Abstract
Background and Aims
Opioid use disorder [OUD] has become a public health crisis among patients with chronic disease. Inflammatory bowel disease [IBD] patients are at high risk for OUD because they suffer from chronic relapsing-remitting pain. We aimed to describe the prevalence and trends in OUD-related diagnoses among hospitalised IBD patients.
Methods
A retrospective study was performed using weighted Nationwide Inpatient Sample data from 2005 to 2014. Adult IBD hospital visits and OUD-related diagnoses were identified using a previously published schema. Annual diagnoses were calculated. Characteristics associated with OUD were assessed using multivariable logistic regression. Associations between OUD and length of stay were assessed overall and separately for surgical and non-surgical stays.
Results
In all, 2.2% of 2585174 weighted discharges with any diagnosis of IBD also had an OUD-related diagnosis, with an 8.8% average annual increase. In multivariable analysis, Crohn’s disease, public payer or no insurance, and psychiatric comorbidities were associated with a higher likelihood of OUD, whereas a primary diagnosis of an IBD-related complication was associated with a lower likelihood. An OUD-related diagnosis was associated with 0.84 days (95% confidence interval [CI] 0.71, 0.97] increased length of stay overall, 2.79 days [95% CI 1.44, 4.14] for surgical stays, and 0.71 days [95% CI 0.59, 0.82] for non-surgical stays.
Conclusions
OUD-related diagnoses are increasing among IBD patients and are associated with increased length of stay. With a rising prevalence, it is important to screen and diagnose OUD in IBD and refer patients for evidence-based treatment to address unmet patient needs and reduce health care utilisation.
Keywords: Substance abuse, Crohn’s disease, ulcerative colitis
1. Introduction
Opioid use disorder [OUD] has reached epidemic proportions with an estimated 2 million Americans currently having a prescription OUD and over 12 million reporting a history of opioid misuse.1,2 OUD is defined as a pattern of opioid use leading to clinically significant impairment and is diagnosed using criteria in the Diagnostic and Statistical Manual of Mental Disorders.3 As opioid prescribing has risen, the number of OUD deaths has nearly quadrupled.4,5 OUD inpatient hospital stays rose 64.1% in the past decade, a 5.7% annual growth rate.6 In response to this epidemic, the Center for Disease Control recently published guidelines on the management of chronic non-cancer pain, reserving prescription opioids only for those where benefits outweigh the risks.7,8
Inflammatory bowel disease [IBD] is a relapsing-remitting chronic disease requiring regular access to health care. Patients with IBD are frequently prescribed opioids and are therefore at risk for OUD-related diagnoses.9 Given that abdominal pain is prevalent in IBD and patients often require procedures or surgical interventions, adequate pain control can be challenging. Furthermore, other pain-related diagnoses such as irritable bowel syndrome, ankylosing spondylitis, and peripheral arthritis can co-exist in IBD and can cause further debilitation. Accompanying psychosocial disorders may put these patients at additional risk for OUD.10
An estimated 17% of IBD patients report opioid use and two-thirds of those have associated misuse behaviour.11–13 A recent study by Burr et al. evaluated the trend in opioid prescribing using a population-based database of IBD patients in the UK.14 Opioid prescriptions increased steadily over the study period, and heavy use was associated with an increase in all-cause mortality.14 We aimed to determine the prevalence and trends associated with OUD among hospitalised IBD patients, using a US nationally representative sample. We hypothesised a prevalence of OUD among hospitalised IBD patients greater than 1%, presuming a prevalence higher than the national prevalence estimate in the general population of 0.8%.15
2. Methods
A retrospective cross-sectional observational study was performed using Nationwide Inpatient Sample [NIS] data from 2005 to 2014. NIS is the largest all-payer inpatient database in the USA. It is funded by the US Agency for Healthcare Research and Quality as part of the Healthcare Cost and Utilisation Project [HCUP]. NIS includes discharge visit-level information including diagnoses, visit-related characteristics, and healthcare utilisation data.16 The unit of analysis for inpatient data is the hospital discharge, and a person who is readmitted will be counted for each admission as for a separate inpatient stay. The data were weighted to represent national estimates.17
The primary objective was to describe the prevalence and annual trends in OUD among the hospitalised IBD population. Secondary objectives included: 1] identifying predictors of OUD in IBD; and 2] determining visit-level outcomes associated with OUD in the hospitalised IBD population, specifically length of stay and IBD-related surgery.
IBD inpatient stays were identified using any discharge diagnosis of either Crohn’s disease (International Classification of Diseases, Ninth Revision, Clinical Modification code [ICD-9-CM] 555.x) or ulcerative colitis [ICD-9-CM code 556.x].18,19 Discharges with an associated OUD diagnosis were identified using a schema previously described in an HCUP statistical brief, containing ICD-9-CM codes 304.00–304.02, 304.70–304.72, 305.50–305.52, 965.00–965.02, 965.09, 970.1, E850.0–850.2, E935.0–935.2, and E940.1.6 These ICD-9-CM codes represent active prescription and illicit opioid misuse and are further defined in Supplementary Table 1, available as Supplementary data at ECCO-JCC online. Patients younger than 18 years, older than 100 years, and those with indeterminate IBD [defined as a diagnosis of both ulcerative colitis and Crohn’s disease within the same encounter] were excluded. Patients older than 100 years were excluded in compliance with the HCUP data use agreement requiring privacy protection against individual identification, which may be uncovered when reporting on characteristics of patients at the extremes of age.20,21
Visit- and patient-level characteristics including age, gender, IBD type, primary payer [Medicare, Medicaid, Private, Uninsured, or other], US region [Northeast, Midwest, South, and West], a primary diagnosis of an IBD-related complication, and psychiatric comorbidities [mood disorder, anxiety and substance abuse] were collected. A primary diagnosis of an IBD-related complication was defined by ICD-9-CM code using a previously described schema which includes nine major complications [fistulising disease or intra-abdominal abscess, bowel obstruction, stricturing disease, haematochezia, malnutrition, anaemia, perianal disease, hypovolaemia, or electrolyte abnormality].18,22 Descriptive statistics were reported using means and standard deviation for continuous variables and frequency and percentages for categorical variables. Year-to-year trends in OUD-associated inpatient stays were analysed. A multivariable logistic regression analysis was performed to determine factors associated with having an OUD-related diagnosis; covariates associated with having an OUD-related diagnosis with a p <0.05 on univariable analysis were retained in the multivariable model.
Health care utilisation was reported using length-of-stay measures. A multivariable linear regression model was constructed to measure the association between length of stay in days and having an OUD-related diagnosis. Variables controlling for length of stay were chosen a priori and included IBD type, in-hospital mortality, discharge against medical advice, IBD-related surgery, comorbid conditions, and Elixhauser comorbidity index.23–29 A comorbid condition was defined as one of a composite of visit-associated diagnoses of venous thromboembolism, pneumonia, sepsis, Clostridium difficile infection, blood transfusion requirement, and total parenteral or enteral nutrition. IBD-related surgery was defined using a composite of ICD-9-CM codes for small bowel and colorectal resections.30 These and other ICD-9-CM codes are available in Supplementary Table 1. A subgroup analysis of length of stay was performed for IBD-related surgical stays versus other inpatient stays. All statistical analyses were performed using STATA version 14.0 [Stata Corp, College Station, TX]. The study protocol was reviewed by the institutional review board and deemed exempt [IRB #1708018502].
3. Results
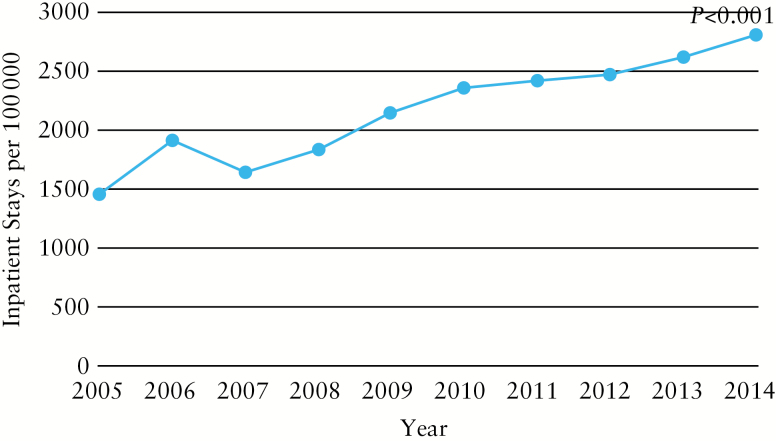
A total of 2596790 weighted adult discharges with any diagnosis of IBD were identified [Figure 1]. After excluding patients older than 100 years and those with diagnoses of both Crohn’s disease and ulcerative colitis, the study population included a total of 2585174 weighted discharges: 36.4% had ulcerative colitis, 63.6% had Crohn’s disease, and 7.5% of discharges were for a primary diagnosis of an IBD-related complication. Further baseline characteristics are reported in Table 1.
Figure 1.
Flow diagram of study population after inclusion and exclusion criteria applied.
Table 1.
Patient- and visit-level characteristics among inflammatory bowel disease patients, associated with opioid use disorder, using univariable and multivariable regression analysis.
| Variable | Overall | Opioid-use disorder | No opioid-use disorder | p-Value | Unadjusted OR | 95% Confidence interval | Adjusted OR | 95% Confidence interval |
|---|---|---|---|---|---|---|---|---|
| Inflammatory bowel disease type | ||||||||
| <0.001 | ||||||||
| Ulcerative colitis | 36.4% | 24.0% | 36.6% | ref | ref | ref | ref | |
| Crohn’s disease | 63.6% | 76.0% | 63.4% | 1.83 | 1.75, 1.91 | 1.69 | 1.61, 1.77 | |
| Primary payer | ||||||||
| <0.001 | ||||||||
| Medicare | 38.0% | 34.5% | 38.1% | 1.29 | 1.23, 1.35 | 1.18 | 1.13, 1.24 | |
| Medicaid | 11.3% | 23.9% | 11.0% | 3.09 | 2.94, 3.25 | 2.42 | 2.29, 2.55 | |
| Private | 41.8% | 29.6% | 42.0% | ref | ref | ref | ref | |
| Uninsured | 5.5% | 8.3% | 5.5% | 2.15 | 2.00, 2.31 | 2.09 | 1.94, 2.26 | |
| Other | 3.4% | 3.7% | 3.4% | 1.55 | 1.40, 1.71 | 1.43 | 1.28, 1.58 | |
| Region | ||||||||
| <0.001 | ||||||||
| Northeast | 22.3% | 23.1% | 22.3% | ref | ref | ref | ref | |
| Midwest | 25.6% | 22.1% | 25.6% | 0.83 | 0.79, 0.88 | 0.77 | 0.73, 0.81 | |
| South | 35.5% | 32.6% | 35.6% | 0.88 | 0.84, 0.93 | 0.84 | 0.79, 0.88 | |
| West | 16.7% | 22.2% | 16.5% | 1.29 | 1.22, 1.37 | 1.33 | 1.26, 1.41 | |
| Primary IBD-related complication | 7.5% | 5.3% | 7.5% | <0.001 | 0.69 | 0.64, 0.75 | 0.69 | 0.63, 0.75 |
| Psychiatric disorder | ||||||||
| Mood disorder | 17.1% | 42.6% | 16.5% | <0.001 | 3.74 | 3.60, 3.88 | 3.06 | 2.93, 3.19 |
| Anxiety | 9.2% | 22.2% | 8.9% | <0.001 | 2.91 | 2.78, 3.04 | 1.87 | 1.78, 1.96 |
| Schizophrenia | 1.3% | 2.9% | 1.2% | <0.001 | 2.42 | 2.17, 2.71 | 1.61 | 1.43, 1.81 |
IBD, inflammatory bowel disease; OR, odds ratio
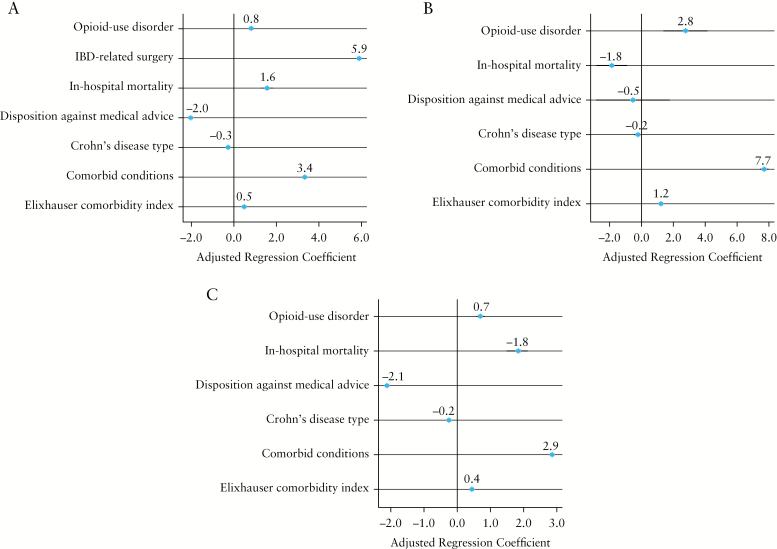
Overall, 2.2% of IBD-related inpatient stays also had an OUD-related diagnosis, with an 8.8% average annual increase in IBD-related inpatient stays with an OUD-related diagnosis from 2005 to 2014 [p <0.001] [Figure 2]. In univariable analysis, IBD patients with OUD-associated inpatient stays were more likely to have Crohn’s disease, to be Medicaid beneficiaries or uninsured, to be hospitalised in the West, and to have comorbid psychiatric disease, and were less likely to be admitted with a primary IBD-related complication [Table 1]. The association between individual IBD-related complications and OUD are reported in Supplementary Table 2, available as Supplementary data at ECCO-JCC online. In multivariable analysis, Crohn’s disease, public payer [Medicare or Medicaid], lack of insurance, and psychiatric comorbidities continued to be associated with a higher likelihood of OUD among IBD inpatient stays, whereas a diagnosis of a primary IBD-related complication was associated with a lower likelihood of an OUD inpatient stay, after controlling for region [Table 1].
Figure 2.
Trends in inflammatory bowel disease patients discharged with an associated opioid-use diagnosis.
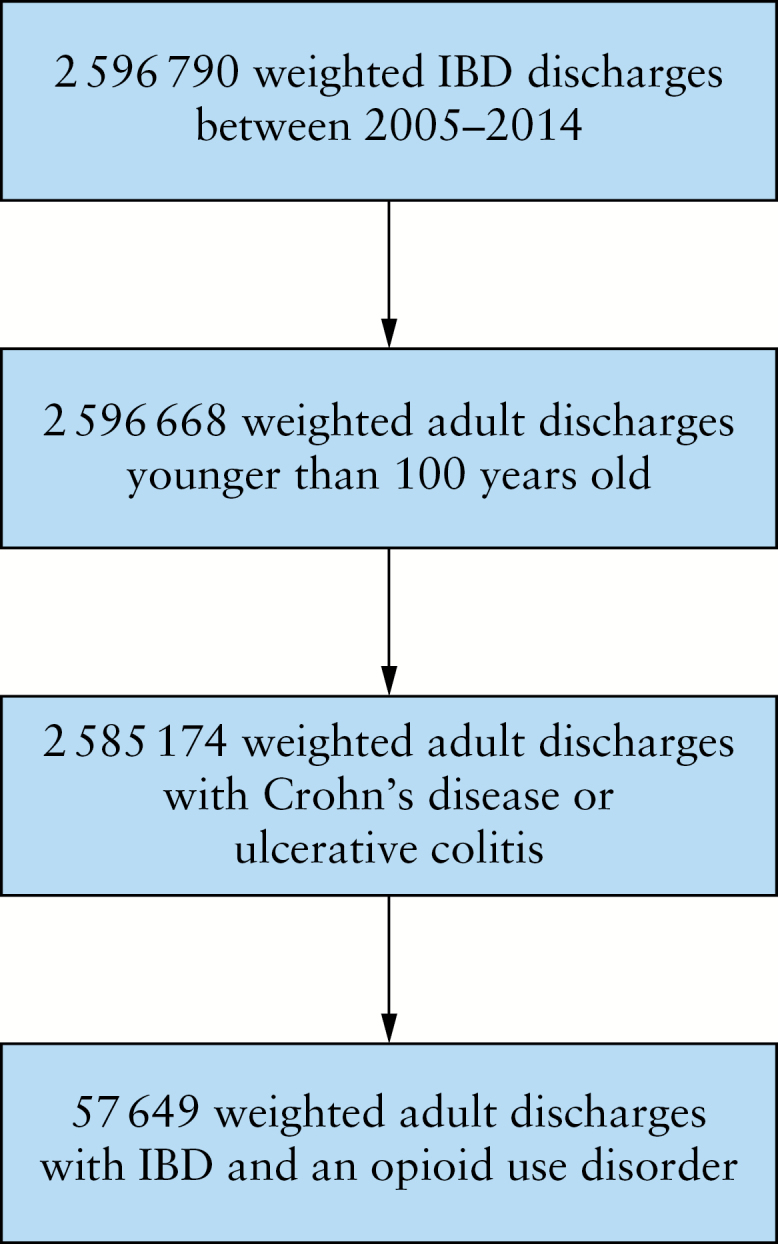
IBD-related inpatient stays with an OUD-related diagnosis were associated with a 0.84 day [95% CI 0.71, 0.97] longer length of stay as compared with other IBD-related inpatient stays, after controlling for Elixhauser comorbidity index, IBD-related surgery, in-hospital death, discharge against medical advice, presence of an associated comorbid condition, and IBD type [Figure 3]. Having an OUD-related diagnosis was associated with a length of stay for surgical discharges increased by 2.79 days [95% CI 1.44, 4.14], and 0.71 days [95% CI 0.59, 0.82] for non-surgical discharges [Figure 3]. Hospitalisations involving an IBD-related surgery were less likely to be associated with an OUD on univariable analysis (unadjusted odds ratio [OR] 0.56, 95% CI 0.52, 0.61) and when controlling for age, IBD type, enteral or parenteral nutrition, and blood transfusion [Supplementary Figure 1, available as Supplementary data at ECCO-JCC online].
Figure 3.
Multivariable model describing the association between length of stay [in days] and opioid use disorder, controlling for a priori covariates. A] All inflammatory bowel disease discharges; B] Subgroup of patients undergoing inflammatory bowel disease [IBD]-related surgery; C] subgroup of patients not undergoing an IBD-related surgery.
4. Discussion
Excessive opioid prescribing is one of many root causes of the opioid epidemic in the USA.31 The published literature has demonstrated an association between prescribing opioids and increased morbidity and mortality among IBD patients, but these studies have focused on the peri-surgical period.32,33 However, outcomes such as overdose deaths are more closely associated with OUD than opioid prescribing alone.4 Thereforeit is critical to investigate OUD in its own right, as opposed to simple post-surgical opioid use. This study focused on IBD patients with a diagnosis of OUD.
Our study demonstrates that OUD-related diagnoses are prevalent among more than 2% of IBD inpatient stays. These OUD estimates for IBD inpatients are higher than the numbers published for the overall inpatient population. Previous studies report a prevalence of OUD of 224.6 inpatient stays per 100000 in the general population.6 This is also higher than outpatient population estimates of OUD, with a reported prevalence of 0.8%.15 Additionally, the rising trend in OUD-related diagnoses among inpatient hospitalisations is evident not only in the general population, but also in the IBD population specifically.13,34–36 Increasing provider awareness of OUD may contribute to rising OUD trends, but its overall influence is likely small, as studies have demonstrated that OUD remains vastly under-recognised.37
Patients with IBD are at risk for opioid misuse, and this is apparent in the higher than average proportion of OUD-related diagnoses among those with inpatient IBD stays.6 Risk factors for OUD can be targeted to identify IBD patients who might benefit from screening for OUD or a review of their opioid prescriptions. We found that Crohn’s disease accounts for more OUD-related discharges than ulcerative colitis [Table 1]. The susceptibility of Crohn’s disease patients to opioid misuse has been reported in a systematic review and is thought to be related to the higher frequency of pain and need for more frequent surgery.11 On the other hand, IBD-related complications and hospitalisations involving an IBD-related surgery were less likely to be associated with OUD diagnoses, possibly secondary to under-recognition of OUD in the setting of severe active disease.37
Further, this study reveals a higher prevalence of OUD-related diagnoses in IBD patients with public payer insurance or who are uninsured. This is consistent with previous findings in other populations that demonstrate a higher rate of opioid use among Medicaid and Medicare enrollees.6,31,34,38–40 Given the inability to determine reasons for Medicaid eligibility in this dataset, it is unclear whether patients with OUD-related diagnoses were more likely to be Medicaid-insured as a result of a disability resulting from chronic pain and substance use disorder.
We also found a strong association between psychiatric disorders and opioid-related diagnoses in IBD hospitalised patients, particularly comorbid mood disorder, anxiety, and schizophrenia. Mood disorders are known to be associated with greater IBD care use and OUD.15,41,42 In a single-centre retrospective study of opioid misuse among IBD patients, Crocker et al. report 20% chronic narcotic use, with depression and anxiety as two independent predictors of misuse.15,43
OUD-related diagnoses were also independently associated with longer length of stay that was particularly marked in the surgical subgroup of patients. A possible explanation of this could be due to more difficulty controlling pain or prolonged ileus from post-surgical opioid requirements. Additionally, patients with OUD are more prone to complications such as respiratory infections or to have co-occurring psychiatric diagnoses that complicate discharge, although we controlled for pneumonia and mood disorders in our multivariable model.44
This study has several limitations. Importantly, because OUD is underdiagnosed, and our data were for inpatient stays, this study likely under-represents OUD among IBD patients.37 Additional factors which could be associated with OUD, such as surgical history, personality traits, family history, and history of substance use, could not be evaluated using this dataset.8,45 Further, as an administrative database, patient identification is limited to ICD-9-CM billing codes which are prone to selection bias. Nonetheless, the ICD-9-CM codes for ulcerative colitis and Crohn’s disease are well validated.18,22 Additionally, as NIS provides visit-level rather than patient-level data, we cannot account for longitudinal follow-up over time or post-discharge outcomes, such as readmissions. This could potentially lead to over-representation of patients who are prone to readmission. One study using HCUP data describes an association between opioid dependence and 30-day readmission in an IBD cohort with an odds ratio of 1.40 [95% CI 1.06, 1.86], but further exploration of the strength of this association is warranted.46
This study also has several strengths. We evaluate the role of OUD on a population level using a large sample size, allowing for generalisability. Though limited by unforeseen confounders, we use multivariable models to control for confounding. Additionally, we specifically identify patients with a billable OUD diagnosis. This allows us to focus on identified OUD disorder which accounts for 5–25% of patients receiving prescription opioids.2 Though OUD is likely under-recognized and underdiagnosed, this differentiates the present study from others that focus on frequency of opioid prescriptions as a marker of opioid misuse or dependence, which is difficult to differentiate from treatment of chronic pain or narcotic diversion, using large datasets.
There has been a recent rise in efforts to bring attention, funding and improved access to OUD treatment. However, to provide high-value interventions, the scope of OUD needs to first be demonstrated. OUD is prevalent among hospitalised IBD patients. Whereas it is important to focus on recognizing pain early in the disease process, and to target inflammation to change the natural history of IBD, we might also consider targeting patients at risk for OUD early in their disease course, substituting opioid alternatives and teaching coping mechanisms.1 For those with identified OUD, treatment should be initiated without stigma. Where risk factors such as Crohn’s disease type and psychiatric comorbidities have been identified, a validated predictive tool should be developed. Patients with IBD and OUD are at high risk for greater health care utilisation and need to be targeted for preventive strategies.
Funding
This work was supported by the Louis and Rachel Rudin Foundation and the National Institute on Drug Abuse [P30DA040500].
Conflict of Interest
ES has received grant/research support from Abbott Laboratories [AbbVie], AstraZeneca, Janssen Research & Development, and Pfizer, and serves as a consultant to AbbVie, Janssen Pharmaceutical, and Takeda Pharmaceuticals. The other authors have no relevant conflicts of interest to disclose.
Author Contributions
SC-M, RR, SG, and CC were involved in the study concept and design, data management, statistical analysis and interpretation of data, drafting of manuscript, and critical revisions. In addition, SC-M and CC were involved in study supervision. ES, RR, AW, SS, and BS were involved in interpretation of data and critical revisions. All authors approved the final version of the article, including the authorship list. Preliminary results were presented at the Crohn’s Colitis Congress, Las Vegas, NV, in January 2018.
Supplementary Data
Supplementary data are available at ECCO-JCC online.
References
- 1. Murthy VH. Ending the opioid epidemic - a call to action. N Engl J Med 2016;375:2413–5. [DOI] [PubMed] [Google Scholar]
- 2. Demsey D, Carr NJ, Clarke H, Vipler S. Managing opioid addiction risk in plastic surgery during the perioperative period. Plast Reconstr Surg 2017;140:613e–9e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Schuckit MA. Treatment of opioid-use disorders. N Engl J Med 2016;375:1596–7. [DOI] [PubMed] [Google Scholar]
- 4. Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid-involved overdose deaths United States, 2010-2015. MMWR Morb Mortal Wkly Rep 2016;65:1445–52. [DOI] [PubMed] [Google Scholar]
- 5. Hedegaard H, Warner M, Miniño AM. Drug overdose deaths in the United States, 1999–2016. NCHS Data Brief 2017;294:1–8. [PubMed] [Google Scholar]
- 6. Weiss AJ, Elixhauser A, Barrett ML. Opioid-related Inpatient Stays and Emergency Department Visits by State, 2009–2014. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, MD: Agency for Healthcare Research and Quality, 2016. [Google Scholar]
- 7. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain - United States, 2016. MMWR Recomm Rep 2016;65:1–49. [DOI] [PubMed] [Google Scholar]
- 8. Ballantyne JC. Opioids for the treatment of chronic pain: mistakes made, lessons learned, and future directions. Anesth Analg 2017;125:1769–78. [DOI] [PubMed] [Google Scholar]
- 9. Targownik LE, Nugent Z, Singh H, Bugden S, Bernstein CN. The prevalence and predictors of opioid use in inflammatory bowel disease: a population-based analysis. Am J Gastroenterol 2014;109:1613–20. [DOI] [PubMed] [Google Scholar]
- 10. Sweeney L, Moss-Morris R, Czuber-Dochan W, Meade L, Chumbley G, Norton C. Systematic review: psychosocial factors associated with pain in inflammatory bowel disease. Aliment Pharmacol Ther 2018;47:715–29. [DOI] [PubMed] [Google Scholar]
- 11. Balbale SN, Trivedi I, O’Dwyer LC, et al. Strategies to identify and reduce opioid misuse among patients with gastrointestinal disorders: a systematic scoping review. Dig Dis Sci 2017;62:2668–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hanson KA, Loftus EV Jr, Harmsen WS, Diehl NN, Zinsmeister AR, Sandborn WJ. Clinical features and outcome of patients with inflammatory bowel disease who use narcotics: a case-control study. Inflamm Bowel Dis 2009;15:772–7. [DOI] [PubMed] [Google Scholar]
- 13. Cross RK, Wilson KT, Binion DG. Narcotic use in patients with Crohn’s disease. Am J Gastroenterol 2005;100:2225–9. [DOI] [PubMed] [Google Scholar]
- 14. Burr NE, Smith C, West R, Hull MA, Subramanian V. Increasing prescription of opiates and mortality in patients with inflammatory bowel diseases in England. Clin Gastroenterol Hepatol 2018;16:534–541.e6. [DOI] [PubMed] [Google Scholar]
- 15. Han B, Compton WM, Blanco C, Crane E, Lee J, Jones CM. Prescription opioid use, misuse, and use disorders in U.S. adults: 2015 national survey on drug use and health. Ann Intern Med 2017;167:293–301. [DOI] [PubMed] [Google Scholar]
- 16. Healthcare Cost and Utilization Project [HCUP]. HCUP National Inpatient Sample [NIS]. Rockville, MD: Agency for Healthcare Research and Quality, 2018. [Google Scholar]
- 17. Healthcare Cost and Resource Utilization Project. Weights for HCUP NIS Data. Rockville, MD: Agency for Healthcare Research and Quality. [Google Scholar]
- 18. Barnes EL, Kochar B, Long MD, et al. Modifiable risk factors for hospital readmission among patients with inflammatory bowel disease in a nationwide database. Inflamm Bowel Dis 2017;23:875–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ananthakrishnan AN, McGinley EL, Binion DG, Saeian K. A nationwide analysis of changes in severity and outcomes of inflammatory bowel disease hospitalisations. J Gastrointest Surg 2011;15:267–76. [DOI] [PubMed] [Google Scholar]
- 20. Agency for the Healthcare Cost and Resource Utilization Project. NIS Checklist. Rockville, MD: Agency for Healthcare Research and Quality, 2017. [Google Scholar]
- 21. Agency for the Healthcare Cost and Resource Utilization Project. Nationwide Data Use Agreement. Rockville, MD: Agency for Healthcare Research and Quality, 2017. [Google Scholar]
- 22. Ananthakrishnan AN, McGinley EL, Binion DG. Does it matter where you are hospitalised for inflammatory bowel disease? A nationwide analysis of hospital volume. Am J Gastroenterol 2008;103:2789–98. [DOI] [PubMed] [Google Scholar]
- 23. Damle RN, Cherng NB, Flahive JM, et al. Clostridium difficile infection after colorectal surgery: a rare but costly complication. J Gastrointest Surg 2014;18:1804–11. [DOI] [PubMed] [Google Scholar]
- 24. Xu J, Tang M, Shen J. Trends and factors affecting hospitalisation costs in patients with inflammatory bowel disease: a two-center study over the past decade. Gastroenterol Res Pract 2013;2013:267630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ananthakrishnan AN, McGinley EL. Infection-related hospitalisations are associated with increased mortality in patients with inflammatory bowel diseases. J Crohns Colitis 2013;7:107–12. [DOI] [PubMed] [Google Scholar]
- 26. Ananthakrishnan AN, McGinley EL, Saeian K, Binion DG. Laparoscopic resection for inflammatory bowel disease: outcomes from a nationwide sample. J Gastrointest Surg 2010;14:58–65. [DOI] [PubMed] [Google Scholar]
- 27. Brady MT, Patts GJ, Rosen A, et al. Postoperative venous thromboembolism in patients undergoing abdominal surgery for IBD: a common but rarely addressed problem. Dis Colon Rectum 2017;60:61–7. [DOI] [PubMed] [Google Scholar]
- 28. Nguyen GC, Munsell M, Harris ML. Nationwide prevalence and prognostic significance of clinically diagnosable protein-calorie malnutrition in hospitalised inflammatory bowel disease patients. Inflamm Bowel Dis 2008;14:1105–11. [DOI] [PubMed] [Google Scholar]
- 29. Ramsey M, Krishna SG, Stanich PP, et al. Inflammatory bowel disease adversely impacts colorectal cancer surgery short-term outcomes and health-care resource utilisation. Clin Transl Gastroenterol 2017;8:e127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Agency for the Healthcare Cost and Resource Utilization Project. Clinical Classifications Software [CCS] for ICD-9-CM. Rockville, MD: Agency for Healthcare Research and Quality, 2017. [Google Scholar]
- 31. Cochran G, Gordon AJ, Lo-Ciganic WH, et al. An examination of claims-based predictors of overdose from a large Medicaid program. Med Care 2017;55:291–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Docherty MJ, Jones RC III, Wallace MS. Managing pain in inflammatory bowel disease. Gastroenterol Hepatol 2011;7:592–601. [PMC free article] [PubMed] [Google Scholar]
- 33. Lichtenstein GR, Feagan BG, Cohen RD, et al. Serious infection and mortality in patients with Crohn’s disease: more than 5 years of follow-up in the TREAT™ registry. Am J Gastroenterol 2012;107:1409–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Shiner B, Leonard Westgate C, Bernardy NC, Schnurr PP, Watts BV. Trends in opioid use disorder diagnoses and medication treatment among veterans with posttraumatic stress disorder. J Dual Diagn 2017;13:201–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Srinath A, Young E, Szigethy E. Pain management in patients with inflammatory bowel disease: translational approaches from bench to bedside. Inflamm Bowel Dis 2014;20:2433–49. [DOI] [PubMed] [Google Scholar]
- 36. Mazer-Amirshahi M, Mullins PM, Rasooly I, van den Anker J, Pines JM. Rising opioid prescribing in adult U.S. emergency department visits: 2001-2010. Acad Emerg Med 2014;21:236–43. [DOI] [PubMed] [Google Scholar]
- 37. Kirson NY, Shei A, Rice JB, et al. The burden of undiagnosed opioid abuse among commercially insured individuals. Pain Med 2015;16:1325–32. [DOI] [PubMed] [Google Scholar]
- 38. Katz C, El-Gabalawy R, Keyes KM, Martins SS, Sareen J. Risk factors for incident nonmedical prescription opioid use and abuse and dependence: results from a longitudinal nationally representative sample. Drug Alcohol Depend 2013;132:107–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Larney S, Bohnert AS, Ganoczy D, et al. Mortality among older adults with opioid use disorders in the Veteran’s Health Administration, 2000-2011. Drug Alcohol Depend 2015;147:32–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Guy GP Jr, Zhang K, Bohm MK, et al. Vital signs: changes in opioid prescribing in the United States, 2006-2015. MMWR Morb Mortal Wkly Rep 2017;66:697–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Poojary P, Saha A, Chauhan K, et al. Predictors of hospital readmissions for ulcerative colitis in the United States: a national database study. Inflamm Bowel Dis 2017;23:347–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Edwards JT, Radford-Smith GL, Florin TH. Chronic narcotic use in inflammatory bowel disease patients: prevalence and clinical characteristics. J Gastroenterol Hepatol 2001;16:1235–8. [DOI] [PubMed] [Google Scholar]
- 43. Crocker JA, Yu H, Conaway M, Tuskey AG, Behm BW. Narcotic use and misuse in Crohn’s disease. Inflamm Bowel Dis 2014;20:2234–8. [DOI] [PubMed] [Google Scholar]
- 44. Menendez ME, Ring D, Bateman BT. Preoperative opioid misuse is associated with increased morbidity and mortality after elective orthopaedic surgery. Clin Orthop Relat Res 2015;473:2402–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ahn WY, Vassileva J. Machine-learning identifies substance-specific behavioral markers for opiate and stimulant dependence. Drug Alcohol Depend 2016;161:247–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Micic D, Gaetano JN, Rubin JN, et al. Factors associated with readmission to the hospital within 30 days in patients with inflammatory bowel disease. Plos One 2017;12:e0182900. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.