Abstract
Postural tachycardia syndrome (POTS) is a heterogeneous clinical syndrome that has gained increasing interest over the past few decades due to its increasing prevalence and clinical impact on health-related quality of life. POTS is clinically characterized by sustained excessive tachycardia upon standing that occurs in the absence of significant orthostatic hypotension and other medical conditions and or medications, and with chronic symptoms of orthostatic intolerance. POTS represents one of the most common presentations of syncope and presyncope secondary to autonomic dysfunction in emergency rooms and in cardiology, neurology, and primary care clinics. The most sensitive method to detect POTS is a detailed medical history, physical examination with orthostatic vital signs or brief tilt table test, and a resting 12-lead electrocardiogram. Additional diagnostic testing may be warranted in selected patients based on clinical signs. While the precise etiology remains unknown, the orthostatic tachycardia in POTS is thought to reflect convergence of multiple pathophysiological processes, as a final common pathway. Based on this, POTS is often described as a clinical syndrome consisting of multiple heterogeneous disorders, with several underlying pathophysiological processes proposed in the literature including partial sympathetic neuropathy, hyperadrenergic state, hypovolemia, mast cell activation, deconditioning, and immune-mediated. These clinical features often overlap, however, making it difficult to categorize individual patients. Importantly, POTS is not associated with mortality, with many patients improving to some degree over time after diagnosis and proper treatment. This review will outline the current understanding of diagnosis, pathophysiology, and prognosis in POTS.
Keywords: postural tachycardia syndrome, orthostatic intolerance, etiology, diagnosis
1. Introduction
Postural tachycardia syndrome (POTS) is one of the most common presentations of presyncope and syncope secondary to autonomic dysfunction. This is a heterogeneous clinical syndrome that is characterized by sustained and excessive sinus tachycardia upon standing, in the absence of orthostatic hypotension and with chronic symptoms of orthostatic intolerance.1, 2 The presence of chronic illness in POTS predisposes to impaired health-related quality of life as well as functional disability that limit activities of daily living.3, 4 While the true prevalence is unknown due to a lack of accurate epidemiologic data, it is estimated to affect between 0.1 to 1% of the United States population.5, 6 POTS has gained increasing clinical interest over the past two decades, in part due to the number of patients presenting in emergency rooms and in cardiology, neurology, and primary care clinics. Given this relatively high prevalence and clinical impact, there is an emerging need to better understand how to identify POTS in the clinical setting and its potential underlying causes. This review will outline the current understanding of the diagnosis, pathophysiology, and prognosis in POTS.
2. Physiology and Pathophysiology of Standing
Approximately one-forth of blood volume resides in the thorax in the supine position. Upon assuming the upright posture, there is an instantaneous shift of 500 to 1000 mL of blood to the capacitance vessels in the lower extremities and splanchnic circulation.7 There is also a secondary shift in which 10 to 25% of the plasma volume is driven out of the vasculature and into the interstitial space in response to gravitational stress.8 These changes in blood volume distribution result in impaired venous return to the heart to reduce cardiac filling, stroke volume, and ultimately blood pressure (BP). The autonomic nervous system compensates for these hemodynamic changes by unloading the high-pressure arterial baroreceptors in the carotid sinus and aortic arch to stimulate sympathetic efferent nerve activity, and concomitantly suppress parasympathetic activity, to the heart and blood vessels. This sympathetic nervous system dominance elicits cardio-acceleration and increases systemic vascular resistance, to enhance venous return to the heart to counteract the initial decline in BP. The skeletal muscle pump system and hormonal mechanisms (e.g. activation of renin-angiotensin and endothelin systems) are also engaged during prolonged standing to maintain BP.9, 10 These compensatory mechanisms are sufficient to maintain hemodynamics upon standing with negligible changes in systolic BP, a small ~5 mm Hg increase in diastolic BP, and a 10 to 20 bpm increase in heart rate (HR). Any abnormality in these autonomic or neurohumoral reflex pathways can result in altered hemodynamic responses during standing, including orthostatic hypotension (drop in BP within 3 minutes of standing ≥20/10 mm Hg) as well as excessive orthostatic tachycardia seen in POTS.
3. Diagnosis
3.1 Diagnostic Criteria
As shown in Table 1, the consensus criteria for diagnosis of POTS is: (1) a sustained increase in HR of at least 30 bpm within 10 minutes of assuming the upright posture (often with absolute upright HR ≥120 bpm); (2) in the absence of sustained orthostatic hypotension (drop in BP >20/10 mmHg); (3) with symptoms of orthostatic intolerance for at least 6 months that are relieved by recumbence; and (4) excluding other causes of sinus tachycardia including acute physiological stimuli (e.g. panic attacks, pain, exercise), dietary influences (e.g. caffeine, alcohol), medications (e.g. sympathomimetics, anticholinergics, rebound effects of β-blocker withdrawal), and other medical conditions (e.g. anemia, dehydration, hyperthyroidism, inappropriate sinus tachycardia). 1, 2 In patients less than 19 years of age, there is a higher HR threshold for POTS (increment ≥40 bpm or absolute upright HR ≥120 bpm) due to physiological orthostatic tachycardia in adolescents and children.11
Table 1.
Diagnostic Criteria for POTS1
| 1. Heart rate increase ≥30 bpm within 10 minutes of upright posture in adults. Heart rate increase of ≥40 bpm within 10 minutes is required in adolescents age 12–19 years. |
| 2. Absence of orthostatic hypotension defined as a sustained drop in blood pressure ≥20/10 mm Hg within 3 minutes of upright posture. |
| 3. Symptoms of orthostatic intolerance for ≥6 months. |
| 4. Absence of overt causes for sinus tachycardia such as acute physiological stimuli, dietary influences, other medical conditions and medications. |
There are some important points to emphasize. First, the HR increase must be sustained. Many people will have a transient increase in HR immediately on standing that gets better after the first 45 seconds. This likely relates to a variant of initial orthostatic hypotension,12 and is not in itself a manifestation of POTS. Second, POTS patients can also sometimes have orthostatic hypotension, especially at times of excessive relative hypovolemia. However, if they only have excessive orthostatic tachycardia in the setting of orthostatic hypotension, then this is not consistent with the diagnosis of POTS. Third, POTS is a chronic disorder. Many people can experience “POTS-like” features acutely with a viral infection, and this usually resolves in a few days. This acute presentation is not POTS. Finally, and most importantly, POTS is a clinical syndrome and not just a physiological finding. The diagnosis cannot be made in the absence of typical symptoms that are worse in the upright posture and better with recumbence.
3.2 Clinical Features
POTS has a strong female predominance (4–5:1), and primarily affects women of childbearing age. Most patients present with POTS between 13 to 50 years of age, with family history of orthostatic intolerance reported in approximately 13% of patients.13 Orthostatic symptoms can include palpitation, chest pain or discomfort, lightheadedness, blurred vision, shortness of breath, headache, nausea, fatigue, and tremulousness.1 Approximately 50% of patients also develop dependent acrocyanosis with standing, a dark red-blue discoloration of legs that is cold to the touch, which is thought to result from decreased blood flow to the skin.14–16 These patients also commonly suffer from cognitive dysfunction (addressed in more depth in the article on Cognitive and Psychological Issues in POTS, elsewhere in this issue),17 sleep disturbances (addressed in more detail in the article on Managing Fatigue in POTS, elsewhere in this issue),18 and exercise intolerance (addressed in more depth in the article on Exercise and Non-Pharmacological Treatment of POTS, elsewhere in this issue).19 These symptoms can be exacerbated by numerous factors including dehydration, heat exposure, prolonged recumbency, alcohol, menstruation, and acute exercise. Syncope is not a predominant feature of POTS (only ~20–30% actually pass out, and this is usually thought to be due to vasovagal syncope)20; however, many patients experience frequent presyncopal episodes that impair functional capacity. Patients often report that POTS symptoms began immediately following an acute stressor (e.g. viral illness, pregnancy, surgery, concussion), but in some patients, symptoms develop more gradually and subtly over time. Many patients report that their symptoms started around puberty. Common comorbidities include chronic fatigue syndrome, hypermobility type of Ehlers-Danlos syndrome, migraine, bowel irregularities, autoimmune disorders, and fibromyalgia.21
3.3. Diagnostic Considerations
The current Heart Rhythm Society Scientific Statement recommendations for evaluation of POTS are shown in Table 2.1 The minimal requirements to detect POTS on initial evaluation is a detailed medical history, physical examination with orthostatic vitals, and a resting 12-lead electrocardiogram (ECG).1 The medical history should document medications, other medical conditions including personal and family history of cardiac disease, joint hypermobility, autoimmunity or neurological disorders, and the nature of tachycardia including potential triggers (e.g. posture, pain, exercise, diet, menstrual cycle), frequency, time of day, association with presyncopal or syncopal episodes, symptoms, and impact on daily activities.
Table 2.
Heart Rhythm Society Recommendations for Evaluation of POTS1
| Investigation | Utility | Comment |
|---|---|---|
| Initial Evaluation | ||
| Medical History | Essential | Document medications, other medical conditions, diet and exercise history, family history, and details on nature of tachycardia including chronicity, triggers, modifying factors, presyncopal or syncopal episodes, symptoms and impact on daily activities. |
| Physical Examination | Essential | Detailed cardiovascular, neurologic, autonomic, and other systems assessment. |
| Orthostatic Vitals | Essential | Blood pressure and heart rate should be measured while lying down (>5 minutes) and ideally again after 1, 3, 5, and 10 minutes of standing. |
| Electrocardiogram | Essential | Rule out pre-existing cardiovascular disease and cardiovascular conduction abnormalities. |
| Additional Evaluation | ||
| Blood Work | Some Patients | In patients with evidence for specific underlying causes such as dehydration, anemia, and hyperthyroidism. Supine and standing norepinephrine levels in patients with evidence for hyperadrenergic POTS. |
| Cardiovascular Testing | Some Patients | In patients with suspected cardiac conduction or structural abnormalities (e.g. Holter monitor, echocardiogram, exercise stress testing). |
| Head-Up Tilt Table Testing | Some Patients | In patients with normal orthostatic vital signs with high clinical suspicion, or in patients with convulsions or seizure disorder. |
| Autonomic Function Tests | Some Patients | In patients with symptoms of autonomic neuropathy, or in patients whose symptoms do not resolve or markedly improve with treatment. |
Abbreviations: POTS, postural tachycardia syndrome
The physical examination should include obtainment of orthostatic vitals and symptoms as well as a comprehensive assessment of cardiovascular, neurologic, autonomic, and other systems. Given that joint hypermobility is frequently seen in these patients, this should be assessed using the Beighton Criteria.22 This brief assessment tests for hyperextensibility of the bilateral thumbs and wrist (to touch forearm), bilateral baby fingers (bent to an acute angle), bilateral elbows (hyperextend >10 degrees), bilateral knee hyperextension, and the ability to touch the floor with the palms without bending the knees. There is another article about Ehlers-Danlos Syndrome and hypermobility in this POTS Issue of Autonomic Neurosciences,23 as well as a recently published consensus statement on Ehlers-Danlos syndrome diagnosis.24
For orthostatic vital signs, BP and HR should ideally be measured after the patient has been supine for at least 5 minutes, and again after 1, 3, 5, and 10 minutes of standing to capture the sustained orthostatic tachycardia. This can be challenging in clinic settings if a bed is not available for supine measurements; however, many patients have a modest elevation in HR even in the seated position (10–15 bpm) that can limit diagnostic sensitivity for POTS identification. POTS patients should exhibit orthostatic tachycardia in the absence of orthostatic hypotension, and many patients will increase BP with standing due to sympathetic overactivity. An important consideration is that there can be significant diurnal variability in POTS, with the degree of orthostatic tachycardia and percentage of patients meeting HR criteria being higher in the morning compared with the afternoon or evening.25 Therefore, obtaining of orthostatic vital signs in the morning may optimize diagnostic sensitivity in these patients.
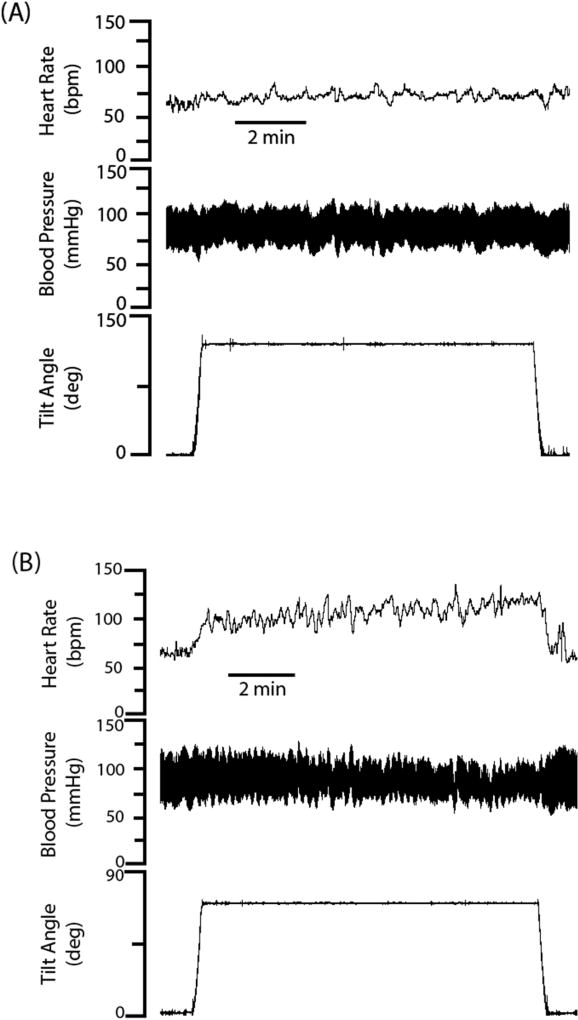
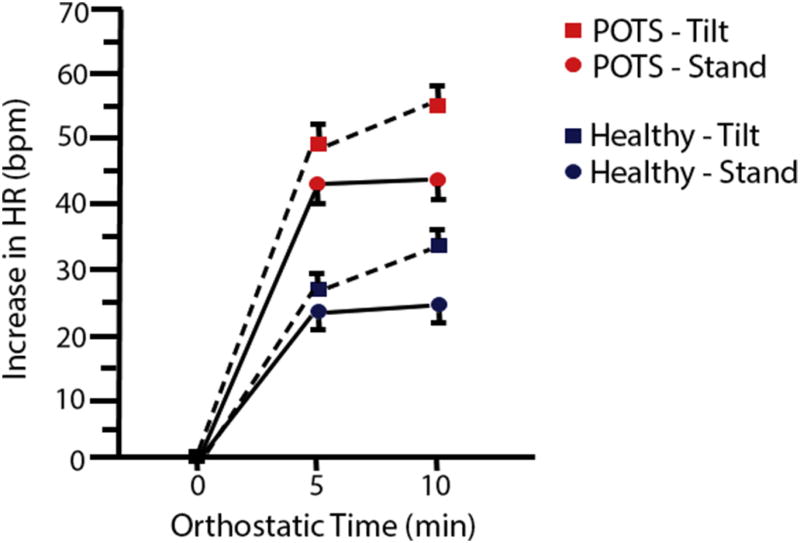
An alternate approach commonly described in the literature to diagnose POTS is the use of passive head-up tilt table testing (HUTT). During HUTT, BP and HR are measured continuously or at fixed intervals while the patient is supine on a standard tilt table, and following an incline to greater than 60° head-up angle (Figure 1). This approach may be useful to document hemodynamics in selected patients with confounding features (e.g. convulsions, seizure disorder, arrhythmia, or frequent syncope), in patients that do not meet HR criteria with active standing but have high clinical suspicion of POTS, or in patients who cannot stand safely for 10 minutes. A few potential limitations include: (1) the physiological responses activated during HUTT are different than active standing, which is more clinically relevant and engages the skeletal muscle pump system; and (2) while HUTT is sensitive to diagnose POTS using the ≥30 bpm diagnostic threshold, it produces greater tachycardia and has less diagnostic specificity compared with standing (Figure 2).26 Therefore, HUTT testing should be interpreted with caution and in the context of symptoms, as “false-positive” orthostatic tachycardia might be seen in the absence of typical POTS symptoms. Both tests can be done, and standing tests alone may be sufficient in some patients. Ambulatory ECG monitoring may also be a useful ancillary test to document elevated HR, and to differentiate sinus tachycardia from other cardiac abnormalities.27 Most of these devices do not record posture or activity limiting their utility to study orthostatic-related HR changes.
Figure 1. Hemodynamic Pattern during Head-Up Tilt Table Testing (HUTT) in POTS.
Panel A: In a healthy subject, heart rate increases only modestly with HUTT, with no significant change in blood pressure. Panel B: In Postural Tachycardia Syndrome (POTS), there is an excessive rise in HR during HUTT, with stable blood pressure.
Figure 2. Orthostatic Heart Rate Increase with Head-Up Tilt Table Testing (HUTT) versus Active Standing.
The mean orthostatic change in heart rate (HR) is shown over a 10-minute period during HUTT and active standing in healthy subjects (blue symbols) and patients with Postural Tachycardia Syndrome (POTS; red symbols). Orthostatic tachycardia is exaggerated with HUTT, with the mean HR value over 30 bpm in both groups, suggesting less sensitivity of this method for diagnosis compared with active standing.
A resting 12-lead ECG is recommended in the diagnosis of POTS to rule out presence of an accessory bypass tract or cardiac conduction abnormalities.1 POTS patients will typically have sinus rhythm or sinus tachycardia. Chest pains in POTS are almost never due to coronary artery obstruction, but may present with electrocardiographic changes in the inferior leads, particularly when the patient is upright.28 Patients with cardiac precipitants (e.g. supine or exertional onset, dyspnea, rapid palpitation) or with abnormal ECG results may have an underlying cardiac cause for tachycardia that warrants additional testing such as echocardiogram or stress test. A Holter monitor or other extended cardiac rhythm monitor may be useful to exclude re-entrant dysrhythmia in patients with history of paroxysmal tachycardia with sudden onset/offset. While POTS does not cause reentrant arrhythmias (such as atrioventricular nodal reentrant tachycardia or atrioventricular reentrant tachycardia), a patient with POTS may also have one of these arrhythmias. If a POTS patient also has one of these other arrhythmias, they may be a candidate for radiofrequency catheter ablation. Successful ablation of the reentrant tachycardia, however, is unlikely to address the tachycardia associated with POTS or other symptoms. Radiofrequency catheter ablation is not recommended for POTS patients without one of these other dysrhythmias.29
Patients with inappropriate sinus tachycardia (IST), in contrast to POTS, will have a high HR even when supine. For IST, the supine HR in clinic is usually over 100 bpm and the mean 24-hour HR is greater than 90 bpm.1 Patients with IST can also have excessive orthostatic tachycardia, but we do not also add in a POTS diagnosis in those cases. Both IST and POTS may be on the same continuum of disorders and are associated with shift to greater sympathetic nervous system influence on HR.30
Routine laboratory tests should be performed on initial evaluation to exclude anemia (complete blood count and iron indices), and hypo- or hyperthyroidism (T3 and T4 levels). Some POTS patients are referred for standardized autonomic function testing to determine the integrity of the sympathetic and parasympathetic nervous systems,31 which can include sinus arrhythmia, hyperventilation, Valsalva maneuver, cold pressor, and isometric handgrip tests. Most POTS patients, however, have intact cardiovagal responses and intact or exaggerated sympathetic noradrenergic reflex responses. Once POTS diagnosis is established, an expanded evaluation approach may be taken to identify potential underlying pathophysiological processes in POTS based on clinical signs, which can include additional autonomic testing for small fiber neuropathy, catecholamine levels, blood volume estimation, and urinary histamine metabolites (described in detail in Section 4). When the history and physical exam suggests another diagnosis may be present, this should be pursued, as POTS can occur secondary to or co-morbid with many conditions that may cause or contribute to autonomic dysfunction. An example is the presence of sicca symptoms suggesting possible Sjögren’s syndrome. Details on expanded evaluation approaches that could be considered for selected patients is available in another article in this POTS issue.32
4. Pathophysiology of POTS
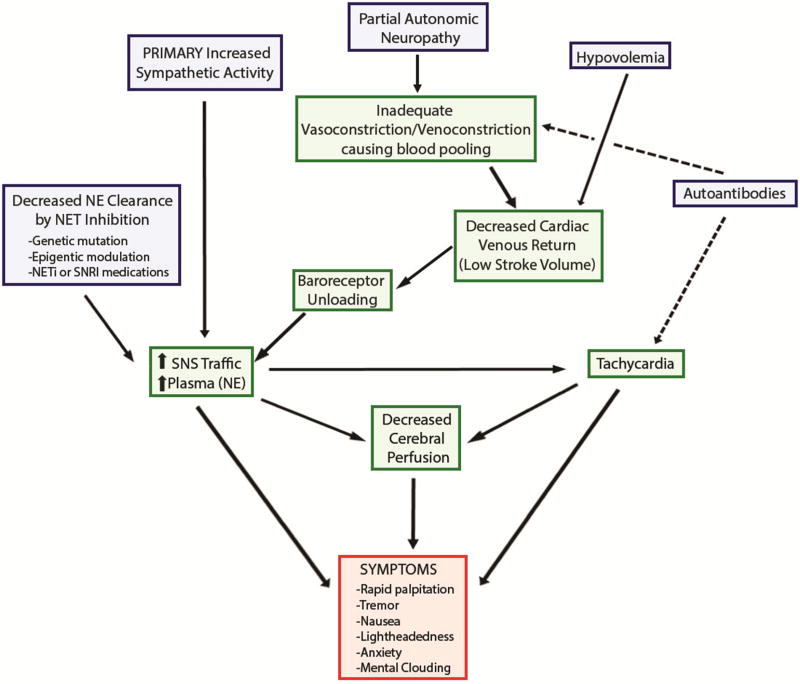
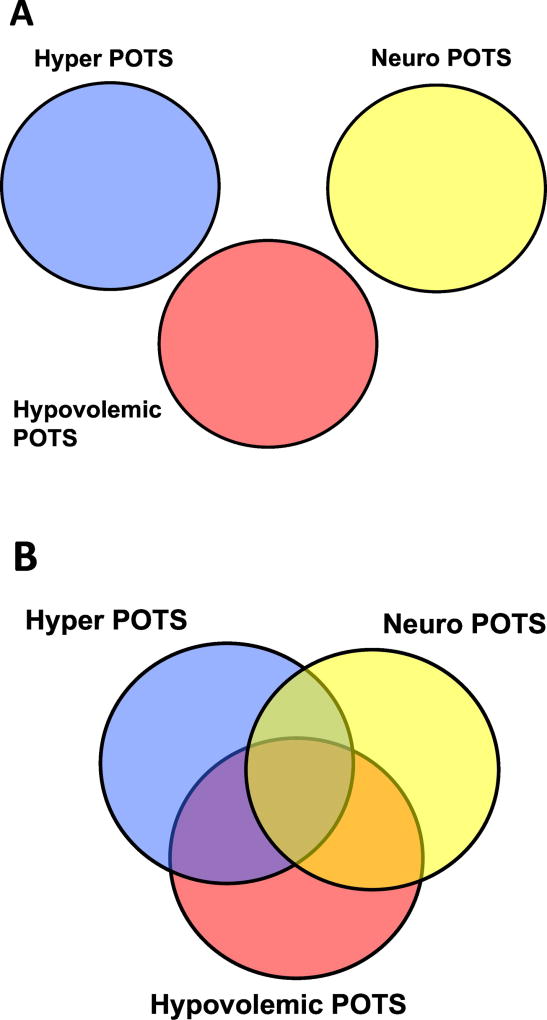
While the precise etiology remains unknown, orthostatic tachycardia in POTS is thought to reflect the convergence of multiple pathophysiological processes, as a final common pathway (Figure 3). Based on this, POTS is often described as a clinical syndrome consisting of multiple heterogeneous disorders. Some have taken to labeling patients with “POTS Subtypes”, with articles published alluding to hyperadrenergic POTS (“Hyper POTS”), neuropathic POTS (“Neuro POTS”), or hypovolemic POTS. Unfortunately, these subtypes do not all have standard definitions, and they are largely based on results from autonomic and laboratory testing. Furthermore, while these “subtypes” are useful as a global pathophysiological construct to understand mechanisms in POTS, the primary problem is the non-exclusivity of these labels, with individual patients often have overlapping clinical features involving more than one “subtype” (Figure 4). A second challenge is that since these “subtypes” do not have universally accepted definitions, so the labels could actually be misleading. While one doctor may use the term “Hyper POTS” to refer to a specific set of findings, another doctor might think that it refers to a different set of findings. In theory, this could harm a patient’s care. In our experience, these “subtype” labels are not clinically helpful.
Figure 3. Schematic Diagram of Multiple Potential Pathophysiologic Processes in POTS.
NE, norepinephrine; NET, norepinephrine transporter; NETi, norepinephrine transporter inhibitor; SNRI, selective norepinephrine reuptake inhibitor; SNS, sympathetic nervous system.
Figure 4. The Problem with POTS “Subtype” Labels.
Panel A: This shows a representation of how many people think about the various POTS “subtype” labels – as clearly distinct entities from each other; Panel B: In reality, these “subtypes” are not mutually exclusive of each other, and many patients may have features consistent with more than one subtype, leading to overlapping subsets.
4.1 Partial Sympathetic Neuropathy
It has been shown that approximately 50% of POTS patients evaluated at tertiary care centers exhibit a neuropathic phenotype associated with partial sympathetic denervation, usually due to a distal small fiber neuropathy producing sympathetic denervation of the lower limbs.13, 33–36 There are no widely accepted criteria for diagnosing neuropathic POTS, but these patients often exhibit patchy anhidrosis in the lower extremities during thermoregulatory sweat testing or quantitative sudomotor axon reflex testing, associated with abnormalities of unmyelinated nerve fibers on skin biopsy (intraepidermal nerve fiber density)35. These patients have also been reported to exhibit cardiac sympathetic denervation assessed by cardiac meta-iodobenzylguanidine (MIBG) scans; however, the clinical implication of this finding remains unclear.35 In POTS, small fiber neuropathy does not present with classic symptoms of typical length-dependent neuropathy.36 Neuropathic POTS may exhibit lower anxiety and depression and higher health-related quality of life compared with other subtypes.36
Despite elevated circulating norepinephrine levels, neuropathic POTS patients have exaggerated leg vasoconstriction in response to local norepinephrine and phenylephrine infusions suggesting denervation hypersensitivity.37 Furthermore, some POTS patients appear to have normal sympathetic neuronal norepinephrine release in the arms, but blunted norepinephrine release in the lower extremities as well as lack of an increase in mean burst area for peroneal muscle sympathetic nerve activity during standing.33, 38 Therefore, some POTS patients may inadequately increase peripheral vascular resistance in the legs in response to norepinephrine release during standing, leading to excessive venous pooling and subsequent sympathetic activation and compensatory increases in HR to maintain BP.
4.2 Hyperadrenergic State
Approximately 50% of POTS patients are reported to exhibit a hyperadrenergic phenotype characterized by similar excessive orthostatic tachycardia, standing plasma norepinephrine ≥600 pg/mL, an increase in systolic BP ≥10 mm Hg, or symptoms of sympathetic activation (e.g. palpitation, tremulousness, anxiety) upon standing.1, 39 Some hyperadrenergic POTS patients have hypersensitivity to isoproterenol, with marked tachycardia at doses producing no hemodynamic effect in healthy individuals.40 During standardized autonomic function testing, increased systolic BP at the end of phase II, and exaggerated overshoot of systolic BP during phase IV, are often noted during performance of the Valsalva maneuver.41 The sympathetic overactivity in POTS may be associated with increased levels of the proinflammatory marker interleukin-6.42 This hyperadrenergic state is usually secondary to hypovolemia or partial sympathetic denervation; however, in ~10% of patients the underlying cause is excessive central sympathetic discharge.16
4.3 Norepinephrine Transporter Deficiency
Norepinephrine is a critical sympathetic neurotransmitter that has its actions terminated by uptake from the synaptic cleft into presynaptic noradrenergic neurons by the norepinephrine transporter (NET). A loss of function single point mutation in the NET gene SLC6A2 was identified in one family with orthostatic tachycardia.43, 44 This mutation resulted in increased plasma norepinephrine levels due to diminished clearance to promote sympathetic activation. While this global mutation is rare, decreased NET protein expression has also been observed in vein biopsies, and decreased NET gene expression in leukocytes, from POTS patients.45, 46 A recent study suggests that this NET protein reduction in POTS and other clinical conditions may in part be explained by the creation of a binding site for microRNA miR-19a-3p.47
While these functional mutations are uncommon, pharmacological agents that inhibit NET are commonly used for treatment of neuropsychiatric conditions. This can include tricyclic antidepressants, NET inhibitors (e.g. atomoxetine, reboxetine), and serotonin-norepinephrine reuptake inhibitors (e.g. duloxetine, venlafaxine). Importantly, pharmacological NET inhibition can increase synaptic norepinephrine levels to mimic clinical presentation of POTS in healthy volunteers.48, 49 Similarly, the central α2 receptor antagonist yohimbine increases synaptic norepinephrine to elicit orthostatic tachycardia in healthy subjects.50, 51 POTS patients are often treated with NET inhibitors for comorbidities such as depression, attention deficit hyperactivity disorder, and fibromyalgia. A small, randomized, placebo-controlled study showed that the NET inhibitor atomoxetine acutely worsens orthostatic tachycardia and symptoms in POTS,52 indicating caution for use of this class of medications in POTS patients.
4.4 Hypovolemia
Low blood volume or hypovolemia is a common finding in POTS, with many patients reported to have deficits in red cell and plasma volume.8, 53–55 A study by Raj et al. showed an approximate 13% deficit in plasma volume in POTS patients using a nuclear medicine test (131I-labeled human serum albumen), while matched healthy subjects had no deficit. Other studies have estimated plasma volume in POTS using dye-dilution or carbon monoxide rebreathing methods.53, 55 This hypovolemia coupled with cardiac atrophy is thought to contribute to reduced stroke volume to elicit compensatory tachycardia to maintain BP. The importance of hypovolemia to orthostatic tolerance in POTS is illustrated by the finding that acute restoration of blood volume with either intravenous saline or the vasopressin analog desmopressin attenuates standing HR and improve symptom burden in these patients.54, 56, 57
The normal compensatory response to a blood volume deficit is activation of the renin-angiotensin system to increase angiotensin II, which stimulates aldosterone release to promote renal sodium and water reabsorption and restore blood volume. Interestingly, POTS patients appear to have a “renin-aldosterone paradox” in response to both hypovolemia and orthostatic challenge. Circulating angiotensin II levels are approximately 2-fold higher in POTS, perhaps due to reduced levels or activity of its degrading enzyme ACE2.8 Despite higher angiotensin II, however, POTS patients have normal BP and lower plasma renin activity and aldosterone suggesting reduced vascular and adrenal responsiveness.8, 55, 58 To further test this, a study by Mustafa et al. examined effects of acute intravenous angiotensin II infusion on target organ responsiveness in POTS patients compared with healthy subjects.59 Blunted pressor responses to angiotensin II infusion were observed in POTS with intact renal plasma flow, aldosterone secretion, and renal sodium reabsorption. This finding suggests potential divergent vascular and renal responsiveness to high angiotensin II in POTS; however, the implications of this finding remain unclear in terms of pathophysiology.
4.5 Mast Cell Activation
Mast cells are a type of white blood cell that reside in close proximity to blood vessels and peripheral nerves and play an important role in the inflammatory response. Since mast cells contain granules rich in histamine and other neuropeptides, their activation may provide a source of circulating vasodilators to elicit reflex sympathetic activation in POTS. Indeed, a subgroup of POTS patients has been reported to present with episodic flushing and comorbid mast cell activation disorder.41 Flushing episodes can be triggered by numerous stimuli (e.g. standing, exercise, meals, sexual intercourse, menstrual cycle) with associated symptoms including lightheadedness, dizziness, shortness of breath, excessive diuresis, nausea, diarrhea, vomiting, and headache. These patients appear to exhibit a hyperadrenergic phenotype, although the direction of causality between mast cell activation and sympathetic overactivity is unclear. Some POTS patients may present with flushing and orthostatic intolerance in the absence of mast cell activation disorder.41 A commonly used and clinically available diagnostic test to assess for mast cell activation is measurement of methylhistamine levels in urine collected within 4 hours of a severe spontaneous flushing episode; however, there are other potential tests that can be used. More detailed information on this topic is provided in an article on Mast Cell Activation Syndrome in POTS in this issue.60
4.6 Immune-Mediated
Many POTS patients report onset following an acute viral illness, perhaps suggesting a contribution of autoimmune factors. An initial study reported a low titer of ganglionic acetylcholine receptor (AChR) antibodies in the serum of approximately 15% of POTS patients.13 A follow-up study showed low AChR antibody levels in 5% of POTS patients, with no differences in seropositive rate or antibody levels from matched healthy subjects.61 Circulating antibodies to α1- and β-adrenergic receptors and cardiac lipid raft-associated proteins have also been discovered in POTS.62–64 In a small ex vivo study with serum from POTS patients, α1-adrenergic autoantibodies exerted a partial peripheral antagonist effect on contractility in rat cremaster arterioles, which could elicit compensatory sympathoneural activation and tachycardia. In contrast, β-adrenergic autoantibodies elicited an agonistic effect on arteriole contractility, which could facilitate tachycardia. These collective data suggest that autoantibodies could contribute to pathophysiology of POTS in some patients, but further research is needed to understand the clinical significance of this finding. Therefore, routine testing of autoantibodies to adrenergic receptors or AChR is not currently recommended. If a patient has clinical features suggestive of an autoimmune disorder that could contribute to autonomic dysfunction, such as Sjögren’s syndrome, then targeted testing may be warranted. A more detailed article on autoimmunity in POTS is provided elsewhere in this issue.65
4.7 Impaired Cerebral Autoregulation
POTS patients exhibit symptoms of orthostatic intolerance in the presence of normal BP, perhaps suggesting deficits in cerebrovascular autoregulation. While several studies have attempted to address this, there remains considerable controversy in the literature regarding the status of cerebral perfusion and autoregulation in POTS, as well as potential underlying mechanisms. Some studies have shown that dynamic cerebral perfusion and autoregulation are preserved in POTS patients during orthostatic stress.66, 67 Others have shown excessive reductions in middle cerebral artery blood velocity measured by transcranial Doppler in POTS during HUTT, perhaps related to sympathetic- or hypocapnic-mediated cerebral vasoconstriction.68–71 Possibly arguing against hyperventilation as the underlying cause, Ocon et al. showed reduced cerebral blood flow and autoregulation in normocapnic POTS patients.68
4.8 Deconditioning
Many POTS patients have impaired health-related quality of life and functional disability,3, 4 which can contribute to physical deconditioning. The physiological responses to orthostatic stress in POTS often resemble the clinical phenotype of patients with deconditioning from prolonged bed rest or space flight (e.g. tachycardia, exercise intolerance, and reductions in left ventricular mass, stroke volume, blood volume).53, 72, 73 It remains controversial, however, whether deconditioning represents a primary cause of POTS, or is secondary to presence of chronic illness. The true prevalence of deconditioning in POTS also remains unclear, with studies showing large variations ranging from 20 to 90% of patients depending on site of patient recruitment and exercise protocols.74–76 Regardless, structured short-term exercise programs can reduce orthostatic tachycardia and improve quality of life, systemic hemodynamics, blood volume, left ventricular mass, and exercise tolerance in POTS patients.77 A review of exercise therapy for POTS patients is discussed in another article in this POTS issue of Autonomic Neurosciences.19
4. Prognosis
While there is limited data on natural history, POTS is thought to reflect a chronic condition that is not associated with significant mortality.1 In a prospective study, clinical outcomes were assessed in adult POTS patients at baseline and at one year of follow-up. This study showed orthostatic symptom improvement and that over one-third of patients no longer met criteria for POTS during HUTT at follow-up.78
A handful of questionnaire-based studies have also reported long-term outcomes of POTS, with focus on disease course in adolescent patients. In one study from the Mayo Clinic, about 60% of adolescent POTS patients reported general improvement in health at an approximate mean of 20 months following initial evaluation and treatment with medications such as midodrine and β-blockers.79 This study was limited by a relatively low response rate to the follow-up survey. In another small series, adolescents with florid POTS reported substantial improvement after diagnosis and treatment with a mean follow-up time of 92 months.80 In this 17 patient study, approximately one-third of patients were completely asymptomatic, half reported significant improvement, 12% remained highly symptomatic, and 62% remained on pharmacological therapy on follow-up consistent with favorable disease progression. In another Mayo Clinic study looking at an average of 5 years of follow-up from initial evaluation, about 19% of patients reported that they had “recovered”. Unfortunately, a significant proportion of patients reported ongoing functional disability.6 Overall, these data suggest that many POTS patients may see some improvement over time following diagnosis and appropriate treatment.
In our experience, while adult POTS patients can clinically improve, “cure” is very unusual. Our goal is to allow our patients to function as well as possible with a combination of non-pharmacological strategies, and medications as required. There is critical need for long-term follow-up studies to better quantify and understand the natural history and prognosis of POTS.
5. Conclusions
POTS is a debilitating disorder of the autonomic nervous system, which manifests with the clinical hallmark of symptomatic orthostatic tachycardia without major changes in BP. This syndrome is associated with frequent presyncopal episodes that can produce substantial impairment in health-related quality of life and functional disability in otherwise healthy young individuals. The minimal requirements to detect POTS in the clinical setting include a detailed medical history, physical examination with orthostatic vital signs (either with stand tests or tilt tests), and resting ECG. Additional testing or referral to a tertiary care center may be needed in selected patients based on clinical signs and symptoms. POTS appears to reflect convergence of multiple pathophysiological processes, and thus the precise etiology remains unknown. While several “subtypes” have been described in the literature to understand mechanisms of POTS, they often have overlapping clinical features, don't have clearly accepted definitions, and are not currently helpful as individual patient labels. A handful of studies have examined long-term outcomes in POTS, and have generally shown some improvement in symptoms and quality of life over time after appropriate diagnosis and treatment. It is clear, however, that further research is critically needed to better understand the underlying pathophysiology and prognosis of POTS.
Acknowledgments
None
Funding Sources
ACA receives research support from the National Institutes of Health (HL122507). SRR receives research support from the Canadian Institutes of Health Research (CIHR; Ottawa, ON, Canada) grant MOP142426 and the Cardiac Arrhythmia Network of Canada (CANet; London, ON, Canada) grants SRG-15-P01-001 and SRG-17-P27-001.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
ACA and JN report no disclosures. SRR is a consultant for Lundbeck NA Ltd. GE Healthcare, Abbott and Allergan.
References
- 1.Sheldon RS, Grubb BP, 2nd, Olshansky B, Shen WK, Calkins H, Brignole M, Raj SR, Krahn AD, Morillo CA, Stewart JM, Sutton R, Sandroni P, Friday KJ, Hachul DT, Cohen MI, Lau DH, Mayuga KA, Moak JP, Sandhu RK, Kanjwal K. 2015 heart rhythm society expert consensus statement on the diagnosis and treatment of postural tachycardia syndrome, inappropriate sinus tachycardia, and vasovagal syncope. Heart Rhythm. 2015;12:e41–63. doi: 10.1016/j.hrthm.2015.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Freeman R, Wieling W, Axelrod FB, Benditt DG, Benarroch E, Biaggioni I, Cheshire WP, Chelimsky T, Cortelli P, Gibbons CH, Goldstein DS, Hainsworth R, Hilz MJ, Jacob G, Kaufmann H, Jordan J, Lipsitz LA, Levine BD, Low PA, Mathias C, Raj SR, Robertson D, Sandroni P, Schatz I, Schondorff R, Stewart JM, van Dijk JG. Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Clin Auton Res. 2011;21:69–72. doi: 10.1007/s10286-011-0119-5. [DOI] [PubMed] [Google Scholar]
- 3.Benrud-Larson LM, Sandroni P, Haythornthwaite JA, Rummans TA, Low PA. Correlates of functional disability in patients with postural tachycardia syndrome: Preliminary cross-sectional findings. Health Psychol. 2003;22:643–648. doi: 10.1037/0278-6133.22.6.643. [DOI] [PubMed] [Google Scholar]
- 4.Benrud-Larson LM, Dewar MS, Sandroni P, Rummans TA, Haythornthwaite JA, Low PA. Quality of life in patients with postural tachycardia syndrome. Mayo Clin Proc. 2002;77:531–537. doi: 10.4065/77.6.531. [DOI] [PubMed] [Google Scholar]
- 5.Robertson D. The epidemic of orthostatic tachycardia and orthostatic intolerance. Am J Med Sci. 1999;317:75–77. doi: 10.1097/00000441-199902000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Bhatia R, Kizilbash SJ, Ahrens SP, Killian JM, Kimmes SA, Knoebel EE, Muppa P, Weaver AL, Fischer PR. Outcomes of adolescent-onset postural orthostatic tachycardia syndrome. J Pediatr. 2016;173:149–153. doi: 10.1016/j.jpeds.2016.02.035. [DOI] [PubMed] [Google Scholar]
- 7.Smith JJ, Porth CM, Erickson M. Hemodynamic response to the upright posture. J Clin Pharmacol. 1994;34:375–386. doi: 10.1002/j.1552-4604.1994.tb04977.x. [DOI] [PubMed] [Google Scholar]
- 8.Raj SR, Biaggioni I, Yamhure PC, Black BK, Paranjape SY, Byrne DW, Robertson D. Renin-aldosterone paradox and perturbed blood volume regulation underlying postural tachycardia syndrome. Circulation. 2005;111:1574–1582. doi: 10.1161/01.CIR.0000160356.97313.5D. [DOI] [PubMed] [Google Scholar]
- 9.Nilsson D, Sutton R, Tas W, Burri P, Melander O, Fedorowski A. Orthostatic changes in hemodynamics and cardiovascular biomarkers in dysautonomic patients. PLoS One. 2015;10:e0128962. doi: 10.1371/journal.pone.0128962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Modesti PA, Cecioni I, Naldoni A, Migliorini A, Neri Serneri GG. Relationship of renin-angiotensin system and et-1 system activation in long-lasting response to postural changes. Am J Physiol. 1996;270:H1200–1206. doi: 10.1152/ajpheart.1996.270.4.H1200. [DOI] [PubMed] [Google Scholar]
- 11.Singer W, Sletten DM, Opfer-Gehrking TL, Brands CK, Fischer PR, Low PA. Postural tachycardia in children and adolescents: What is abnormal? J Pediatr. 2012;160:222–226. doi: 10.1016/j.jpeds.2011.08.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wieling W, Krediet CT, van Dijk N, Linzer M, Tschakovsky ME. Initial orthostatic hypotension: Review of a forgotten condition. Clin Sci (Lond) 2007;112:157–165. doi: 10.1042/CS20060091. [DOI] [PubMed] [Google Scholar]
- 13.Thieben MJ, Sandroni P, Sletten DM, Benrud-Larson LM, Fealey RD, Vernino S, Lennon VA, Shen WK, Low PA. Postural orthostatic tachycardia syndrome: The mayo clinic experience. Mayo Clin Proc. 2007;82:308–313. doi: 10.4065/82.3.308. [DOI] [PubMed] [Google Scholar]
- 14.Freeman R, Lirofonis V, Farquhar WB, Risk M. Limb venous compliance in patients with idiopathic orthostatic intolerance and postural tachycardia. J Appl Physiol (1985) 2002;93:636–644. doi: 10.1152/japplphysiol.00817.2001. [DOI] [PubMed] [Google Scholar]
- 15.Stewart JM. Pooling in chronic orthostatic intolerance: Arterial vasoconstrictive but not venous compliance defects. Circulation. 2002;105:2274–2281. doi: 10.1161/01.cir.0000016348.55378.c4. [DOI] [PubMed] [Google Scholar]
- 16.Raj SR. The postural tachycardia syndrome (pots): Pathophysiology, diagnosis & management. Indian Pacing Electrophysiol J. 2006;6:84–99. [PMC free article] [PubMed] [Google Scholar]
- 17.Raj VO M, Arnold AC. Cognitive and psychological issues in postural tachycardia syndrome. Auton Neurosci. 2018 doi: 10.1016/j.autneu.2018.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Newton J. Managing fatigue in pots. Auton Neurosci. 2018 doi: 10.1016/j.autneu.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 19.Fu Q. Exercise and non-pharmacological treatment of pots. Auton Neurosci. 2018 doi: 10.1016/j.autneu.2018.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shen WK, Sheldon RS, Benditt DG, Cohen MI, Forman DE, Goldberger ZD, Grubb BP, Hamdan MH, Krahn AD, Link MS, Olshansky B, Raj SR, Sandhu RK, Sorajja D, Sun BC, Yancy CW. 2017 acc/aha/hrs guideline for the evaluation and management of patients with syncope: Executive summary: A report of the american college of cardiology/american heart association task force on clinical practice guidelines and the heart rhythm society. J Am Coll Cardiol. 2017;70:620–663. doi: 10.1016/j.jacc.2017.03.002. [DOI] [PubMed] [Google Scholar]
- 21.Garland EM, Celedonio JE, Raj SR. Postural tachycardia syndrome: Beyond orthostatic intolerance. Curr Neurol Neurosci Rep. 2015;15:60. doi: 10.1007/s11910-015-0583-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morlino S, Dordoni C, Sperduti I, Venturini M, Celletti C, Camerota F, Colombi M, Castori M. Refining patterns of joint hypermobility, habitus, and orthopedic traits in joint hypermobility syndrome and ehlers-danlos syndrome, hypermobility type. Am J Med Genet A. 2017;173:914–929. doi: 10.1002/ajmg.a.38106. [DOI] [PubMed] [Google Scholar]
- 23.Roma MMCL, De Wandele I, Francomano CA, Rowe PC. Postural tachycardia syndrome and other forms of orthostatic intolerance in ehlers-danlos syndrome. Auton Neurosci. 2018 doi: 10.1016/j.autneu.2018.02.006. [DOI] [PubMed] [Google Scholar]
- 24.Malfait F, Francomano C, Byers P, Belmont J, Berglund B, Black J, Bloom L, Bowen JM, Brady AF, Burrows NP, Castori M, Cohen H, Colombi M, Demirdas S, De Backer J, De Paepe A, Fournel-Gigleux S, Frank M, Ghali N, Giunta C, Grahame R, Hakim A, Jeunemaitre X, Johnson D, Juul-Kristensen B, Kapferer-Seebacher I, Kazkaz H, Kosho T, Lavallee ME, Levy H, Mendoza-Londono R, Pepin M, Pope FM, Reinstein E, Robert L, Rohrbach M, Sanders L, Sobey GJ, Van Damme T, Vandersteen A, van Mourik C, Voermans N, Wheeldon N, Zschocke J, Tinkle B. The 2017 international classification of the ehlers-danlos syndromes. Am J Med Genet C Semin Med Genet. 2017;175:8–26. doi: 10.1002/ajmg.c.31552. [DOI] [PubMed] [Google Scholar]
- 25.Brewster JA, Garland EM, Biaggioni I, Black BK, Ling JF, Shibao CA, Robertson D, Raj SR. Diurnal variability in orthostatic tachycardia: Implications for the postural tachycardia syndrome. Clin Sci (Lond) 2012;122:25–31. doi: 10.1042/CS20110077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Plash WB, Diedrich A, Biaggioni I, Garland EM, Paranjape SY, Black BK, Dupont WD, Raj SR. Diagnosing postural tachycardia syndrome: Comparison of tilt testing compared with standing haemodynamics. Clin Sci (Lond) 2013;124:109–114. doi: 10.1042/CS20120276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kirbis M, Grad A, Meglic B, Bajrovic FF. Comparison of active standing test, head-up tilt test and 24-h ambulatory heart rate and blood pressure monitoring in diagnosing postural tachycardia. Funct Neurol. 2013;28:39–45. [PMC free article] [PubMed] [Google Scholar]
- 28.Friesinger GC, Biern RO, Likar I, Mason RE. Exercise electrocardiography and vasoregulatory abnormalities. Am J Cardiol. 1972;30:733–740. doi: 10.1016/0002-9149(72)90147-6. [DOI] [PubMed] [Google Scholar]
- 29.Page RL, Joglar JA, Caldwell MA, Calkins H, Conti JB, Deal BJ, Estes NAM, 3rd, Field ME, Goldberger ZD, Hammill SC, Indik JH, Lindsay BD, Olshansky B, Russo AM, Shen WK, Tracy CM, Al-Khatib SM. 2015 acc/aha/hrs guideline for the management of adult patients with supraventricular tachycardia: A report of the american college of cardiology/american heart association task force on clinical practice guidelines and the heart rhythm society. J Am Coll Cardiol. 2016;67:e27–e115. doi: 10.1016/j.jacc.2015.08.856. [DOI] [PubMed] [Google Scholar]
- 30.Nwazue VC, Paranjape SY, Black BK, Biaggioni I, Diedrich A, Dupont WD, Robertson D, Raj SR. Postural tachycardia syndrome and inappropriate sinus tachycardia: Role of autonomic modulation and sinus node automaticity. J Am Heart Assoc. 2014;3:e000700. doi: 10.1161/JAHA.113.000700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Low PA, Tomalia VA, Park KJ. Autonomic function tests: Some clinical applications. J Clin Neurol. 2013;9:1–8. doi: 10.3988/jcn.2013.9.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goodman B. Evaluation of a pots patient. Auton Neurosci. 2018 doi: 10.1016/j.autneu.2018.04.004. [DOI] [PubMed] [Google Scholar]
- 33.Jacob G, Costa F, Shannon JR, Robertson RM, Wathen M, Stein M, Biaggioni I, Ertl A, Black B, Robertson D. The neuropathic postural tachycardia syndrome. N Engl J Med. 2000;343:1008–1014. doi: 10.1056/NEJM200010053431404. [DOI] [PubMed] [Google Scholar]
- 34.Peltier AC, Garland E, Raj SR, Sato K, Black B, Song Y, Wang L, Biaggioni I, Diedrich A, Robertson D. Distal sudomotor findings in postural tachycardia syndrome. Clin Auton Res. 2010;20:93–99. doi: 10.1007/s10286-009-0045-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Haensch CA, Tosch M, Katona I, Weis J, Isenmann S. Small-fiber neuropathy with cardiac denervation in postural tachycardia syndrome. Muscle Nerve. 2014;50:956–961. doi: 10.1002/mus.24245. [DOI] [PubMed] [Google Scholar]
- 36.Gibbons CH, Bonyhay I, Benson A, Wang N, Freeman R. Structural and functional small fiber abnormalities in the neuropathic postural tachycardia syndrome. PLoS One. 2013;8:e84716. doi: 10.1371/journal.pone.0084716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Streeten DH. Pathogenesis of hyperadrenergic orthostatic hypotension. Evidence of disordered venous innervation exclusively in the lower limbs. J Clin Invest. 1990;86:1582–1588. doi: 10.1172/JCI114878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bonyhay I, Freeman R. Sympathetic nerve activity in response to hypotensive stress in the postural tachycardia syndrome. Circulation. 2004;110:3193–3198. doi: 10.1161/01.CIR.0000147280.90339.E9. [DOI] [PubMed] [Google Scholar]
- 39.Garland EM, Raj SR, Black BK, Harris PA, Robertson D. The hemodynamic and neurohumoral phenotype of postural tachycardia syndrome. Neurology. 2007;69:790–798. doi: 10.1212/01.wnl.0000267663.05398.40. [DOI] [PubMed] [Google Scholar]
- 40.Abe H, Nagatomo T, Kohshi K, Numata T, Kikuchi K, Sonoda S, Mizuki T, Kuroiwa A, Nakashima Y. Heart rate and plasma cyclic amp responses to isoproterenol infusion and effect of beta-adrenergic blockade in patients with postural orthostatic tachycardia syndrome. J Cardiovasc Pharmacol. 2000;36(Suppl 2):S79–82. doi: 10.1097/00005344-200000006-00017. [DOI] [PubMed] [Google Scholar]
- 41.Shibao C, Arzubiaga C, Roberts LJ, 2nd, Raj S, Black B, Harris P, Biaggioni I. Hyperadrenergic postural tachycardia syndrome in mast cell activation disorders. Hypertension. 2005;45:385–390. doi: 10.1161/01.HYP.0000158259.68614.40. [DOI] [PubMed] [Google Scholar]
- 42.Okamoto LE, Raj SR, Gamboa A, Shibao CA, Arnold AC, Garland EM, Black BK, Farley G, Diedrich A, Biaggioni I. Sympathetic activation is associated with increased il-6, but not crp in the absence of obesity: Lessons from postural tachycardia syndrome and obesity. Am J Physiol Heart Circ Physiol. 2015;309:H2098–2107. doi: 10.1152/ajpheart.00409.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Robertson D, Flattem N, Tellioglu T, Carson R, Garland E, Shannon JR, Jordan J, Jacob G, Blakely RD, Biaggioni I. Familial orthostatic tachycardia due to norepinephrine transporter deficiency. Ann N Y Acad Sci. 2001;940:527–543. doi: 10.1111/j.1749-6632.2001.tb03703.x. [DOI] [PubMed] [Google Scholar]
- 44.Shannon JR, Flattem NL, Jordan J, Jacob G, Black BK, Biaggioni I, Blakely RD, Robertson D. Orthostatic intolerance and tachycardia associated with norepinephrine-transporter deficiency. N Engl J Med. 2000;342:541–549. doi: 10.1056/NEJM200002243420803. [DOI] [PubMed] [Google Scholar]
- 45.Lambert E, Eikelis N, Esler M, Dawood T, Schlaich M, Bayles R, Socratous F, Agrotis A, Jennings G, Lambert G, Vaddadi G. Altered sympathetic nervous reactivity and norepinephrine transporter expression in patients with postural tachycardia syndrome. Circ Arrhythm Electrophysiol. 2008;1:103–109. doi: 10.1161/CIRCEP.107.750471. [DOI] [PubMed] [Google Scholar]
- 46.Bayles R, Harikrishnan KN, Lambert E, Baker EK, Agrotis A, Guo L, Jowett JB, Esler M, Lambert G, El-Osta A. Epigenetic modification of the norepinephrine transporter gene in postural tachycardia syndrome. Arterioscler Thromb Vasc Biol. 2012;32:1910–1916. doi: 10.1161/ATVBAHA.111.244343. [DOI] [PubMed] [Google Scholar]
- 47.Marques FZ, Eikelis N, Bayles RG, Lambert EA, Straznicky NE, Hering D, Esler MD, Head GA, Barton DA, Schlaich MP, Lambert GW. A polymorphism in the norepinephrine transporter gene is associated with affective and cardiovascular disease through a microrna mechanism. Mol Psychiatry. 2017;22:134–141. doi: 10.1038/mp.2016.40. [DOI] [PubMed] [Google Scholar]
- 48.Vincent S, Bieck PR, Garland EM, Loghin C, Bymaster FP, Black BK, Gonzales C, Potter WZ, Robertson D. Clinical assessment of norepinephrine transporter blockade through biochemical and pharmacological profiles. Circulation. 2004;109:3202–3207. doi: 10.1161/01.CIR.0000130847.18666.39. [DOI] [PubMed] [Google Scholar]
- 49.Schroeder C, Tank J, Boschmann M, Diedrich A, Sharma AM, Biaggioni I, Luft FC, Jordan J. Selective norepinephrine reuptake inhibition as a human model of orthostatic intolerance. Circulation. 2002;105:347–353. doi: 10.1161/hc0302.102597. [DOI] [PubMed] [Google Scholar]
- 50.Barbe P, Galitzky J, Riviere D, Senard JM, Lafontan M, Garrigues M, Berlan M. Effects of physiological and pharmacological variation of sympathetic nervous system activity on plasma non-esterified fatty acid concentrations in man. Br J Clin Pharmacol. 1993;36:25–30. doi: 10.1111/j.1365-2125.1993.tb05887.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Murburg MM, Villacres EC, Ko GN, Veith RC. Effects of yohimbine on human sympathetic nervous system function. J Clin Endocrinol Metab. 1991;73:861–865. doi: 10.1210/jcem-73-4-861. [DOI] [PubMed] [Google Scholar]
- 52.Green EA, Raj V, Shibao CA, Biaggioni I, Black BK, Dupont WD, Robertson D, Raj SR. Effects of norepinephrine reuptake inhibition on postural tachycardia syndrome. J Am Heart Assoc. 2013;2:e000395. doi: 10.1161/JAHA.113.000395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fu Q, Vangundy TB, Galbreath MM, Shibata S, Jain M, Hastings JL, Bhella PS, Levine BD. Cardiac origins of the postural orthostatic tachycardia syndrome. J Am Coll Cardiol. 2010;55:2858–2868. doi: 10.1016/j.jacc.2010.02.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jacob G, Shannon JR, Black B, Biaggioni I, Mosqueda-Garcia R, Robertson RM, Robertson D. Effects of volume loading and pressor agents in idiopathic orthostatic tachycardia. Circulation. 1997;96:575–580. doi: 10.1161/01.cir.96.2.575. [DOI] [PubMed] [Google Scholar]
- 55.Stewart JM, Glover JL, Medow MS. Increased plasma angiotensin ii in postural tachycardia syndrome (pots) is related to reduced blood flow and blood volume. Clin Sci (Lond) 2006;110:255–263. doi: 10.1042/CS20050254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Coffin ST, Black BK, Biaggioni I, Paranjape SY, Orozco C, Black PW, Dupont WD, Robertson D, Raj SR. Desmopressin acutely decreases tachycardia and improves symptoms in the postural tachycardia syndrome. Heart Rhythm. 2012;9:1484–1490. doi: 10.1016/j.hrthm.2012.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ruzieh M, Baugh A, Dasa O, Parker RL, Perrault JT, Renno A, Karabin BL, Grubb B. Effects of intermittent intravenous saline infusions in patients with medication-refractory postural tachycardia syndrome. J Interv Card Electrophysiol. 2017;48:255–260. doi: 10.1007/s10840-017-0225-y. [DOI] [PubMed] [Google Scholar]
- 58.Fu Q, VanGundy TB, Shibata S, Auchus RJ, Williams GH, Levine BD. Menstrual cycle affects renal-adrenal and hemodynamic responses during prolonged standing in the postural orthostatic tachycardia syndrome. Hypertension. 2010;56:82–90. doi: 10.1161/HYPERTENSIONAHA.110.151787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mustafa HI, Raj SR, Diedrich A, Black BK, Paranjape SY, Dupont WD, Williams GH, Biaggioni I, Robertson D. Altered systemic hemodynamic and baroreflex response to angiotensin ii in postural tachycardia syndrome. Circ Arrhythm Electrophysiol. 2012;5:173–180. doi: 10.1161/CIRCEP.111.965343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Doherty TAWAA. Mast cell activation disorder in pots. Auton Neurosci. 2018 [Google Scholar]
- 61.Vernino SBM, Hopkins S, Okamoto LE, Black BK, Paranjape SY, Raj SR. The prevalence of ganglionic achr antibodies in poastural tachycardia syndrome (pots) Clin Auton Res. 2016;26:328. [Google Scholar]
- 62.Fedorowski A, Li H, Yu X, Koelsch KA, Harris VM, Liles C, Murphy TA, Quadri SMS, Scofield RH, Sutton R, Melander O, Kem DC. Antiadrenergic autoimmunity in postural tachycardia syndrome. Europace. 2017;19:1211–1219. doi: 10.1093/europace/euw154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wang XL, Ling TY, Charlesworth MC, Figueroa JJ, Low P, Shen WK, Lee HC. Autoimmunoreactive iggs against cardiac lipid raft-associated proteins in patients with postural orthostatic tachycardia syndrome. Transl Res. 2013;162:34–44. doi: 10.1016/j.trsl.2013.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Li H, Yu X, Liles C, Khan M, Vanderlinde-Wood M, Galloway A, Zillner C, Benbrook A, Reim S, Collier D, Hill MA, Raj SR, Okamoto LE, Cunningham MW, Aston CE, Kem DC. Autoimmune basis for postural tachycardia syndrome. J Am Heart Assoc. 2014;3:e000755. doi: 10.1161/JAHA.113.000755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Vernino S. Autoimmunity and autoantibodies in pots: Current state. Auton Neurosci. 2018 [Google Scholar]
- 66.Schondorf R, Benoit J, Stein R. Cerebral autoregulation is preserved in postural tachycardia syndrome. J Appl Physiol (1985) 2005;99:828–835. doi: 10.1152/japplphysiol.00225.2005. [DOI] [PubMed] [Google Scholar]
- 67.Endo A, Fujita Y, Fuchigami T, Takahashi S, Mugishima H, Skatani K. Changes in cerebral blood oxygenation induced by active standing test in children with pots and nms. Adv Exp Med Biol. 2014;812:253–261. doi: 10.1007/978-1-4939-0620-8_34. [DOI] [PubMed] [Google Scholar]
- 68.Ocon AJ, Medow MS, Taneja I, Clarke D, Stewart JM. Decreased upright cerebral blood flow and cerebral autoregulation in normocapnic postural tachycardia syndrome. Am J Physiol Heart Circ Physiol. 2009;297:H664–673. doi: 10.1152/ajpheart.00138.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Medow MS, Del Pozzi AT, Messer ZR, Terilli C, Stewart JM. Altered oscillatory cerebral blood flow velocity and autoregulation in postural tachycardia syndrome. Front Physiol. 2014;5:234. doi: 10.3389/fphys.2014.00234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Del Pozzi AT, Schwartz CE, Tewari D, Medow MS, Stewart JM. Reduced cerebral blood flow with orthostasis precedes hypocapnic hyperpnea, sympathetic activation, and postural tachycardia syndrome. Hypertension. 2014;63:1302–1308. doi: 10.1161/HYPERTENSIONAHA.113.02824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Jordan J, Shannon JR, Black BK, Paranjape SY, Barwise J, Robertson D. Raised cerebrovascular resistance in idiopathic orthostatic intolerance: Evidence for sympathetic vasoconstriction. Hypertension. 1998;32:699–704. doi: 10.1161/01.hyp.32.4.699. [DOI] [PubMed] [Google Scholar]
- 72.Levine BD, Zuckerman JH, Pawelczyk JA. Cardiac atrophy after bed-rest deconditioning: A nonneural mechanism for orthostatic intolerance. Circulation. 1997;96:517–525. doi: 10.1161/01.cir.96.2.517. [DOI] [PubMed] [Google Scholar]
- 73.Tank J, Baevsky RM, Funtova II, Diedrich A, Slepchenkova IN, Jordan J. Orthostatic heart rate responses after prolonged space flights. Clin Auton Res. 2011;21:121–124. doi: 10.1007/s10286-010-0106-2. [DOI] [PubMed] [Google Scholar]
- 74.Parsaik A, Allison TG, Singer W, Sletten DM, Joyner MJ, Benarroch EE, Low PA, Sandroni P. Deconditioning in patients with orthostatic intolerance. Neurology. 2012;79:1435–1439. doi: 10.1212/WNL.0b013e31826d5f95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Burkhardt BE, Fischer PR, Brands CK, Porter CB, Weaver AL, Yim PJ, Pianosi PT. Exercise performance in adolescents with autonomic dysfunction. J Pediatr. 2011;158:15–19. doi: 10.1016/j.jpeds.2010.07.020. 19 e11. [DOI] [PubMed] [Google Scholar]
- 76.Arnold AC, Okamoto LE, Diedrich A, Paranjape SY, Raj SR, Biaggioni I, Gamboa A. Low-dose propranolol and exercise capacity in postural tachycardia syndrome: A randomized study. Neurology. 2013;80:1927–1933. doi: 10.1212/WNL.0b013e318293e310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Shibata S, Fu Q, Bivens TB, Hastings JL, Wang W, Levine BD. Short-term exercise training improves the cardiovascular response to exercise in the postural orthostatic tachycardia syndrome. J Physiol. 2012;590:3495–3505. doi: 10.1113/jphysiol.2012.233858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kimpinski K, Figueroa JJ, Singer W, Sletten DM, Iodice V, Sandroni P, Fischer PR, Opfer-Gehrking TL, Gehrking JA, Low PA. A prospective, 1-year follow-up study of postural tachycardia syndrome. Mayo Clin Proc. 2012;87:746–752. doi: 10.1016/j.mayocp.2012.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lai CC, Fischer PR, Brands CK, Fisher JL, Porter CB, Driscoll SW, Graner KK. Outcomes in adolescents with postural orthostatic tachycardia syndrome treated with midodrine and beta-blockers. Pacing Clin Electrophysiol. 2009;32:234–238. doi: 10.1111/j.1540-8159.2008.02207.x. [DOI] [PubMed] [Google Scholar]
- 80.Sousa A, Lebreiro A, Freitas J, Maciel MJ. Long-term follow-up of patients with postural tachycardia syndrome. Clin Auton Res. 2012;22:151–153. doi: 10.1007/s10286-011-0155-1. [DOI] [PubMed] [Google Scholar]