Abstract
Demodex mite infestation of the palpebral conjunctiva as focal inflammatory nodule has been not reported. A 46-year-old man presented with lower palpebral conjunctival nodules in his left eye. Slit-lamp examination showed focal inflammatory nodules at the inferior palpebral conjunctiva accompanied by conjunctival hyperemia and purulent secretion. Excisional biopsy of this lesion was performed. Pathological evaluations revealed inflammatory granuloma associated with Demodex species in the palpebral conjunctiva. This is the first report of Demodex-related palpebral conjunctival inflammatory nodule and may be helpful in future Demodex-associated studies.
Keywords: Conjunctival nodule, Demodex, demodicosis
Demodex (class Arachnida, superorder Acariformes), a microscopic, obligate, and elongated mite, is the most common ectoparasite on the human body surface. There are many species of Demodex; however, only Demodex folliculorum and Demodex brevis are found on the human body surface.[1] D. folliculorum is found in hair and lash follicles, whereas D. brevis exists in sebaceous and meibomian glands. They often coexist on the same areas of the skin, such as the face, cheeks, forehead, nose, and external ear tract, where active sebum excretion favors their habitation and breeding.[2,3] Several cases of ocular Demodex infestation have been reported in various ophthalmic diseases such as trichiasis, madarosis, blepharitis, lipid tear deficiency, tear film disturbance, chalazia, and keratoconjunctivitis.[4,5] However, until now, focal inflammatory nodule at the palpebral conjunctiva associated with this organism has not been reported. Here, we describe the first case of focal inflammatory nodules on the palpebral conjunctiva associated with Demodex species in a healthy middle-aged man.
Case Report
A 46-year-old man visited our outpatient clinic with lower palpebral conjunctival masses in his left eye accompanied by ocular pain, tenderness, foreign body sensation, tearing, and conjunctival redness 4 weeks before consult. The patient had no history of prior ocular or immunological diseases such as blepharitis, chalazia, or rosacea. Three weeks before visit, the patient underwent incisional drainage procedure under suspicion of chalazion at the private clinic; however, there was no drainage. Following 2 weeks of oral antibiotics and anti-inflammatory drugs, there was no improvement at the lesion. On examination, his visual acuity in both the eyes was 20/20 without correction. Slit-lamp examination showed hyperemic conjunctiva with mucopurulent secretions in the inferior fornix. By pulling the inferior eyelids, about 1 mm × 1 mm sized 2 focal inflammatory nodules were observed in the palpebral conjunctival surface. A photograph of the inferior palpebral conjunctiva was obtained through the slit lamp [Fig. 1]. Cylindrical dandruff was not observed on the eyelashes. The findings of the right eye were unremarkable.
Figure 1.

Slit-lamp photograph of a 46-year-old man with palpebral focal conjunctival nodule in his left eye
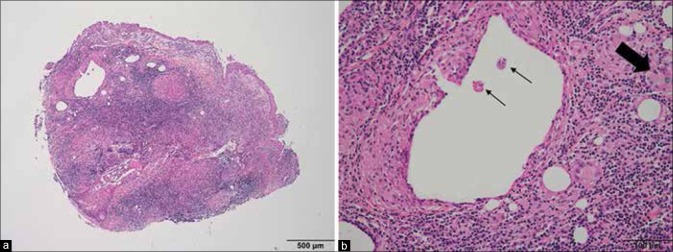
Excisional biopsy of the lesions was performed. Between the two nodules, we found a presence of the Demodex mites in the deep-located nodule. On low-power examination, the specimen had dense lymphocytic infiltration with granuloma formation and lipid dropout spaces associated with foreign body-type granulomatous inflammation [Fig. 2a]. A dilated residual gland filled with inflammatory exudates was also visible. On high-power examination, Demodex organisms in a lipid dropout space and foreign body-type multinucleated giant cell engulfing a mite were observed [Fig. 2b]. Periodic acid-Schiff and tissue Gram stains did not demonstrate fungal or bacterial infections. Therefore, pathological evaluation revealed that the inflammatory granuloma was associated with Demodex species [Fig. 2].
Figure 2.
Biopsy of lower palpebral conjunctival masses showed Demodex-associated inflammatory granuloma (a) Lipid dropout space associated with foreign body-type granulomatous inflammation was observed (H and E, ×40) (b) Demodex organisms in lipid dropout space (small arrows) and a mite engulfed by a multinucleated giant cell were observed (large arrow) (H and E, ×200)
After 1 week, the conjunctiva was no longer congested and the palpebral conjunctival lesion was stable without surgical complication. Weekly lid scrubs with 50% tea tree oil (TTO) were performed, and daily lid scrubs with 10% TTO shampoo were advised for 2 months according to a previously reported method.[4] One year after the operation, the lesion was stable without evidence of recurrence.
Discussion
Demodex infestation has been reported in various dermatologic conditions, such as pustular folliculitis, papulopustular scalp eruptions, perioral dermatitis, and hyperpigmented patches of the face.[2,3] In the eyes, besides blepharitis, ocular demodicosis has been also reported as various presentations such as eyelash loss or abnormal alignment as well as lipid tear deficiency due to chronic inflammation in the meibomian gland, conjunctivitis, recurrent chalazia, or sight-threatening keratitis.[4,5,6] However, until now, ocular demodicosis presenting with palpebral conjunctival inflammatory nodule has not been reported.
In the present case, a healthy 46-year-old man presented at our hospital with lower palpebral conjunctival mass in his eyes. The result of pathological evaluation was consistent with granulomatous inflammation associated with the Demodex species. Although exact identification between D. folliculorum and D. brevis by pathologic examination is very difficult, we assume that D. brevis was the causative organism rather than D. folliculorum because lesions of the posterior lid surface are usually associated with D. brevis as mentioned above. As we diagnosed ocular demodicosis by tissue sampling and by hematoxylin and eosin staining instead of lash sampling and microscopic examination, which is the current definitive diagnostic method, inaccurate differentiation between these two species remains a limitation of this report.
Previously published articles described the ocular Demodex-killing effects of TTO in vitro and in vivo and introduced a new clinical treatment and lid scrubbing with TTO.[4,7] In the same manner, our patient was also successfully treated with additional lid scrubbing with TTO after conjunctival mass excision.
Clinical aspects of chalazia are characteristically presenting as a firm, large, and painless lid nodule without definitive inflammation. On the other hand, our patient showed about 1 mm × 1 mm sized soft 2 focal inflammatory nodules in the palpebral conjunctival surface accompanied with ocular pain, tenderness, foreign body sensation, tearing, and conjunctival redness. In addition, there was a history of no internal material drainage by surgery performed at the local clinic. Therefore, we could diagnose as focal inflammatory nodules rather than chalazia due to these differences.
Conclusion
To the best of our knowledge, this is the first case report of ocular demodicosis initially presenting as focal inflammatory nodule at the palpebral conjunctiva. In addition, this parasite needs to be taken into consideration in the differential diagnosis of associated organisms of inflammatory granulomatous nodule in the palpebral conjunctiva.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The study was partially supported by the CNUH Biomedical Research Institute (CRI 13906-22).
References
- 1.English FP, Nutting WB. Demodicosis of ophthalmic concern. Am J Ophthalmol. 1981;91:362–72. doi: 10.1016/0002-9394(81)90291-9. [DOI] [PubMed] [Google Scholar]
- 2.Baima B, Sticherling M. Demodicidosis revisited. Acta Derm Venereol. 2002;82:3–6. doi: 10.1080/000155502753600795. [DOI] [PubMed] [Google Scholar]
- 3.Forton F, Germaux MA, Brasseur T, De Liever A, Laporte M, Mathys C, et al. Demodicosis and rosacea: Epidemiology and significance in daily dermatologic practice. J Am Acad Dermatol. 2005;52:74–87. doi: 10.1016/j.jaad.2004.05.034. [DOI] [PubMed] [Google Scholar]
- 4.Gao YY, Di Pascuale MA, Elizondo A, Tseng SC. Clinical treatment of ocular demodecosis by lid scrub with tea tree oil. Cornea. 2007;26:136–43. doi: 10.1097/01.ico.0000244870.62384.79. [DOI] [PubMed] [Google Scholar]
- 5.Kheirkhah A, Casas V, Li W, Raju VK, Tseng SC. Corneal manifestations of ocular demodex infestation. Am J Ophthalmol. 2007;143:743–9. doi: 10.1016/j.ajo.2007.01.054. [DOI] [PubMed] [Google Scholar]
- 6.Liu J, Sheha H, Tseng SC. Pathogenic role of demodex mites in blepharitis. Curr Opin Allergy Clin Immunol. 2010;10:505–10. doi: 10.1097/ACI.0b013e32833df9f4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gao YY, Di Pascuale MA, Li W, Baradaran-Rafii A, Elizondo A, Kuo CL, et al. In vitro and in vivo killing of ocular demodex by tea tree oil. Br J Ophthalmol. 2005;89:1468–73. doi: 10.1136/bjo.2005.072363. [DOI] [PMC free article] [PubMed] [Google Scholar]