Abstract
Purpose
As racial and ethnic heterogeneity in the U.S. population increases, it is important that the health care workforce, including surgery, mirror that diversity. Structural and perceptual barriers may contribute to an underrepresentation of African-American and Latino surgeons. Understanding these barriers may translate into interventions, and in turn, improved diversification of the U.S. surgery workforce.
Method
In 2016, the authors conducted in-depth semistructured interviews to explore structural and perceptual barriers African-American and Latino surgeons face. The authors used conventional qualitative techniques to analyze data and identify themes.
Results
The authors interviewed 23 participants and observed three major themes characterizing the path to becoming a surgeon: creating a path to medicine, surgical culture, and mentorship. Subthemes provided further nuance. For creating a path to medicine, the subthemes were personal attributes, family support, community assets/barriers, and minority experience. For surgical culture, the subthemes comprised quality of life, surgeon-patient relationship, and restoring health. For mentorship, the subthemes were aspirational figures, formal programs/peer support, and professional opportunities. The experiences described by African-Americans and Latinos were similar, but the experiences of participants of different self-identified childhood socioeconomic status were dissimilar.
Conclusions
The path to a surgical career as experienced by African-American and Latino surgeons is heavily influenced by mentors mediating their integration into surgical culture and engendering a feeling of belonging. Future surgeons from groups underrepresented in medicine would benefit from identifying aspirational figures early, a structured introduction into the rigors of the profession, and a deconstruction of negative surgical norms.
According to the Association of American Medical Colleges (AAMC) report, Diversity in the Physician Workforce: Facts & Figures, 2014, African-Americans and Latinos represented, respectively, 4.4% and 4.8% of physicians in 2014 as compared to 52.4% representation by non-Hispanic White physicians and 11% representation by Asian physicians (the remaining physicians were “Other” or “Unknown”).1 Another study, of 40 years of AAMC demographics data (1966 to 2006), has shown that rates in surgery specifically are also dim: African-Americans and Latinos represent, respectively, 5.4% and 4.8% of all U.S. surgeons compared to the 71.1% representation of non-Hispanic Whites.2 As the racial and ethnic heterogeneity of the U.S. population increases, it is important that the health care workforce, including surgery, mirror that diversity.3,4 A sizable research base documents how patients benefit from a diverse physician workforce.5–7 Indeed, in its 2001 “Statement on Diversity,” the American College of Surgeons (ACS) recognized that the recruitment of underrepresented groups, including women and minorities, is essential to maintaining the strength of its organization.8 While recognizing that diversity is a core component in maintaining the excellence of a professional organization, the ACS statement lacks a specific strategy to achieve that goal. Persons who are underrepresented in medicine (URM), defined by the AAMC as those belonging to racial and ethnic populations underrepresented in the medical profession relative to their number in the general population (primarily African-Americans, Latinos, and Native Americans/Alaskan Natives), may face unique structural and perceptual barriers that impede their participation and inclusion in medical training. These barriers may also adversely affect the provision of care for some patient populations and negatively shape the diversity of the U.S. surgical workforce—both now and in the future.
Previous studies have illustrated the marked differences between URM surgeons and their non-Hispanic White surgeon counterparts. For example, one study reported that underrepresented minority surgeons were more likely to be non-board-certified.9 Another study showed that the proportion of women and African-Americans in almost every board-certified surgical specialty workforce remained lower than in the overall board-certified workforce.10
More research is needed to understand the experiences of URM surgeons. Specifically, the medical community knows little about URM experiences in training and paths to a career in surgery. Such information may inform future strategies to increase the diversity of the surgical workforce and the representation of URM surgeons.
The information that does exist about the experiences of racial-ethnic minorities in surgery includes data on perceptual barriers, which have been identified in surveys as social isolation, a sense that training is too long, and a fear of being recruited due only to one’s minority status.11 This research does not provide detailed information about how individuals experience such structural or perceptual barriers—even though such experiences may play a critical role in their decisions to enter or remain in a profession. Understanding how African-American and Latino surgeons choose their profession, complete their training, and overcome perceptual and structural barriers may be critical to guiding strategies that encourage URM physicians to consider and select surgery. Research to provide detailed narratives on the perspectives and experiences of URM surgeons could thus help inform a national strategy to enhance the recruitment and retention of a more diverse surgical workforce.
In this study, we sought to explore and characterize the range of experiences in terms of structural and perceptual barriers among practicing African-American and Latino surgeons. Our goals were (1) to characterize the path to becoming a surgeon as described by African-American and Latino participants, and (2) to identify key themes related to entering and progressing in a surgical career that might serve as a roadmap to support aspiring surgeons who have a URM background.
Method
Participants and recruitment
We employed purposeful sampling to include surgeons with variation in years in practice, practice setting, geographical region, sex, and race-ethnicity (Latino, African-American). First, we contacted 23 potential participants, constituting a convenience sample of surgeons known to us. Two of us (J.G.U. and M.M-G.) contacted potential participants via e-mail requesting their participation in a qualitative study on African-American and Latino surgeons’ career paths. Eligible surgeons had completed at least three years of general surgery residency. We excluded surgeons practicing in the subspecialties of urology, ophthalmology, otolaryngology, neurosurgery, orthopedic surgery, oral/maxillofacial surgery, and obstetrics and gynecology since the pathway to careers in those subspecialties entails an independent application process. We also excluded surgeons who do not identify as African-American or Latino.
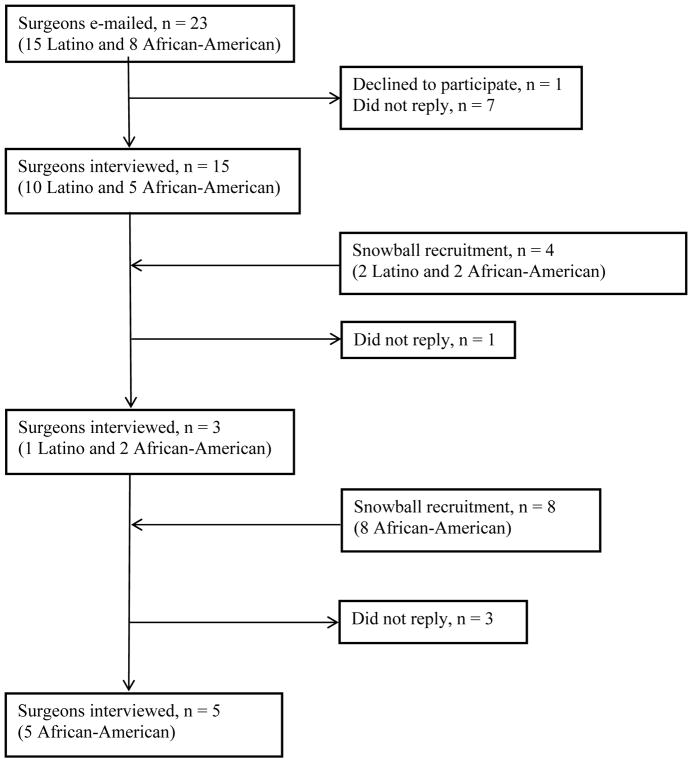
Recruitment procedures included an initial e-mail, a second two weeks later, and a third six weeks after the first contact. We asked potential participants to recommend colleagues who both met our inclusion criteria and who might be interested in participating to augment the sample size. This snowball sampling strategy yielded contact information for 12 additional surgeons (see Figure 1). We ended recruitment when we reached thematic saturation (i.e., when interviews yielded no new information).12 Participation was voluntary, and all participants provided their verbal consent. We offered all participants a $50 gift card and entered them into a raffle to win an electronic tablet computer as incentives to participate. All recruitment and interviews occurred from October 2015 to January 2016.
Figure 1.
Recruitment of participants for a qualitative study in 2016 of Latino and African-American surgeons. The authors recruited surgeons and interviewed them to determine the perceptual and structural barriers and facilitators they faced on the path to becoming a surgeon. The authors contacted 35 surgeons (12 through snowball recruitment). Of these 35, 1 declined and 11 did not reply. The authors interviewed 23 surgeons.
Interviews and data
One of us (J.G.U.) conducted all of the interviews either in person or by phone in two parts: (1) structured background and demographic questions, and (2) an approximately 30 minute semi-structured interview.
The background and demographic information we requested included each participant’s, age, gender, fluency in a language other than English, perceived childhood socioeconomic status (SES; see below), surgical specialty, number of years in practice, completion (or not) of a research year during residency, completion (or not) of a clinical fellowship, current practice type, residency training type, undergraduate (baccalaureate) institution, medical school, and residency training site. We grouped participating surgeons arbitrarily, based on their age, as early career surgeons (≤ 45 years old), mid-career surgeons (46–53 years old), or late career surgeons (≥ 54 years old). In this study, we did not define SES in terms of specific monetary or income categories since both inflation and region affect values, but, instead, in term’s of each participant’s perspective of their childhood SES (“low SES,” “middle SES,” or “high SES”). All interviews were audio-recorded.
We designed semi-structured interview to explore participants’ professional development during high school, college (baccalaureate education), medical school, residency/fellowship, and current practice. We asked four questions: (1) What was your path to becoming a surgeon?, (2) What intrinsic qualities helped or hindered you along your path?, (3) How did your family and/or community help or hinder you along your path?, and (4) What do you value most in your role as a surgeon? The interviewer (J.G.U.) asked probing questions as necessary to elicit additional information. A priori, two of us (J.G.U. and G.M.) pilot-tested the question matrix on volunteers and made modifications according to these experiences.
The salient characteristics of the interviewer (J.G.U.) include being a surgeon and from an ethnic group traditionally designated as URM. One of us, a senior qualitative researcher (G.R.) mentored and trained the interviewer. The audio recordings were professionally transcribed and de-identified by a paid third party (Keystrokes, Santa Monica, California). We used Dedoose (Hermosa Beach, California), a web-based qualitative data analysis system to extract, organize and manage, and code the data. The study was approved by the University of California Los Angeles Human Research Protection Program.
Analysis
We used descriptive statistics to calculate frequencies, means, and standard deviations (SDs) for demographic variables.
We used conventional qualitative methods to analyze the interview transcripts and to define codes and keywords which we derived from the data.13–16 Three of us (J.G.U., G.M., and O.V.) each individually read the transcripts several times and independently analyzed the transcripts. We categorized concepts into codes, which we used to label discrete comments in the transcripts. The process was iterative, and, as we read and reread the transcripts, we revised and expanded code categories, as necessary, to create a coding scheme. Next, we (J.G.U., G.M., and O.V.) de-briefed to resolve differences and to use the resulting code book to code all transcripts. Two of us (J.G.U. and O.V.) used pile-sorting to code quotations into subthemes. (Pile-sorting is the process of printing quotations onto individual separate cards, placing all of them onto a large flat surface, and then sorting them into groups of similar statements.17) One of us (G.M.) arbitrated any disagreements. This iterative process yielded the categorization of codes into three broad themes and 10 subthemes.
To decrease bias and to ensure consistency and validity, we organized a diverse team to assess and refine the project—starting prior to the first interviews and continuing throughout the process of analysis. The researchers on the study team had training in anthropology, qualitative research, psychiatry, family medicine and primary care, and health services research. Further, the team included a male and female surgeon, and one medical student.
Results
Twenty-three surgeons participated in our study (see Table 1). They ranged in age from 38 to 68 years of age (mean = 45 years; SD = 8). The majority were men (n = 20; 87%), and about half were African-American (n = 12, 52%) and about half were Latino (n = 11, 48%). About half of the participating surgeons (n = 11; 48%) were from a perceived middle SES background. The surgeons practiced in 10 states across the continental United States, and had been in practice from 1 to 30 years (mean = 9.48 years; SD = 8). About three quarters (n = 17; 74%) identified as subspecialists, working in thoracic surgery, vascular surgery, plastics, surgical oncology, endocrinology, pediatric surgery, colorectal surgery, bariatric/minimally invasive surgery, and trauma/critical care. The majority of the surgeons (n = 20; 87%) currently saw patients in an academic setting. Almost all of the participants (n = 21; 91%) completed a clinical fellowship; most (n = 19; 83%) trained in an academic affiliated residency program; and nearly three quarters (n = 16; 70%) had completed a dedicated research year during residency training.
Table 1.
Demographic Characteristics of 23 Latino and African-American Surgeons Interviewed to Determine the Perceptual and Structural Barriers and Facilitators They Experienced on Their Journey to Becoming a Surgeon, 2016
| Characteristics | No. (% of 23) |
|---|---|
| Age in yearsa | |
| ≤ 45 | 14 (61) |
| 46 – 53 | 5 (22) |
| ≥ 54 | 4 (17) |
| Gender | |
| Male | 20 (87) |
| Female | 3 (13) |
| Race/Ethnicity | |
| African-American | 12 (52) |
| Latino | 11 (48) |
| Fluent in a second language | 14 (61) |
| SES during childhoodb | |
| Low SES | 10 (43) |
| Middle SES | 11 (48) |
| High SES | 2 (9) |
| Undergraduate (baccalaureate) institution | |
| Public | 8 (35) |
| Private | 15 (65) |
| Medical School | |
| Public | 11 (48) |
| Private | 12 (52) |
| Type of surgeon | |
| General | 6 (26) |
| Subspecialistc | 17 (74) |
| Years in practiced | |
| ≤ 5 | 9 (39) |
| 6 – 10 | 6 (26) |
| 11 – 15 | 3 (13) |
| ≥ 16 | 5 (22) |
| Residency training | |
| Academic | 19 (83) |
| Community | 4 (17) |
| Completed a resident research year | 16 (70) |
| Completed a fellowship | 21 (91) |
| State residencee | |
| California | 14 (61) |
| Pennsylvania | 1 (4) |
| Texas | 1 (4) |
| Louisiana | 1 (4) |
| Arizona | 1 (4) |
| Washington | 1 (4) |
| Maryland | 1 (4) |
| North Carolina | 1 (4) |
| Connecticut | 1 (4) |
| Massachusetts | 1 (4) |
| Practice type | |
| Academic | 20 (87) |
| Community/Private | 3 (13) |
Abbreviation: SES indicates socio-economic status.
The mean age of the 23 physicians was 45 years (standard deviation = 8)
In this study, the authors did not define SES in terms of specific monetary or income categories since both inflation and region affect values, but, instead, in terms of each participant’s perspective of their childhood SES (“low SES,” “middle SES,” or “high SES”).
Subspecialties include thoracic surgery, vascular surgery, plastics, surgical oncology, endocrinology, pediatric surgery, colorectal surgery, bariatric/minimally invasive surgery, and trauma/critical care.
The authors measured years in practice as number of years after completing training (residency or fellowship). The mean number of years in practice was 9 (standard deviation = 8)
Percentage does not equal 100 due to rounding.
We identified three major themes that characterized our participants’ experience of becoming surgeons: (1) creating a path to medicine, (2) surgical culture, and (3) mentorship. We describe each theme, along with their subthemes, below. We also provide representative quotations demonstrating the range of experiences both below and in Table 2. We identify quotations from African-American and Latino surgeons using, respectively, (AA) and (L).
Table 2.
Quotations Representing Subthemes From a Qualitative Study of 23 Latino and African-American Surgeons Interviewed About The Perceptual and Structural Barriers and Facilitators They Experienced on Their Journey to Becoming a Surgeon, 2016
| Themes and subthemes | Illustrative excerpts representing subthemes |
|---|---|
| Theme 1: Creating a path to medicine | |
| Personal attributes |
|
| Family support |
|
| Community assets/barriers |
|
| Minority experience |
|
| Theme 2: Surgical culture | |
| Quality of life |
|
| Surgeon/patient relationship |
|
| Restore health |
|
| Theme 3: Mentorship | |
| Aspirational figures |
|
| Formal programs/peer support |
|
| Professional opportunity |
|
Abbreviations: AA indicates African-American; L, Latino.
Theme 1: Creating a path to medicine
Most participants characterized the starting point on their path to medicine as either an unstructured experience relying on self-discovery, or a structured path formed by family members before them. The differentiation in structured versus unstructured path most closely mirrored the participants’ perceived childhood SES.
Specifically, participants from a low SES background described struggling to transform what felt like a far-off dream into a tangible goal. They had the desire to become a physician, but no idea of where to begin or whom to ask for help. Their experiences contrasted directly with those participants from a high SES background. These participants reported broad exposure to education and professional role models; they could envision a future as a physician.
For some participants, differences in academic preparation had an early and long-term effect on their journey to becoming a physician. To illustrate, one Latino participant commented, “From a very early age, my written communication skills were not very good. I was valedictorian of my high school, and I graduated not knowing how to write.” The surgeons who perceived their childhood SES as low described graduating at the top of their class from resource-poor public school systems only to realize how far behind they were academically compared to their high SES counterparts who did not describe struggling academically. Participants, specifically those who perceived a low childhood SES, often mentioned unequal academic preparation as an ongoing issue still relevant when they wrote grants for academic funding or communicated scientific findings. Four subthemes provided nuance to the theme of creating a path to medicine: personal attributes, family support, community assets and barriers, and the minority experience.
Personal attributes
Many of the participants described specific, personal characteristics that helped them attain their career goals. Participants described being stubborn, persistent, and not fearing failure. Many participants communicated this sense of self-worth bluntly yet eloquently. One Latino surgeon clearly stated his own strengths:
So being an advocate for yourself; knowing what you want to do; being a hard worker and not being discouraged. So, I mean, it’s true and we joke about it in surgery that we thrive on negative reinforcement. Like I don’t really care so much when you tell me how good I am. Like I want to know what the bad things are so that I can make it better. And so it’s this continual striving to better yourself so that you can continue to be competitive.
Family support
Family support was integral to the surgeons we interviewed. They often illustrated this support through examples that conveyed core family values or parental influence on striving for and reaching career goals. Uniformly, participants described the importance of their family upbringing and being endued with a strong sense of self-worth and capacity.
A surgeon’s core set of values were particularly important; surgeons called upon these principles to overcome the challenges of residency training. To illustrate, one participant described being chastised by a senior resident many miles from home early during residency training, and tapping into this unshakeable resolve to succeed: “that to me is a result of having been raised in a family and environment that allowed me to develop and maintain a positive sense of self” (AA).
Despite a strong sense of self-worth, participants who were the first physicians in their family had difficulty describing to family members the intensity of the training and the time needed to become a surgeon. For some participants, the struggles of academic study and acquiring the critical technical skills required in surgery were amplified by family members asking, “‘You’re still not a doctor? I thought you were a doctor.’ It was very difficult for people to wrap their brain around how long it takes to finally be a bona fide surgeon” (L).
Community assets and barriers
Most participants described the setting they were raised in, as well as how that setting either helped them attain or hindered them from reaching their career goals. Participants’ experience of their childhood community mirrored their perception of their childhood SES. The surgeons described how their immediate surroundings influenced them and shaped their self-expectations. Those who perceived a low childhood SES described an environment of low expectations and having to explain why they would want more from life than the status quo. Participants from high SES backgrounds mentioned multiple people in their community who reaffirmed their belief that they could pursue anything without having to provide justification. Visualizing one’s role in surgery and blending into the broader surgical community was easier for middle and high SES participants. One surgeon admitted, “The underrepresented minorities who survive in this setting tend to be those of us who were surrounded by some affluence and kind of lived in a white culture well before surgery” (AA).
Minority experience
The participants all spoke of their experience as a minority—as characterized by others stereotyping them or categorizing them by their skin color. They described feeling like an outsider and/or working twice as hard to achieve equal recognition. They relayed an overwhelming sense of working hard to belong among peers, to appear familiar (i.e., like other surgical trainees, as opposed to trainees defined by their URM status or skin color)—in addition to learning how to become surgeons.
The struggle to belong in the medical field, especially in the surgical discipline, as participants had envisioned, often started early in their career. Participants were often subtly encouraged to pursue a medical career that would take them “back to their community.” One participant sought help on composing a personal statement as part of their medical school application. The advisor quickly assumed the applicant wanted to help the “community” and return to practice there. The surgeon commented:
I remember sitting there thinking, ‘This guy, number one, he has no clue of who I am. Number two, if I go back and help my community, I’m from Buckhead in Atlanta—which is the equivalent of Beverly Hills within L.A., they don’t need another one of me in Buckhead; you are making an assumption about me and trying to push me in a certain direction.’ (AA)
Theme two: Surgical culture
Most participants highlighted surgical culture, explicitly describing what it means to be a surgeon and how many think surgeons fit a particular mold. One Latino participant commented, “Surgery is kind of clubby. There’s a certain kind of person, a certain kind of look, and certain kinds of organizations you join, like a frat.” Identifying with the prototypical surgeon was a source of internal contention for participants, particularly during medical school. Many of the participants viewed surgery as a white-male-dominated field, not particularly friendly or open to those who might be different.
The surgeon participants also offered positive characterizations of surgical culture that often outweighed the negative surgical stereotypes. Specifically, the surgeons enjoyed providing patient care and learning and applying technical skills. They also took pride in the personal sacrifices they made to protect the well-being of the patients before them (e.g., being late for a family dinner party after checking on a patient once more before leaving the hospital). Three subthemes arose in relation to surgical culture: quality of life, surgeon-patient relationship, and restoring health.
Quality of life
The surgeons we interviewed—irrespective of their race/ethnicity or perceived childhood SES status—expressed an understanding that surgery entails personal sacrifice during training (and even beyond) to provide high-quality patient care. They realized that the time commitment spent in medical school and residency becomes only greater in the final stage of career development: practice. One participant’s comment reflected the sentiment of most participants: “The lifestyle commitment is I think the biggest barrier. If you really understand what it means to become a surgeon” (L).
Surgeon-patient relationship
The surgeons participating in our study highlighted the deep, meaningful nature of surgeon-patient relationships. They often spoke of what a privilege operating on someone is and of the immediate gratification they felt from their intervention. Most participants stated that the reason they existed was to guide patients through a trying time in life and that their commitment to patients often extended outside of the operating room. To illustrate, one African-American surgeon eloquently articulated:
You have a special relationship with patients, you save people’s lives, you work with them closely. I have this very long-term view of surgery. Once I operate on you, you can come and see me. I have people who I’ve operated on five or ten years ago come and see me all the time.
In addition to enjoying the technical aspect of surgery, most surgeons greatly enjoyed the patient-surgeon relationship as the bond with patients added deeper meaning to their work.
Restoring health
In response to the question about what they valued about being a surgeon, the participants commented on helping patients return to health and regain (sometimes nearly instantly) function. Across childhood SES status and race/ethnicity categories, surgeons described being in the trade of helping to protect and restore health. One participant’s comment illustrates what others also expressed: “To be able to intervene to try to save somebody’s life, that’s a positive thing. And I think that’s a good thing” (AA).
Theme three: Mentorship
Surgeon participants uniformly highlighted the importance of mentorship for shaping their career. Many conveyed how they struggled without adequate mentors to function as intermediaries or guides to navigate the culture of surgery. Most participants did not realize the importance of what seemed like inconsequential decisions when planning their career; these participants recognized that they would have benefited from a mentor. Those who enjoyed excellent mentorship relayed how a mentor, attuned to their experience, could guide them past barriers. One Latino surgeon commented, “I was fortunate that my boss, who is a minority, is attuned to what that’s like. Also coming from an immigrant family, he understands the hopes and the pressures that come from immigrant parents.” We detected three subthemes—aspirational figures, formal programs and peer support, and professional opportunities—which provided nuance to the theme of mentorship.
Aspirational figures
Participants described visualizing themselves in the role of a surgeon and the positive effect this future self-image had on their career. In particular, seeing themselves mirrored in someone successful was important. The surgeons most commonly described identifying aspirational figures either during high school or, as for the following participant, during medical school: “Two of the chief residents happened to be the first African-American chief residents at a highly respectable Harvard surgical residency program, and they were outstanding” (AA). For most participants, seeing accomplished and respected peers in the field they aspired to enter made their goals more tangible. The participant quoted immediately above went on to say, “I said, ‘I want to be like those guys, like Michael Jordan, I want to be like Mike’” (AA).
Formal programs and peer support
Another subtheme involved the formal programs and peer support that shaped participants’ interest in and access to medical careers. For low SES participants, participating in formal programs (e.g., Minorities in Biomedical Research, the National Institutes of Health) and joining peer networks (e.g., the Latino Medical Student Association [LMSA], Society of Black Academic Surgeons [SBAS]) were especially important. These structured activities increased their exposure to and awareness of opportunities, including the possibility of attending different academic training institutions. One Latino participant recalled a defining moment:
I remember going to my first LMSA event at UCLA [University of California Los Angeles] with one of my other Latino buddies, and he also wanted to go into medicine. I remember seeing this pediatric cardiologist from UCLA speaking and, man, that lady was really motivational. I just remember feeling very like, “You know, I’m capable,” and I’m like “I can do this, you know, this lady’s telling me I can do it.”
The participants of this study also noted that despite providing structured activities, many URM programs lacked foresight and provided no resources for assisting program participants with the next step of career development.
Professional opportunities
Lastly, participants mentioned professional opportunities. Specifically, they felt mentors were most effective when they created professional opportunities and proactively gave them career guidance. One African-American surgeon clearly expressed this sentiment when describing the African-American mentor discovered during residency: “I realized that there is a difference in mentorship. I had never really felt like anybody took me under their wing, and that’s what I had with this amazing mentor.”
Discussion and Conclusions
In conducting this qualitative study of African-American and Latino surgeons, we detected three themes for becoming a surgeon: creating a path to medicine, surgical culture, and mentorship. Associated subthemes provided further nuance. The experiences described by African-American and Latino participants were similar, but the experiences of participants who perceived their childhood SES differently were dissimilar. Our study offers a deeper understanding of the structural and perceptual barriers that African-Americans and Latinos who chose a surgical profession encounter.
Previous research shows that URM medical school applicants face many barriers (perceptual, financial, etc.,) on their path to a career in medicine. Aspiring URM physicians and dentists have noted that inadequate institutional resources, limited clinical opportunities, strained personal resources, and inadequate guidance and mentoring are the biggest barriers to continuing on the path to a medical career.18 These barriers are amplified by structural inequalities in academic institutions.19 Our findings expand this knowledge to surgeons. Participants who perceived their childhood SES as low described attending resource-poor school systems and the consequent effects on pursuing a professional degree. The focus of this study was not the effect of the educational system for low SES URM applicants; nonetheless, primary and secondary education clearly play a role in career preparation and early opportunity. Importantly, training programs should recognize that some URM physicians, particularly those with a lower childhood SES, may need—but feel reticent to request—a more robust academic orientation and greater educational support.
The underrepresentation of African-Americans and Latinos in surgery is well described. As mentioned earlier, a 2006 article reports that African-Americans and Latinos represented 5.4% and 4.8% of all U.S. surgeons as compared to 71.1% representation by whites.2 Within academia, the disparity is even starker: African-American and Latino surgeons represent, respectively, 2.9% and 3.6% of the surgical faculty—the lowest among the medical disciplines.20 Since then the rates of African-American and Latino physicians have not drastically increased.1 It is therefore not surprising that our participants found mentorship was available but highlighted a lack of colleagues with whom they could identify. Based on our results, we believe that identifying aspirational figures who look like aspiring surgeons is most important at the high school and medical school levels of career development. Thus, URM surgeons could actively influence the career aspirations of URM adolescents by participating in high school or community outreach events. Butler and colleagues have described the Diverse Surgeons Initiative, a program created in the late 1990s, to increase students’ exposure to minimally invasive surgery and, in turn, increase the number of URM surgeons.21 Formal federal funding or explicit support from residency training sites for similar programs may be effective outreach for URM medical students interested in surgery.
Even with great opportunities and role models, the reality of surgical training entails, according to our participants, feeling isolated and without support. Our findings mirror reported feelings of isolation and poor program fit described in prior surgery research. In a survey of 4,339 surgical residents, Wong and colleagues found that Black residents were less likely to feel happy at work compared to white residents (73.9% vs 62.2%, P < 0.001).22 In the same study, Black and Asian residents were more likely than their white colleagues to report that attendings would think poorly of them if they asked for help (20.4% and 18.4% vs 13.5% respectively, P = 0.002).22
With the goal of creating mentorship networks and ameliorating feelings of isolation, URM surgeons have developed professional associations. One example is the SBAS established in 1987 with the specific goal of supporting African-American surgeons working in the field of academic surgery. Multiple participants in our study commented on the importance of SBAS for networking, meeting fellow surgeons, and finding mentors. Outreach by SBAS and the Association of Women Surgeons, has been, and will continue to be, of critical importance for URM applicants in the surgery pipeline.
The study has limitations. We used a convenience sample of African-American and Latino surgeons who had completed surgical training. We did not include those who considered surgical training (and opted for another specialty), those who dropped out of surgical training, or those from other racial or ethnic minority groups (e.g., Native American surgeons). We assumed, due to the nature of the study and limited interviewing time, that we did not earn the complete trust of the participants, especially regarding any of the significant psychosocial stressors they may have experienced along their path to becoming surgeons. Therefore, we may actually understate some of the stressors URM minorities experience in becoming surgeons. One of us—J.G.U., a surgeon and a member of the study group—completed all of the semi-structured interviews, which may have introduced bias; however, we tried to minimize potential bias by asking open-ended questions, engaging in reflexivity, and forming a diverse research team with diverse areas of expertise.
Additionally, we likely encountered some themes reflecting secular trends that no longer apply or have had a greater bearing for previous generations of physicians (i.e., work hour restrictions and supervision). Although we reached thematic saturation, our sampling of surgeons could have been broader. Given the small number of URM surgeons, procuring broader geographic representation was challenging. Furthermore, academic surgeons were disproportionately over-represented in the study. Finally, despite inviting a large number of female URM surgeons, we were unable to recruit a sample comparable in number to the sample of URM male surgeons. Our small sample of women likely did not permit full characterization of gender-based differences, over and above URM status or SES background, that women experience when becoming surgeons. The strengths of our study are successfully recruiting a sample of African-American and Latino surgeons whose childhood SES backgrounds, number of years in practice, and specialties differed, and who, nonetheless, described similar themes in their journey to becoming surgeons.
The number of URM applicants to general surgery will likely remain low as long as the overall number of URM applicants to medical school remains low. To increase URM interest in medicine, high school teachers and counselors should expose students to broad fields of study without limiting students’ opportunities according to the experiences they have had so far. Further, advisors of college (baccalaureate) students must create networks of opportunity and exposure to help students who are committed to reaching a goal find their way. Providing experiences and exposure to medicine and surgery during high school and college may require increased interactions with URM surgeons.
Surgical faculty may increase the entrance and completion of surgical training among URM applicants and learners by emphasizing the unique responsibility and meaningful physician-patient relationships surgeons value and enjoy. In addition, faculty must acknowledge the long hours and sacrifice needed to complete training and subsequently care for patients, but they must also emphasize the value of patient care and pride in restoring patient’s health and function. Pride in one’s work and commitment to care is likely a strong source of motivation for potential surgeons—as reflected in our sample. Finally, the leaders of medical schools, surgery residency programs, and other surgical institutions must realize that for some URM faculty, financial and perceptual barriers to a career in surgery remain, which require direct acknowledgement, discussion, and action.
In conclusion, the path to a career in surgery for African-American and Latino surgeons is heavily influenced by multiple factors. These factors include (1) perceived childhood SES, which in turn, affects a potential surgeon’s identity and expectations; (2) strong mentors who help navigate surgical culture; and (3) developing a sense of belonging. Our data suggest that future surgeons, especially URM trainees from low SES backgrounds, may benefit from identifying early aspirational figures and participating in a structured introduction into the rigors of the profession (e.g., a program or organization focused on the experience of URM physicians/surgeons). Further, deconstructing some of the negative norms surrounding surgery, which limit the inclusion of URM physicians and women, by promoting the values of providing high-quality patient care may make surgery more attractive to URM trainees.
Acknowledgments
The authors thank all of the participating surgeons for their time and generous support in completing this study. They also wish to thank Dr. Patricia O’Sullivan (University of California San Francisco School of Medicine) for her advice and support regarding the design and analysis of this qualitative study, and Pamela Derish, MA (Department of Surgery at the University of California San Francisco) for editing assistance.
Funding/Support: J.G. Ulloa was supported by the Veterans Affairs (VA) Office of Academic Affiliations through the VA/Robert Wood Johnson Clinical Scholars Program. G. Moreno received support from a National Institute on Aging (NIA) Paul B. Beeson Career Development Award (K23 AG042961-01), the American Federation for Aging Research, and the University of California Los Angeles Resource Center for Minority Aging Research/Center for Health Improvement of Minority Elderly (RCMAR/CHIME) under National Institutes of Health/NIA grant P30AG021684.
Footnotes
Other disclosures: None reported
Ethical approval: The study was approved by the University of California Los Angeles Human Research Protection Program.
Disclaimers: The content does not necessarily represent the official views of the National Institute on Aging or the National Institutes of Health.
Contributor Information
Jesus G. Ulloa, Surgery resident, Department of Surgery, University of California San Francisco, San Francisco, California. At the time of this research, he was a Robert Wood Johnson Foundation clinical scholar, University of California Los Angeles and Veterans Affairs, Los Angeles Health Service Research & Development Center of Innovation, Los Angeles, California.
Omar Viramontes, Medical student, David Geffen School of Medicine, University of California Los Angeles, Los Angeles, California.
Gery Ryan, Assistant dean, Academic Affairs, RAND Health, RAND Corporation, Santa Monica, California.
Kenneth Wells, Professor, Department of Psychiatry, David Geffen School of Medicine, University of California Los Angeles, Los Angeles, California.
Melinda Maggard-Gibbons, Assistant professor, Department of Surgery, David Geffen School of Medicine, University of California Los Angeles and Veterans Affairs, Los Angeles Health Service Research & Development Center of Innovation, Los Angeles, California.
Gerardo Moreno, Associate professor, Department of Family Medicine, Director of the PRIME Program, David Geffen School of Medicine, University of California Los Angeles, Los Angeles, California.
References
- 1.Association of American Medical Colleges. [Accessed April 17, 2018];Diversity in the Physician Workforce: Facts & Figures 2014. 2014 http://aamcdiversityfactsandfigures.org/
- 2.Butler PD, Longaker MT, Britt LD. Major deficit in the number of underrepresented minority academic surgeons persists. Annals of surgery. 2008;248:704–711. doi: 10.1097/SLA.0b013e31817f2c30. [DOI] [PubMed] [Google Scholar]
- 3.Smedley BD, Syme SL, editors. Promoting Health: Intervention Strategies from Social and Behavioral Research. Washington, DC: National Academies Press; 2000. [PubMed] [Google Scholar]
- 4.Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: The National Academies Press; 2003. [PubMed] [Google Scholar]
- 5.Sarto G. Of disparities and diversity: Where are we? Am J Obstet Gynecol. 2005;192:1188–1195. doi: 10.1016/j.ajog.2004.12.065. [DOI] [PubMed] [Google Scholar]
- 6.Komaromy M, Grumbach K, Drake M, et al. The role of Black and Hispanic physicians in providing health care for underserved populations. N Engl J Med. 1996;334:1305–1310. doi: 10.1056/NEJM199605163342006. [DOI] [PubMed] [Google Scholar]
- 7.Laveist TA, Nuru-Jeter A. Is doctor-patient race concordance associated with greater satisfaction with care? J Health Soc Behav. 2002;43:296–306. [PubMed] [Google Scholar]
- 8.American College of Surgeons. [Accessed April 17, 2018];Diversity at ACS. 2018 https://www.facs.org/about-acs/careers-at-acs/diversity.
- 9.Andriole DA, Jeffe DB. Certification by the American Board of Surgery among US medical school graduates. J Am Coll Surg. 2012;214:806–815. doi: 10.1016/j.jamcollsurg.2012.01.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Andriole DA, Jeffe DB, Schechtman KB. Is surgical workforce diversity increasing? Journal of the American College of Surgeons. 2007;204:469–477. doi: 10.1016/j.jamcollsurg.2006.12.035. [DOI] [PubMed] [Google Scholar]
- 11.Mahoney MR, Wilson E, Odom KL, Flowers L, Adler SR. Minority faculty voices on diversity in academic medicine: Perspectives from one school. Acad Med. 2008;83:781–786. doi: 10.1097/ACM.0b013e31817ec002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morse JM. The significance of saturation. Qual Health Res. 1995;5:147–149. [Google Scholar]
- 13.Boyatzis RE. Transforming Qualitative Information: Thematic Analysis and Code Development. Thousand Oaks, CA: Sage Publications; 1998. [Google Scholar]
- 14.Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 15.Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13:117. doi: 10.1186/1471-2288-13-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: A synthesis of recommendations. Acad Med. 2014;89:1245–1251. doi: 10.1097/ACM.0000000000000388. [DOI] [PubMed] [Google Scholar]
- 17.Ryan GW, Bernard HR. Techniques to Identify Themes. Field Methods. 2003;15:85–109. [Google Scholar]
- 18.Freeman BK, Landry A, Trevino R, Grande D, Shea JA. Understanding the leaky pipeline: Perceived barriers to pursuing a career in medicine or dentistry among underrepresented-in-medicine undergraduate students. Acad Med. 2016;91:987–993. doi: 10.1097/ACM.0000000000001020. [DOI] [PubMed] [Google Scholar]
- 19.Cooper RA. Impact of trends in primary, secondary, and postsecondary education on applications to medical school. II: Considerations of race, ethnicity, and income. Acad Med. 2003;78:864–876. doi: 10.1097/00001888-200309000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Butler PD, Silverstein SM, Dakin SC. Visual perception and its impairment in schizophrenia. Biological psychiatry. 2008;64:40–47. doi: 10.1016/j.biopsych.2008.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Butler PD, Britt LD, Richard CE, et al. The diverse surgeons’ initiative: Longitudinal assessment of a successful national program. Journal of the American College of Surgeons. 2015;220:362–369. doi: 10.1016/j.jamcollsurg.2014.12.006. [DOI] [PubMed] [Google Scholar]
- 22.Wong RL, Sullivan MC, Yeo HL, Roman SA, Bell RH, Jr, Sosa JA. Race and surgical residency: Results from a national survey of 4339 US general surgery residents. Annals of Surgery. 2013;257:782–787. doi: 10.1097/SLA.0b013e318269d2d0. [DOI] [PubMed] [Google Scholar]