Supplemental Digital Content is available in the text
Keywords: body fat, cutoff points, lipids, prehypertension, receiving operating characteristic analysis
Abstract
Recently, prehypertension has been considered as a risk factor for cardiovascular disease because it can progress to hypertension. The association between obesity and dyslipidemia with raised blood pressure has been reported in some studies; however, the ability of indicators of such conditions to predict prehypertension has been scarcely explored. In this cross-sectional study, we compared the ability of indicators of accumulated and circulating fat to discriminate between prehypertensive and normotensive Mexico City residents (n = 1377). The indicators were classified based on the parameters needed for their calculation: including only circulating fat (IOCFi) (e.g., Castelli risk indexes), including only accumulated fat (IOAFi) (e.g., waist circumference [WC]), and mixed (e.g., lipid accumulation product [LAP]). We compared the areas under the receiving operating characteristic curves (AURCs) and estimated the cutoff points for each indicator and their associated risk of prehypertension. The IOAFi had the greatest AURCs, followed by mixed and IOCFi; the AURCs for WC were the highest (AURC = 0.688 and 0.666 for women and men, respectively). The highest odds ratios for prehypertension were those associated with the cutoff points for IOAFi and LAP (e.g., OR = 2.8 for women with WC > 83.5 cm and OR = 2.6 for men with WC > 87.5 cm). Early detecting people at risk of cardiovascular disease is a necessity and given that WC had a better performance than the other indexes and it is relatively easy to measure, it has the potential of being used as a complementary measure in routine clinical examinations and by the general population as an auto-screening measurement to detect prehypertension.
1. Introduction
Raised blood pressure is a major risk factor for cardiovascular disease (CVD) and it is estimated to account for 7.5 million deaths worldwide, with prevalence rates over 40% in people older than 25 years.[1] It is known that prehypertension is very likely to progress to hypertension and, consequently, can increase the probabilities of developing CVD[2,3]; in fact, the Strong Heart Study identified that 38% of prehypertensive people developed hypertension,[2] and a recent meta-analysis showed that prehypertension is associated with CVD mortality.[4] The estimated worldwide prevalence of prehypertension in adults is 25% to 50%,[5] while in Mexico is 37.5%.[6]
Both obesity and dyslipidemia (in other words, accumulated and circulating fat) have been associated with the presence of prehypertension, hypertension, and increased cardiovascular risk[7,8]; indeed, prehypertension is more prevalent in people with dyslipidemia[9] and obesity.[10] Different body-fat-related measurements and indexes are currently used as indicators of cardiovascular risk and some of them have been tested as predictors of hypertension or prehypertension.[11–14] Some of the indicators consider only circulating fat, that is, Castelli risk indexes 1 and 2, and atherogenic index of plasma (AIP), while others involve body-composition-related measurements, such as waist circumference (WC), waist to height ratio (WtHR), and body mass index (BMI).[15] Furthermore, in recent years, a variety of indexes combining anthropometric measurements and lipid profile have emerged: lipid accumulation product (LAP) and visceral adiposity index (VAI) among them[16,17]; however, in the clinical practice, AIP and Castelli index 1 continue to be the most used indicators of cardiovascular risk.[18]
Some studies have shown that prehypertension is associated with a variety of cardiovascular alterations, such as impaired cardiac structure and function and reduced nitric-oxide-dependent vasodilation.[19,20] Preventing the onset of CVD is a worldwide priority[21] and the earlier preventive strategies are implemented the greater their impact on health is expected. Because diagnosis of hypertension frequently occurs at advanced stages of the disease,[22] it is necessary to identify the individuals at risk as soon as possible, for instance, those with prehypertension. The aim of this study was to compare several indicators of circulating and/or accumulated fat regarding its ability to discriminate between normotensive and prehypertensive men and women living in Mexico City, to detect the indicator(s) that better associates with such condition. Additionally, we also estimated cutoff points for prehypertension for each of the indicators and the odds ratios (ORs) of prehypertension considering those values.
2. Methods
2.1. Volunteers
Participants were clinically healthy volunteers recruited for the Tlalpan 2020 cohort from September 2014 to August 2016. Tlalpan 2020 is a longitudinal study aimed to evaluate the impact of traditional and nontraditional risk factors on hypertension incidence in a population of Mexico City. Study design, methods, and selection criteria for the Tlalpan 2020 cohort were described in detail elsewhere.[23] Overall, people from all the municipalities of Mexico City were invited to participate through massive dissemination methods, such as social networks (Facebook and Twitter), radio, television, and distribution of brochures and posters in health, community, work, and cultural centers and schools. Participants were women and men aged 20 to 50 years, living in Mexico City, and not suffering from hypertension. People previously diagnosed with diabetes mellitus, dysthyroidism, cerebrovascular disease, ischemic cardiopathy, acute coronary syndrome, or cancer with an effect on survival, as well as pregnant women, people taking antihypertensive medication or those with mental and cognitive disabilities were excluded. For the purpose of this cross-sectional analysis, among recruited participants, those who had no complete baseline data or were taking lipid-lowering medication at baseline were excluded from this analysis. All participants were informed about the procedures reported here and signed the respective informed consent. The Tlalpan 2020 study follows the principles of the declaration of Helsinki and was approved by the Institutional Bioethics Committee of the Instituto Nacional de Cardiología Ignacio Chávez (National Institute of Cardiology Ignacio Chavez) under number 13-802.
Participants included in the analysis were classified according to their blood pressure measurements (Section 2.2) in 2 groups: normotensive and prehypertensive.
Information regarding smoking habit and alcohol consumption was recorded. Participants who reported to have smoked 100 or more cigarettes in their lifetime and, additionally, smoked daily or some days at the time of the survey, were classified as current smokers.[24] People who, at the time of survey, reported to consume alcohol regardless of frequency, were classified as current alcohol consumers.
Also, the long version (7 days) of the International Physical Activity Questionnaire (IPAQ)[25] was applied to participants to assess physical activity. A categorical indicator of physical activity was obtained, classifying it as low, moderate, and high, according to the criteria of the IPAQ working group.
2.2. Blood pressure assessment
Before starting blood pressure measurement, participants were asked to remain seated for at least 10 minutes. Blood pressure was measured 3 times with a 3-minute interval between each measurement and the average of them was recorded. A cuff whose size was suitable for the arm of each participant and a mercury sphygmomanometer (empire N; Riester, Jungingen, Germany), previously calibrated at our institution, were used. Participants were excluded from the cohort when their systolic blood pressure (SBP) was ≥140 mm Hg and/or their diastolic blood pressure (DBP) was ≥90 mm Hg.[26] The rest of participants were classified as prehypertensive when SBP was ≥120 and <140 mm Hg and/or DBP was ≥80 and <90 mm Hg[3]; while participants with SBP < 120 mm Hg and DBP < 80 mm Hg were classified as normotensive.
2.3. Anthropometric measurements
Weight, height, and WC measurements were performed with the patient fasting, shoeless, and wearing a hospital gown in accordance with the International Society for the Advancement of Kinanthropometry (ISAK).[27] Briefly, weight was measured on a mechanic scale (SECA 700), with capacity of 220 kg and precision of 0.05 kg, with the patient placed at the center of the platform, in upright position and the arms freely hanging to the sides. To measure the height on a stadiometer SECA 220, participants were asked to maintain an erect position, with the scapula, buttocks, heels, and back part of the skull projected in the same vertical plane, and head oriented in the plane of Frankfurt. The cursor of the stadiometer was set firmly on the vertex, and the reading was recorded. WC was measured between the last costal arch and the iliac crest, at the narrowest part of the abdomen, by using a measuring tape made of glass fiber Bodyflex, with length of 150 cm.
2.4. Biochemical parameters
Venous blood samples were obtained after an overnight fast of 12 hours. Serum total cholesterol (TC), high-density lipoprotein-cholesterol (HDL-C), low-density lipoprotein-cholesterol (LDL-C), triglycerides (TGs), glucose, creatinine, and uric acid were measured in automatic analyzers at the Central Lab of our institution. Serum lipid levels were used to calculate the indicators described in Section 2.5.
Sodium and potassium excretions were determined in 24-hour urine samples by using the ion-selective electrode method, as a surrogate of sodium and potassium intake. Urinary creatinine was determined by the Jaffe's colorimetric assay to assess the completeness of 24-hour urine samples: only those samples with creatinine excretion standard rates (15–25 mg/kg/24 h for men and 10–20 mg/kg/24 h for women) were considered as complete and used for a sub-analysis (Section 2.6).
2.5. Calculations for lipid and anthropometric indicators
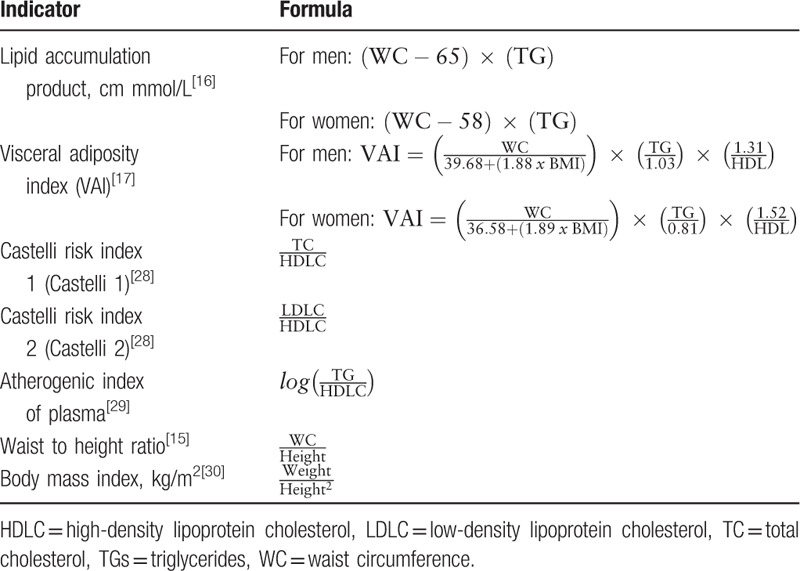
Indicators were grouped according to the elements needed for their calculation: including only circulating fat (IOCFi), including only accumulated fat (IOAFi), and mixed. The IOCFi included Castelli risk index 1 (Castelli 1), Castelli risk index 2 (Castelli 2), and AIP; IOAFi comprised WC, WtHR, and BMI; and mixed indicators included LAP and VAI. Calculations for all these indicators (except for WC) are summarized in Table 1.
Table 1.
Calculations for anthropometric and lipid indicators.
2.6. Statistical analysis
Analysis of variance (ANOVA) was used to compare biochemical, anthropometric, and clinical parameters, between normotensive and prehypertensive men and women, when homogeneity of variances assumption was satisfied, or Kruskall–Wallis when it was not; in both cases, the tests were followed by multiple comparisons with Bonferroni adjustment. Categorical variables were analyzed by Pearson Chi-squared test. Student t test or Mann–Whitney U test, as needed, was used to compare between all men versus all women. Statistical significance was considered when P < .05.
The receiving operating characteristic (ROC) analysis was employed to test the ability of all the indicators (IOCFi, IOAFi, and mixed) to discriminate normotensive from prehypertensive people through the areas under the ROC curve (AURC). A statistically significant discriminatory power was considered when P < .05. The AURCs were also obtained after performing a missing data analysis through the multiple imputation method (5 imputations); such information is displayed in supplementary Tables 1 and 2.
Sensitivity and specificity were retrieved from the statistical package for the social sciences (SPSS) for several possible cutoff points for each parameter to identify the presence of prehypertension; the “best” cutoff point was selected based on the required sensitivity approach,[31] establishing a minimum of 0.80, together with the maximum specificity when sensitivity ≥0.80.
Univariate and multivariate logistic regression analyzes were performed, for men and women separately, to estimate the unadjusted and adjusted OR and 95% confidence interval for the presence of prehypertension associated to each of the studied parameters. To this end, values of each parameter were split at 2 levels: below and above their respective previously identified cutoff point. Estimations were adjusted by age, physical activity, smoking habit and alcohol consumption. An OR was considered statistically significant when P < .05. A sub-analysis with sodium and potassium excretion as covariates was also performed, and it included only those participants who provided complete 24-hour urine samples (supplementary Table 3).
The whole statistical analysis was carried out by using SPSS v. 22 (IBM, Chicago, IL).
3. Results
3.1. General characteristics of participants and blood pressure status
Until August 2016, a total of 1523 persons had been evaluated for eligibility. Seventy-seven people were excluded from the Tlalpan 2020 cohort during their basal visit due to hypertension (4 of them for hypertension combined with diabetes) and 49 for reasons different to hypertension (e.g., diabetes, dysthyroidism, CVD, and other causes). In addition, 7 people had no complete data for this study, and 13 were taking lipid-lowering medication (Fig. 1). Therefore, 1377 people were included in the present study (902 women and 475 men). Seventy-six percent of participants provided a complete 24-hour urine sample (Section 2.4 for criteria) and their data were used for a multiple logistic regression sub-analysis, with sodium and potassium excretion as covariates (supplementary Table 3).
Figure 1.
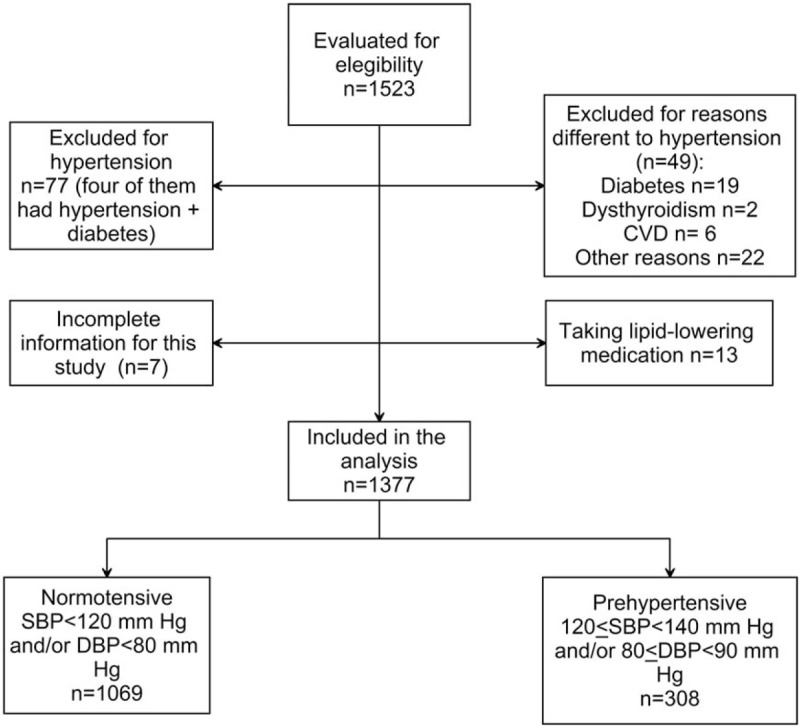
Flow diagram of participants. A total of 1523 participants were evaluated for eligibility and 1377 of them were included in this study. CVD = cardiovascular disease, DBP = diastolic blood pressure, SBP = systolic blood pressure.
Prehypertension was more frequent among men than women, 35% and 16%, respectively. Men were significantly younger than women (Table 2). Prehypertensive people were older and displayed higher values of weight, SBP, and DBP than normotensive ones (Table 2). A significant difference was observed between normotensive men and women for SBP and DBP, while these parameters were not different between prehypertensive men and women. Additionally, it was observed that SBP and DBP were 6% and 7%, respectively, higher in men compared to women.
Table 2.
General characteristics of participants of the study and biochemical parameters.
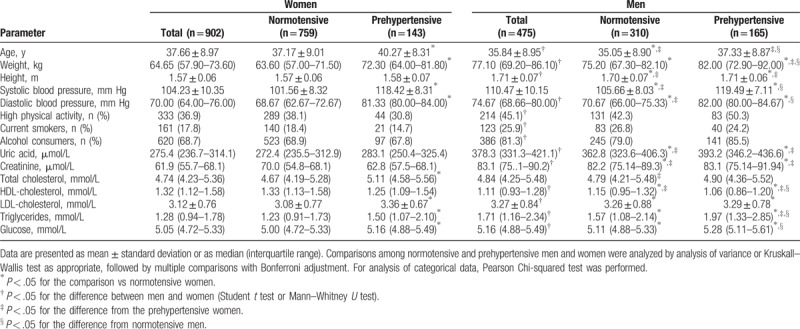
3.2. Biochemical parameters
All biochemical parameters were higher in men than in women, except for HDL-C (Table 2). Uric acid, creatinine, and LDL-C levels were not different between blood pressure groups (for both, men and women). TC was significantly increased only in prehypertensive women; while in prehypertensive men, it was similar to normotensive men and women. Glucose and TGs were significantly higher in prehypertensive compared to normotensive for both men and women (Table 2).
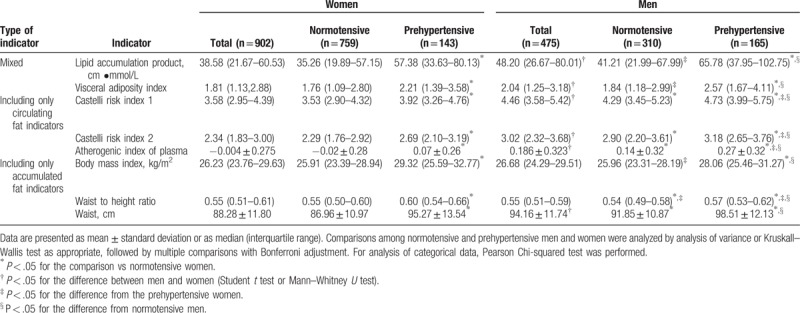
3.3. Lipid and anthropometric indicators
All lipid and anthropometric indicators were higher in men than in women, except for BMI and WtHR, which did not display any significant difference between genders. All the indicators were significantly higher in prehypertensive people (Table 3). When prehypertensive men and women were compared, all the IOCFi and WtHR significantly differed between genders, being the WtHR higher in women than men.
Table 3.
Lipid and anthropometric indicators.
3.4. ROC analysis and cutoff points for lipid and anthropometric indicators
A shown in Figure 2, and based on the ROC analysis, all the indicators were able to discriminate between normotensive and prehypertensive men and women, with a higher discriminatory power for women (except for VAI and AIP). Overall, IOAFi exhibited the highest values for AURC, followed by mixed and IOCFi. After a missing data analysis, that was performed because we did not have complete data for 7 participants, the AURCs were similar to those obtained from the original data (supplementary Tables 1 and 2).
Figure 2.
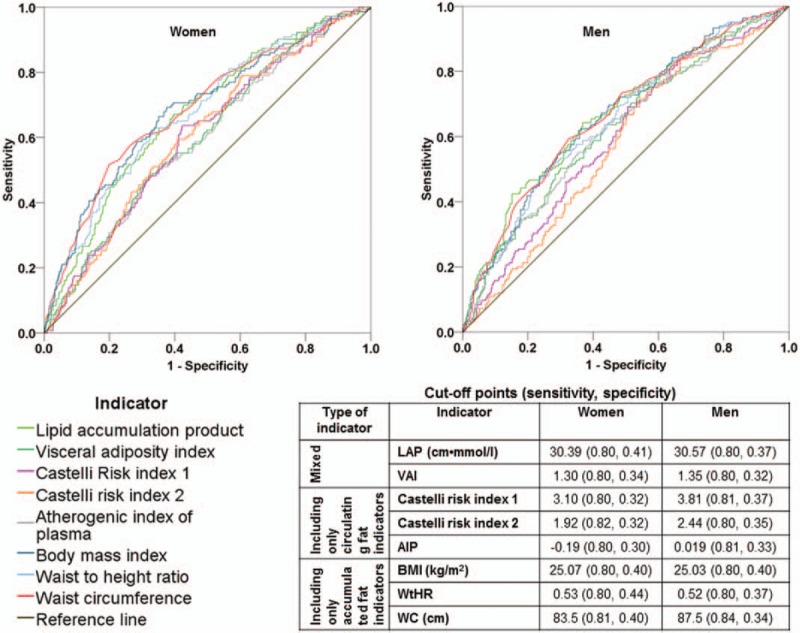
Receiving operating characteristic (ROC) curves discriminating between normotensive and prehypertensive people and cutoff points for cardiovascular risk indicators. All the indicators significantly discriminated between normotensive and prehypertensive men and women. The highest areas under the ROC curves were those of waist circumference, waist to height ratio, and lipid accumulation product for both, women (top left) and men (top right). The cutoff points, with their respective sensitivity and specificity, are displayed in the table at the bottom right. AIP = atherogenic index of plasma, BMI = body mass index, LAP = lipid accumulation product, VAI = visceral adiposity index, WC = waist circumference, WtHR = waist to height ratio.
Since all the studied parameters displayed statistical significance in the ROC analysis, their cutoff points were calculated. Cutoff values were higher for men than for women in all the parameters, except for WtHR, BMI, and LAP, where they were very close to each other (Fig. 2). We search for the maximum specificity among all those possible cutoff values having a minimum sensitivity of 0.80; specificity was higher for men in mixed indicators and IOAFi and for women in IOCFi. More details about sensitivity and specificity, together with negative and positive predictive values, are provided in supplementary Table 4.
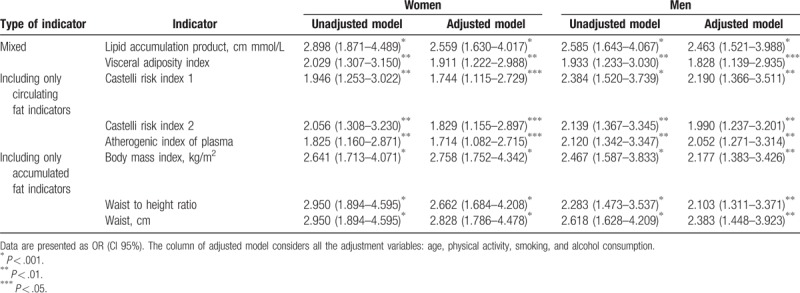
3.5. Logistic regression
The ORs were calculated from logistic regression based on the cutoff points of the table embedded in Figure 2. The unadjusted models resulted in the highest ORs for IOAFi and the mixed indicator LAP, for both women and men. In the models adjusted for all the covariates, IOAFi were the ones with the highest ORs for women, while for men, LAP was the one with the highest OR (Table 4). Age and physical activity were the only statistical significant covariates for women, in the models for all the indicators; the same covariates were statistically significant for men only for the model of AIP and age was for the model of BMI.
Table 4.
Odds ratios of prehypertension associated with each of the indicators.
4. Discussion
The relevance of detecting prehypertension has been recently recognized[32] and its association with obesity and dyslipidemia has been documented.[9,33] The present study evaluated the ability of several body-fat-related indicators to discriminate between normotensive and prehypertensive men and women. We found that indicators related to accumulated fat (named here IOAFi) were the best predictors for prehypertension, followed by mixed indicators (LAP and VAI), and finally by those related only to circulating fat (named here IOCFi).
In agreement with other studies,[9,33] prehypertensive men and women displayed a worse lipid profile compared with normotensives. Also, prehypertensive people displayed significantly higher values of all the indicators studied in this work, regardless of the type of indicator. We found here that IOAFi, such as WC, WtHR, but also a mixed indicator, LAP, had the higher AURCs; interestingly, all of them include the measurement of WC for their calculation, which is a measure of adiposity that considers the accumulation of abdominal fat.[34] Other recent works have shown a relationship between blood pressure and WC or related measurements; for instance, Caminha et al[35] reported an association between hypertension and WtHR in Brazilian women, and Ma et al[11] found that WtHR and WC (in addition to BMI) were associated with prehypertension in Chinese women and men. The AURCs in the study of Ma et al[11] to evaluate the ability of anthropometric measurements to discriminate between normotensive and prehypertensive people were lower than those obtained in our study.
It is possible that we obtained stronger associations with prehypertension for accumulated fat compared with circulating fat, as observed in the ROC analysis, because the fat accumulated in the body has circulated in the organism, probably representing a chronic exposure to circulating fat, with the consequent affection of vascular tissue.[36] Perivascular adipose tissue (PVAT) surrounds the majority of blood vessels and releases vasoactive mediators such as angiotensin peptides, reactive oxygen species, chemokines, and cytokines, so it is implicated in contraction and relaxation mechanisms[37]; however, changes in the secretory profile of PVAT have been observed in obesity, tilting the balance to favor a procontractile effect.[37] Additionally, it is known that dyslipidemia can increase media intima thickness affecting the contractile function of vascular endothelia.[9]
Cutoff points for anthropometric indicators to identify the risk of prehypertension have been scarcely explored: Ma et al[11] reported cutoff points of 79.95 cm in men and 76.85 cm in women, for WC; 21.84 in men and 21.47 in women, for BMI; and 0.476 in men and 0.494 in women for WtHR. All these cutoff points were below those reported in our study. In fact, the World Health Organization (WHO) highlights the importance of considering the impact of ethnicity on the assessment of disease risk associated with measures of abdominal obesity[15]; this imposes the need to establish cutoff points for each specific population. Current recommendations in our country for a healthy WC state 80 and 90 cm as cutoff values for women and men, respectively[38]; however, these values are based on the WC criteria established by the International Federation of Diabetes for the assessment of metabolic syndrome in Asian populations.[39]
There are just a few studies in Mexican population regarding cutoff values for WC and they were calculated for obesity, diabetes, or hypertension: a study in women aged 22 to 41 years with Mayan ancestry reported a cutoff for WC of 93 cm to identify central obesity [40]; a study in women and men aged 20 to 65 years determined 90 and 94 cm as cutoff points for hypertension[41]; and the study by Berber et al[42] reported 85 and 90 cm as cutoff values for WC in women and men, respectively, for hypertension and diabetes. A lower cutoff point could be expected in the case of prehypertension; in fact, we obtained a value of 83.5 cm to discriminate between normotensive and prehypertensive women and 87.5 for men. Interestingly, in our study, like in those mentioned above, close WC cutoff values between women and men were observed, with only 4 cm of difference between genders, contrarily to the 10 and 14 cm differences between men and women for the WC cutoff values established by the International Diabetes Federation[39] and the WHO,[15] respectively.
Regarding BMI and WtHR, their median values were significantly higher in prehypertensive women compared to prehypertensive men, although cutoff points for these parameters were very similar between genders (BMI = 25.07 and 25.03 kg/m2, and WtHR = 0.53 and 0.52 for women and men, respectively). The same behavior was observed in a Japanese population with diabetes.[43] The WtHR cutoff points for the identification of prehypertension observed in our study are in agreement with those previously reported by Berber et al[42] in a Mexican population to predict hypertension (0.525 and 0.535 for men and women, respectively).
Respect to the rest of indicators, to our knowledge, there are no reports of cutoff points regarding prehypertension; although some studies report associations between raised blood pressure and LAP, VAI, Castelli atherogenic risk indexes, and AIP.[12–14,42,43] The cutoff points reported here could be considered for further validation in future studies to be used in our population to screen for prehypertension.
In agreement with the results of this study, Wakabayashi[13] previously reported the superiority of LAP over Castelli risk indexes to predict hypertension in middle-aged men; we also observed a better performance of LAP compared with Castelli indexes, for both men and women.
The highest ORs for prehypertension associated with the cutoff points reported here were those for IOAFi and LAP. Age and physical activity also had a significant effect on prehypertensive status in all the adjusted models for women. To this respect, exercise by itself has been reported to reduce blood pressure, but an added effect is obtained when physical activity is accompanied with a behavioral weight loss program, also impacting body composition.[44] Probably, this is the reason why we obtained a significant effect of physical activity, in addition to the indicators, on prehypertensive status.
Alcohol consumption and tobacco smoking did not significantly affect the relationships between prehypertension and the studied indicators. The association between smoking and/or consuming alcohol and prehypertension has not been clearly established,[45] thus further research on the role of these factors in prehypertension is needed.
The subanalysis including sodium and potassium excretion as covariates (supplementary Table 3) showed no significant effect for potassium and a significant effect of sodium only in the logistic regression models for VAI and Castelli risk index for men. It is worth mentioning that when models were constructed without a fat indicator, sodium excretion had a significant association with blood pressure status. This is in agreement with several studies associating elevated dietary sodium consumption and high blood pressure.[46,47]
In relation to the prevalence of prehypertension, some studies have evaluated it in different populations; for instance, in the Jichi Medical School cohort, which included Japanese individuals aged 18 or more, they reported a prevalence of 34.8% and 31.8%, for men and women, respectively.[48] A more recent study in China, reported a larger difference between men and women, 45.0% for men and 33.6% for women.[49] In our study, the prevalence of prehypertension was also higher in men than in women (32% vs 15.4%).
Although this study provides information regarding the association between prehypertension and accumulated and circulating fat indicators, as well as cutoff points for Mexican people, it might have some limitations; for instance, it is a cross-sectional study, so a causal association between fat indicators and prehypertension cannot be assured. Also, a probabilistic random sampling was not performed; thus, generalizability of results might be limited. Furthermore, data on physical activity, alcohol intake, and smoking habit relay on the study participants’ self-report which can introduce a memory bias. Another potential selection bias is that the study population included clinically healthy volunteers, who could be more likely concerned about their health; thus, even though our conclusions are consistent with other studies,[11] they might not be extended to the general population.
Even though the last version of the Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults of the American College of Cardiology and the American Heart Association recommends pharmacological treatment when SBP is ≥130 mm Hg, according to our national guidelines,[50] only life style changes are recommended for people whose SBP is ≥120 and <140 mm Hg, and it is until SBP reaches 140 mm Hg when pharmacologic strategies should be implemented. It is important to consider that visceral adipose tissue is related to increased risk of developing hypertension from prehypertension[51] and that decreasing such tissue reduces the risk.[2,52] In addition, Caminha et al[35] suggested that distribution of fat at the central level can maximize hemodynamic changes observed in obesity. Considering that WC by itself represents an excess of body fat in the abdomen,[53] teaching people on how to measure their WC could be an strategy to make them aware of the need of attending a detailed medical examination to monitor their blood pressure, potentially reducing the probability of developing hypertension and their associated cardiovascular complications in the future.
In summary, the IOAFi and the LAP index are strongly associated with prehypertension in this sample of the Mexican Tlalpan 2020 cohort, while traditional indicators of cardiovascular risk such as Castelli indexes and AIP displayed a poorer association with prehypertension. An advantage of WC is that it can be relatively easy to measure and does not need biochemical determinations, so that it has the potential of being used in routine clinical examinations and as an auto-screening measurement to encourage people who exceed the proposed cutoff points to attend a medical examination.
Acknowledgment
The authors thank all the participants of this study.
Author contributions
Conceptualization: Susana Rivera-Mancía, Eloísa Colín-Ramírez, Oscar Infante, Jesús Vargas-Barrón, Maite Vallejo.
Data curation: Susana Rivera-Mancía, Eloísa Colín-Ramírez, Raúl Cartas-Rosado.
Formal analysis: Susana Rivera-Mancía, Eloísa Colín-Ramírez.
Funding acquisition: Susana Rivera-Mancía, Maite Vallejo.
Investigation: Susana Rivera-Mancía, Eloísa Colín-Ramírez, Raúl Cartas-Rosado, Maite Vallejo.
Methodology: Susana Rivera-Mancía, Eloísa Colín-Ramírez, Maite Vallejo.
Project administration: Susana Rivera-Mancía.
Software: Raúl Cartas-Rosado.
Supervision: Eloísa Colín-Ramírez, Maite Vallejo.
Writing – original draft: Susana Rivera-Mancía.
Writing – review & editing: Eloísa Colín-Ramírez, Raúl Cartas-Rosado, Oscar Infante, Jesús Vargas-Barrón, Maite Vallejo.
Supplementary Material
Footnotes
Abbreviations: AIP = atherogenic index of plasma, ANOVA = analysis of variance, AURC = area under the ROC curve, BMI = body mass index, CVD = cardiovascular disease, DBP = diastolic blood pressure, HDL-C = high-density lipoprotein-cholesterol, IOAFi = including only accumulated fat, IOCFi = including only circulating fat, IPAQ = International Physical Activity Questionnaire, LAP = lipid accumulation product, LDL-C = low-density lipoprotein cholesterol, OR = odds ratio, PVAT = perivascular adipose tissue, ROC = receiving operating characteristic, SBP = systolic blood pressure, SPSS = statistical package for the social sciences, TC = total cholesterol, TG = triglyceride, VAI = visceral adiposity index, WC = waist circumference, WHO = World Health Organization, WtHR = waist to height ratio.
This study was supported by CONACYT grant 247237. Funding was also received from AstraZeneca Mexico (collaboration agreement without number). SRM, ECR, and RCR are supported as research fellows of the program “Cátedras CONACYT” (project no: 1591) of the National Council for Research and Technology (CONACYT).
The authors have no funding and conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].World Health Organization. Raised blood pressure. 2017. Available at: http://www.who.int/gho/ncd/risk_factors/blood_pressure_prevalence_text/en/. Accessed March 5, 2018. [Google Scholar]
- [2].De Marco M, de Simone G, Roman MJ, et al. Cardiovascular and metabolic predictors of progression of prehypertension into hypertension: the Strong Heart Study. Hypertension 2009;54:974–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Ishikawa Y, Ishikawa J, Ishikawa S, et al. Progression from prehypertension to hypertension and risk of cardiovascular disease. J Epidemiol 2017;27:8–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Huang Y, Su L, Cai X, et al. Association of all-cause and cardiovascular mortality with prehypertension: a meta-analysis. Am Heart J 2014;167:160–8. [DOI] [PubMed] [Google Scholar]
- [5].Egan BM, Stevens-Fabry S. Prehypertension—prevalence, health risks, and management strategies. Nat Rev Cardiol 2015;12:289–300. [DOI] [PubMed] [Google Scholar]
- [6].Rodríguez-Ramírez M, Simental-Mendía LE, González-Ortiz M, et al. Prevalence of prehypertension in Mexico and its association with hypomagnesemia. Am J Hypertens 2015;28:1024–30. [DOI] [PubMed] [Google Scholar]
- [7].Dalal JJ, Padmanabhan TNC, Jain P, et al. LIPITENSION: Interplay between dyslipidemia and hypertension. Indian J Endocrinol Metab 2012;16:240–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Recio-Rodriguez JI, Gomez-Marcos MA, Patino-Alonso MC, et al. Abdominal obesity vs general obesity for identifying arterial stiffness, subclinical atherosclerosis and wave reflection in healthy, diabetics and hypertensive. BMC Cardiovasc Disord 2012;12:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Karasek D, Vaverkova H, Halenka M, et al. Prehypertension in dyslipidemic individuals; relationship to metabolic parameters and intima-media thickness. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 2013;157:41–9. [DOI] [PubMed] [Google Scholar]
- [10].Robles Romero MÁ, Guzmán Pantoja JE, Herrera Guadalupe BA, et al. Prevalence or arterial prehypertension and hypertension ans their relationship with obesity. Aten Primaria 2009;41:473–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Ma M, Tan X, Zhu S. Prehypertension and its optimal indicator among adults in Hubei Province, Central China, 2013–2015. Clin Exp Hypertens 2017;39:532–8. [DOI] [PubMed] [Google Scholar]
- [12].Onat A, Can G, Kaya H, et al. Atherogenic index of plasma” (log10 triglyceride/high-density lipoprotein-cholesterol) predicts high blood pressure, diabetes, and vascular events. J Clin Lipidol 2010;4:89–98. [DOI] [PubMed] [Google Scholar]
- [13].Wakabayashi I. Associations of blood lipid-related indices with blood pressure and pulse pressure in middle-aged men. Metab Syndr Relat Disord 2015;13:22–8. [DOI] [PubMed] [Google Scholar]
- [14].Gao X, Wang G, Wang A, et al. Comparison of lipid accumulation product with body mass index as an indicator of hypertension risk among Mongolians in China. Obes Res Clin Pract 2013;7:e308–14. [DOI] [PubMed] [Google Scholar]
- [15].World Health, Organization Waist Circumference and Waist-hip Ratio: Report of a WHO Expert Consultation, Geneva, 8-11 December 2008. Geneva: World Health Organization; 2011. [Google Scholar]
- [16].Kahn HS. The “lipid accumulation product” performs better than the body mass index for recognizing cardiovascular risk: a population-based comparison. BMC Cardiovasc Disord 2005;5:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Amato MC, Giordano C, Galia M, et al. Visceral adiposity index: a reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care 2010;33:920–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Edwards MK, Blaha MJ, Loprinzi PD. Atherogenic index of plasma and triglyceride/high-density lipoprotein cholesterol ratio predict mortality risk better than individual cholesterol risk factors, among an older adult population. Mayo Clin Proc 2017;92:680–1. [DOI] [PubMed] [Google Scholar]
- [19].Santos ABS, Gupta DK, Bello NA, et al. Prehypertension is associated with abnormalities of cardiac structure and function in the atherosclerosis risk in communities study. Am J Hypertens 2016;29:568–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Weil BR, Stauffer BL, Greiner JJ, et al. Prehypertension is associated with impaired nitric oxide-mediated endothelium-dependent vasodilation in sedentary adults. Am J Hypertens 2011;24:976–81. [DOI] [PubMed] [Google Scholar]
- [21].World Health Organization. Cardiovascular Disease. Strategic priorities. WHO. 2017. Available at: http://www.who.int/cardiovascular_diseases/priorities/en/. Accessed March 5, 2018). [Google Scholar]
- [22].Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2013;31:1281–357. [DOI] [PubMed] [Google Scholar]
- [23].Colín-Ramírez E, Rivera-Mancía S, Infante-Vázquez O, et al. Protocol for a prospective longitudinal study of risk factors for hypertension incidence in a Mexico City population: the Tlalpan 2020 cohort. BMJ Open 2017;7:e016773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Centers for Disease Control, Prevention (CDC) State-specific secondhand smoke exposure and current cigarette smoking among adults - United States, 2008. MMWR Morb Mortal Wkly Rep 2009;58:1232–5. [PubMed] [Google Scholar]
- [25].Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003;35:1381–95. [DOI] [PubMed] [Google Scholar]
- [26].Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003;42:1206–52. [DOI] [PubMed] [Google Scholar]
- [27].International Standards for Anthropometric Assessment. Australia: The International Society for the Advancement of Kinanthropometry, ISAK; 2001. [Google Scholar]
- [28].Vargas HO, Nunes SOV, Barbosa DS, et al. Castelli risk indexes 1 and 2 are higher in major depression but other characteristics of the metabolic syndrome are not specific to mood disorders. Life Sci 2014;102:65–71. [DOI] [PubMed] [Google Scholar]
- [29].Dobiásová M, Frohlich J. The plasma parameter log (TG/HDL-C) as an atherogenic index: correlation with lipoprotein particle size and esterification rate in apoB-lipoprotein-depleted plasma (FER(HDL)). Clin Biochem 2001;34:583–8. [DOI] [PubMed] [Google Scholar]
- [30].Keys A, Fidanza F, Karvonen MJ, et al. Indices of relative weight and obesity. J Chronic Dis 1972;25:329–43. [DOI] [PubMed] [Google Scholar]
- [31].López-Ratón ML. Optimal cutoff points for classification in diagnostic studies: new contributions and software development. 2016. Available at: https://minerva.usc.es/xmlui/handle/10347/14593. Accessed March 5, 2018. [Google Scholar]
- [32].Pannarale G, Moroni C, Acconcia MC, et al. The natural history of prehypertension. A 20-year follow-up. Eur Rev Med Pharmacol Sci 2017;21:1329–34. [PubMed] [Google Scholar]
- [33].Yu D, Huang J, Hu D, et al. Association between prehypertension and clustering of cardiovascular disease risk factors among Chinese adults. J Cardiovasc Pharmacol 2009;53:388–400. [DOI] [PubMed] [Google Scholar]
- [34].Leitzmann MF, Moore SC, Koster A, et al. Waist circumference as compared with body-mass index in predicting mortality from specific causes. PLoS One 2011;6:e18582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Caminha TCS, Ferreira HS, Costa NS, et al. Waist-to-height ratio is the best anthropometric predictor of hypertension: a population-based study with women from a state of northeast of Brazil. Medicine (Baltimore) 2017;96:e5874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Brookheart RT, Michel CI, Schaffer JE. As a matter of fat. Cell Metab 2009;10:9–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Ramirez JG, O’Malley EJ, Ho WSV. Pro-contractile effects of perivascular fat in health and disease. Br J Pharmacol 2017;174:3482–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Secretaría de Salud. NORMA Oficial Mexicana NOM-043-SSA2-2012, Servicios básicos de salud. Promotion and education for health in the matter of food. Criteria to provide guidance. 2013. Available at: http://dof.gob.mx/nota_detalle.php?codigo=5285372&fecha=22/01/2013. Accessed March 5, 2018. [Google Scholar]
- [39].Alberti G, Zimmet P, Shaw J, et al. The IDF consensus worldwide definition of the metabolic syndrome. 2006. Available at: https://www.idf.org/e-library/consensus-statements/60-idfconsensus-worldwide-definitionof-the-metabolic-syndrome. Accessed March 5, 2018. [Google Scholar]
- [40].Banik SD, Dickinson F. Waist circumference cut-off in relation to body mass index and percentage of body fat in adult women from Merida, Mexico. Anthropol Anz 2015;72:369–83. [DOI] [PubMed] [Google Scholar]
- [41].Macias N, Quezada AD, Flores M, et al. Accuracy of body fat percent and adiposity indicators cut off values to detect metabolic risk factors in a sample of Mexican adults. BMC Public Health 2014;14:341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Berber A, Gómez-Santos R, Fanghänel G, et al. Anthropometric indexes in the prediction of type 2 diabetes mellitus, hypertension and dyslipidaemia in a Mexican population. Int J Obes Relat Metab Disord 2001;25:1794–9. [DOI] [PubMed] [Google Scholar]
- [43].Wakabayashi I. Gender-related differences in cardiometabolic risk profile of Japanese patients with diabetes. J Womens Health 2014;23:1046–53. [DOI] [PubMed] [Google Scholar]
- [44].Blumenthal JA, Sherwood A, Gullette ECD, et al. Exercise and weight loss reduce blood pressure in men and women with mild hypertension: effects on cardiovascular, metabolic, and hemodynamic functioning. Arch Intern Med 2000;160:1947–58. [DOI] [PubMed] [Google Scholar]
- [45].Unsal S, Ozkara A, Albayrak T, et al. Evaluation of prehypertension and masked hypertension rate among clinically normotensive patients. Clin Exp Hypertens 2016;38:218–24. [DOI] [PubMed] [Google Scholar]
- [46].Cogswell ME, Mugavero K, Bowman BA, et al. Dietary sodium and cardiovascular disease risk—measurement matters. N Engl J Med 2016;375:580–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Takase H, Sugiura T, Kimura G, et al. Dietary sodium consumption predicts future blood pressure and incident hypertension in the Japanese normotensive general population. J Am Heart Assoc 2015;4:e001959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Ishikawa Y, Ishikawa J, Ishikawa S, et al. Prevalence and determinants of prehypertension in a Japanese general population: The Jichi Medical School Cohort Study. Hypertens Res 2008;31:1323–30. [DOI] [PubMed] [Google Scholar]
- [49].Wang Z, Chen Z, Zhang L, et al. Status of hypertension in China: results from the China hypertension survey, 2012–2015. Circulation 2018;137:2344–56. [DOI] [PubMed] [Google Scholar]
- [50].Secretaría de Salud. Draft of the Official Mexican Standard PROY-NOM-030-SSA2-2017, for prevention, detection, diagnosis, treatment, and control of systemic arterial hypertension. 2017. Available at: http://www.dof.gob.mx/nota_detalle.php?codigo=5480159&fecha=19/04/2017. Accessed June 23, 2018. [Google Scholar]
- [51].Sullivan CA, Kahn SE, Fujimoto WY, et al. Change in intra-abdominal fat predicts the risk of hypertension in Japanese Americans. Hypertension 2015;66:134–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Hwang Y-C, Fujimoto WY, Kahn SE, et al. Greater visceral abdominal fat is associated with a lower probability of conversion of prehypertension to normotension. J Hypertens 2017;35:1213–8. [DOI] [PubMed] [Google Scholar]
- [53].Ellulu MS. Obesity, cardiovascular disease, and role of vitamin C on inflammation: a review of facts and underlying mechanisms. Inflammopharmacology 2017;25:313–28. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


