Abstract
Many children with autism spectrum disorder display challenging behaviors. These behaviors are not limited to those with cognitive and/or language impairments. The Collaborative and Proactive Solutions framework proposes that challenging behaviors result from an incompatibility between environmental demands and a child’s “lagging skills.” The primary Collaborative and Proactive Solutions lagging skills—executive function, emotion regulation, language, and social skills— are often areas of weakness for individuals with autism spectrum disorder. The purpose of this study was to evaluate whether these lagging skills are associated with challenging behaviors in youth with autism spectrum disorder without intellectual disability. Parents of 182 youth with autism spectrum disorder (6–15 years) completed measures of their children’s challenging behaviors, executive function, language, emotion regulation, and social skills. We tested whether the Collaborative and Proactive Solutions lagging skills predicted challenging behaviors using multiple linear regression. The Collaborative and Proactive Solutions lagging skills explained significant variance in participants’ challenging behaviors. The Depression (emotion regulation), Inhibit (executive function), and Sameness (executive function) scales emerged as significant predictors. Impairments in emotion regulation and executive function may contribute substantially to aggressive and oppositional behaviors in school-age youth with autism spectrum disorder without intellectual disability. Treatment for challenging behaviors in this group may consider targeting the incompatibility between environmental demands and a child’s lagging skills.
Keywords: autism spectrum disorder, challenging behaviors, cognitive-behavioral treatment, emotion regulation, executive function
Many children with autism spectrum disorder (ASD) display challenging behaviors, including aggression and oppositionality, which can result in a multitude of negative outcomes, such as physical injury, significant interference with daily activities, and impaired quality of life for the child and their family members. Challenging behaviors in youth with ASD have been found to be more associated with parent and teacher stress than any other child or caregiver characteristic (Lecavalier et al., 2006). In addition, aggression is the chief presenting complaint of children with ASD who complete an inpatient psychiatric stay (Siegel and Gabriels, 2014). The purpose of this study was to examine challenging behaviors in youth with ASD without intellectual disability (ID) in the context of the Collaborative and Proactive Solutions (CPS) framework (formerly Collaborative Problem Solving) (Greene, 2010).
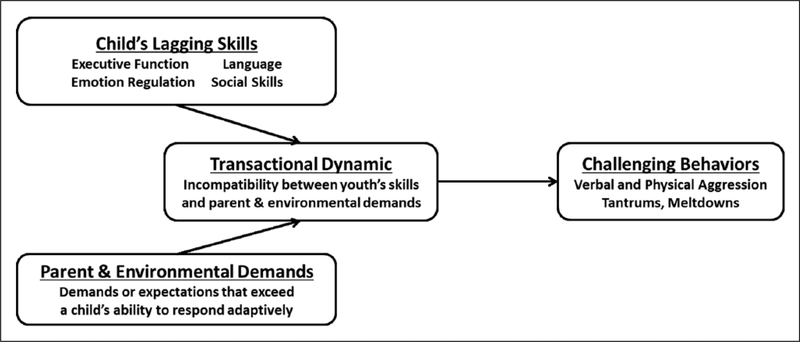
CPS is an evidence-based cognitive-behavioral treatment designed to reduce challenging behaviors in school-age children with oppositional defiant disorder (ODD) and attention-deficit/hyperactivity disorder (e.g. Greene, 2010; Greene et al., 2004, 2006; Johnson et al., 2012; Ollendick et al., 2016). The CPS framework is based on several key concepts thought to underlie challenging behaviors. As shown in Figure 1, these concepts include a child’s “lagging” or impaired skills, environmental demands, and the degree of fit or compatibility between these child characteristics and environmental characteristics. Instead of viewing a child’s challenging behavior as willful (i.e. “My child won’t do what I ask”), the CPS framework emphasizes the incompatibility between environmental demands and the child’s lagging skills (i.e. “My child can’t do what I ask”), which leads to challenging behaviors. As an example of child-environment incompatibility, consider a child with executive function impairments who lacks the skills to independently complete his homework in a brief time period. When this child’s parent insists that he complete his homework before dinnertime, a mismatch between the child’s skills and environmental demands occurs.
Figure 1.
Collaborative and Proactive Solutions (CPS) framework (e.g. Greene, 2010).
This study focused on the lagging skills component of CPS. According to the transactional and reciprocal CPS framework, a child’s lagging skills increase the likelihood of child-environment incompatibility, which in turn gives rise to challenging behaviors (Greene and Doyle, 1999). The primary CPS lagging skills include executive function (e.g. limited working memory, poor impulse control), emotion regulation (e.g. emotional reactivity, chronic irritability and/or anxiety), language (e.g. limited expressive language, difficulty with language processing), and social skills (e.g. poor perception of social cues, difficulty starting conversations). The CPS framework also delineates cognitive flexibility as a lagging skill (e.g. black-and-white thinking, difficulty deviating from rules or routine) that is distinct from executive function; however, given that literature largely supports cognitive flexibility as an executive function skill (Miyake et al., 2000), we included it under the executive functioning domain for the purposes of this article.
CPS treats challenging behaviors by (1) targeting the way parents and children collaboratively and proactively identify, communicate about, and attempt to resolve problems and (2) building skills that will prevent challenging behaviors in the future. The initial focus of treatment is helping parents conceptualize their child’s challenging behavior as the byproduct of incompatibility between environmental demands and the child’s lagging skills. This includes identifying the child’s specific skill impairments related to challenging behavior and prioritizing unsolved problems. Next, parents learn a structure for engaging in a collaborative discussion with their child, and they practice these discussions in session with the child to address unsolved problems. Parents and children learn to articulate their own concerns, understand the other person’s concerns, and generate collaborative solutions. By focusing on the concerns presented by both the youth and the parent, there is no punitive emphasis on blame or “willful” behavior, freeing up families to focus on what the child would do if he or she had the skills to do it. A recent randomized controlled trial demonstrated that CPS is an effective treatment for youth aged 7–14 years with ODD, with treatment gains from 12 75-min sessions maintained at 6-month follow-up (Ollendick et al., 2016). However, this trial specifically excluded children with ASD. No previous studies have examined the effects of CPS for youth with ASD and challenging behaviors.
The lack of CPS research with youth with ASD is surprising because all of the lagging skills targeted in CPS are often areas of weakness for individuals with ASD (e.g. American Psychiatric Association (APA), 2013; Corbett et al., 2009; Granader et al., 2014; Mazefsky et al., 2013). In addition, emerging evidence supports the notion that specific skill impairments may contribute to challenging behaviors in youth with ASD. For example, Lawson et al. (2015) found that executive function problems, specifically greater cognitive and behavioral inflexibility, predicted parent-reported challenging behaviors in 70 children with ASD. Another study of individuals aged 8–20 years found that those with ASD, compared to typically developing control participants, use cognitive reappraisal (an adaptive emotion regulation strategy) less frequently, leading to increased levels of challenging behaviors (Samson et al., 2015). However, to the best of our knowledge, no previous studies have examined the CPS lagging skills of executive function, emotion regulation, language, and social skills together in a model predicting challenging behaviors in people with ASD.
Considering the relationship between lagging skills, environmental demands, and challenging behaviors raises an important question about whether a diagnosis of ODD is appropriate for a child with ASD. A large proportion of school-age children with ASD exhibit ODD symptoms (e.g. Gadow et al., 2005). Nearly 30% of a population-derived sample of youth with ASD met diagnostic criteria for ODD based on a standardized parent interview (Simonoff et al., 2008), which is a much higher rate than the average prevalence estimate of ODD in the general population (3.3%) (APA, 2013). However, the label of ODD implies that the problem resides solely within the child, taking a unidirectional approach and failing to consider the interaction between lagging skills and environmental demands that exceed a child’s capacity to respond adaptively.
The majority of current treatments for challenging behaviors in youth with ASD do not explicitly target the incompatibility between a child’s skills and environmental demands. From a psychopharmacological perspective, the treatment target has been to reduce irritability, which is thought to underlie the challenging behaviors. The Food and Drug Administration (FDA) has approved the use of risperidone and aripiprazole for reducing irritability in ASD based on several randomized controlled trials (Marcus et al., 2009; Owen et al., 2009; Research Units on Pediatric Psychopharmacology Autism Network (RUPP-AN), 2002; Shea et al., 2004). While no other medication carries FDA approval in ASD, several others have been shown to improve irritability when used either as monotherapy or adjunctively (Ghanizadeh and Moghimi-Sarani, 2013; Gordon et al., 1993; Jaselskis et al., 1992; Posey et al., 2004). However, all of these pharmacological interventions carry a risk of adverse events, and in the case of risperidone and aripiprazole, serious health complications (Correll and Carlson, 2006; Correll et al., 2006; De Castro et al., 2008; Roke et al., 2009; Safer, 2004). This profile has led to the extensive monitoring of patients on second-generation antipsychotics with baseline, quarterly, semi-annual, and annual lab tests, which are often difficult for children with ASD.
Traditional psychosocial treatments for challenging behaviors in school-age children with ASD include applied behavior analysis (e.g. Vismara and Rogers, 2010) or other behavioral strategies (e.g. Machalicek et al., 2007) and parent training (e.g. Bearss et al., 2013; Solomon et al., 2008). These approaches rely on behavioral principles to create or modify reinforcers in the child’s environment, with the desired target of behavioral compliance. In non- ASD populations, these treatments are less effective for older children and adolescents because the sole reliance on behavioral principles is no longer developmentally appropriate (Frick, 2001). CPS may be a more appealing and effective treatment for this older age group, given its focus on lagging skills, parent-child collaboration to develop mutually beneficial goals, and self-determination in children. Furthermore, CPS is in line with a recent call for clinicians to provide treatments that promote autonomy and self-determination in individuals with ASD (Hodgetts and Park, 2017).
This study focused on school-age youth with ASD without ID because they are often overlooked in research on challenging behaviors, despite recent findings that this group is highly likely to engage in challenging behaviors. In a Simons Simplex Collection study of 1380 youth with ASD aged 4–17 years (Kanne and Mazurek, 2011), parents reported that 56% of youth currently demonstrated physical aggression toward a caregiver or family member, and 32% toward non-caregivers or nonfamily members, as assessed by the Autism Diagnostic Interview-Revised (ADI-R) (Lord et al., 1994) items about aggression. Lifetime history rates of aggression were 68% and 49% toward family members and nonfamily members, respectively. Aggression was unrelated to IQ, clinician-rated ASD symptom severity, gender, parental marital status, parental education level, or receptive communication abilities. Mazurek et al. (2013) also found no relationship between aggression and IQ in an ASD sample from the Autism Treatment Network (ATN). The current rate of physical aggression in their sample of 1584 youth with ASD aged 2–17 years was 53.7%, as reported by parents using a single item from the ATN Parent Survey. These two studies are limited in that only a few items assess aggression and they are not age/sex-normed; however, collectively, these two large-scale studies highlight that aggression in ASD is not restricted to those with severe cognitive and/or language impairments.
The aim of this study was to evaluate whether the CPS lagging skills are associated with challenging behaviors in school-age children with ASD without ID. We defined challenging behavior to include physical aggression (e.g. hitting other children), verbal aggression (e.g. teasing others), and oppositionality (e.g. arguing with parents). We hypothesized that the CPS lagging skills would explain significant variance in our participants’ challenging behaviors, given that youth with ASD often demonstrate deficits in the lagging skills proposed to be relevant. No a priori hypotheses were made about which skills would best explain variance in challenging behaviors in children with ASD.
Methods
Participants
A total of 182 youth with ASD were included in this study (172 males; age: 6–15.58 years, M = 9.32, SD = 2.25; IQ: 70–165, M = 104.26, SD = 18.67; 80.8% White; 8.2% Hispanic; 7.7% Biracial; 6.0% Black; 1.6% Asian). All children met the Diagnostic and Statistical Manual of Mental Disorders, 4th ed., text rev. (DSM-IV-TR) (APA, 2000) diagnostic criteria for autistic disorder, Asperger’s disorder, or pervasive developmental disorder—not otherwise specified, with expert clinical opinion informed by the Autism Diagnostic Observation Schedule, 2nd ed. (Lord et al., 2012) and the ADI-R (Lord et al., 1994). Additional inclusionary criteria were an age of 6–17 years and an IQ score >70, as determined by The Differential Abilities Scale, 2nd ed. (DAS-II) (Elliott, 2007) (n = 147) or the Wechsler Abbreviated Scale of Intelligence (WASI) (Psychological Corporation, 1999) (n = 35) during the study visit. Of the 182 participants, 147 were collected at the Center for Autism Research at the Children’s Hospital of Philadelphia and 35 were collected at the Center for Autism Spectrum Disorders at Children’s National Health System. A subset of the participants (30%) was taking psychotropic medications, including stimulants (24%), alpha 2A agonists (15%), selective serotonin reuptake inhibitors (9%), atypical antipsychotics (7%), norepinephrine-dopamine reuptake inhibitors (3%), mood stabilizers (2%), non-benzodiazapine anxiolytics (0.5%), and tricyclic antidepressants (0.5%).
Measures
The dependent variable of Challenging Behaviors was measured by the Aggression scale of the parent-reported Behavior Assessment System for Children, 2nd ed. (BASC- 2) (Reynolds and Kamphaus, 2004). This scale captures not only physical aggression (e.g. “hits other children”) but also verbal aggression (e.g. “teases others”) and ODD symptoms (e.g. “argues with parents,” “annoys others on purpose,” and “loses temper too easily”). The BASC-2 assesses both adaptive and problematic behaviors in youth. Higher T-scores reflect concerns on the clinical scales (e.g. aggression, anxiety), while lower T-scores denote problems on the adaptive scales (e.g. social skills).
The CPS lagging skills were all measured by parent report, with specific scales selected to best map onto the CPS assessment of lagging skills (Greene, 2010). Executive Function included the Inhibition, Working Memory, Shift, and Planning scales of the Behavior Rating Inventory of Executive Function—Parent form (BRIEF) (Gioia et al., 2000), along with the Sameness Behavior subscale of the Repetitive Behaviors Scale-Revised (RBS-R) (Bodfish et al., 2000). The BRIEF is a measure of executive function in everyday situations. Results are reported as T-scores, with higher scores indicating greater impairment. The RBS-R is an informant-report of the frequency and severity of repetitive behaviors in individuals with ASD. Items are rated from 0 (behavior does not occur) to 3 (behavior occurs and is a severe problem). The RBS-R Sameness subscale and BRIEF Shift scale both capture cognitive inflexibility in their focus on resistance to change and difficulty with transitions (Bodfish et al., 2000; Gioia et al., 2000). Emotion Regulation was measured by the Anxiety and Depression scales of the BASC-2, which capture impairments in the ability to manage negative feelings. Social Skills included the Social Skills scale of the BASC-2 and the Social Responsiveness Scale (SRS) (Constantino and Gruber, 2005) total score. The SRS is a 65-item informant-report of ASD-related social impairments, including social awareness, social information processing, reciprocal social communication, social motivation, and restricted interests/ repetitive behaviors. Higher T-scores indicate more autistic traits. Language was measured by the Communication domain of the Vineland Adaptive Behavior Scales, 2nd ed. (VABS-2) (Sparrow et al., 2005). The VABS-2 is an assessment of adaptive behaviors, with lower standard scores (M = 100; SD = 15) indicating lower adaptive skills.
Procedures
Data were drawn from multiple studies at the Center for Autism Research at the Children’s Hospital of Philadelphia and the Center for Autism Spectrum Disorders at Children’s National Health System, all with Institutional Review Board approval. Participants were not specifically recruited for a research study on challenging behaviors. Prior to participation, consent was obtained from all legal guardians, and assent was obtained from all children. All participants and their guardians completed a battery of measures. If participants were re-recruited from prior studies within 1 year, diagnostic and cognitive tests were not repeated. All measures were completed within 12 months of our primary outcome measure (BASC-2).
Data analyses
All statistical analyses were conducted using SPSS version 22. A descriptive analysis was initially completed to quantify distribution and any potential skew or kurtosis within the sample. All regression models included challenging behaviors as the dependent variable, with age, IQ, and recruitment site entered in the first block as covariates of no interest. We also ran all models without these covariates and found the same pattern of results, so we retained the covariates for completeness in the presented results. Each CPS skill was first examined individually (with the component scales entered as separate variables into the second block) to determine whether it could successfully explain variance in challenging behaviors, above and beyond the covariates. Next, to determine the variables contributing the most variance (i.e. best predictors), all component scales from the four CPS skills were entered into the second block simultaneously to explain variance in challenging behaviors.
Results
Descriptive statistics are presented in Table 1. A total of 41 participants (22.5% of the total sample) fell in the At-Risk or Clinically Significant classification range for challenging behaviors. Results of the linear regression analyses with each of the four lagging skills entered into the model separately are presented in Table 2. Participant age, participant IQ, and recruitment site were not significant predictors of challenging behaviors (p = 0.496). With each CPS skill entered into the model separately to examine the unique variance contributed by each lagging skill area, executive function, emotion regulation, and social skills each explained significant variance in challenging behaviors, above age, IQ, and recruitment site. The only non-significant lagging skill predictor was language (p = 0.107). As for the component scales, the Inhibit (executive function skill), Sameness (executive function skill), Anxiety (emotion regulation skill), and Depression (emotion regulation skill) scales, along with the SRS total (social skills), were all significant predictors of challenging behaviors. The model with all CPS skills entered together explained 40% of the variance in challenging behaviors, after adjusting for the total number of variables (Table 3). In this combined model, only the Depression (emotion regulation skill), Inhibit (executive function skill), and Sameness (executive function skill) scales were significant predictors. Depression, our index of emotion regulation skills (e.g. is easily upset, cries easily, changes moods quickly), was the strongest predictor of challenging behaviors.
Table 1.
Descriptive statistics for study measures (n = 182).
| Mean (SD) | Min-Max | % ≥ T-score of 60 | |
|---|---|---|---|
| Challenging behaviors | |||
| BASC-2 Aggression | 51.74 (11.19) | 32–97 | 22.5 |
| Executive function | |||
| BRIEF Inhibit | 62.91 (11.44) | 37–88 | 61.5 |
| BRIEF Working Memory | 66.03 (10.84) | 38–87 | 77.5 |
| BRIEF Planning | 64.20 (10.60) | 33–87 | 66.5 |
| BRIEF Shift | 69.63 (11.59) | 40–95 | 84.6 |
| RBS-R Sameness | 7.02 (5.17) | 0–27 | − |
| Emotion regulation | |||
| BASC-2 Anxiety | 53.58 (12.92) | 17–91 | 28.6 |
| BASC-2 Depression | 56.85 (12.61) | 35–103 | 34.1 |
| Social skills | |||
| BASC-2 Social Skills | 39.41 (9.15) | 20–65 | 62.6a |
| SRS Total | 77.59 (12.69) | 45–114 | 93.4 |
| Mean (SD) | Min-Max | % ≤ SS of 85 | |
| Language | |||
| VABS-2 Communication | 86.15 (14.89) | 54–125 | 53.0 |
BASC-2: Behavior Assessment System for Children (2nd ed.); BRIEF: Behavior Rating Inventory of Executive Function; RBS-R: Repetitive Behavior Scale-Revised; SRS: Social Responsiveness Scale; VABS-2: Vineland Adaptive Behavior Scales (2nd ed.); SS: standard score.
All measures were parent-reported. All measures produce a T-score, except for the RBS-R (raw score) and VABS-2 (standard score). Only 179 participants had RBS-R scores, and 181 participants had VABS-2 scores. Total scores on the RBS-R Sameness subscale can range from 0 (indicating that behaviors do not occur) to 33 (indicating that all 11 behaviors listed occur in a severely problematic manner).
Reflects the percentage of participants with a T-score ⩽ 40 because the Social Skills scale is an adaptive scale, with lower scores indicating more problems.
Table 2.
Results of linear regressions with each CPS skill entered separately.
| Model | R2 | Adjusted R2 | F-change | B | t |
|---|---|---|---|---|---|
| Step 1 | 0.013 | −0.003 | 0.799 | ||
| Age | −0.075 | −0.992 | |||
| IQ | 0.006 | 0.079 | |||
| Recruitment site | −0.083 | −1.059 | |||
| Step 2 (each skill entered separately) | |||||
| Executive function | 0.289 | 0.259 | 13.595** | ||
| BRIEF Inhibit | 0.369** | 4.534 | |||
| BRIEF Working Memory | −0.078 | −0.789 | |||
| BRIEF Planning | 0.097 | 0.930 | |||
| BRIEF Shift | 0.085 | 0.981 | |||
| RBS-R Sameness | 0.171* | 2.208 | |||
| Emotion regulation | 0.364 | 0.346 | 48.517** | ||
| BASC-2 Anxiety | −0.180* | −2.510 | |||
| BASC-2 Depression | 0.681** | 9.401 | |||
| Social skills | 0.135 | 0.110 | 12.326** | ||
| BASC-2 Social Skills | −0.026 | −0.327 | |||
| SRS Total | 0.341** | 4.266 | |||
| Language | 0.040 | 0.018 | 2.621 | ||
| VABS-2 Communication | −0.137 | −1.619 |
BRIEF: Behavior Rating Inventory of Executive Function; RBS-R: Repetitive Behavior Scale-Revised; BASC-2: Behavior Assessment System for Children (2nd ed.); SRS: Social Responsiveness Scale; VABS-2: Vineland Adaptive Behavior Scales (2nd ed.).
For each CPS skill, the component scales were entered together in the same block.
p < 0.05
p < 0.001.
Table 3.
Results of linear regression with CPS skills entered together.
| Models | R2 | Adjusted R2 | F-change | B | t |
|---|---|---|---|---|---|
| Model 1 (covariates only) | 0.025 | 0.008 | 1.502 | ||
| Age | −0.085 | −1.124 | |||
| IQ | 0.016 | 0.201 | |||
| Recruitment site | −0.132 | −1.675 | |||
| Model 2 | 0.446 | 0.402 | 12.473** | ||
| Covariates | |||||
| Executive function | |||||
| BRIEF Inhibit | 0.273** | 3.507 | |||
| BRIEF Working Memory | −0.048 | −0.534 | |||
| BRIEF Planning | 0.030 | 0.314 | |||
| BRIEF Shift | −0.008 | −0.090 | |||
| RBS-R Sameness | 0.158* | 2.188 | |||
| Emotion regulation | |||||
| BASC-2 Anxiety | −0.123 | −1.515 | |||
| BASC-2 Depression | 0.494** | 6.119 | |||
| Social skills | |||||
| BASC-2 Social Skills | −0.093 | −1.310 | |||
| SRS Total | −0.024 | −0.265 | |||
| Language | |||||
| VABS-2 Communication | 0.112 | 1.527 |
BRIEF: Behavior Rating Inventory of Executive Function; RBS-R: Repetitive Behavior Scale -Revised; BASC-2: Behavior Assessment System for Children (2nd ed.); SRS: Social Responsiveness Scale; VABS-2: Vineland Adaptive Behavior Scales (2nd ed.).
p < 0.05
p < 0.001.
Discussion
Our data support the association between CPS lagging skills and challenging behaviors in youth with ASD without ID. According to the CPS framework, a variety of child characteristics may contribute to an incompatibility with environmental demands, and these lagging skills can differ between children exhibiting challenging behaviors (e.g. Greene, 2010). This study demonstrates that impairments in emotion regulation and executive function may particularly contribute to challenging behaviors in school-age children with ASD without ID, which is consistent with recent research (Lawson et al., 2015; Patel et al., 2016; Samson et al., 2015). Specifically, our findings suggest that an emotionally dysregulated or irritable child with ASD, limited impulse control, and cognitive inflexibility is more likely to engage in challenging behaviors. In this sample, language impairment was not a significant predictor of challenging behaviors, which supports the notion that not all skills must be lagging to increase the likelihood of challenging behaviors.
In our sample of youth with ASD without ID, 22.5% fell in the At-Risk or Clinically Significant classification range for challenging behaviors. This rate is notably lower than the rates of physical aggression found in two recent large-scale studies (Kanne and Mazurek, 2011; Mazurek et al., 2013), which is likely due to differences in measure- ment. The two large-scale studies relied on a single question to assess whether or not aggression was present. We used the Aggression scale of the BASC-2, a normed behavioral rating scale that produces standardized scores. Our rate of 22.5% is similar to the percentage of children with ASD and significant ODD symptoms found in other studies using normed, dimensional measures (e.g. Gadow et al., 2005).
This study is the first investigation of the CPS lagging skills in children with ASD. Our focus on school-age youth without ID is important because this group is often overlooked in research on aggression and other disruptive behaviors. Similar to two large-scale studies that included youth both with and without ID (Kanne and Mazurek, 2011; Mazurek et al., 2013), we found no relationship between IQ and challenging behaviors, which highlights that aggressive and oppositional behaviors are common problems across the range of cognitive functioning.
Based on our preliminary findings, and assuming a causal relationship between the risk factors identified here and challenging behaviors, treatment for challenging behaviors in school-age youth with ASD without ID may need to specifically target the child’s emotion regulation and executive function difficulties. This could be accomplished in a number of ways, including cognitive-behavioral therapy targeting emotion dysregulation, cognitive training therapy for executive function (e.g. Unstuck and On Target) (Kenworthy et al., 2014), or CPS. CPS would target these skills in situations where there is an incompatibility between environmental demands and a child’s lagging skills. Although previous CPS studies have specifically excluded children with ASD from trial participation (e.g. Johnson et al., 2012; Ollendick et al., 2016), the lagging skills targeted in CPS are common areas of weakness for individuals with ASD (e.g. APA, 2013; Granader et al., 2014; Mazefsky et al., 2013), making them good targets for intervention. In addition, a growing literature on effective cognitive-behavioral interventions for co-occurring symptoms in ASD, such as anxiety (e.g. Reaven et al., 2012; Storch et al., 2013) and executive functioning impairment (Kenworthy et al., 2014), supports the use of adapting a cognitive-behavioral approach such as CPS for treating challenging behaviors in this population. Thus, future treatment studies aimed at reducing challenging behaviors in youth with ASD may consider evaluating CPS as another treatment option; furthermore, it is likely that CPS will need modifications to account for the unique learning styles and unsolved problems of youth with ASD (Lang et al., 2010).
The primary limitation of this study is that we were only able to examine the child-level variable of lagging skills, which is just one of the components of CPS. We had no measures of environmental demands or parental expectations that comprise the other half of the dynamic translation that CPS posits as causal to challenging behaviors. Future investigations can probe for interactions between lagging skills and environmental demands or parental expectations that give rise to challenging behaviors. The study was also limited in the sole reliance on cross-sectional data and parent-reported measures. We conducted secondary analyses with data drawn from multiple studies, meaning that we did not design a study a priori to examine the CPS lagging skills with ideal measures. At the same time, a strength of the study is that our recruitment materials did not bias the sample in favor of families experiencing challenging behaviors. Of note, the participants were not assessed for comorbid psychiatric diagnoses, and it is possible that elevations on the Depression scale, our index of emotion regulation skills, reflect a comorbid depression diagnosis. Follow-up studies with more in-depth clinical phenotyp-ing are needed to confirm these findings, especially longitudinal studies to examine which lagging skills best predict future challenging behaviors in youth with ASD. Longitudinal research could also investigate the potential interaction between the child’s age and lagging skills in the prediction of challenging behaviors. Similarly, future research could use multi-informant, multi-method approaches and examine which types of environmental factors are most likely to exceed a child’s capacity to respond adaptively. In CPS, these factors are typically described as environmental demands or parental expectations; however, other possibilities that may be particularly problematic for children with ASD include sensory input or a change in routine (APA, 2013).
In conclusion, this study is the first to demonstrate that the CPS lagging skills may be useful for understanding challenging behaviors in older children with ASD without ID. Indeed, our findings suggest that children with lagging skills in emotion regulation and executive function are more likely to exhibit challenging behaviors. This study contributes to a burgeoning literature quantifying challenging behaviors in children with ASD without ID. Future research can determine whether emotion regulation and executive function impairments predict later challenging behavior, and whether the CPS treatment is effective in children with ASD without ID.
Acknowledgements
Portions of these findings were presented at the 2016 International Meeting for Autism Research. Lauren Kenworthy is a co-author of the BRIEF and receives royalty payments from its publisher. The other authors of this article report no conflicts of interest.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by funding from the National Institute of Mental Health (K23MH086111, PI: B.E.Y.; R21MH092615, PI: B.E.Y.; RC1MH088791, PI: R.T.S.) and the National Institute of Child Health and Human Development (P30HD040677; PI: V.G.), a New Program Development Award to B.E.Y. through the Intellectual and Developmental Disabilities Research Center funded by the National Institute of Child and Human Development (P30HD026979, PI: M.Y.), a grant from the Philadelphia Foundation (PI: B.E.Y.), grants from the Pennsylvania Department of Health (SAP #4100042728, SAP #4100047863) to R.T.S., a grant from Pfizer to R.T.S., a grant from the Robert Wood Johnson Foundation (#6672) to R.T.S., the Isadore and Bertha Gudelsky Family Foundation, and the Singer Family Foundation.
References
- American Psychiatric Association (APA) (2000) Diagnostic and Statistical Manual of Mental Disorders. 4th ed. (text revision). Washington, DC: APA. [Google Scholar]
- American Psychiatric Association (APA) (2013) Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: APA. [Google Scholar]
- Bearss K, Lecavalier L, Minshawi N, et al. (2013) Toward an exportable parent training program for disruptive behaviors in autism spectrum disorders. Neuropsychiatry 3(2): 169–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodfish JW, Symons FJ, Parker DE, et al. (2000) Varieties of repetitive behavior in autism: comparisons to mental retardation. Journal of Autism and Developmental Disorders 30(3): 237–243. [DOI] [PubMed] [Google Scholar]
- Constantino JN and Gruber CP (2005) Social Responsiveness Scale (SRS). Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Corbett BA, Constantine LJ, Hendren R, et al. (2009) Examining executive functioning in children with autism spectrum disorder, attention deficit hyperactivity disorder and typical development. Psychiatry Research 166(2–3): 210–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Correll CU and Carlson HE (2006) Endocrine and metabolic adverse effects of psychotropic medications in children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry 45(7): 771–791. [DOI] [PubMed] [Google Scholar]
- Correll CU, Penzner JB, Parikh UH, et al. (2006) Recognizing and monitoring adverse events of second-generation antipsychotics in children and adolescents. Child and Adolescent Psychiatric Clinics of North America 15(1): 177–206. [DOI] [PubMed] [Google Scholar]
- De Castro MJ, Fraguas D, Laita P, et al. (2008) QTc changes after 6 months of second-generation antipsychotic treatment in children and adolescents. Journal of Child and Adolescent Psychopharmacology 18(4): 381–383. [DOI] [PubMed] [Google Scholar]
- Elliott CD (2007) The Differential Abilities Scale. 2nd ed. San Antonio, TX: Harcourt Assessments, Inc. [Google Scholar]
- Frick PJ (2001) Effective interventions for children and adolescents with conduct disorder. Canadian Journal of Psychiatry 46(7): 597–608. [DOI] [PubMed] [Google Scholar]
- Gadow KD, DeVincent CJ, Pomeroy J, et al. (2005) Comparison of DSM-IV symptoms in elementary school-age children with PDD versus clinic and community samples. Autism 9(4): 392–415. [DOI] [PubMed] [Google Scholar]
- Ghanizadeh A and Moghimi-Sarani E (2013) A randomized double blind placebo controlled clinical trial of N-Acetylcysteine added to risperidone for treating autistic disorders. BMC Psychiatry 13: 196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gioia GA, Isquith PK, Guy SC, et al. (2000) Behavior Rating Inventory of Executive Function. Lutz, FL: Psychological Assessment Resources. [Google Scholar]
- Gordon CT, State RC, Nelson JE, et al. (1993) A double-blind comparison of clomipramine, desipramine, and placebo in the treatment of autistic disorder. Archives of General Psychiatry 50(6): 441–447. [DOI] [PubMed] [Google Scholar]
- Granader Y, Wallace GL, Hardy KK, et al. (2014) Characterizing the factor structure of parent reported executive function in autism spectrum disorders: the impact of cognitive inflexibility. Journal of Autism and Developmental Disorders 44(12): 3056–3062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene RW (2010) Collaborative problem solving In: Murrihy RC, Kidman AD and Ollendick TH (eds) Clinical Handbook of Assessing and Treating Conduct Problems in Youth. New York: Springer, pp.193–220. [Google Scholar]
- Greene RW, Ablon JS and Martin A (2006) Innovations: child and adolescent psychiatry: use of collaborative problem solving to reduce seclusion and restraint in child and adolescent inpatient units. Psychiatric Services 57(5): 610–612. [DOI] [PubMed] [Google Scholar]
- Greene RW, Ablon JS, Monuteaux M, et al. (2004) Effectiveness of collaborative problem solving in affectively dysregulated youth with oppositional defiant disorder: initial findings. Journal of Consulting and Clinical Psychology 72(6): 1157–1164. [DOI] [PubMed] [Google Scholar]
- Greene RW and Doyle AE (1999) Toward a transactional conceptualization of oppositional defiant disorder: implications for assessment and treatment. Clinical Child and Family Psychology Review 2(3): 129–148. [DOI] [PubMed] [Google Scholar]
- Hodgetts S and Park E (2017) Preparing for the future: a review of tools and strategies to support autonomous goal setting for children and youth with autism spectrum disorders. Disability and Rehabilitation 39(6): 535–543. [DOI] [PubMed] [Google Scholar]
- Jaselskis CA, Cook EH, Fletcher KE, et al. (1992) Clonidine treatment of hyperactive and impulsive children with autistic disorder. Journal of Clinical Psychopharmacology 12(5): 322–327. [PubMed] [Google Scholar]
- Johnson M, Östlund S, Fransson G, et al. (2012) Attention- deficit/hyperactivity disorder with oppositional defiant disorder in Swedish children: an open study of collaborative problem solving. Acta Paediatrica 101(6): 624–630. [DOI] [PubMed] [Google Scholar]
- Kanne SM and Mazurek MO (2011) Aggression in children and adolescents with ASD: prevalence and risk factors. Journal of Autism and Developmental Disorders 41(7): 926–937. [DOI] [PubMed] [Google Scholar]
- Kenworthy L, Anthony LG, Naiman DQ, et al. (2014) Randomized controlled effectiveness trial of executive function intervention for children on the autism spectrum. Journal of Child Psychology and Psychiatry 55(4): 374–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang R, Regester A, Lauderdale S, et al. (2010) Treatment of anxiety in autism spectrum disorders using cognitive behaviour therapy: a systematic review. Developmental Neurorehabilitation 13(1): 53–63. [DOI] [PubMed] [Google Scholar]
- Lawson RA, Papadakis AA, Higginson CI, et al. (2015) Everyday executive function impairments predict comorbid psychopathology in autism spectrum and attention deficit hyperactivity disorders. Neuropsychology 29(3): 445–453. [DOI] [PubMed] [Google Scholar]
- Lecavalier L, Leone S and Wiltz J (2006) The impact of behaviour problems on caregiver stress in young people with autism spectrum disorders. Journal of Intellectual Disability Research 50(3): 172–183. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M and Le Couteur A (1994) Autism diagnostic interview-revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders 24(5): 659–685. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore PC, et al. (2012) Autism Diagnostic Observation Schedule. 2nd ed. Torrance, CA: Western Psychological Services. [Google Scholar]
- Machalicek W, O’Reilly MF, Beretvas N, et al. (2007) A review of interventions to reduce challenging behavior in school settings for students with autism spectrum disorders. Research in Autism Spectrum Disorders 1(3): 229–246. [Google Scholar]
- Marcus RN, Owen R, Kamen L, et al. (2009) A placebo-controlled, fixed-dose study of aripiprazole in children and adolescents with irritability associated with autistic disorder. Journal of the American Academy of Child and Adolescent Psychiatry 48(11): 1110–1119. [DOI] [PubMed] [Google Scholar]
- Mazefsky CA, Herrington J, Siegel M, et al. (2013) The role of emotion regulation in autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry 52(7): 679–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazurek MO, Kanne SM and Wodka EL (2013) Physical aggression in children and adolescents with autism spectrum disorders. Research in Autism Spectrum Disorders 7(3): 455–465. [Google Scholar]
- Miyake A, Friedman NP, Emerson MJ, et al. (2000) The unity and diversity of executive functions and their contributions to complex “frontal lobe” tasks: a latent variable analysis. Cognitive Psychology 41(1): 49–100. [DOI] [PubMed] [Google Scholar]
- Ollendick TH, Greene RW, Austin KE, et al. (2016) Parent management training and collaborative & proactive solutions: a randomized control trial for oppositional youth. Journal of Clinical Child and Adolescent Psychology 45(5): 591–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owen R, Sikich L, Marcus RN, et al. (2009) Aripiprazole in the treatment of irritability in children and adolescents with autistic disorder. Pediatrics 124(6): 1533–1540. [DOI] [PubMed] [Google Scholar]
- Patel S, Day TN, Jones N, et al. (2016) Association between anger rumination and autism symptom severity, depression symptoms, aggression, and general dysregulation in adolescents with autism spectrum disorder. Autism 21: 181–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posey DJ, Kem DL, Swiezy NB, et al. (2004) A pilot study of D-cycloserine in subjects with autistic disorder. American Journal of Psychiatry 161(11): 2115–2117. [DOI] [PubMed] [Google Scholar]
- Psychological Corporation (1999) Manual for the Wechsler Abbreviated Scale of Intelligence. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Reaven J, Blakeley Smith A, Culhane Shelburne K, et al. (2012) Group cognitive behavior therapy for children with high- functioning autism spectrum disorders and anxiety: a randomized trial. Journal of Child Psychology and Psychiatry 53(4): 410–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Research Units on Pediatric Psychopharmacology Autism Network (RUPP-AN) (2002) Risperidone in children with autism and serious behavioral problems. New England Journal of Medicine 347(5): 314–321. [DOI] [PubMed] [Google Scholar]
- Reynolds CR and Kamphaus RW (2004) Behavior Assessment System for Children. 2nd ed. Bloomington, MN: Pearson Education. [Google Scholar]
- Roke Y, Van Harten PN, Boot AM, et al. (2009) Antipsychotic medication in children and adolescents: a descriptive review of the effects on prolactin level and associated side effects. Journal of Child and Adolescent Psychopharmacology 19(4): 403–414. [DOI] [PubMed] [Google Scholar]
- Safer DJ (2004) A comparison of risperidone-induced weight gain across the age span. Journal of Clinical Psychopharmacology 24(4): 429–436. [DOI] [PubMed] [Google Scholar]
- Samson AC, Hardan AY, Lee IA, et al. (2015) Maladaptive behavior in autism spectrum disorder: the role of emotion experience and emotion regulation. Journal of Autism and Developmental Disorders 45(11): 3424–3432. [DOI] [PubMed] [Google Scholar]
- Shea S, Turgay A, Carroll A, et al. (2004) Risperidone in the treatment of disruptive behavioral symptoms in children with autistic and other pervasive developmental disorders. Pediatrics 114(5): 634–641. [DOI] [PubMed] [Google Scholar]
- Siegel M and Gabriels RL (2014) Psychiatric hospital treatment of children with autism and serious behavioral disturbance. Child and Adolescent Psychiatric Clinics of North America 23(1): 125–142. [DOI] [PubMed] [Google Scholar]
- Simonoff E, Pickles A, Charman T, et al. (2008) Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population- derived sample. Journal of the American Academy of Child and Adolescent Psychiatry 47(8): 921–929. [DOI] [PubMed] [Google Scholar]
- Solomon M, Ono M, Timmer S, et al. (2008) The effectiveness of parent-child interaction therapy for families of children on the autism spectrum. Journal of Autism and Developmental Disorders 38(9): 1767–1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sparrow SS, Cicchetti DV and Balla DA (2005) Vineland Adaptive Behavior Scales. 2nd ed. Circle Pines, MN: AGS Publishing. [Google Scholar]
- Storch EA, Arnold EB, Lewin AB, et al. (2013) The effect of cognitive-behavioral therapy versus treatment as usual for anxiety in children with autism spectrum disorders: a randomized, controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry 52(2): 132–142. [DOI] [PubMed] [Google Scholar]
- Vismara LA and Rogers SJ (2010) Behavioral treatments in autism spectrum disorder: what do we know? Annual Review of Clinical Psychology 6(1): 447–468. [DOI] [PubMed] [Google Scholar]