Abstract
Imaging is increasingly being used in dermatology for documentation, diagnosis, and management of cutaneous disease. The lack of standards for dermatologic imaging is an impediment to clinical uptake. Standardization can occur in image acquisition, terminology, interoperability, and metadata. This paper presents the International Skin Imaging Collaboration position on standardization of metadata for dermatologic imaging. Metadata is essential to ensure that dermatologic images are properly managed and interpreted. There are two standards-based approaches to recording and storing metadata in dermatologic imaging. The first uses standard consumer image file formats, and the second is the file format and metadata model developed for the Digital Imaging and Communication in Medicine (DICOM) standard. DICOM would appear to provide an advantage over using consumer image file formats for metadata as it includes all the patient, study, and technical metadata necessary to use images clinically. Whereas, consumer image file formats only include technical metadata and need to be used in conjunction with another actor—for example, an electronic medical record—to supply the patient and study metadata. The use of DICOM may have some ancillary benefits in dermatologic imaging including leveraging DICOM network and workflow services, interoperability of images and metadata, leveraging existing enterprise imaging infrastructure, greater patient safety, and better compliance to legislative requirements for image retention.
Keywords: Dermatology, Metadata, DICOM, Standards, Enterprise imaging
Introduction
Imaging is increasingly having an important role in dermatology due to the highly visual nature of cutaneous disease. The growth in the use of imaging in dermatology is expected to increase in an exponential manner. Prior to digital still cameras being widely available, dermatologists developed very specific detailed terminology to describe skin conditions in written text in order to document the consultation process [1]. There is an increasing tendency to replace text with digital images particularly in electronic medical records (EMRs). Additionally, the role of imaging is extending beyond documentation to that of diagnosis and management (e.g., pre-surgical margin mapping [2, 3] and sequential dermoscopic imaging [4]). This extended use of imaging has been driven by a number of paradigms: firstly, the increasing range of image acquisition modalities—for example, dermoscopy, total-body photography (TBP), high-frequency ultrasound (HFUS), reflectance confocal microscopy (RCM), and optical coherence tomography (OCT)—to supplement conventional digital photography; secondly, the increasing acceptance and use of teledermatology for remote diagnosis of skin cancer [5]; and thirdly, the maturing of computer-assisted skin lesion analysis and computer-aided diagnosis (CAD) [6].
The lack of standards in dermatologic imaging has been identified as an impediment to the effective implementation of imaging into clinical practice [7]. Dermatologic imaging standardization requires a parallel effort to address image acquisition techniques [8, 9], applied terminology, interoperability, privacy concerns, and metadata. Imaging standardization may result in earlier detection of skin cancer, improved monitoring of skin lesions over time, improved diagnostic accuracy, decreased number of unnecessary biopsies, and therefore a reduction in morbidity and associated costs [1].
In 2013, the International Skin Imaging Collaboration (ISIC) [10] was established across academic, industrial, and community members with the overall objective to develop and disseminate digital standards for dermatologic imaging with the ultimate goal of reducing melanoma mortality. While the ISIC objective specifically includes melanoma as the driving clinical force to lead the standardization of imaging, the overall needs of dermatologic imaging are considered. This paper represents the ISIC position on metadata models for dermatologic imaging after consideration of the following objectives: a description of how metadata is used in current dermatologic imaging, an assessment of available methods for metadata implementation, a critical evaluation of available metadata models in the context of dermatologic imaging, and a proposal to develop standardized metadata definitions for dermatology.
Background
Metadata and Dermatologic Imaging
Metadata is essential to ensure that dermatologic images are properly managed and interpreted [11]. The broad definition of metadata is “data about data” [12]. More specifically, metadata is text-based information that describes the dermatologic imaging study. Metadata is used to assist in diagnostic processes by identifying the patient, identifying the body part imaged, identifying the laterality of the body part imaged, identifying the orientation of the lesion in the image, identifying the magnification factor of the acquired images, recording the level and type of compression in the stored image, recording the pixel size in the stored image thereby allowing geometrical measurement of skin lesions, linking imaging studies to facilitate mapping of changes in a skin lesion over time, and by linking images within an imaging study (e.g., localized, close-up, and dermoscopy) to facilitate accurate identification of skin lesions. Further, metadata is used to record acquisition parameters (e.g., acquisition device, camera settings) thereby enabling auditing compliance to imaging and practice guidelines [8, 13], and enabling sequential reproducibility of imaging. Image parameter metadata (e.g., matrix size, bit depth, photometric interpretation) is necessary for display software to appropriately render the pixel data. Furthermore, metadata is used to index images in a repository (e.g., vendor neutral archive [VNA]) to allow context-based storage and retrieval of images for primary (e.g., clinical) and secondary (e.g., teaching and research) use.
Results
There are two standards-based approaches to recording and storing metadata in dermatologic imaging.
Consumer Image File Formats
The first approach consists of standard consumer image file format—for example, the Tagged Image File Format (TIFF) [14] or the Joint Photographic Experts Group (JPEG) format [15]. In consumer image file formats, metadata is stored at the beginning of an image file as a “header,” though it is usually limited to structural elements describing the format of the pixel data itself. Such headers are often extensible with manufacturer- or industry-specific content. The digital still camera industry, for example, has extended TIFF and JPEG with additional metadata defined by the exchangeable image file format (EXIF) [16]. Consumer image file formats were developed for general imaging applications; however, they can be used in dermatologic imaging. Due to the generalized application, EXIF is limited to storing image acquisition metadata and does not define metadata required in the clinical context (e.g., patient demographics). To address this limitation, dermatologic images stored in consumer image file format need to be linked to a patient’s chart or jacket within an EMR or integrated with dedicated medical image management software. The metadata implemented by an EMR, medical image management software, or acquisition modality vendor are, however, stored in a proprietary database, which may or may not be accessible via a standard application programming interface (API).
DICOM
The second standard approach for recording and storing metadata is the file format and metadata model developed specifically for medical imaging, namely, the Digital Imaging and Communication in Medicine (DICOM) standard. DICOM is a comprehensive, international medical image management standard that, among its many parts, defines standardized, structured, and coded metadata models that are patient-, modality-, and specialty-specific.
DICOM Metadata
The DICOM metadata model includes the necessary patient, study, and technical metadata necessary to use images clinically [17]. In DICOM, there is a discrete metadata definition for different imaging modalities. For example, there is a different metadata definition for computerized tomography (CT) images and ultrasound images. The rationale for this is that, while there may be common metadata items (e.g., patient name) for different image types, there is also fundamentally different metadata—for example, table height and gantry tilt are CT-specific acquisition parameters, whereas transducer frequency is specific to ultrasound imaging.
DICOM metadata definitions are known as Information Object Definitions (IODs). An IOD is an object-oriented (modular) metadata definition and, as such, related metadata attributes are organized into modules. An IOD is the amalgamation of all modules needed to describe an imaging study. The object-orientated design allows modules (e.g., patient module) to be “reused” across different IODs, which facilitate the efficient definition of new IODs as only specialty-specific modules are required to define a new IOD. The growth in adoption of specialty-specific extensions to DICOM is evidence of the effectiveness of the object-orientated strategy [18].
The DICOM metadata definition has also standardized the structure of data values ensuring, for example, consistent date, time, and patient name formats. Further, DICOM has defined sets of code string values, to ensure that values of attributes (e.g., sex, body part examined) will be selected from a pre-defined list of those allowable.
Discussion
Rationale for DICOM
There is a well-recognized need for standards to advance the use of digital imaging in dermatology [1, 7, 11, 19, 20]. If DICOM becomes widely adopted as a standard for dermatologic imaging, there is substantial room for improvement in the form of dermatology-specific metadata extensions (e.g., dermoscopic acquisition technique, photographic parameters, orientation, linked images). Today, dermatological imaging largely uses consumer file formats and there appears to be little impetus to change current practice. Dissemination of DICOM into clinical sites requires substantial technical and workflow challenges to be addressed [17, 21]. For these reasons, it is worthwhile to explore whether DICOM provides advantages over the current practices in dermatologic imaging to warrant the investment of effort.
DICOM is an open standard, meaning the documents that describe technical specifications (e.g., metadata definitions, the commands used in communication protocols) are publically available and any vendor can use them royalty free to implement DICOM into their product set. Whether or not a vendor uses DICOM in their product set is completely voluntary. Therefore, the success of DICOM adoption will be to a significant extent dependent on vendors of dermatologic products adopting the Standard. Consumers (healthcare providers and institutions) have a significant influence since they can determine the functionality they would like to incorporate in their clinical practice and drive a demand supply for DICOM.
It should be noted the use of DICOM is largely transparent to the end user of an imaging network (e.g., a dermatologist). From the perspective of the dermatologist, the use of DICOM is analogous to that of an Internet user who can perform tasks such as browsing and Internet banking without being familiar with the underlying information and communication technology protocols (e.g., hypertext transfer protocol [HTTP], transport layer security [TLS]).
DICOM was originally developed for radiology, where it has become ubiquitous as the core standard on which Picture Archiving and Communications Systems (PACSs) are based. It has since been adopted by many other medical imaging specialties including ophthalmology, dentistry, cardiology, nuclear medicine, oncology, pathology, surgical specialties who perform image-guided surgery (e.g., neurosurgery, ENT, orthopedics), and specialties that acquire endoscopic or laparoscopic imaging. One impetus for the adoption of DICOM into dermatology is the thinking that consistency with the rest of image-producing specialties would be advantageous to dermatology [7, 22]. Further, there is recognition that DICOM would facilitate consistent encoding and non-proprietary metadata [19, 22], which cannot be achieved with the practice of attaching dermatologic images to the patient record in a proprietary database.
DICOM Network and Workflow Services
In addition to standard metadata models, DICOM also defines protocols for the communication of images from one biomedical device (e.g., acquisition modality, image repository, display device) to another. The communication protocols are known as DICOM network services and are used for the electronic storage of images (e.g., from image acquisition modality to image repository) and the subsequent query and retrieval of images from a repository for clinical use. DICOM network services can be used to implement image-based, store-and-forward telehealth consultations by enabling the transmission of images with their embedded metadata from a remote acquisition site to a specialist-end location.
DICOM has been extended with Web (HTTP) services that mirror the traditional network protocols and simplify the implementation within Web browsers and from mobile devices. This family of services, collectively referred to as DICOMweb, includes support for retrieval, storage, and query [23]. These services enable simpler mobile capture and display implementations. For example, these services allow consumer format camera pictures in JPEG format to be uploaded with identifying DICOM metadata in an accompanying text file. The content of JPEG and metadata files can be transcoded into DICOM format at the receiving end, where additional structural and context-specific metadata can also be added. This approach is described in the IHE Web Image Capture (WIC) profile [24]. On retrieval, these services allow a viewer to retrieve either the entire binary DICOM image file, or the image pixel data in JPEG format for direct rendering in a Web browser.
DICOM also defines workflow services that were developed with the goal of improving the efficiency, scalability, and accuracy of image acquisition, storage, and display of medical images [25]. One such workflow service is DICOM Modality Worklist (MWL). MWL allows the operator of an acquisition modality to query a worklist server (e.g., scheduling system, hospital information system) for patient demographics, thereby obviating the need to manually enter patient demographics. The use of MWL is commonplace in radiology and can also be used in other medical specialties—for example, in ophthalmologic imaging, the use of MWL has reduced misnaming or misfiling of images by 76% when compared to manual data entry at the imaging modality [26]. It is recognized that the image acquisition workflow in visible light specialties like dermatology differs from radiology in that it may not involve placement of an order. The acquisition occurs instead in the context of a patient “encounter” and is sometimes referred to as “encounter-based” workflow as distinct from “order-based” workflow [27]. However, such encounters may well still be scheduled (e.g., the clinic visit is scheduled), and even if not, other systems managing the encounter, such as the EMR, can still serve as a suitable source of metadata, potentially mediated using DICOM MWL.
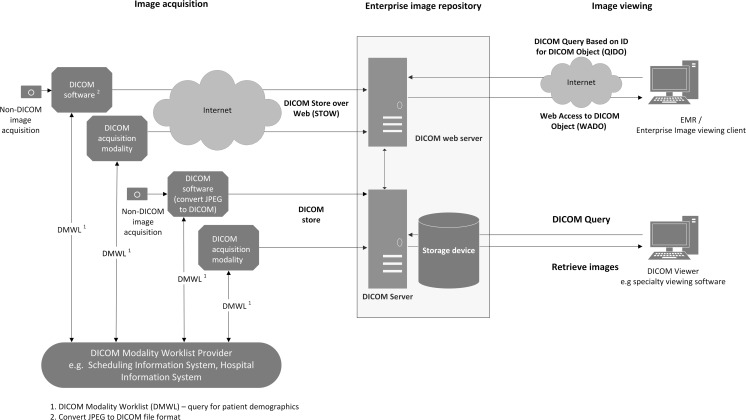
DICOM network and workflow services facilitate an efficient, accurate, and scalable imaging service. A supplementary advantage for using DICOM as the metadata model for dermatologic imaging is that it enables a complete DICOM-based imaging service. Figure 1 demonstrates the architecture of a DICOM-based imaging network.
Fig. 1.
DICOM-based imaging network
Interoperability
DICOM-compliant devices use standardized metadata models, image file formats, and communication protocols resulting in interoperability of both the metadata and images between different devices in an imaging network, regardless of the manufacturer. Interoperability is the ability of two or more information systems or different components within an information system (subsystems) to exchange information and to use the information that has been exchanged [28]. DICOM provides the means to electronically transfer images and associated metadata from one device to another (e.g., acquisition device to image repository) or from one information system to another (e.g., image repository to EMR). The electronic exchange may be intra-organizational or interorganizational.
The interoperability afforded by DICOM allows separation of the imaging subsystems, namely acquisition, storage, and display. Separation of imaging subsystems can reduce hardware redundancy and allow “best of breed” selection of each device in the imaging pipeline. Further, it can improve the efficiency of an imaging network from both clinical and management perspectives by removing the need to interact with multiple equipment and information system components [11]. Often, dermatologic imaging storage is distributed (as opposed to centralized), meaning images are stored on the acquisition modality or on an image management system within the dermatology department, which inhibits a patient-centric view of all dermatologic imaging. Having images archived in a central repository (as opposed to modality or departmental storage systems) enables treating physicians to overcome this limitation and have instant access to all the patient images. It also allows for other departments (e.g., histopathology) to view images [17], which may aid interpretation [29]. The use of a centralized infrastructure managed as an enterprise-wide initiative may also mitigate cost, scalability, management, reliability, availability, and security concerns.
Enterprise Imaging
Centralized management of imaging most often occurs in large hospitals or integrated groups of ambulatory facilities that share a common infrastructure [17]. This approach is known as Enterprise Imaging [30] and typically uses a so-called VNA, which is an Enterprise Image Repository (EIR) that consolidates images and imaging documents (e.g., diagnostic reports) from multiple feeder sources and departments, and is agnostic to the vendor that created or consumes the images, hence the name. An EIR often contains multiple storage levels including a disaster recovery archive. This architecture ensures high levels of compliance to legislative requirements for the retention of medical records (which includes images) [31]. Further, EIRs provide economies of scale for computer hardware infrastructure and the trained support personnel required to manage the archive [17, 32]. Progressive consolidation of healthcare providers into larger organizations additionally drives the trend towards enterprise imaging.
An EIR typically uses DICOM as the underlying file format and imaging communication protocol. Complementary healthcare interoperability standards such as HL7 are also used by EIRs [33]. HL7 is used to exchange text-based information (as opposed to images) between information systems (e.g., sending the diagnostic imaging report from the radiology information system to the EMR). The Integrating the Healthcare Enterprise (IHE) initiative ensures the consistent use of DICOM and HL7 to achieve interoperability [34]. IHE publishes technical frameworks containing integration profiles that stipulate which HL7 and DICOM transactions should be used to achieve interoperability for a specific-use case. For example, an EIR that supports the IHE Invoke Image Display (IID) profile [35] allows a single (but configurable) method to display medical images from an EMR. There is little doubt that generic enterprise image viewing software would be deficient in some of the diagnostic functionality that is currently provided by specialist dermatologic imaging software (e.g., lesion mapping in TBP, CAD). Hence, it is important to maintain the ability to view, process, and analyze dermatologic images with specialist software even if images are stored in a central repository like an EIR. The same issue was encountered in cardiology and radiology with the advent of coronary artery analysis software and CT colonography [36]. The solution was to launch the specialist image processing and analysis software from a generic PACS workstation. Customized context integration between the generic PACS and specialist software allowed a selected study to be loaded automatically. In a multi-vendor environment, standards defining how a hosting system interacts with hosted applications are useful. The IID profile can be used to launch specialist software from within a viewer or another application [29]. The same approach can be used to perform specialist dermatologic image processing.
It is also possible to archive and distribute consumer format images without encapsulating them in DICOM, by transmitting, storing, and indexing the metadata separately from the images, and treating the images as if they were just like any other kind of “document.” Three different methods to do this have arisen in practice:
Proprietary document content management systems,
Proprietary electronic medical record systems that are image-enabled,
Systems that support the IHE cross-enterprise document sharing (XDS) profile [37].
The primary advantages of such approaches are the convenience of being able to store and retrieve the images in their original form without having to encapsulate and extract them from DICOM (which requires specialized software), and the ease of integration with indexing and access mechanisms that are common to all types of persistent objects. The primary disadvantages are the need to develop viewers for image content, since images are not documents, the lack of standardization of specialized metadata beyond identifiers and relatively simple descriptors, and the difficulty of export of the metadata with the images, whether for transport to another site or system, or migration at the end of product life. If such a non-DICOM approach is to be taken, it is at least preferable that some sort of standard be used, and IHE XDS is an improvement over entirely proprietary approaches.
It is also possible to store DICOM files directly using XDS, as if each DICOM image was a document. There is a specialization of XDS, known as cross-enterprise document sharing for imaging (XDS-I) [38]. XDS-I can be used to implement an XDS architecture specifically for large numbers of DICOM image files, by storing a manifest (list) of DICOM files for each archived study as an XDS document and referencing their location in another system, from which the images are accessible by various means (DICOM, WADO, and using XDS transport).
An EIR can enable interorganizational sharing of DICOM or non-DICOM images using either proprietary portals, XDS or XDS-I, thereby allowing an authorized, authenticated clinician from an external organization to query and retrieve images. DICOMweb services are also intended to facilitate image sharing beyond the enterprise, and particularly for physician and patient portals accessed via mobile devices. There is growing use of third-party government-funded or commercial services that provide national or regional repositories of images for radiology and cardiology. These typically provide access via standard DICOM, DICOMweb, and XDS-I services. Image exchange on standard DICOM CDs remains widespread in radiology and cardiology, and the same mechanism can be used for dermatology images. Encrypted email is not commonly used, and unsecured email of images containing or accompanied by identifying information should be avoided.
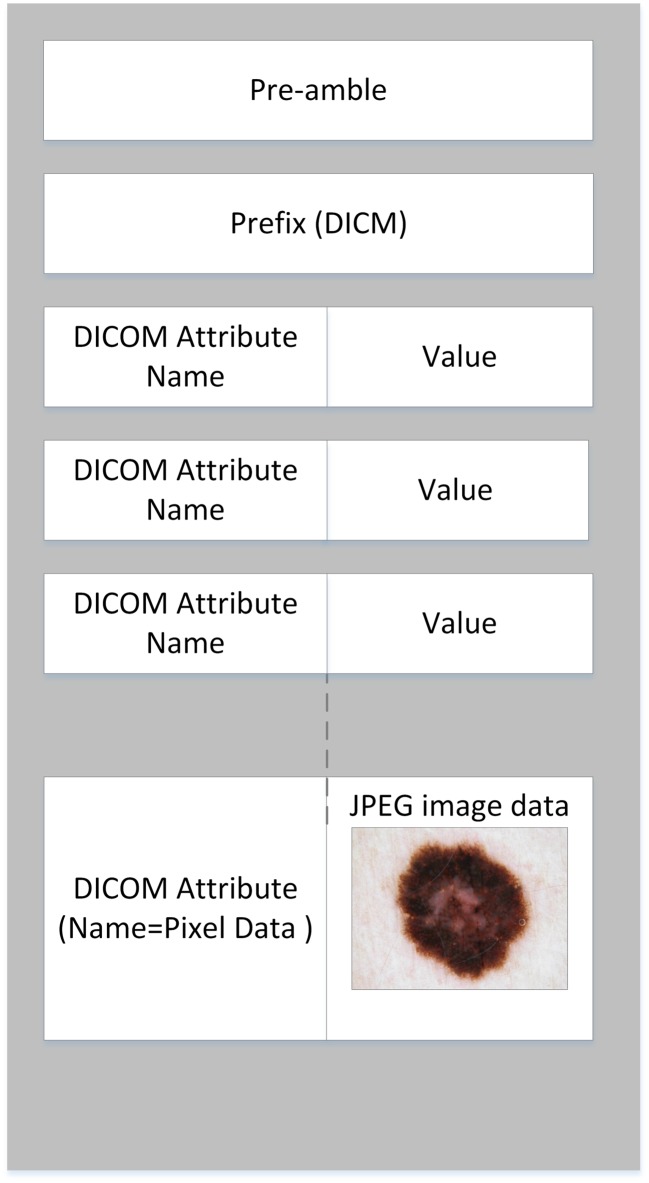
DICOM File Format
A DICOM file is the amalgamation of the metadata and pixel data within a single file. Any type of image file can be encoded as a DICOM file using the template shown in Fig. 2. DICOM did not try to develop new image compression standards and instead relied on existing International Standards Organization (ISO) standards [11]. For example, for visible light images, the pixel data in a DICOM file is usually encoded in JPEG lossy compressed format. One limitation of the current DICOM information model is that it does not yet define attributes to encode photographic camera technique metadata, though this may be present in the DICOM-encapsulated JPEG bit stream as EXIF [17]. Use of the DICOM file format may improve patient safety by ensuring there is no risk of separation of the image and the relevant metadata (e.g., patient demographics) [39]. The DICOM file format may simplify the electronic exchange as it allows images and metadata to be transmitted as a single transaction, whereas the use of consumer image file formats would require one transaction for the transfer of images and a second, often proprietary, transaction to transfer the metadata. Hence, the American Telemedicine Association has promoted the use of DICOM for teledermatology [22].
Fig. 2.
DICOM file format template
Image Migration
When replacing legacy imaging modalities or image repositories, it may be necessary to migrate data to the replacement system for reasons including clinical continuity, requirements for medical record retention, to avoid vendor “lock in,” and to avoid having to maintain obsolete imaging equipment as a means of maintaining non-migrated data. The use of DICOM facilitates the migration of images and metadata from one repository to another in a way that mitigates many of the technical challenges that arise with data migration from proprietary databases [40]. This method also reduces the cost of migration and improves fidelity of migrated data [41].
Privacy, Sensitivity of Access, and De-Identification
In any clinical system, all medical records (including images) need to be reliably linked to a specific patient’s identity. In DICOM, this is achieved by embedding an identifying number such as a medical record number in the metadata, along with various relevant patient descriptive attributes such as name, age, sex, and date of birth. Since in a clinical setting, the patient is and needs to be identifiable, the issue of being able to identify the patient by looking at the content of the image pixel data itself does not arise.
However, with visible light images, the explicit nature of the images may give rise to sensitivity about which users have permission to view images. Such concerns arise less often for other specialties, such as radiology or cardiology, except perhaps in the case of celebrity patients. Access control based on user role, patient category, and image type is usually handled in the EMR, PACS, and EIR by implementation-specific mechanisms. Authenticated user identity can be communicated by standard mechanisms to assist with control, i.e., access may be denied except to designated members of the appropriate care team. Confidentiality constraints can also be explicitly communicated in DICOM metadata attributes, though this is rarely implemented.
For teaching, and research purposes, actual patient identity may need to be removed from both the metadata and the pixel data. This is true whether the pixel data contains an identifiable body part, such as the face, or a visible label in the field of view, such as a paper identity strip. DICOM defines which metadata attributes need to be de-identified in a standard profile [42, 43]. Blacking out (redacting) pixel data may be performed as necessary. DICOM attributes are available that define whether or not the metadata or pixel data contains identifying information and whether or not it has been de-identified and in what manner. Even for lossy compressed images, techniques have been developed that allow for minimal loss when redacting JPEG pixel data, including that encapsulated in DICOM images [44].
Current State of DICOM and Dermatology
To date, there have been only a few early adopters of DICOM for dermatologic imaging—notably, the US Department for Veteran’s Affairs [25]. There is no dermatology-specific IOD currently defined in DICOM. However, camera-acquired images, or indeed any true color image, can be encoded in DICOM format using general-purpose IODs, namely the Visible Light (VL) Photographic image and Secondary Capture (SC) image IODs. However, these IODs lack a rich specialty-specific metadata model that represents one of the advantages of using DICOM for dermatologic imaging. Some incremental progress is being made—for example, work is in progress to add a standard list of codes for dermatology anatomic sites (based on the New York University Interdisciplinary Melanoma Cooperative Group’s numbering system) to the base standard [45]. Photographic images that have been acquired in consumer formats can be encapsulated as a DICOM VL Photographic object by way of import software that associates metadata with the image (e.g., the JPEG compressed pixel data) and “wraps” them together in a DICOM format, without loss of image fidelity [17]. There is an increasing number of cameras, mobile device applications, and dermatoscopes that can natively acquire images in DICOM formats [46]. DICOM currently contains IODs for HFUS and OCT. The Ophthalmology group (WG09) added the latter. Some dermatology applications generate relatively large-sized images and large numbers of images, for example, whole body photography. Large numbers of DICOM images are not a particular concern for archival size or performance, since radiology and cardiology studies are typically very large, and visible light images are lossy compressed. However, storage of a single image of the whole body with a very large number of rows and columns can be challenging. A similar problem has been addressed in DICOM Whole Slide images used for anatomical pathology slide microscopy applications by the use of multi-frame images where each frame is a tile in a larger array [47].
There are many mature parts to DICOM that could currently be used in dermatology and many bodies of work that are currently being undertaken under the auspices of DICOM that will be of benefit to the dermatology community, for example, methods of color standardization [48], processes to support clinical trials and research using imaging, technical solutions to provide security during information exchange, and methods to utilize standard Web services for use in medical imaging. In addition to the encapsulation of consumer image file formats, portable document format (PDF) files can also be encapsulated into a DICOM object. This may allow supplementary information (e.g., referral information) to be linked to an image. Ancillary IODs (e.g., DICOM Structured Reports [SRs]) have been defined for image interpretation results. There are likely advantages to dermatology by leveraging these existing efforts in imaging.
Working Group 19 Dermatology
Extension of DICOM is undertaken by working groups (WGs) who advance discrete bodies of work. The DICOM Standards Committee (DSC) provides governance of the working groups. Working groups are comprised of manufacturing companies, service organizations, consulting companies, biomedical professional organizations, trade associations, other standards-developing organizations, and government agencies worldwide [49]. There is currently no active DICOM WG dedicated to dermatologic imaging. A previous attempt to develop dermatology-specific extensions to the DICOM standard was abandoned in 2009, when the dermatologic imaging group (WG 19) disbanded. At that time, dermatologic imaging was largely limited to digital still photography using commercial off-the-shelf cameras and used primarily for non-diagnostic purposes, and the existing VL Photographic IOD was deemed to be sufficient for interoperability. The lack of dermatology-specific vendor investment in standards development was cited as a reason for suspending the effort [50].
A Potential Adoption Roadmap
WG 19 could reconvene to develop dermatology-specific extensions to DICOM. It is useful to consider the experience of another specialty-specific group, WG 09 Ophthalmology. A case study on how ophthalmic-specific extensions to the DICOM standard was developed for ocular imaging has been published [51]. This paper describes achievements of the ophthalmology WG over a 12-year time period and serves to highlight that endorsement by clinical professional bodies (e.g., American Academy of Ophthalmology, American Glaucoma Society) is an enabler of success. Additionally, the timeframes highlight that standards development is a continual cycle of refinement and enhancement, in part due to the snowballing use of imaging afforded by standardization and in part due to a changing technological landscape.
A logical first step in developing dermatologic-specific extensions to the DICOM standard is to develop metadata definitions (i.e., IODs) for dermoscopic images (dermoscopy is a non-invasive diagnostic technique that links clinical dermatology and dermatopathology by enabling the visualization of morphological features not seen by the naked eye [52]), followed potentially by the development of structured report IODs. Due to the object-oriented architecture of DICOM, most of the work has been done with module definitions that are common to all image IODs (e.g., patient, general study, general series, general equipment, general image). We have learned from the development of ophthalmic extensions to the DICOM standard that additional modules (e.g., ophthalmic image, ocular region imaged, ophthalmic photograph acquisition parameters, and ophthalmic photographic parameters) are required. The additional modules required for dermatology are likely to be similar to what was developed for ophthalmology.
Currently, visible light IODs can be used to encapsulate skin imaging from an external camera into DICOM format. Determination will have to be done whether visible light objects could be enriched with dermatologic metadata to enhance their use for dermatology, or alternatively whether a specific dermatologic photography IOD is needed.
One potential area of enrichment is defining DICOM attributes that can encode EXIF metadata, which describe the photographic technique used and are currently lacking in DICOM. These describe such things as exposure, sensitivity, focal length, and other camera-related factors. They are not dermatology-specific but are generally applicable to external photography, and work is in progress [53] to add them since the International Color Consortium Medical Imaging Working Group (ICC MIWG) identified their absence [48].
Further, determination will be required to see if existing ultrasound IODs are suitable for the HFUS examination performed in dermatology and similarly whether existing OCT IODs are suitable for dermatology. RCM and dermoscopy are likely to require the development of new IODs. In their proposal for standardization, the International Dermoscopy Society has identified standardized metadata that will inform both image and structured report IODs [20].
In 2009, Madden predicated that one of the drivers for standards in dermatology would be “those who provide services that require all imaging specialties to be integrated into the digital healthcare infrastructure [50].” There is now widespread recognition that the EMR is the primary point of contact between clinicians and all patient-related information, hence the integration of all imaging systems with that infrastructure is key. To this end, there has been the establishment of an Enterprise Imaging collaborative working group between the Society of Imaging Informatics in Medicine (SIIM) and the Healthcare Information and Management Systems Society (HIMSS) [30]. This collaboration is contributing to efforts to extend existing standards like DICOM for skin imaging and other medical specialties.
Conclusion
In dermatology, standardization of imaging is relatively immature. Hence, the development of standards for dermatology will require substantial and protracted investment. DICOM would appear to provide advantage over using consumer image file formats for metadata. This is because the DICOM metadata model includes all the patient, study, and technical metadata necessary to use images clinically. Whereas, consumer image file formats only include technical metadata and need to be used in conjunction with another actor (e.g., EMR) to supply the patient and study metadata. There are numbers of spinoffs to using the DICOM metadata model. These include leveraging DICOM network and workflow services to implement an efficient, accurate, and scalable imaging network; being able to transfer images and metadata in a single transaction thereby facilitating teledermatology; interoperability of images and metadata; interorganizational and intra-organizational image sharing; leveraging existing infrastructure; greater patient safety; and better compliance to legislative requirements for image retention. The beneficiaries of these advantages are likely to be larger institutions that have multi-modality dermatologic imaging and an enterprise imaging strategy, use an EMR, conduct research, and practice teledermatology. Whether DICOM provides advantages over the current practices in dermatologic imaging to warrant the investment of effort for dermatology to adopt DICOM is likely a question that can only be answered after DICOM has been tried in more real-world dermatology implementations. These implementations will be needed to quantify both the cost of adoption and the benefits gained, but it is expected that the economies of scale and mitigation of risk inherent in standardized enterprise-wide rather than isolated proprietary departmental solutions will prevail. Both commercial and open-source tools for conversion of consumer format images to DICOM are readily available, so this hypothesis is easily tested.
Acknowledgments
The authors acknowledge the contribution of the International Skin Imaging Collaboration: Melanoma Project working group members. We acknowledge David Clunie as co-first author of this manuscript.
Funding Information
Liam Caffery receives funding under a collaborative research agreement between Memorial Sloan Kettering Cancer Center and The University of Queensland. Liam Caffery and H. Peter Soyer are supported in part by the Centre of Research Excellence in Telehealth funded by Australia’s National Health and Medical Research Council (NHMRC APP1061183). Allan Halpern is supported in part by the National Institutes of Health/National Cancer Institute Cancer Center Support Grant P30 CA008748.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- 1.Hibler BP, Qi QC, Rossi AM. Current state of imaging in dermatology. Semin Cutan Med Surg. 2016;35:2–8. doi: 10.12788/j.sder.2016.001. [DOI] [PubMed] [Google Scholar]
- 2.Alawi SA, Kuck M, Wahrlich C, et al. Optical coherence tomography for presurgical margin assessment of non-melanoma skin cancer - a practical approach. Exp Dermatol. 2013;22:547–551. doi: 10.1111/exd.12196. [DOI] [PubMed] [Google Scholar]
- 3.Chen CS, Elias M, Busam K, Rajadhyaksha M, Marghoob AA. Multimodal in vivo optical imaging, including confocal microscopy, facilitates presurgical margin mapping for clinically complex lentigo maligna melanoma. Br J Dermatol. 2005;153:1031–1036. doi: 10.1111/j.1365-2133.2005.06831.x. [DOI] [PubMed] [Google Scholar]
- 4.Tromme I, Devleesschauwer B, Beutels P et al.: Selective Use of Sequential Digital Dermoscopy Imaging Allows a Cost Reduction in the Melanoma Detection Process: A Belgian Study of Patients with a Single or a Small Number of Atypical Nevi. Plos One. 9, 2014 [DOI] [PMC free article] [PubMed]
- 5.Bashshur RL, Shannon GW, Tejasvi T, Kvedar JC, Gates M. The Empirical Foundations of Teledermatology: A Review of the Research Evidence. Telemed J E Health. 2015;21:953–979. doi: 10.1089/tmj.2015.0146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Esteva A, Kuprel B, Novoa RA, et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature. 2017; 542: 115−+. [DOI] [PMC free article] [PubMed]
- 7.Marghoob AA, International Skin Imaging Collaboration Melanoma Project Working G Standards in Dermatologic Imaging. Jama Dermatol. 2015;151:819–821. doi: 10.1001/jamadermatol.2015.32. [DOI] [PubMed] [Google Scholar]
- 8.Finnane A, Curiel-Lewandrowski C, Wimberley G, et al. Proposed Technical Guidelines for the Acquisition of Clinical Images of Skin-Related Conditions. Jama Dermatol. 2017;153:453–457. doi: 10.1001/jamadermatol.2016.6214. [DOI] [PubMed] [Google Scholar]
- 9.Katragadda C, Finnane A, Soyer HP, et al. Technique Standards for Skin Lesion Imaging A Delphi Consensus Statement. Jama Dermatol. 2017;153:207–213. doi: 10.1001/jamadermatol.2016.3949. [DOI] [PubMed] [Google Scholar]
- 10.International Society for Digital Imaging of the Skin ISIC Project 2017 Available at:http://isdis.net/isic-project/ (Accessed: December 2017)
- 11.Gibaud B. The quest for standards in medical imaging. Eur J Radiol. 2011;78:190–198. doi: 10.1016/j.ejrad.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 12.Baca M and Getty Research Institute. Introduction to metadata. Third edition. ed. Los Angeles: Getty Research Institute, 2016, p.pages cm.
- 13.McKoy K, Antoniotti NM, Armstrong A, et al. Practice Guidelines for Teledermatology. Telemed J E Health. 2016;22:981–990. doi: 10.1089/tmj.2016.0137. [DOI] [PubMed] [Google Scholar]
- 14.Aldus Corporation TIFF Revision 6.0 1992 Available at:https://www.itu.int/itudoc/itu-t/com16/tiff-fx/docs/tiff6.pdf (Accessed: December 2017)
- 15.JPEG Standard for digital compression and encoding of continuous-tone still images. Part 1 - Requirements and implementation guidelines. International Standards Organisation/International Electrotechincal Commission, 1994.
- 16.Camera and Imaging Products Association Exchangeable Image File Format for Digital Still Cameras - CIPA DC-008, JEITA CP-3451C Translation 2016 Available at:http://cipa.jp/std/documents/e/DC-008-Translation-2016-E.pdf (Accessed: December 2017)
- 17.Clunie DA, Dennison DK, Cram D, Persons KR, Bronkalla MD, Primo HR. Technical Challenges of Enterprise Imaging: HIMSS-SIIM Collaborative White Paper. J Digit Imaging. 2016;29:583–614. doi: 10.1007/s10278-016-9899-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bidgood WD, Jr, Horii SC. Modular extension of the ACR-NEMA DICOM standard to support new diagnostic imaging modalities and services. J Digit Imaging. 1996;9:67–77. doi: 10.1007/BF03168859. [DOI] [PubMed] [Google Scholar]
- 19.Quigley EA, Tokay BA, Jewell ST, Marchetti MA, Halpern AC. Technology and Technique Standards for Camera-Acquired Digital Dermatologic Images A Systematic Review. Jama Dermatol. 2015;151:883–890. doi: 10.1001/jamadermatol.2015.33. [DOI] [PubMed] [Google Scholar]
- 20.Malvehy J, Puig S, Argenziano G, Marghoob AA, Soyer HP. International Dermoscopy Society Board m. Dermoscopy report: proposal for standardization. Results of a consensus meeting of the International Dermoscopy Society. J Am Acad Dermatol. 2007;57:84–95. doi: 10.1016/j.jaad.2006.02.051. [DOI] [PubMed] [Google Scholar]
- 21.Towbin AJ, Roth CJ, Bronkalla M, Cram D. Workflow Challenges of Enterprise Imaging: HIMSS-SIIM Collaborative White Paper. J Digit Imaging. 2016;29:574–582. doi: 10.1007/s10278-016-9897-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Krupinski E, Burdick A, Pak H, et al. American Telemedicine Association’s Practice Guidelines for Teledermatology. Telemed J E Health. 2008;14:289–302. doi: 10.1089/tmj.2007.0129. [DOI] [PubMed] [Google Scholar]
- 23.DICOM Standards Committee DICOM PS3.18. Web Services 2017 Available at: http://dicom.nema.org/medical/dicom/current/output/chtml/part18/PS3.18.html (Accessed: December 2017)
- 24.Integrating the Healthcare Enterprise Web-based Image Capture 2017 Available at: http://wiki.ihe.net/index.php/Web-based_Image_Capture (Accessed: December 2018)
- 25.Caffery L. An Analysis of DICOM and Its Use for Image Management and Communication in Store-and-Forward Telehealth. In: Raad H, editor. Telemedicine. Hauppauge, NY: Nova Science Publishers, Inc.; 2015. pp. 33–534. [Google Scholar]
- 26.Pandit RR, Boland MV. Impact of Digital Imaging and Communications in Medicine Workflow on the Integration of Patient Demographics and Ophthalmic Test Data. Ophthalmology. 2015;122:227–232. doi: 10.1016/j.ophtha.2014.08.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cram D, Roth CJ, Towbin AJ. Orders- Versus Encounters-Based Image Capture: Implications Pre- and Post-Procedure Workflow, Technical and Build Capabilities, Resulting, Analytics and Revenue Capture: HIMSS-SIIM Collaborative White Paper. J Digit Imaging. 2016;29:559–566. doi: 10.1007/s10278-016-9888-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.IEEE Standard Computer Dictionary: A Compilation of IEEE Standard Computer Glossaries. IEEE Std 610. 1991: 1–217.
- 29.Ferrara G, Argenyi Z, Argenziano G et al.: The Influence of Clinical Information in the Histopathologic Diagnosis of Melanocytic Skin Neoplasms. Plos One. 4, 2009 [DOI] [PMC free article] [PubMed]
- 30.Roth CJ, Lannum LM, Persons KRA. Foundation for Enterprise Imaging: HIMSS-SIIM Collaborative White Paper. Journal of Digital Imaging. 2016;29:530–538. doi: 10.1007/s10278-016-9882-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Scheinfeld N. Photographic images, digital imaging, dermatology, and the law. Arch Dermatol. 2004;140:473–476. doi: 10.1001/archderm.140.4.473. [DOI] [PubMed] [Google Scholar]
- 32.Karthiyayini M, Thavavel V and Selvam NS. Cloud based Vendor Neutral Archive: Reduces Imaging Rates and Enhances Patient Care. Icaccs 2015 Proceedings of the 2nd International Conference on Advanced Computing & Communication Systems. 2015.
- 33.Langer SG, Persons K, Erickson BJ, Blezek D. Towards a more cloud-friendly medical imaging applications architecture: a modest proposal. J Digit Imaging. 2013;26:58–64. doi: 10.1007/s10278-012-9545-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Siegel EL, Channin DS. Integrating the Healthcare Enterprise: A Primer. Radiographics. 2001;21:1339–1341. doi: 10.1148/radiographics.21.5.g01se381339. [DOI] [PubMed] [Google Scholar]
- 35.Integrating the Healthcare Enterprise Invoke Image Display Rev. 1.3 - Trial Implementation 2016 Available at: https://www.ihe.net/uploadedFiles/Documents/Radiology/IHE_RAD_Suppl_IID.pdf (Accessed: December 2017)
- 36.Wang KC, Filice RW, Philbin JF, Siegel EL, Nagy PG. Five Levels of PACS Modularity: Integrating 3D and Other Advanced Visualization Tools. Journal of Digital Imaging. 2011;24:1096–1102. doi: 10.1007/s10278-011-9366-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Integrating the Healthcare Enterprise IHE IT Infrastructure (ITI) Technical Framework Volume 1 (ITI TF-1) Integration Profiles 2017 Available at: https://www.ihe.net/uploadedFiles/Documents/ITI/IHE_ITI_TF_Vol1.pdf (Accessed: December 2017)
- 38.Seifert P. Intergrating the Healthcare Enterprise Cross-Enterprise Document Sharing for Imaging (XDS-I.b) 2011 Available at: http://www.ihe.net/Technical_Framework/upload/IHE_RAD_Suppl_XDS-I-b_Rev1-2_TI_2011-02-18.pdf (Accessed: September 2017)
- 39.Caffery L. Teledermatology PACS. In: Soyer HP BM, Smith AC, Wurm EMT, (ed.). Telemedicine in dermatology. Heidelberg: Springer, 2012, p. 133–42.
- 40.van Ooijen PMA, Aryanto KY, Broekema A, Horii S. DICOM data migration for PACS transition: procedure and pitfalls. Int J Comput Ass Rad. 2015;10:1055–1064. doi: 10.1007/s11548-014-1123-8. [DOI] [PubMed] [Google Scholar]
- 41.Behlen FM, Sayre RE, Weldy JB, Michael JS. “Permanent” records: Experience with data migration in radiology information system and picture archiving and communication system replacement. Journal of Digital Imaging. 2000;13:171–174. doi: 10.1007/BF03167653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.DICOM Standards Committee DICOM PS3.15 Security and Sytem Managment Profiles. Annex E- Attribute Confidentiality Profiles 2017 Available at: http://dicom.nema.org/medical/dicom/current/output/chtml/part15/chapter_E.html (Accessed: December 2017)
- 43.Freymann JB, Kirby JS, Perry JH, Clunie DA, Jaffe CC. Image Data Sharing for Biomedical Research-Meeting HIPAA Requirements for De-identification. Journal of Digital Imaging. 2012;25:14–24. doi: 10.1007/s10278-011-9422-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Clunie DA, Gebow D: Block selective redaction for minimizing loss during de-identification of burned in text in irreversibly compressed JPEG medical images. J Med Imaging. 2, 2015 [DOI] [PMC free article] [PubMed]
- 45.National Electrical Manufacturers Association CP-1674 - Add Dermatology Anatomic Site Context Group and NYU Numbering System Coding Scheme 2016 Available at: ftp://medical.nema.org/medical/dicom/cp/cp1674_02_nyuskinlesionnumbering.pdf (Accessed: December 2017)
- 46.Cram D, Stratton R, Clark S. Review of Dicompass DICOM Camera App for Android. Journal of Digital Imaging. 2016;29:3–6. doi: 10.1007/s10278-015-9854-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.DICOM Standards Committee, Working Group 26, Pathology Supplement 145: Whole Slide Microscopic Image IOD and SOP Classes 2010 Available at: ftp://medical.nema.org/medical/dicom/final/sup145_ft.pdf (Accessed: December 2017)
- 48.Badano A, Revie C, Casertano A, et al. Consistency and Standardization of Color in Medical Imaging: a Consensus Report. Journal of Digital Imaging. 2015;28:41–52. doi: 10.1007/s10278-014-9721-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.National Electrical Manufacturers Association Procedures for the DICOM standards committe 2015 Available at: http://dicom.nema.org/Dicom/Geninfo/Procedures.htm (Accessed: December 2017)
- 50.Madden BC. A propsal for Working Group 19 - Dermatologic Standards 2009 Available at: http://dicom.nema.org/dicom/minutes/wg-06/2009/2009-08-24/dicom-dermatology-whitepaper.doc (Accessed: September 2017)
- 51.Boland MV, Schuman JS, Mattox CG, Soc AG. American Glaucoma Society Position Statement: Electronic Data Standards for Clinical Practice. J Glaucoma. 2013;22:174–175. doi: 10.1097/IJG.0b013e318231205d. [DOI] [PubMed] [Google Scholar]
- 52.Argenziano G, Soyer HP. Dermoscopy of pigmented skin lesions--a valuable tool for early diagnosis of melanoma. Lancet Oncol. 2001;2:443–449. doi: 10.1016/S1470-2045(00)00422-8. [DOI] [PubMed] [Google Scholar]
- 53.National Electrical Manufacturers Association CP-1736 - Add Visible Light Photography Attributes corresponding to EXIF 2.31 2017 Available at: ftp://medical.nema.org/medical/dicom/cp/cp1736_01_EXIF.pdf (Accessed: December 2017)