOI] [PubMed] [Google Scholar]
- [14].Goßrau G. Postherpetic neuralgia. Schmerz 2014;28:93–102. [DOI] [PubMed] [Google Scholar]
- [15].Van SR, Sadosky A, Lucero M, et al. A cross-sectional survey of health state impairment and treatment patterns in patients with postherpetic neuralgia. Age Ageing 2006;35:132–7. [DOI] [PubMed] [Google Scholar]
- [16].Qin L, Fu Y. Literature review on acupuncture for PHN [in Chinese]. Henan Tradit Chin Med 2012;32:250–2. [Google Scholar]
- [17].Ou D, Zhou C. System evaluation of RCT systematic about the treatment of postherpetic neuralgia by using fire needle. Clin J Tradit Chin Med 2015;27:115–9. [Google Scholar]
- [18].Li Z. Observation of the fire needle and point injection for PHN. Guide J Tradit Chin Med Pharmacol 2013;19:63–4. [Google Scholar]
- [19].Liu P. The effect of fire needle and gastrodin for PHN. J Guiyang Coll Tradit Chin Med 2008;18:2–3. [Google Scholar]
- [20].Nie B, Ma X. Evaluation of the half needling with fire needle for herpes zoster. J Jiangxi Univ TCM 2006;18:38–9. [Google Scholar]
- [21].Ma X, Li J, Jiang Y. The fire needle and cupping and body acupuncture for PHN. JETCM 2011;19:1864–5. [Google Scholar]
- [22].Zhu Y, Zhu L, Li Y, et al. Jiaji points combined with surrounding needling for the treatment of postherpetic neuralgia: a meta-analysis. J Clin Rehab Tiss Eng Res 2011;15:2064–8. [Google Scholar]
- [23].Li W, Peng W, Zhou J, et al. Acupuncture for postherpetic neuralgia: a systematic review protocol. BMJ Open 2014;4:e005725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available at: www.cochrane-handbook.org. [accessed on 11.25.2016]. [Google Scholar]
- [25].Chen J, Zhang Z, Tong J. Clinical observation of effect of fire needle in treating neuralgia due to herpes zoster. Mod Hosp 2007;7:78–9. [Google Scholar]
- [26].Chen Y. Observation on acupuncture for 40 cases of PHN. Chin J Prim Med Pharm 2011;18:79–80. [Google Scholar]
- [27].Chen Y. The clinical observation on fire needle combine cobamamide in treating post-herpetic neuralgia. Chin Manipul Rehabilit Med 2013;4:66–7. [Google Scholar]
- [28].Dai J, Zhang L, Su X, et al. Observation of acupuncture and cupping on PHN. J Chengdu Coll 2012;7:75–6. [Google Scholar]
- [29].Jiang X, Jin Z. Observation of herb on PHN strengthening by scalp acupuncture. Hubei J Tradit Chin Med 2013;35:58–9. [Google Scholar]
- [30].Tong B. The fire acupuncture on 30 cases of PHN. Capital Med 2014;16:68. [Google Scholar]
- [31].Wang H, Xie Z, Feng J. Gabapentin and acupuncture for PHN. Chin J Gonvalescent Med 2014;23:130–1. [Google Scholar]
- [32].Zhao R. The bloodletting therapy for 30 cases of PHN. Shanexi J Tradit Chin Med 2011;32:595–7. [Google Scholar]
- [33].Wu A. Observation of acupuncture and herb for PHN. China Naturopathy 2017;25:57–8. [Google Scholar]
- [34].Zhang Y, Peng Y, He N. Observation of fire needle and bloodletting for PHN. J Sichuan Tradit Chin Med 2014;33:165–7. [Google Scholar]
- [35].Zuo X, Wang Z, Cui W, et al. Clinical effect of skin needle stabbing combined with blood - letting puncture and cupping for the treatment of neuralgia caused by herpes zoster. J Clin Acupunct Moxibust 2015;31:20–2. [Google Scholar]
- [36].Fan L. Pyonex and point injection for PHN. Contemp Med 2016;22:156–7. [Google Scholar]
- [37].Liu G, Liu C. Treatment of 68 cases of shingles by puncturing collateral plus cupping. J Acupunct Tuina Sci 2003;1:11. [Google Scholar]
- [38].Ding X. Observation about the clinical effect of electro-acupuncture combined with moxibustion on the 56 patients with post herpetic neuralga (PHN) of herpes zoster. J China Tradit Chin Med Info 2011;2:40–1. [Google Scholar]
- [39].Huang X, Yang B. Effect of acupuncture for 23 cases of PHN. J Clin Acupunct Moxibust 2010;26:22–3. [Google Scholar]
- [40].Li W, Cai G, Wang Y. Clinical observation of 30 cases of PHN with electroacupuncture and bloodletting. Mod Diagn Treat 2014;25:1506–7. [Google Scholar]
- [41].Wang X, Zhang F, Xu A. Observation of elongated needle and bloodletting for PHN. J Pract Tradit Chin Med 2015;31:943–4. [Google Scholar]
- [42].Wang M, Cai S. Clinical observation of acupuncture combined with plum blossom tapping and cupping treatment to shingles neuralgia. J Shanxi Univ Chin Med 2017;40:58–66. [Google Scholar]
- [43].Fang X, Han L, Wu H. Effect of electroacupuncture on PHN. Military Surg 2013;56:1427–8. [Google Scholar]
- [44].Zhu M, Kuang L, Yang H, et al. Observation on 126 cases of PHN with acupuncture. J TCM Univ Hunan 2006;26:52–3. [Google Scholar]
- [45].State Administration of Traditional Chinese Medicine of the People's Republic of China. The TCM Standards of Diagnosis and Syndrome. 1994;Nanjing: Nanjing University Press, 144. [Google Scholar]
- [46].Ministry of Science and Technology of the People's Republic of China. The Disease Diagnosis and Improvement Standard. 1998;Beijing: People's Military Medical Press, 281. [Google Scholar]
- [47].The PHN Consensus Group. The China consensus on diagnosis and treatment for postherpetic neuralgia. Chin J Pain Med 2016;22: 161–167. [Google Scholar]
- [48].Ursini T, Tontodonati M, Manzoli L, et al. Acupuncture for the treatment of severe acute pain in herpes zoster: results of a nested, open-label, randomized trial in the VZV pain study. BMC Complement Altern Med 2011;11:46. [DOI] [PMC free article] [PubMed] [Google Scholar]


